Introduction
A major public health issue and one of the leading
causes of death worldwide is breast cancer (BC). BC is the third
most prevalent malignancy in Thailand, and its occurrence is
steadily rising (1,2). The World Health Organization has
reported that >20,000 new cases of BC (11.6% of all cases) were
reported in Thailand in 2020(3).
There are currently only a few standard treatments available for
breast cancer because of the negative side-effects, high cost and
cancer development associated with current treatments. New
complementary therapies are therefore required and one option that
has drawn interest from cancer patients is treatment with Thai
traditional formulary medicine (TTFM) or a combination of
contemporary medicine and specific natural items, such as herbs
(4-6).
TTFMs are a valuable legacy of Thai ancestral
knowledge. Numerous herbs used in TTFM recipes have been previously
reported to have anti-fungal, anti-bacterial, anti-genotoxic,
anti-inflammatory and anti-cancer properties (7-9).
Over hundreds of years, different TTFM recipes have been
successfully utilized to treat symptoms related to breast and
intestinal problems. The TTFM recipe used in the present study was
taken from the TTFM, Atisaravak scripture and included seventeen
dried herbs (Table I).
 | Table IThe portion of the herb used and the
amount of each ingredient in the Thai traditional formulary
medicine formulation. |
Table I
The portion of the herb used and the
amount of each ingredient in the Thai traditional formulary
medicine formulation.
| Scientific
name | Common name | Part used | Ratio (%) | (Refs.) |
|---|
| Ligusticum
sinense Oliv.cv. Chaxiong | Sichuan lovage | Rhizome | 4.76 | (10,11) |
| Angelica
dahurica | Chinese
angelica | Root | 4.76 | (12) |
| Atractylodes
lancea (Thunb.) DC | Cang Zhu | Rhizome | 4.76 | (13) |
| Artemisia
annua L | Sweet wormwood | Leaf and
flower | 4.76 | (14) |
| Angelica
sinensis (Oliv.) Diels | Danggui | Root | 4.76 | N/A |
| Lepidium
sativum L | Garden cress | Seed | 4.76 | (15) |
| Nigella
sativa L | Black cumin | Seed | 4.76 | (16,17) |
| Cuminum
cyminum L | Cumin | Fruit | 4.76 | (17) |
| Foeniculum
vulgare Miller | Fennel | Fruit | 4.76 | N/A |
| Anethum
graveolens L | Dill | Fruit | 4.76 | (18) |
| Amomum
villosum Lour | Bastard
cardamom | Seed | 4.76 | (19) |
| Amomum
kravanh | Cambodian
cardamom | Fruit | 4.76 | (20) |
| Syzygium
aromaticum (L.) Merr. & L.M.Perry | Cloves | Flower | 4.76 | (21) |
| Caesalpinia
sappan L | Sappan Wood | Wood | 9.52 | (22) |
| Maclura
cochinchinensis (Lour.) Corner | Cockspur thorn | Wood | 9.52 | N/A |
| Curcuma
zedoaria | Zedoary | Rhizome | 9.52 | (23) |
| Punica
granatum L | Pomegranate | Peel | 9.52 | (24,25) |
Moreover, consuming a diet rich in micronutrients
such as fiber, minerals, vitamins and phytonutrients has been
reported to reduce the risk of BC and to demonstrated preventative
anti-cancer activity (26). Many
phytochemical compounds including phenolic compounds (such as,
coumarins, flavonoids, lignans, phenolic acids, quinones, stilbenes
and tannins), nitrogen compounds (such as alkaloids, amines and
betalains), vitamins (such as A, C, D and E) and terpenes
(including carotenoids) derived from certain herbs in the TTFM
recipe have been reported to have the cytotoxic effects against
certain cancer cells, such as non-small cell lung cancer (13,14),
cervical cancer (27), colon cancer
(28), gastric cancer (29), leukemic cancer (15,24)
and breast cancer (22,23,25).
Furthermore, a previous in vitro study reported that a
variety of phytochemical substances plays a crucial part in
inflammation in breast cancer (30).
The mixture of TTFM recipe in this combination may
balance the effects of each phytochemical, lessen any adverse
effects and increase the efficacy of the treatment because each
herb, according to TTFM, possesses a range of medicinal
characteristics. However, no research has either proven the
efficacy of the TTFM formula against breast cancer cells or has
elucidated the underlying molecular mechanisms (31).
Therefore, the present study assessed the secondary
metabolites (phytochemical profile) of the TTFM extracts and their
effects against cancer cells as well as biological properties, such
as their effects on programmed cell death and the effect of whole
RNA expression upon treatment in breast cancer cells.
Materials and methods
Preparation of TTFM extraction
The dried plant materials (Table I) were purchased from a Thai
traditional medicine shop (Chao-Krom-Poe Dispensary Pharmacy). The
mixed plant materials were boiled in 3.15 l of water for 30 min.
After passing through the sterile voile fabric, the sample was
centrifuged at 1,610 x g at 4˚C for 20 min. The pellet was
discarded, while the supernatants were lyophilized and then kept at
-20˚C until use.
High-performance liquid chromatography
(HPLC) fractionation
HPLC fractionation was performed before liquid
chromatography with tandem mass spectroscopy (LC-MS/MS) analysis.
Briefly, 20 µg of dried TTFM extracts were incubated in 90%
methanol at 25˚C and shaken at 1,300 rpm for 20 min. The mixture
was then centrifuged at 17,000 x g at 4˚C for 10 min, the
supernatants were then collected and transferred to an HPLC vial
(Agilent Technologies, Inc.). Fractionations were performed using
reversed phase high performance liquid chromatography (RP-HPLC) on
an Agilent 1200 HPLC device coupled with a 1260 Infinity II with a
UV detector (Agilent Technologies, Inc.). The solvents used for
HPLC fractionation were ultrapure water (type I water) subjected to
purification with a MilliQ system (Merck KGaA) to obtain an
electrical resistance of 18.2 MW as solvent A and acetonitrile of
HPLC grade (RCI Labscan, Ltd.) as solvent B. The column stationary
phase was graphitic porous carbon (Hypercarb; 100x2.1 mm; particle
size, 3 µm; Thermo Fisher Scientific, Inc.) with a controlled
temperature of 65±0.8˚C. The mobile phases with a flow rate of 0.2
ml/min were programmed as follows: 0-5 min, isocratic elution of 5%
B; 5-40 min, gradient elution of 2.28% B/min; 40-50 min, isocratic
elution of 100% B (column wash); 50-65 min, isocratic elution of 5%
B (recondition of the HPLC column); four fractions (2 ml each) were
collected for LC-MS/MS analysis.
Ultra-high performance liquid
chromatography-MS/MS (UHPLC-MS/MS) characterization
Data dependent analysis was used for untargeted
metabolomics measurements, which were performed using a Dionex
Ultimate 3000 HPLC coupled with an Orbitrap Q exactive focus mass
spectrometer (Thermo Fisher Scientific, Inc.). The heated
electrospray ionisation source parameters were set as follows:
Sheath gas flow rate of 30 arbitrary unit; aux gas flow of 10
l/min; spray voltage of 3 kV; capillary temperature of 350˚C;
S-lens RF level of 60; auxiliary gas heater temperature of 300˚C.
Separation of polar metabolites was performed using an Acclaim™
Polar Advantage II (250x3 mm; Thermo Fisher Scientific, Inc.) set
to a 3 µm particle size. The mobile phases were prepared according
to the aforementioned method. The settings for the LC gradient were
0-5 min, isocratic elution of 1% B; 5-40 min, gradient elution of
1.5% B/min; 40-47 min, isocratic elution of 100% B (column wash);
47-65 min, isocratic elution of 1% B (recondition of the HPLC
column).
Differential peak identification was performed using
MS-Dial software (version 4.90) (32). Raw files were converted into
Analysis Base Framework (ABF) format using an ABF file converter
(http://www.reifycs.com/AbfConverter/index.html). In
MS-DIAL, the converted files were processed with default parameters
for deconvolution, peak picking, alignment and compound
identification based on public MSP-formatted libraries (MSPs) for
both positive and negative ionization modes (http://prime.psc.riken.jp/compms/msdial/main.html#MSP).
The MS/MS analytical conditions (scan range, 70-1035 m/z) comprised
a minimum peak height of 1,000 amplitude, m/z search tolerance of
0.01 Da, data acquisition with centroid mode and the filter of peak
alignment before removal of features based on blank
information.
