Introduction
Postherpetic neuralgia (PHN) is a common type of
neuropathic pain that persists for >3 months after a rash heals
from acute herpes zoster (HZ) (1,2). PHN
typically manifests as spontaneous pain, hyperalgesia and allodynia
that last for several months or even a lifetime and seriously
affects the physical and mental health of patients (3). PHN is the most common complication of
HZ that mainly affects patients >50 years of age (4), and its incidence increases with
age.
PHN is difficult to treat and pharmacological
therapy is currently the primary treatment for PHN (5). Pregabalin, gabapentin and tricyclic
antidepressants are first-line therapeutic drugs recommended for
PHN (6). Since long-term medication
is needed, adverse effects such as dizziness, drowsiness, dry mouth
and edema are often observed in patients with PHN. Opioids,
including tramadol, morphine and oxycodone, should generally be
considered for PHN with severe pain after consultation with a
specialist, and should only be prescribed with appropriate goals
followed by close monitoring (2).
However, these Western medical practices have only achieved mild
successes in pain alleviation. Numerous patients with PHN still
respond poorly to pharmacological treatments such as gabapentinoids
(7). Therefore, an effective and
safe therapy for PHN is urgently needed.
Studies have found that bloodletting puncture and
cupping (BLP-C) may effectively reduce pain in patients with PHN
with fewer or no adverse effects on physical health. BLP-C is a
Traditional Chinese Medicine (TCM) treatment modality based on the
meridian theory, which has an important role in the field of
complementary and alternative medicine. BLP stimulates the
acupoints on the patient's body to promote blood circulation,
remove blood stasis and dredge the meridians, thereby relieving
pain. Cupping uses the heat of combustion to achieve suction
(negative pressure) inside a glass cup, which is then applied to
specific parts of the body. This suction induces congestion or
hemostasis at selected acupoints (8), resulting in therapeutic effects such
as promoting skin blood flow (9),
increasing the pain threshold, improving local anaerobic metabolism
(10), attenuating inflammation and
regulating cellular immune responses (11). In clinical practice, BLP-C has been
found to be moderately effective in the management of PHN. However,
there is currently no comprehensive systematic review and
meta-analysis that quantitatively assessed the efficacy of BLP-C in
the treatment of PHN. Therefore, the present meta-analysis aimed to
assess the efficacy and safety of BLP-C in PHN patients by
performing a data synthesis from randomized-controlled trials
(RCTs) and to provide a reliable reference for clinical
decision-making.
Materials and methods
Registration
The protocol of this review has been registered in
PROSPERO (https://www.crd.york.ac.uk/PROSPERO/) on October 24th,
2022 (no. CRD42022367056).
Search strategies
Relevant RCTs were searched in the China National
Knowledge Infrastructure (CNKI; https://www.cnki.net), Wanfang (www.wanfangpaper.net), CQVIP (http://www.cqvip.com), SinoMed (http://www.sinomed.ac.cn), Cochrane Library
(https://www.cochranelibrary.com/?contentLanguage=eng),
PubMed (https://pubmed.ncbi.nlm.nih.gov), Web of Science
(https://www.webofscience.com/wos) and
Embase (https://www.embase.com) databases from
inception to September 2022 without any language restrictions. The
title, abstract and full text of the studies were reviewed and
screened independently by two investigators (WK and YL) to
determine eligibility for inclusion in the meta-analysis. Any
disagreement was resolved by a third investigator (CX).
The relevant studies were searched using subject and
entry terms. Chinese databases were searched using Chinese
(Mandarin) search terms ‘Ci Luo Ba Guan’ (BLP-C) and ‘Dai Zhuang
Pao Zhen Hou Yi Shen Jing Tong/Dai Zhuang Pao Zhen Hou Yi Liu Shen
Jing Tong’ (PHN). English databases were searched by the English
search terms ‘acupuncture’, ‘blood-letting’, ‘pricking’, ‘cupping’,
‘postherpetic neuralgia’ and ‘PHN’. The search strategy for PubMed
is outlined in Table SI.
Eligibility criteria
The inclusion criteria for the present study were as
follows: i) Participants: Patients medically diagnosed with PHN,
regardless of ethnicity, nationality or course of the disease; ii)
interventions and controls: Intervention in the treatment group
included BLP-C therapy or BLP-C combined with other TCM therapies.