Cell culture
The mouse 4T1 cell line [American Type Culture
Collection (ATCC) CRL-2539™], which mimics stage IV human breast
cancer, were cultured in RPMI-1640 medium (Gibco; Thermo Fisher
Scientific, Inc.) supplemented with 10% heat-inactivated fetal
bovine serum (Gibco; Thermo Fisher Scientific, Inc.), 2 mM
L-glutamine (Gibco; Thermo Fisher Scientific, Inc.), 1 mM sodium
pyruvate (Gibco; Thermo Fisher Scientific, Inc.), 10 mM HEPES
(Gibco; Thermo Fisher Scientific, Inc.), 4,500 mg/l glucose (Gibco;
Thermo Fisher Scientific, Inc.), 1,500 mg/l sodium bicarbonate
(Gibco; Thermo Fisher Scientific, Inc.) and 1%
Antibiotic-Antimycotic (Gibco; Thermo Fisher Scientific, Inc.). The
breast cancer MDA-MB-231 cell line (gift from The Ketchart
Laboratory, Faculty of Medicine, Chulalongkorn University) was
cultured in DMEM supplemented with 10% heat-inactivated fetal
bovine serum (Gibco; Thermo Fisher Scientific, Inc.) and 1%
Antibiotic-Antimycotic (Gibco; Thermo Fisher Scientific, Inc.). The
study also included the normal EpH4-Ev breast cell line (ATCC
CRL-30639™), as the control, which was cultured in Dulbecco's
Modified Eagle's Medium (DMEM, Gibco; Thermo Fisher Scientific,
Inc.) supplemented with 10% Calf Bovine Serum (ATCC), 1.2 µg/ml
puromycin dihydrochloride (Merck KGaA) and 1%
Antibiotic-Antimycotic (Gibco; Thermo Fisher Scientific, Inc.). All
cells were maintained under 5% CO2 at 37˚C.
Cell viability assay
An MTT test was used to perform a cell viability
assay. Briefly, each of the cell lines were seeded
(1x104) in 96 well-microplates and incubated under 5%
CO2 at 37˚C for 24 h. Then, cells were exposed to TTFM
extracts (final concentrations, 0, 25, 50, 75, 100, 200 and 400
µg/ml). After adding extracts, cells were incubated for 5 days
without changing the medium or substituting the TTFM extracts.
After incubation, treated cells were assessed with 0.4 mg/m of the
membrane-permeable MTT dye (Abcam) for 3 h. The water-insoluble
formazan crystals were dissolved in DMSO (Merck KGaA) and the
absorbance (570 nm) was quantified using a microplate reader
(Thermo Fisher Scientific, Inc.).
Apoptosis assay
4T1 cells were seeded (1x105) in 24
well-microplates and incubated under 5% CO2 at 37˚C for
24 h. Cells were then treated with TTFM extracts and incubated at
37˚C for 72 h. The cells were then harvested and washed twice with
cold PBS (Gibco; Thermo Fisher Scientific, Inc.). Cells were
stained using a FITC Annexin V Apoptosis detection kit with
propidium iodide (Biolegend, Inc.) in the dark at 25˚C for 15 min.
Finally, the fluorescent intensity of stained cells was evaluated
using a BD™ LSR II flow cytometer (BD Biosciences). The data were
analyzed using BD FACSDiva™ Software v. 6.1.3 (BD Biosciences).
RNA preparation and sequencing
(RNA-seq)
Total RNA was extracted from TTFM-treated 4T1 cells,
TTFM-treated EpH4-Ev cells, and untreated cells using a RNeasy mini
kit (Qiagen, Inc.). The concentration and RNA integrity were
assessed using a Qubit RNA assay kit and Qubit RNA IQ assay kit
(Invitrogen; Thermo Fisher Scientific, Inc.). A
Bioanalyzer® (Agilent Technologies, Inc.) was used to
verify the quality and the integrity of processed samples. The
library preparation and RNA sequencing were performed commercially
by Vishuo Biomedical Pte., Ltd. according to the manufacturer's
standard protocols. The library preparation was performed using a
NEBNext® Ultra™ RNA Library Prep Kit for
Illumina® (Illumina, Inc.). Briefly, 1 g of total RNA
was utilized. Oligo(dT) beads were used to isolate poly(A) mRNA.
High temperature (94˚C) and divalent cations were used to fragment
the mRNA. Random primers from the Library Prep Kit were used for
cDNA synthesis. For first strand cDNA synthesis, 25˚C (10 min),
42˚C (15 min), and 70˚C (15 min) were used, followed by second
strand cDNA synthesis at 16˚C (1 h). T-A ligation was then used to
add adaptors to both ends of the purified double-stranded cDNA,
which had previously been treated to repair both ends and add a
dA-tail in a single reaction. Then, DNA clean beads were used for
size-selection (>200 nt) of the adaptor-ligated DNA. Each
library was verified using an Bioanalyzer® Agilent High
Sensitivity Chip (Agilent Technologies, Inc.) and quantified using
KAPA Library Quantification Kits (Hoffmann-La Roche, Ltd).
Subsequently, libraries with various indexes were multiplexed (3 nM
final concentration) and loaded onto a NovaSeq 6000 instrument
(Illumina, Inc.) with NovaSeq 6000 SP Reagent Kit v1.5 (300 cycles;
Illumina, Inc.) for paired-end (2x150) sequencing according to the
manufacturer's protocols.
RNA-seq data analysis
For the analysis of differentially expressed genes,
the RNA-seq data were processed as previously reported (33). The trimmed reads were aligned to the
mouse reference genome (GRCm39/mm10) using HISAT2 v.2.1.0(34) with default parameters. The
prevalence of transcripts was quantified using Cufflinks
v.2.2.1(35). Differentially
expressed genes were then investigated using DESeq2 (version
1.24.0) (36) with an adjusted
cut-off of P<0.05. The gene ontology and relevant biological
pathways were identified using GOSeq (v1.34.1) (37) and Kyoto Encyclopedia of Genes and
Genomes (KEGG) database (38),
respectively.
Reverse transcription-quantitative
(RT-q)PCR analysis
Total RNA was extracted from TTFM-treated 4T1 cells,
TTFM-treated EpH4-Ev cells, and untreated cells according to the
aforementioned method. Reverse transcription was performed by
mixing the total RNA with oligo(dT) primers and incubated at 65˚C
for 5 min. After that the component was mixed with 4 µl of 5x
reaction buffer for RT (Thermo Fisher Scientific, Inc.), 0.5 µl of
40 U/µl Ribolock RNase Inhibitor (Thermo Fisher Scientific, Inc.),
1 µl of 200 U/µl RevertAid Reverse Transcriptase (Thermo Fisher
Scientific, Inc.) and 2 µl of 10 mM dNTP mix (Promega) at 42˚C for
1 h. Next, the RT-qPCR assay was performed using the StepOnePlus™
Real-Time PCR System (Applied Biosystems; Thermo Fisher Scientific,
Inc.). Amplifications were performed in 10 µl reaction solutions
containing 5 µl of 2x PanGreen™ Universal SYBR Green Master Mix
(Bio-Helix Co., Ltd.), 0.25 µl each of 10 µM gene-specific primers,
3.5 µM of nuclease-free water and 1 µl of cDNA. The PCR conditions
were as follows: 95˚C for 2 min; followed by 40 cycles of 95˚C for
15 s, 60˚C for 20 s and 75˚C for 30 s. The specificity of each pair
of primers was evaluated using melting curve analysis (95˚C for 15
s, 60˚C for 1 min and 95˚C for 15 s). The experiment was performed
with technical triplicates. The relative expression of target genes
normalized with Actb was determined using the
2-ΔΔCq method (39). The
primers for Slc5a8, Arhgap9, and Cybb were
designed in the present study, whereas the primers for Actb,
Bcl2, Bax, Casp8, and Casp9 were used
according to previous studies (40-43).
The gene-specific primers used are presented in Table SI.
Statistical analysis
The apoptosis assay was assessed using one-way ANOVA
followed by Tukey's multiple comparisons test. The cell viability
and quantification of mRNA expression were assessed using the
unpaired t-test. Statistical analysis was performed using
GraphPad Prism version 9.3.0 (Dotmatics). P<0.05 was considered
to indicate a statistically significant difference.
Results
Metabolite profiles of TTFM
extracts
The LC-MS/MS data were processed and evaluated using
MS-Dial software to identify the TTFM extract profiles. Based on
the combined information from accurate mass, isotope ratios,
retention-time prediction and MS/MS fragment matching, a total of
226 compounds were identified in the TTFM extract. A total of 64
compounds were identified in the negative ion mode (Table SII) and 162 compounds were
identified in the positive ion mode (Table SIII). Several of the metabolites
identified have been previously reported to have anti-cancer
properties, including betaine, costunolide, cyanidin, d-limonene,
geranic acid, ginkgolide A, hinokitiol, l-arginine, oleic acid,
parecoxib, pentadecanoic acid, sinapic acid, syringic acid,
tanshinone I, tryptanthrin and vinpocetine (Table II).
 | Table IICompounds extracted from Thai
traditional formulary medicine reported to exert anti-cancer
properties. |
Table II
Compounds extracted from Thai
traditional formulary medicine reported to exert anti-cancer
properties.
| Compound name | Pathway | Cancer type | (Refs.) |
|---|
| Betaine | Suppression of the
colon tumor formation by inhibition of NF-κB and inflammatory
cytokines such as TNF-α, IL-6, iNOS and COX-2 | Colitis-associated
colon cancer | (55) |
| Costunolide | Elevation of the
expression of pro-apoptotic protein Bax while lowering the
expression of anti-apoptotic proteins, including Bcl-2 and
Bcl-xL | Skin cancer and
Melanoma | (44,45) |
| | Suppression of
melanoma cell growth via the AKT/mTOR signaling pathway | | |
| Cyanidin | Activation of
apoptosis by caspase-3 cleavage and DNA fragmentation through the
Bcl-2 and Bax signaling pathway | Breast cancer | (46,47) |
| | Down-regulation of
Sirt1 expression via inhibition of mRNA translation | | |
| D-limonene | Suppression of lung
cancer growth and induction of apoptosis via a mechanism involving
autophagy | Lung cancer | (60) |
| Geranic acid | Induction of
apoptosis by induction of the activity of the caspase-3
protein | Colon cancer | (61) |
| Ginkgolide A | Inhibitory effect
appeared to be cell cycle blockage at G0/G1
to S phase | Ovarian cancer | (56) |
| Hinokitiol | Increased reactive
oxygen species level and activated apoptosis and autophagy through
the ERK1/2 signaling pathway | Endometrial cancer
and breast cancer | (48,49) |
| | Inhibition of
heparanase via extracellular signal-regulated kinase and protein
kinase B signaling pathway | | |
| L-arginine | Enhancement of
anti-tumor effects in breast cancer mice by improving the immune
status | Breast cancer | (62) |
| | Increased the
proliferation of CD8+ and CD4+ Th1 effector T
cells and IFN-γ, as well as decreased frequency of myeloid-derived
suppressor cells | | |
| Oleic acid | Decreased
IFN-γ-induced expression of PD-L1, Bax, Bcl-2 and caspase 3
Inhibition of PD-1 expression and induction of apoptosis via STAT
phosphorylation | Lung cancer | (50) |
| Parecoxib | Inhibition of
epithelial-mesenchymal transition and metastasis by downregulation
of the Wnt/β-catenin signaling pathway | Colon cancer | (57) |
| Pentadecanoic
acid | Increased the
expression of cleaved caspase-3, -7, -8 and -9, which are involved
in the induction of apoptosis | Breast cancer | (51) |
| | Inhibition of
JAK2/STAT3 signaling pathway | | |
| Sinapic acid | Downregulation of
the AKT/Gsk-3β signal pathway | Pancreatic
cancer | (58) |
| Syringic acid | Induction of
apoptosis, inhibition of inflammation and the suppression of the
mTOR/AKT signaling pathway | Gastric cancer | (52) |
| Tanshinone I | Induction of
apoptosis by activation of the expression of caspase 3,
downregulation of the level of the anti-apoptotic protein, Bcl-2,
and upregulation of the level of the pro-apoptotic protein,
Bax | Breast cancer | (53) |
| Tryptanthrin | Suppression of the
expression of NOS1, COX-2 and NF-κB in mouse tumor tissues, and
regulation of IL-2, IL-10 and TNF-α | Breast cancer | (59) |
| | Exertion of
anti-cancer activities via modulation of the inflammatory
epithelial-mesenchymal transition | | |
| Vinpocetine | Activation of Akt
and STAT3 but had no effects on MAPK signaling pathways | Breast cancer | (54) |
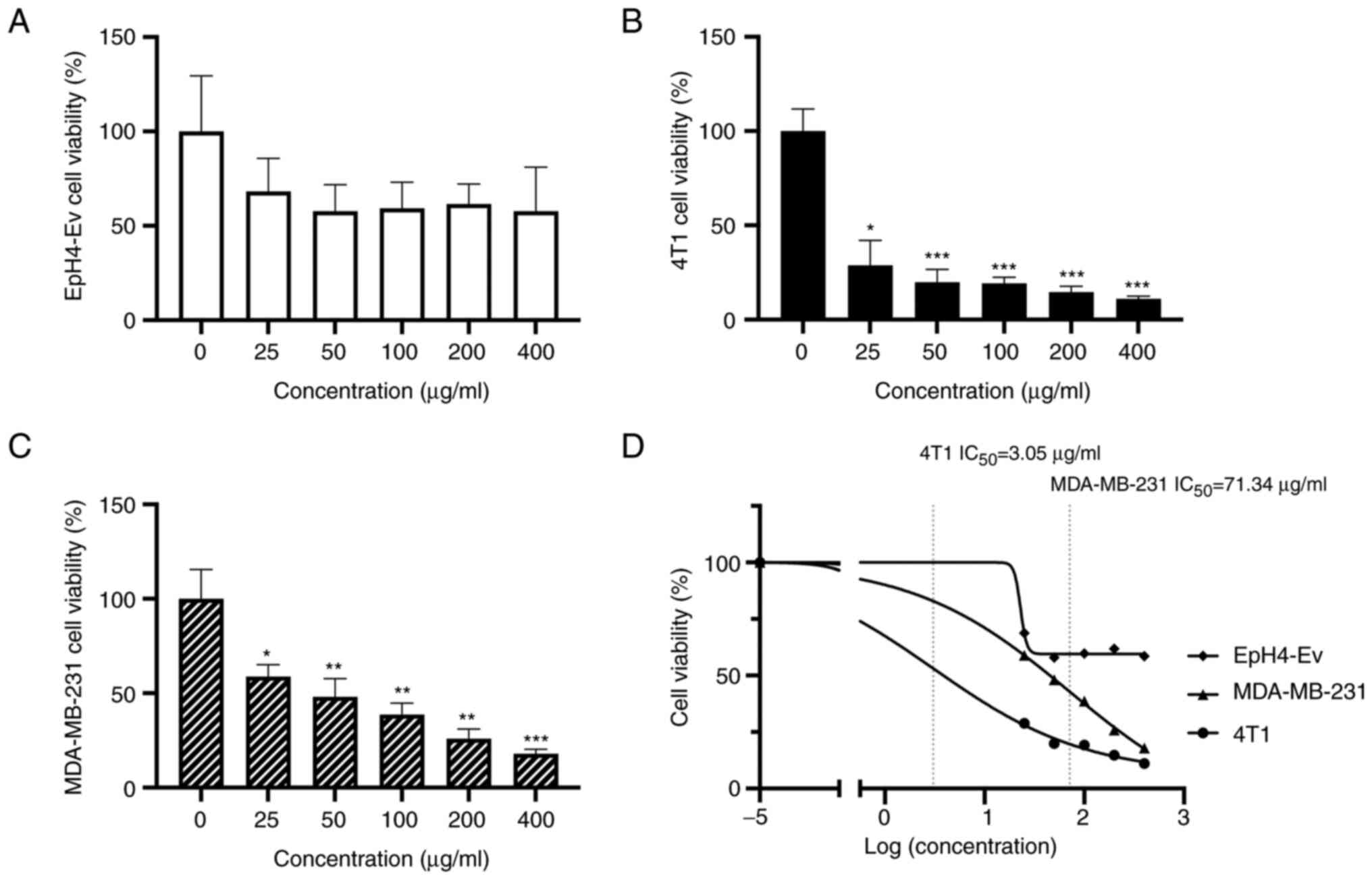
Effects of TTFM extracts on breast
cancer cells
The 4T1 and MDA-MB-231 breast cancer cells and the
EpH4-Ev normal breast cells were treated with TTFM (0-400 µg/ml)
for 5 days. TTFM extracts significantly decreased the viability of
4T1 and MDA-MB-231 cells in a dose-dependent manner; however, no
significant affect was demonstrated for the EpH4-Ev cells (Fig. 1A-C). The IC50 values for
TTFM extracts against 4T1 and MDA-MB-231 cells were 3.05 and 71.34
µg/ml, respectively (Fig. 1D). An
IC50 value for EpH4-Ev was not determined.