Intervention in the control group was conventional Western medicine
therapy; iii) outcomes: Overall efficacy [efficacy=(cured +
markedly improved + improved)/total number of cases in each group
x100%], visual analogue scale (VAS) score (12) and Pittsburgh sleep quality index
(PSQI) (13); iv) study type: RCT.
The exclusion criteria for this study were as follows: i)
Participants: Patients diagnosed with a special type of HZ, such as
HZ ophthalmicus, HZ sacralis or incomplete HZ; ii) study type:
Studies that did not describe outcome measures in detail or had an
inaccessible full text.
Literature screening and data
extraction
Literature screening and data extraction were
performed independently by two investigators (WK and YL). Any
disagreement was resolved by a third investigator (XC). Data were
extracted according to a pre-designed Excel 2019 data extraction
form, including basic literature information, study type, basic
subject information, interventions for the treatment group and
control group, intervention time, outcome measures, safety
evaluation and other observational measures.
Quality assessment
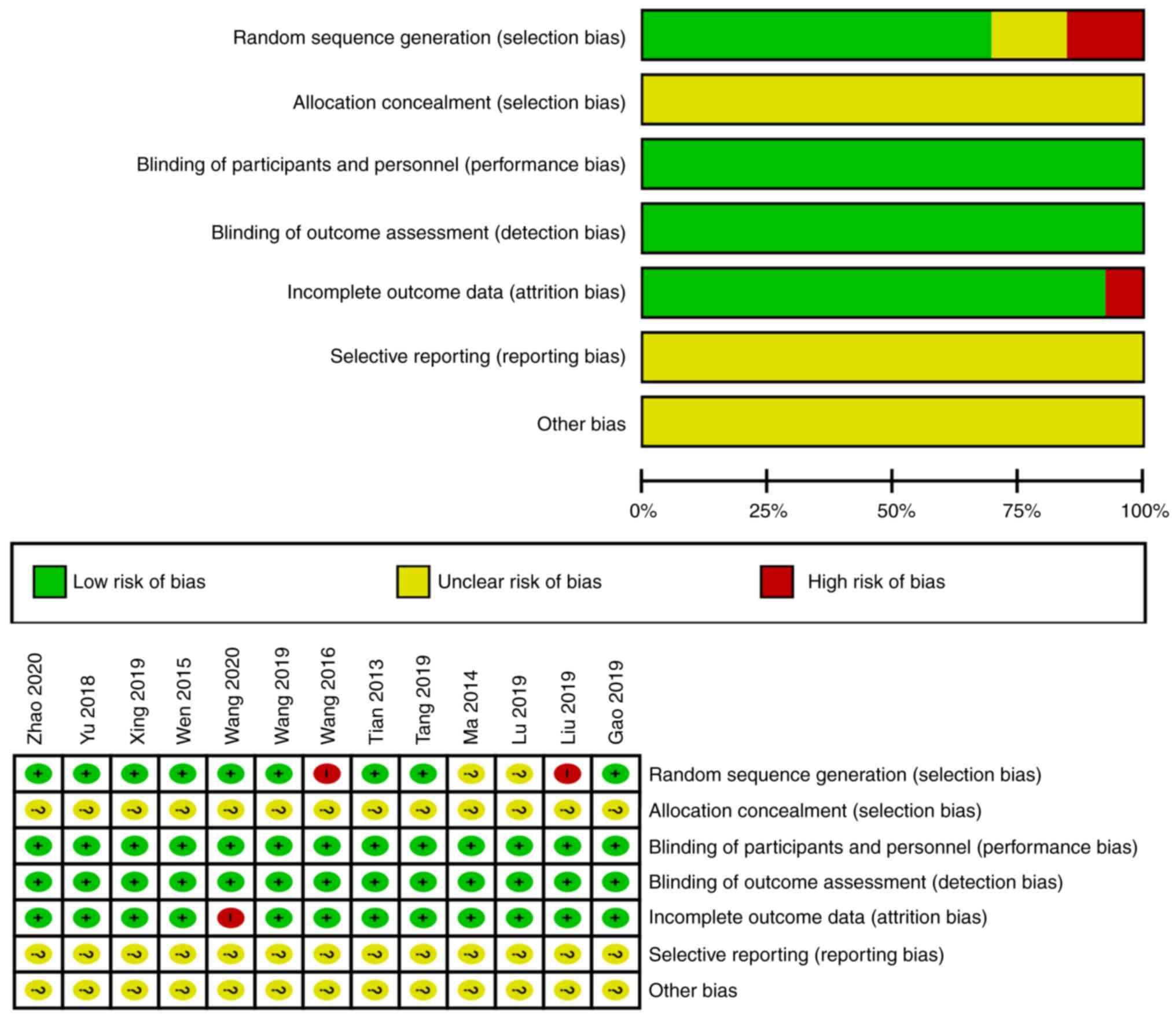
The quality of the articles was assessed
independently by two investigators (WK and YL) using the Cochrane
risk of bias (RoB) tool (methods.cochrane.org). The RoB tool assesses risk of
bias in 7 domains, namely sequence generation, allocation
concealment, blinding of participants and personnel, blinding of
outcome evaluation, incomplete outcome data, selective reporting
and other biases. The possible answers for each domain are Yes (+);
Not clear (?) and No (-). Yes (+) indicates a low risk of bias for
the respective domain; Not clear (?) indicates an unclear or
uncertain risk of bias for the respective domain; No (-) indicates
a high risk of bias for the respective domain.
Data synthesis and statistical
analysis
The collected data were processed and analyzed by
RevMan 5.4 (Cochrane Collaboration) and StataSE15 (StataCorp LP).
Dichotomous and continuous variables were pooled using the risk
ratio (RR) and weighted mean difference (WMD), respectively.