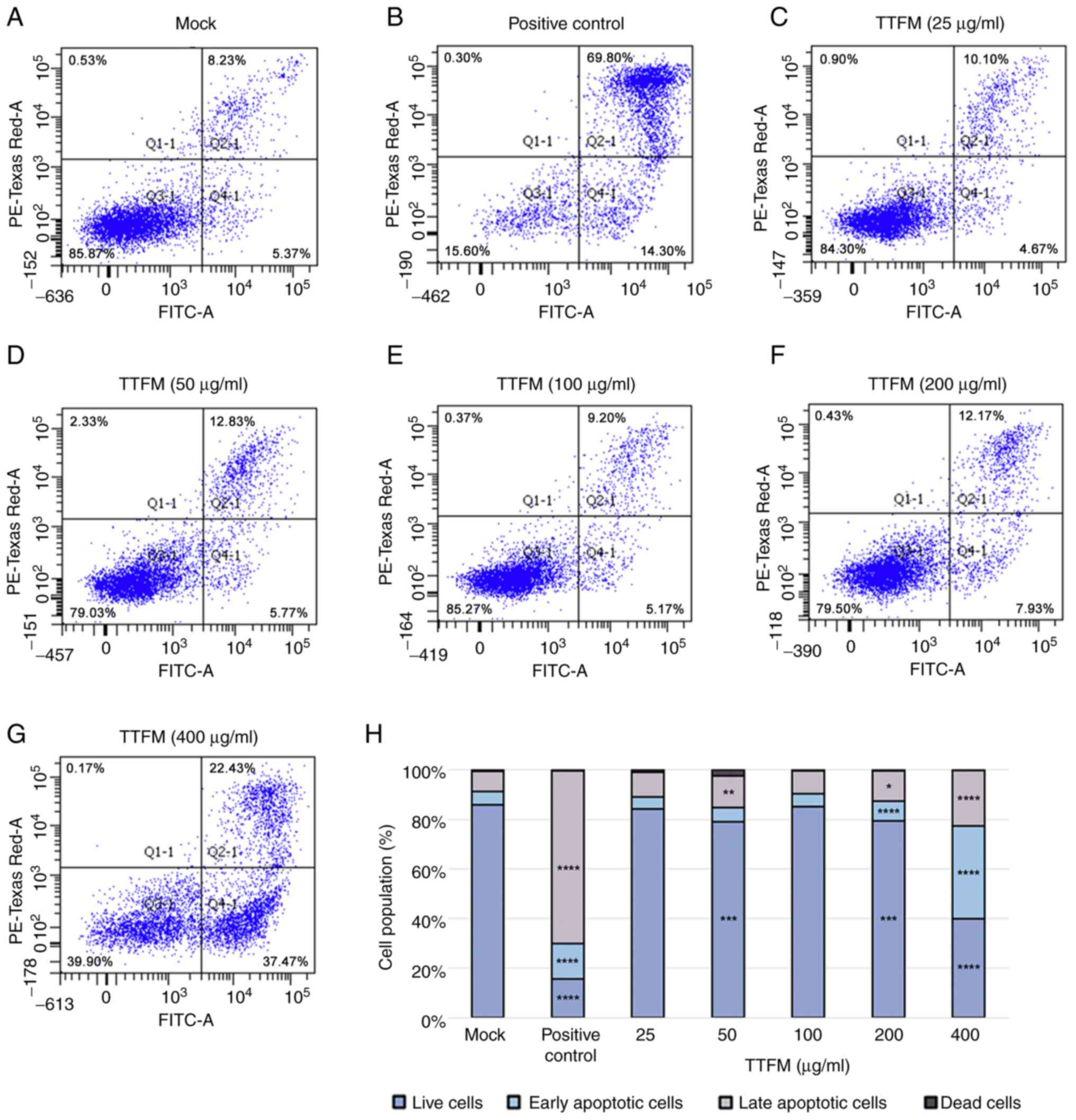
Effects of TTFM extracts on the
apoptotic process
To ensure that there was a sufficient cell
population for use in the apoptotic assay, 4T1 cells were treated
with 0-400 µg/ml of TTFM extracts and incubated for 3 days rather
than 5 days. The mock (negative control) analysis demonstrated that
~86% of the 4T1 cells were alive, with the rest appearing as late
apoptotic cells (8%), early apoptotic cells (5%) and dead cells
(1%) (Fig. 2A and H). The proportion of early and late
apoptotic cells increased by 2.7 and 8.5-fold, respectively, after
the addition of the apoptotic inducer (positive control; 1 mM
H2O2) compared with the mock group. The
apoptotic inducer significantly enhanced the proportion of early
and late apoptotic cells (Fig. 2B
and H); however, the lower TTFM
extract concentrations (25 and 50 µg/ml) only slightly raised the
numbers of late apoptotic cells by about 1 and 1.2-fold when
compared with the mock (Fig. 2C,
D and H). When the treatment concentration was
raised to 200 and 400 µg/ml, the proportion of late apoptotic cells
significantly increased by 1.5 and 2.7-fold, respectively.
Furthermore, the proportion of early apoptotic cells significantly
increased by 6.9 and 2.7-fold, respectively (Fig. 2F-H). Subsequently, studies were
performed to evaluate how TTFM extracts affected the gene
expression profiles of the cells.
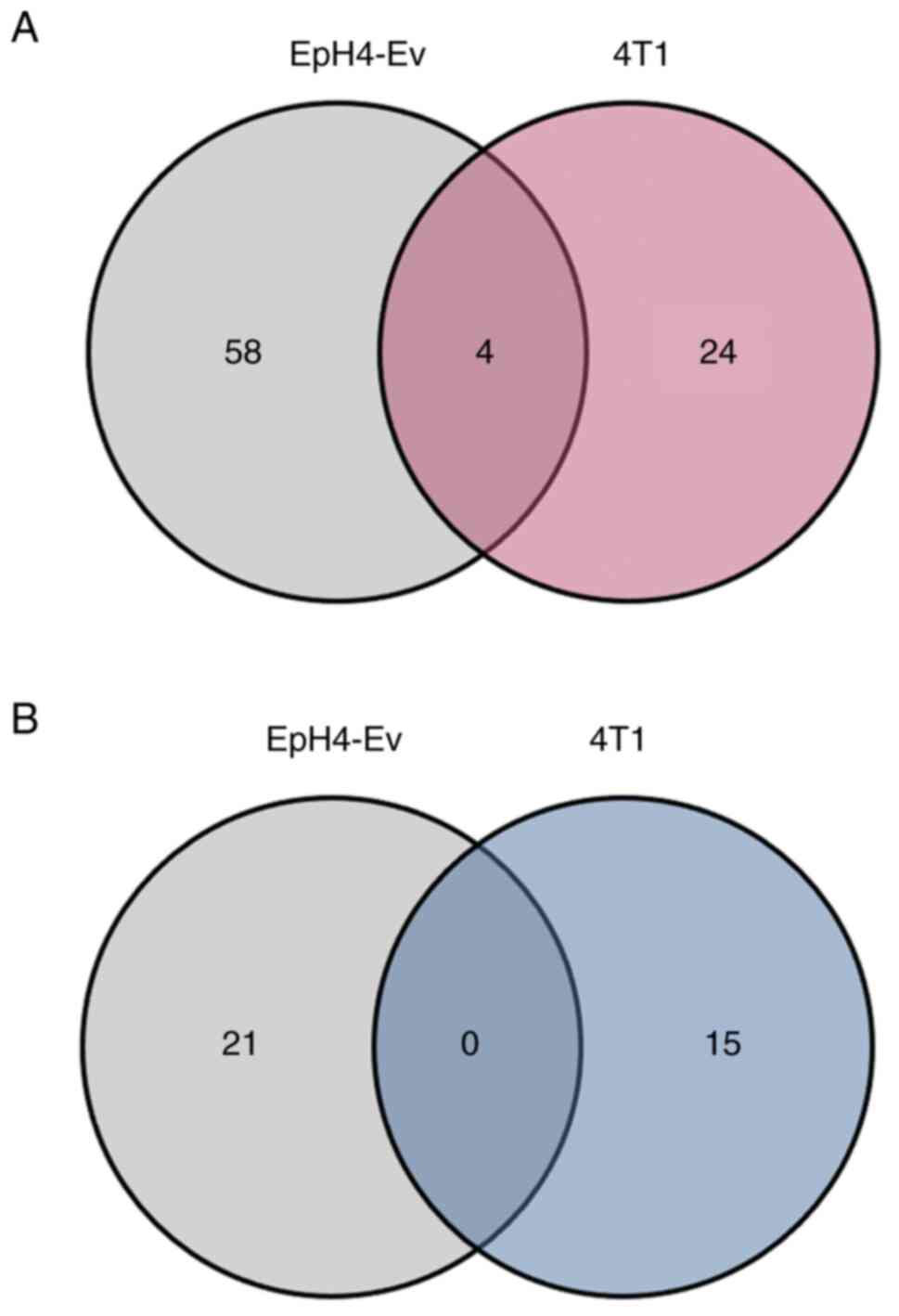
Effects of TTFM extracts on breast
cancer cell pathways and entire mRNA transcripts
To further evaluate the effect of TTFM on gene
expression in breast cancer cells, RNA-seq analysis was performed.
Briefly, cells were exposed to TTFM extracts for 72 h at a final
concentration of 25 µg/ml and the total RNA was collected in
triplicate. A total of 55,359 protein-coding and non-protein coding
genes were identified in both EpH4-Ev and 4T1 cells, respectively.
TTFM treatment resulted in 62 and 28 genes whose expression was
raised in EpH4-Ev and 4T1 cells, respectively, and 21 and 15 genes,
respectively, whose expression was decreased more than twofold with
statistical significance (|log2fold-change|>1,
P<0.05) compared with the corresponding untreated control
(Fig. 3).
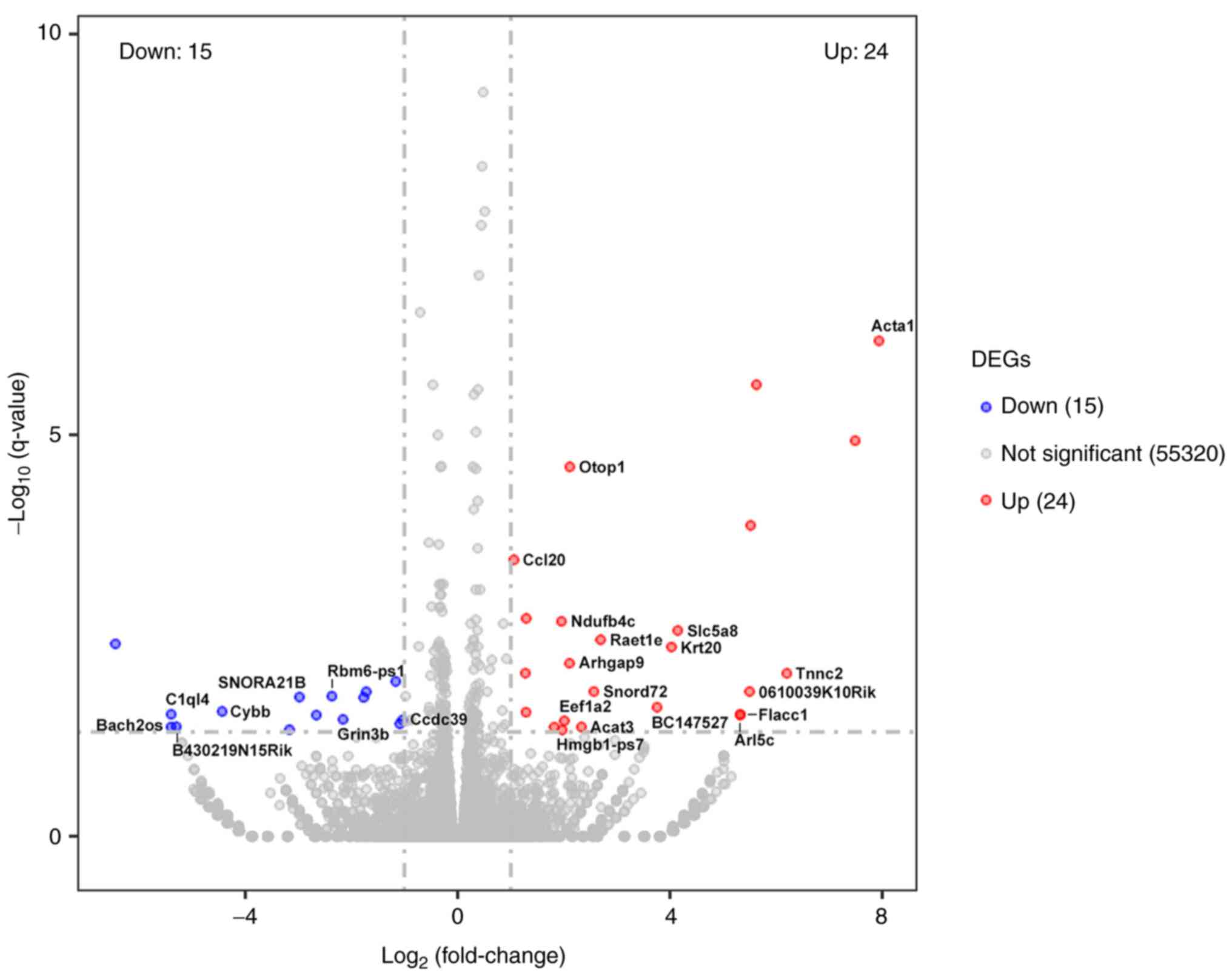
TTFM regulated the mRNA expression levels of 25
known genes in 4T1 breast cancer cells (Fig. 4 and Table SIV). Following treatment with TTFM
extracts, the mRNA expression levels of Acta1, Tnnc2,
0610039K10Rik, Flacc1, Arl5c, Slc5a8,
Krt20, BC147527, Raet1e, Snord72,
Acat3, Otop1, Arhgap9, Eef1a2,
Hmgb1-ps7, Ndufb4c and Ccl20 were
significantly increased. Conversely, the mRNA expression levels of
Ccdc39, Rbm6-ps1, Grin3b, SNORA21B,
Cybb, B430219N15Rik, C1ql4 and Bach2os
were significantly decreased after TTFM treatment. Among those
genes, TTFM treatment significantly increased the expression of
Slc5a8 and Rho Arhgap9, compared with untreated
cells. Adversely, compared to the untreated control group, the TTFM
treatment markedly decreased the expression of Cybb and
Bach2os (Fig. 4 and Table SIV), which had previously been
reported to be involved in cell death. Notably, these significantly
differently expressed genes, were categorized into six major
biological processes based on KEGG pathway enrichment analysis
(Table SV): organismal systems (7
genes), metabolism (2 genes), human diseases (9 genes),
environmental information processing (5 genes), cellular process (1
genes) and genetic information processing (1 gene).
TTFM extracts have different effects
on Slc5a8, Arhgap9, Cybb and apoptosis-related gene expression in
normal breast and breast cancer cell lines
To validate the effects of TTFM on mRNA transcripts,
RT-qPCR was performed. In brief, cells were treated with TTFM
extracts for 72 h at a final concentration of 25 µg/ml, and the
total RNA was collected in triplicate, followed by cDNA synthesis.
The results demonstrated that TTFM treatment significantly enhanced
the mRNA expression levels of Slc5a8 and Arhgap9
genes, and significantly reduced the mRNA expression levels of
Cybb in TTFM-treated 4T1 cells compared with TTFM-treated
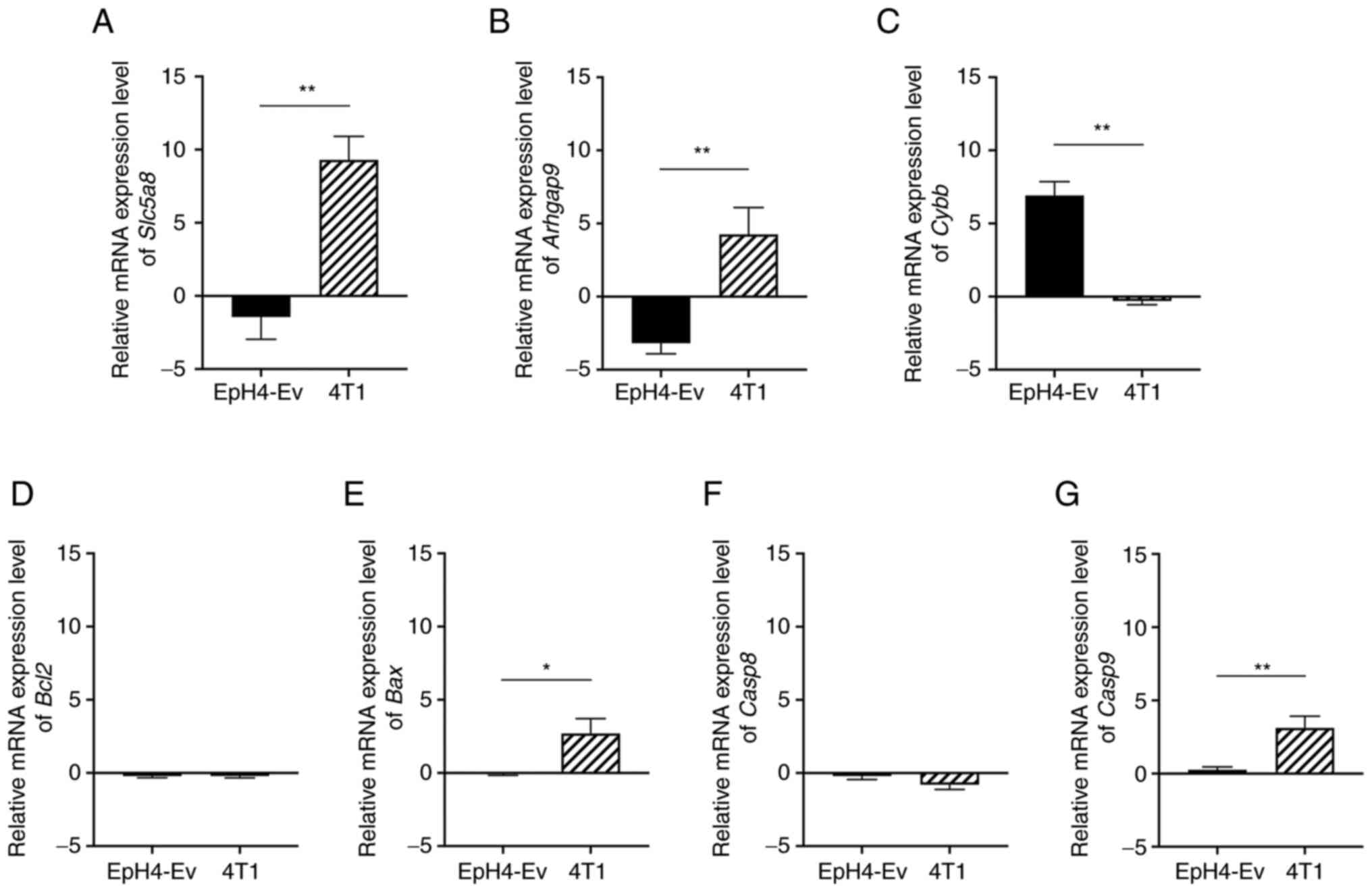
EpH4-Ev cells (Fig. 5A-C).