Heterogeneity was evaluated using the I2 statistic and
was considered absent when P>0.1 and I2≤50%. The
meta-analysis was conducted using a fixed-effects or random-effects
model and the presence of bias among studies for different
interventions was judged using a funnel plot. A fixed-effects model
was used when the studies were assumed to be homogeneous, while a
random-effects model was used when there was heterogeneity among
the studies.
Results
Literature search
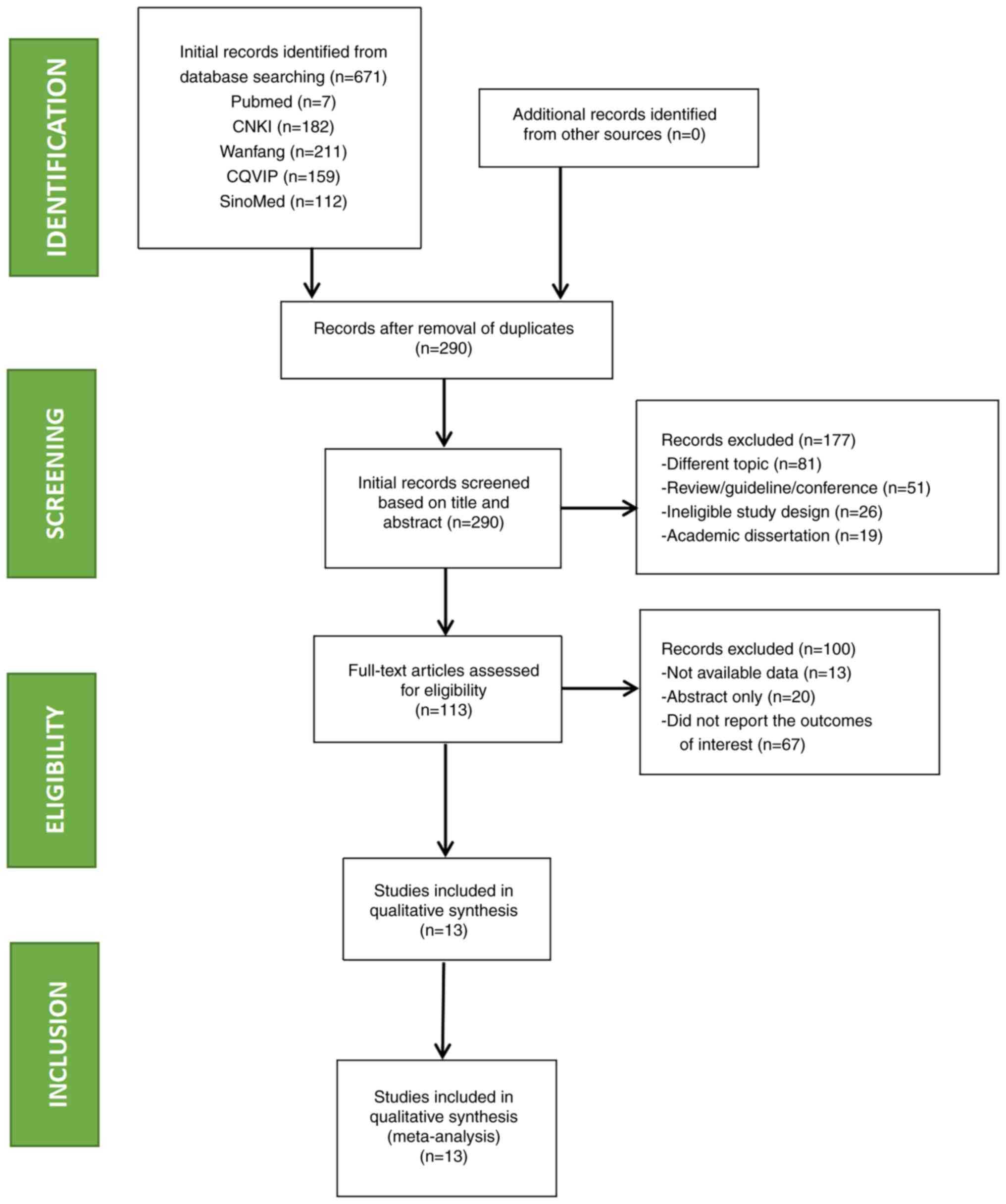
A total of 671 records were initially identified
through database searching, of which 381 were duplicates. After a
preliminary review of titles and abstracts, 177 records were
excluded for not meeting the inclusion criteria. Of the remaining
113 records, 67 were excluded due to the lack of outcomes of
interest, 13 were excluded due to no available data and 20 were
excluded due to abstract-only access. Finally, a total of 13 RCTs
involving 1,129 patients with PHN were included (14-26).
The process of study search and selection is illustrated in
Fig. 1.
Characteristics of included
studies
A total of 13 RCTs were included in the present
review (14-26),
all of which were conducted in China and published in Chinese.
Basic information on the included RCTs is provided in Table I.
 | Table IBasic characteristics of included
studies. |
Table I
Basic characteristics of included
studies.
| Author, year | Number of cases
(Exp/Ctr) | Age, years
(Exp/Ctr) | Duration of
disease, months (Exp/Ctr) | Intervention
(Exp/Ctr) | Course of
treatment, days | Operating
point | Outcome
indicators | (Refs.) |
|---|
| Gao, 2019 | 30/30 |
71.78±7.53/73.16±7.34 |
20.04±1.68/13.56±15.00 |
PC+A+TCM/Carbamazepine | 14 | Ashi Xue | ①②④⑦ | (14) |
| Liu, 2019 | 40/40 |
50.25±10.17/50.18±10.38 | / | PC/Pregabalin | 30 | Ashi Xue | ①②③ | (15) |
| Lu, 2019 | 30/30 |
66.50±2.69/69.90±2.52 |
9.38±2.87/10.16±2.38 |
PC+A/Pregabalin | 10 | Ashi Xue | ①②③④ | (16) |
| Ma, 2014 | 68/68 |
56.4±0.00/51.3±0.00 | / | PC+A+TCM/VitB1 | 30 | Ashi Xue | ①②③⑤ | (17) |
| Tang, 2019 | 30/30 |
59.5±10.30/61.67±8.20 | / |