Moreover, TTFM treatment significantly increased the mRNA
expression levels of Bax and Casp9 in TTFM-treated
4T1 cells compared with TTFM-treated EpH4-Ev cells (Fig. 5D-G).
Discussion
Previous studies have reported that numerous plant
extracts have cytotoxic effects against cancer cells (7,30). The
present study evaluated the effects of TTFM extracts on breast
cancer cell viability using the MTT assay. The results suggested
that TTFM extracts possessed anti-breast cancer activity. These
findings demonstrated that the TTFM extracts had different effects
on cancer cells and normal cells, which could lead to more severe
cytotoxicity in breast cancer cells.
LC-MS/MS analysis demonstrated that TTFM extracts
included numerous secondary metabolites. Some of which have been
previously reported to have anti-cancer properties, including
costunolide (44,45), cyanidin (46,47),
hinokitiol (48,49), oleic acid (50), pentadecanoic acid (51), syringic acid (52), tanshinone I (53) and vinpocetine (54), which have been reported to inhibit
cancer cell growth and proliferation via the induction of
apoptosis. The results of the present study were consistent with
reports from previous studies that certain metabolites found in
medicinal plants might promote apoptosis in breast cancer, possibly
reducing the viability of breast cancer cells (46,51,53).
The compounds betaine (55),
ginkgolide A (56), parecoxib
(57), sinapic acid (58) and tryptanthrin (59). which have been previously reported
to induce cancer cell death by inhibiting cell proliferation and
migration in certain types of cancer, such as colon cancer, ovarian
cancer, pancreatic cancer and breast cancer through different
pathways were also found in TTFM extracts. Furthermore, certain
metabolites such as d-limonene (60), geranic acid (61), l-arginine (62) and pentadecanoic acid (51) have been previously reported to have
demonstrated synergistic effects, enhancing anti-cancer properties
of drugs and compounds. It could be hypothesized that the
synergistic effects from mixtures of several metabolites are
crucial for the anti-breast cancer activity of TTFM extracts.
However, the present study lacks data to support the specific
mechanism of action for specific components in the TTFM extract,
which is a limitation of the present study.
In cancer cells, increased or decreased expression
of certain transcripts has been reported to promote cancer cell
growth. Previous studies reported that the expression of
Slc5a8, a putative tumor suppressor, was repressed in
certain cancers, including breast cancer, through DNA methylation
(63). Up-regulation of
Slc5a8 in cancer cells has been reported to induce apoptosis
when its substrates, which are HDAC inhibitors, are present
(63). The RNA-seq results of the
present study demonstrated that the expression of Slc5a8 was
increased following treatment with TTFM extracts. These findings
were consistent with a previous study that reported that
up-regulation of Slc5a8 in the breast cancer MB231 cell line
prevented cells from forming colonies in vitro and tumors
in vivo (64).
Furthermore, previous studies reported that the MAPK
signaling pathway was regulated by Arhgap9 in breast cancer
(65). High levels of
Arhgap9 expression inhibited activation of the PI3K/AKT/mTOR
signaling pathway, which prevented cell proliferation, invasion and
migration (66). The present study
demonstrated that TTFM extracts treatment also increased
Arhgap9 mRNA expression levels.
Previous studies reported that Cybb was
involved in the immune regulation of tumor metastasis and that the
expression level of Cybb was higher in triple-negative
breast cancer compared with normal tissue (67). In the present study, Cybb
mRNA expression levels were significantly suppressed by TTFM
treatment. Bach2os are oncogenic lncRNAs that might act as
drivers of tumor progression (68).
In the present study, following TTFM extract treatment,
Bach2os was down regulated in the RNA-seq data.
TTFM treatment significantly enhanced Bax and
Casp9 mRNA expression levels in TTFM-treated 4T1 cells
compared with TTFM-treated EpH4-Ev cells. A previous study reported
that increasing the expression of Bax and Caspase-9, two key
regulators of the intrinsic pathway of apoptosis, was necessary for
the induction of apoptosis in cancer cells (51,53,69).
When apoptotic stimuli are present, BAX translocate from the
cytosol to mitochondria, resulting in dimerization, integration and
cytochrome c release, which results in caspase-9 activation and
apoptosis (69). Taken together,
the results demonstrated that TTFM may have caused breast cancer
cells to become cytotoxic by inducing apoptosis. However, the
pathways need to be further elucidated and evaluated to support
this.
In conclusion, the present study demonstrated the
anti-breast cancer activity of TTFM water extracts. The levels of
certain transcripts were altered by TTFM, and this process most
likely caused cell death by inducing apoptosis. However, further
experiments are required to evaluate how the TTFM extracts used
specifically regulate genes and proteins. The TTFM extracts used in
the present study are suggested as a potential for further
development of anti-breast cancer therapeutics.
Supplementary Material
Sequences of primers used for reverse
transcription-quantitative PCR.
Identification of metabolite compound
in TTFM extracts in the negative ion mode.
Identification of metabolite compound
in TTFM extracts in the positive ion mode.
Representative protein-coding genes
significantly affected by Thai traditional formulary medicine in
4T1 cells.
Pathway categorization based on KEGG
pathway enrichment analysis.
Acknowledgements
We would like to thank Assoc. Professor Dr
Wannarasmi Ketchart (Faculty of Medicine, Chulalongkorn University,
Bangkok, Thailand) who kindly provided the MDA-MB-231 cells.
Funding
Funding: The present study was supported by the Thailand Science
Research and Innovation Fund (grant no. CU_FRB640001_01_30_4) and
the Ratchadapiseksompotch Fund (RA-MF-69/64; Faculty of Medicine,
Chulalongkorn University). The study was supported by the 100th
Anniversary Chulalongkorn University Fund for Doctoral
Scholarship.
Availability of data and materials
The RNA-sequencing datasets generated and/or
analyzed during the current study are available in the National
Center for Biotechnology Information (NCBI) Sequence Read Archive
(accession no. SRR18848741-SRR18848746 and
SRR18848748-SRR18848753). The data are also available through the
NCBI GenBank (accession no. PRJNA830310).
All other data used and/or analyzed during the
present study are available from the corresponding authors on
reasonable request.
Authors' contributions
SP and NT devised the study. KC reviewed the TTFM
Atisaravak scripture and selected the TTFM recipe. AK performed the
experiments, analyzed the data and interpreted the results. WJ and
PKa performed the LC-MS/MS. PKl collected and analyzed the data. PC
performed RNA extraction. PS performed data analysis. AK prepared
this manuscript. SP and NT oversaw, revised the final manuscript
and confirm the authenticity of all the raw data. All authors have
read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global Cancer Statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249.
2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Thaineua V, Ansusinha T, Auamkul N,
Taneepanichskul S, Urairoekkun C, Jongvanich J, Kannawat C,
Traisathit P and Chitapanarux I: Impact of regular Breast
Self-Examination on breast cancer size, stage, and mortality in
Thailand. Breast J. 26:822–824. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Ferlay J, Ervik M, Lam F, Colombet M, Mery
L and Piñeros M: Global Cancer Observatory: Cancer Today France:
International Agency for Research on Cancer. Journal.
2021:2020.
|
|
4
|
Kim C and Kim B: Anti-Cancer natural
products and their bioactive compounds inducing ER stress-mediated
apoptosis: A review. Nutrients. 10(1021)2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Chen S, Wang Z, Huang Y, O'Barr SA, Wong
RA, Yeung S and Chow MS: Ginseng and anticancer drug combination to
improve cancer chemotherapy: A critical review. Evid Based
Complement Alternat Med. 2014(168940)2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Demain AL and Vaishnav P: Natural products
for cancer chemotherapy. Microb Biotechnol. 4:687–699.