PC+A/Pregabalin | 14 | Ashi Xue | ①②③⑥ | (18) |
| Tian, 2013 | 32/32 | 61.00/61.00 | 4.00/4.00 | PC/Pregabalin | 16 | Ashi Xue | ③⑧ | (19) |
| Wang, 2016 | 49/40 |
58.26±2.16/57.26±2.21 |
4.02±0.43/4.00±0.44 |
PC+TCM/Ibuprofen | 84 | Ashi Xue | ①②③⑤ | (20) |
| Wang, 2019 | 39/39 |
58.30±3.20/59.10±2.80 |
4.20±1.30/4.00±1.40 |
PC+A/Pregabalin | 10 | Ashi Xue | ①②③④ | (21) |
| Wang, 2020 | 35/35 | 58.60/57.80 |
2.09±0.34/2.06±0.32 | PC/Gabapentin | 16 | Ashi Xue | ①②③⑦⑧ | (22) |
| Wen, 2015 | 25/25 |
45.00±20.00/45.00±21.00 | / | PC+A/Carbamazepine,
Mecobalamin, VitB1 | 14 | Ashi Xue | ①②③⑥ | (23) |
| Xing, 2019 | 36/36 |
68.25±7.42/67.94±6.39 |
3.23±1.05/3.47±0.74 |
PC+A/Gabapentin | 22 | Ashi Xue | ①②③ | (24) |
| Yu, 2018 | 115/115 |
42.41±5.19/43.26±5.28 |
7.98±2.27/7.94±2.30 |
PC+A+TCM/Paracetamol, Codeine | 12 | Ashi Xue | ①②③⑤ | (25) |
| Zhao, 2013 | 42/38 |
54.26±0.00/51.72±0.00 |
6.12±0.00/6.28±0.00 |
PC+TCM/Carbamazepine | 21 | Ashi Xue | ①②③⑤ | (26) |
Participants. The 13 RCTs (14-26)
involved 1,129 patients with PHN, including 574 males and 555
females. Except for the 4 patients who dropped out from one study
(22), all remaining patients were
included in the statistical analysis.
Interventions in the treatment group. As
indicated in Table I, among the 13
included RCTs (14-26),
BLP-C was the intervention in three studies (15,19,22),
BLP-C combined with acupuncture was used in five studies (16,18,21,23,24),
BLP-C combined with TCM was used in two studies (20,26)
and BLP-C combined with acupuncture and TCM were used in three
studies (14,17,25).
The specific characteristics of the included BLP-C
studies are listed in Table I. In
all of the 13 studies included, Ashi Xue had been selected as the
puncture site for BLP-C (14-26).
Interventions in the control group. Western
medicine was used as the intervention for the control group.
Pregabalin was used in five studies (15,16,16,19,21),
carbamazepine was used in two studies (14,26),
gabapentin was used in two studies (22,24)
and ibuprofen was used in one study (20). In the other three studies (17,20,25),
different combinations of two or three Western medicines