2011.PubMed/NCBI View Article : Google Scholar
|
|
7
|
McGrowder DA, Miller FG, Nwokocha CR,
Anderson MS, Wilson-Clarke C, Vaz K, Anderson-Jackson L and Brown
J: Medicinal herbs used in traditional management of breast cancer:
Mechanisms of action. Medicines (Basel). 7(47)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Rayan A, Raiyn J and Falah M: Nature is
the best source of anticancer drugs: Indexing natural products for
their anticancer bioactivity. PLoS One. 12(e0187925)2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Abdollahzadeh S, Mashouf R, Mortazavi H,
Moghaddam M, Roozbahani N and Vahedi M: Antibacterial and
antifungal activities of punica granatum peel extracts against oral
pathogens. J Dent (Tehran). 8:1–6. 2011.PubMed/NCBI
|
|
10
|
Hu PY, Zhong YH, Feng JF, Li DX, Deng P,
Zhang WL, Lei ZQ, Liu XM and Zhang GS: Pharmacokinetics of five
phthalides in volatile oil of Ligusticum sinense Oliv.cv. Chaxiong,
and comparison study on physicochemistry and pharmacokinetics after
being formulated into solid dispersion and inclusion compound. BMC
Complement Med Ther. 21(129)2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Wei Q, Yang J, Ren J, Wang A, Ji T and Su
Y: Bioactive phthalides from Ligusticum sinense Oliv cv. Chaxiong.
Fitoterapia. 93:226–232. 2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Wu M, Li T, Chen L, Peng S, Liao W, Bai R,
Zhao X, Yang H, Wu C, Zeng H and Liu Y: Essential oils from Inula
japonica and Angelicae dahuricae enhance sensitivity of MCF-7/ADR
breast cancer cells to doxorubicin via multiple mechanisms. J
Ethnopharmacol. 180:18–27. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Guo W, Liu S, Ju X, Du J, Xu B, Yuan H,
Qin F and Li L: The antitumor effect of hinesol, extract from
Atractylodes lancea (Thunb.) DC. by proliferation, inhibition, and
apoptosis induction via MEK/ERK and NF-κB pathway in non-small cell
lung cancer cell lines A549 and NCI-H1299. J Cell Biochem.
120:18600–18607. 2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Lang SJ, Schmiech M, Hafner S, Paetz C,
Steinborn C, Huber R, Gaafary ME, Werner K, Schmidt CQ, Syrovets T
and Simmet T: Antitumor activity of an Artemisia annua herbal
preparation and identification of active ingredients.
Phytomedicine. 62(152962)2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Basaiyye SS, Kashyap S, Krishnamurthi K
and Sivanesan S: Induction of apoptosis in leukemic cells by the
alkaloid extract of garden cress (Lepidium sativum L.). J Integr
Med. 17:221–228. 2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Khan MA, Chen HC, Tania M and Zhang DZ:
Anticancer activities of Nigella sativa (black cumin). Afr J Tradit
Complement Altern Med. 8 (5 Suppl):S226–S232. 2011.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Korff JM, Menke K, Schwermer M, Falke K,
Schramm A, Längler A and Zuzak TJ: Antitumoral effects of curcumin
(Curcuma longa L.) and thymoquinone (Nigella sativa L.) on
neuroblastoma cell lines. Complement Med Res. 28:164–168.
2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Al-Sheddi ES, Al-Zaid NA, Al-Oqail MM,
Al-Massarani SM, El-Gamal AA and Farshori NN: Evaluation of
cytotoxicity, cell cycle arrest and apoptosis induced by Anethum
graveolens L. essential oil in human hepatocellular carcinoma cell
line. Saudi Pharm J. 27:1053–1060. 2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Yue J, Zhang S, Zheng B, Raza F, Luo Z, Li
X, Zhang Y, Nie Q and Qiu M: Efficacy and mechanism of active
fractions in fruit of amomum villosum lour. for gastric cancer. J
Cancer. 12:5991–5998. 2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Weerapol Y, Manmuan S, Chaothanaphat N,
Okonogi S, Limmatvapirat C, Limmatvapirat S and Tubtimsri S: Impact
of fixed oil on ostwald ripening of anti-oral cancer nanoemulsions
loaded with amomum kravanh essential oil. Pharmaceutics.
14(938)2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Dwivedi V, Shrivastava R, Hussain S,
Ganguly C and Bharadwaj M: Comparative anticancer potential of
clove (Syzygium aromaticum)-an Indian spice-against cancer cell
lines of various anatomical origin. Asian Pac J Cancer Prev.
12:1989–1993. 2011.PubMed/NCBI
|
|
22
|
Naik Bukke A, Nazneen Hadi F, Babu KS and
Shankar PC: In vitro studies data on anticancer activity of
Caesalpinia sappan L. heartwood and leaf extracts on MCF7 and A549
cell lines. Data Brief. 19:868–877. 2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Gao XF, Li QL, Li HL, Zhang HY, Su JY,
Wang B, Liu P and Zhang AQ: Extracts from Curcuma zedoaria inhibit
proliferation of human breast cancer cell MDA-MB-231 in vitro. Evid
Based Complement Alternat Med. 2014(730678)2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Tamborlin L, Sumere BR, de Souza MC,
Pestana NF, Aguiar AC, Eberlin MN, Simabuco FM, Rostagno MA and
Luchessi AD: Characterization of pomegranate peel extracts obtained
using different solvents and their effects on cell cycle and
apoptosis in leukemia cells. Food Sci Nutr. 8:5483–5496.
2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Dikmen M, Ozturk N and Ozturk Y: The
antioxidant potency of Punica granatum L. Fruit peel reduces cell
proliferation and induces apoptosis on breast cancer. J Med Food.
14:1638–1646. 2011.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Shapira N: The potential contribution of
dietary factors to breast cancer prevention. Eur J Cancer Prev.
26:385–395. 2017.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Cao W, Li XQ, Wang X, Fan HT, Zhang XN,
Hou Y, Liu SB and Mei QB: A novel polysaccharide, isolated from
Angelica sinensis (Oliv.) Diels induces the apoptosis of cervical
cancer HeLa cells through an intrinsic apoptotic pathway.
Phytomedicine. 17:598–605. 2010.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Nalini N, Manju V and Menon VP: Effect of
spices on lipid metabolism in 1,2-dimethylhydrazine-induced rat
colon carcinogenesis. J Med Food. 9:237–245. 2006.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Lee TK, Lee D, Lee SR, Ko YJ, Sung Kang K,
Chung SJ and Kim KH: Sesquiterpenes from Curcuma zedoaria rhizomes
and their cytotoxicity against human gastric cancer AGS cells.
Bioorg Chem. 87:117–122. 2019.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Kapinova A, Kubatka P, Golubnitschaja O,
Kello M, Zubor P, Solar P and Pec M: Dietary phytochemicals in
breast cancer research: Anticancer effects and potential utility
for effective chemoprevention. Environ Health Prev Med.
23(36)2018.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Ekor M: The growing use of herbal
medicines: Issues relating to adverse reactions and challenges in
monitoring safety. Front Pharmacol. 4(177)2014.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Tsugawa H, Cajka T, Kind T, Ma Y, Higgins
B, Ikeda K, Kanazawa M, VanderGheynst J, Fiehn O and Arita M:
MS-DIAL: Data-independent MS/MS deconvolution for comprehensive
metabolome analysis. Nat Methods. 12:523–526. 2015.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Jevapatarakul D, T-Thienprasert J,
Payungporn S, Chavalit T, Khamwut A and T-Thienprasert NP:
Utilization of Cratoxylum formosum crude extract for synthesis of
ZnO nanosheets: Characterization, biological activities and effects
on gene expression of nonmelanoma skin cancer cell. Biomed
Pharmacother. 130(110552)2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Kim D, Langmead B and Salzberg SL: HISAT:
A fast spliced aligner with low memory requirements. Nat Methods.
12:357–360. 2015.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Trapnell C, Williams BA, Pertea G,
Mortazavi A, Kwan G, van Baren MJ, Salzberg SL, Wold BJ and Pachter
L: Transcript assembly and quantification by RNA-Seq reveals
unannotated transcripts and isoform switching during cell
differentiation. Nat Biotechnol. 28:511–515. 2010.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Love MI, Huber W and Anders S: Moderated
estimation of fold change and dispersion for RNA-seq data with
DESeq2. Genome Biol. 15(550)2014.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Young MD, Wakefield MJ, Smyth GK and
Oshlack A: Gene ontology analysis for RNA-seq: Accounting for
selection bias. Genome Biol. 11(R14)2010.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Kanehisa M, Araki M, Goto S, Hattori M,
Hirakawa M, Itoh M, Katayama T, Kawashima S, Okuda S, Tokimatsu T
and Yamanishi Y: KEGG for linking genomes to life and the
environment. Nucleic Acids Res. 36(Database issue):D480–D484.
2008.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408.
2001.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Gong H, Sun L, Chen B, Han Y, Pang J, Wu
W, Qi R and Zhang TM: Evaluation of candidate reference genes for
RT-qPCR studies in three metabolism related tissues of mice after
caloric restriction. Sci Rep. 6(38513)2016.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Daneshforouz A, Nazemi S, Gholami O,
Kafami M and Amin B: The cytotoxicity and apoptotic effects of
verbascoside on breast cancer 4T1 cell line. BMC Pharmacol Toxicol.
22(72)2021.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Chi W, Li F, Chen H, Wang Y, Zhu Y, Yang
X, Zhu J, Wu F, Ouyang H, Ge J, et al: Caspase-8 promotes
NLRP1/NLRP3 inflammasome activation and IL-1β production in acute
glaucoma. Proc Natl Acad Sci USA. 111:11181–11186. 2014.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Xu W, Guo G, Li J, Ding Z, Sheng J, Li J
and Tan W: Activation of Bcl-2-Caspase-9 apoptosis pathway in the
testis of asthmatic mice. PLoS One. 11(e0149353)2016.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Lee SH, Cho YC and Lim JS: Costunolide, a
sesquiterpene lactone, suppresses skin cancer via induction of
apoptosis and blockage of cell proliferation. Int J Mol Sci.
22(2075)2021.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Huang H, Yi J, Park S, Zhang H, Kim E,
Park S, Kwon W, Jang S, Zhang X, Chen H, et al: Costunolide
suppresses melanoma growth via the AKT/mTOR pathway in vitro and in
vivo. Am J Cancer Res. 11:1410–1427. 2021.PubMed/NCBI
|
|
46
|
Cho E, Chung EY, Jang HY, Hong OY, Chae
HS, Jeong YJ, Kim SY, Kim BS, Yoo DJ, Kim JS and Park KH:
Anti-cancer Effect of Cyanidin-3-glucoside from Mulberry via
Caspase-3 Cleavage and DNA Fragmentation in vitro and in vivo.
Anticancer Agents Med Chem. 17:1519–1525. 2017.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Liang L, Liu X, He J, Shao Y, Liu J, Wang
Z, Xia L, Han T and Wu P: Cyanidin-3-glucoside induces mesenchymal
to epithelial transition via activating Sirt1 expression in triple
negative breast cancer cells. Biochimie. 162:107–115.
2019.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Chen HY, Cheng WP, Chiang YF, Hong YH, Ali
M, Huang TC, Wang KL, Shieh TM, Chang HY and Hsia SM: Hinokitiol
exhibits antitumor properties through induction of ROS-Mediated
apoptosis and p53-Driven cell-cycle arrest in endometrial cancer
cell lines (Ishikawa, HEC-1A, KLE). Int J Mol Sci.
22(8268)2021.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Wu YJ, Hsu WJ, Wu LH, Liou HP, Pangilinan
CR, Tyan YC and Lee CH: Hinokitiol reduces tumor metastasis by
inhibiting heparanase via extracellular signal-regulated kinase and
protein kinase B pathway. Int J Med Sci. 17:403–413.
2020.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Yamagata K, Uzu E, Yoshigai Y, Kato C and
Tagami M: Oleic acid and oleoylethanolamide decrease
interferon-ү-induced expression of PD-L1 and induce apoptosis in
human lung carcinoma cells. Eur J Pharmacol.
903(174116)2021.PubMed/NCBI View Article : Google Scholar
|
|
51
|
To NB, Nguyen YT, Moon JY, Ediriweera MK
and Cho SK: Pentadecanoic acid, an odd-chain fatty acid, suppresses
the stemness of MCF-7/SC human breast cancer stem-like cells
through JAK2/STAT3 signaling. Nutrients. 12(1663)2020.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Pei J, Velu P, Zareian M, Feng Z and
Vijayalakshmi A: Effects of syringic acid on apoptosis,
inflammation, and AKT/mTOR signaling pathway in gastric cancer
cells. Front Nutr. 8(788929)2021.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Nizamutdinova IT, Lee GW, Son KH, Jeon SJ,
Kang SS, Kim YS, Lee JH, Seo HG, Chang KC and Kim HJ: Tanshinone I
effectively induces apoptosis in estrogen receptor-positive (MCF-7)
and estrogen receptor-negative (MDA-MB-231) breast cancer cells.
Int J Oncol. 33:485–491. 2008.PubMed/NCBI
|
|
54
|
Huang EW, Xue SJ, Zhang Z, Zhou JG, Guan
YY and Tang YB: Vinpocetine inhibits breast cancer cells growth in
vitro and in vivo. Apoptosis. 17:1120–1130. 2012.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Kim DH, Sung B, Chung HY and Kim ND:
Modulation of Colitis-associated colon tumorigenesis by baicalein
and betaine. J Cancer Prev. 19:153–160. 2014.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Ye B, Aponte M, Dai Y, Li L, Ho MC,
Vitonis A, Edwards D, Huang TN and Cramer DW: Ginkgo biloba and
ovarian cancer prevention: Epidemiological and biological evidence.
Cancer Lett. 251:43–52. 2007.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Wong CH, Chang WL, Lu FJ, Liu YW, Peng JY
and Chen CH: Parecoxib expresses anti-metastasis effect through
inhibition of epithelial-mesenchymal transition and the
Wnt/β-catenin signaling pathway in human colon cancer DLD-1 cell
line. Environ Toxicol. 37:2718–2727. 2022.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Huang Z, Chen H, Tan P, Huang M, Shi H,
Sun B, Cheng Y, Li T, Mou Z, Li Q and Fu W: Sinapic acid inhibits
pancreatic cancer proliferation, migration, and invasion via
downregulation of the AKT/Gsk-3β signal pathway. Drug Dev Res.
83:721–734. 2022.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Zeng Q, Luo C, Cho J, Lai D, Shen X, Zhang
X and Zhou W: Tryptanthrin exerts anti-breast cancer effects both
in vitro and in vivo through modulating the inflammatory tumor
microenvironment. Acta Pharm. 71:245–266. 2021.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Yu X, Lin H, Wang Y, Lv W, Zhang S, Qian
Y, Deng X, Feng N, Yu H and Qian B: d-limonene exhibits antitumor
activity by inducing autophagy and apoptosis in lung cancer. Onco
Targets Ther. 11:1833–1847. 2018.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Ramasamy S, Abdul Wahab N, Zainal Abidin
N, Manickam S and Zakaria Z: Growth inhibition of human gynecologic
and colon cancer cells by Phyllanthus watsonii through apoptosis
induction. PLoS One. 7(e34793)2012.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Cao Y, Wang Q, Du Y, Liu F, Zhang Y, Feng
Y and Jin F: l-arginine and docetaxel synergistically enhance
anti-tumor immunity by modifying the immune status of tumor-bearing
mice. Int Immunopharmacol. 35:7–14. 2016.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Ganapathy V, Gopal E, Miyauchi S and
Prasad PD: Biological functions of SLC5A8, a candidate tumour
suppressor. Biochem Soc Trans. 33(Pt 1):237–240. 2005.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Coothankandaswamy V, Elangovan S, Singh N,
Prasad PD, Thangaraju M and Ganapathy V: The plasma membrane
transporter SLC5A8 suppresses tumour progression through depletion
of survivin without involving its transport function. Biochem J.
450:169–178. 2013.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Piao XM, Jeong P, Yan C, Kim YH, Byun YJ,
Xu Y, Kang HW, Seo SP, Kim WT, Lee JY, et al: A novel tumor
suppressing gene, ARHGAP9, is an independent prognostic biomarker
for bladder cancer. Oncol Lett. 19:476–486. 2020.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Sun J, Zhao X, Jiang H, Yang T, Li D, Yang
X, Jia A, Ma Y and Qian Z: ARHGAP9 inhibits colorectal cancer cell
proliferation, invasion and EMT via targeting PI3K/AKT/mTOR
signaling pathway. Tissue Cell. 77(101817)2022.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Liu Z, Li M, Jiang Z and Wang X: A
Comprehensive immunologic portrait of triple-negative breast
cancer. Transl Oncol. 11:311–329. 2018.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Diermeier SD, Chang KC, Freier SM, Song J,
El Demerdash O, Krasnitz A, Rigo F, Bennett CF and Spector DL:
Mammary tumor-associated RNAs impact tumor cell proliferation,
invasion, and migration. Cell Rep. 17:261–274. 2016.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Ichim G and Tait SW: A fate worse than
death: Apoptosis as an oncogenic process. Nat Rev Cancer.
16:539–548. 2016.PubMed/NCBI View Article : Google Scholar
|