(acetaminophen, codeine, mecobalamin, vitamin B1, Fenbid and
carbamazepine) were used. The duration of intervention in the
control group was the same as that in the treatment group.
Efficacy assessment. The overall efficacy was
reported in 12 of the 13 eligible studies (14-26),
the VAS score was reported by 12 studies (15-26),
the PSQI was reported by 3 studies (14,16,21),
the incidence of adverse reactions was reported by 4 studies
(17,20,25,26)
and the recurrence rate was reported by 2 studies (18,23).
In addition, serum levels of pain-related factors, namely substance
P and IL-6, were reported by two studies (19,22).
Quality assessment of included
studies
Among the 13 included studies, the random sequence
generation method was used in 11 studies (14,15,18-26),
the random number table method was adopted in nine studies
(14,18,19,21-26),
random grouping was conducted according to the visit time in one
study (20), random grouping was
conducted according to the admission time in one study (15), and the term ‘random’ was mentioned
in the remaining two studies (16,17)
without describing the random grouping method. BLP-C was used as
the intervention in these studies. Allocation concealment and
blinding are not feasible for BLP-C because the traces left by the
procedure are usually visible and may last for several days.
Therefore, it is difficult to carry out the masking process and
impossible to use any blinding methods. However, the patients
showed good compliance and the non-blinding method was unlikely to
affect the results. Follow-up at three months (18) and one year (23) were respectively mentioned in two
studies (18,23) and the recurrence rate was
statistically analyzed. One study (22) reported four cases of dropout and
provided explanations. The outcome data were complete in the other
12 studies (14-21,23-26)
and no dropout cases were reported. Baseline characteristics were
comparable among the 13 studies (14-26),
but selective reporting and other bias were unclear. The quality
assessment results of the 13 studies (14-26)
are summarized in Fig. 2.
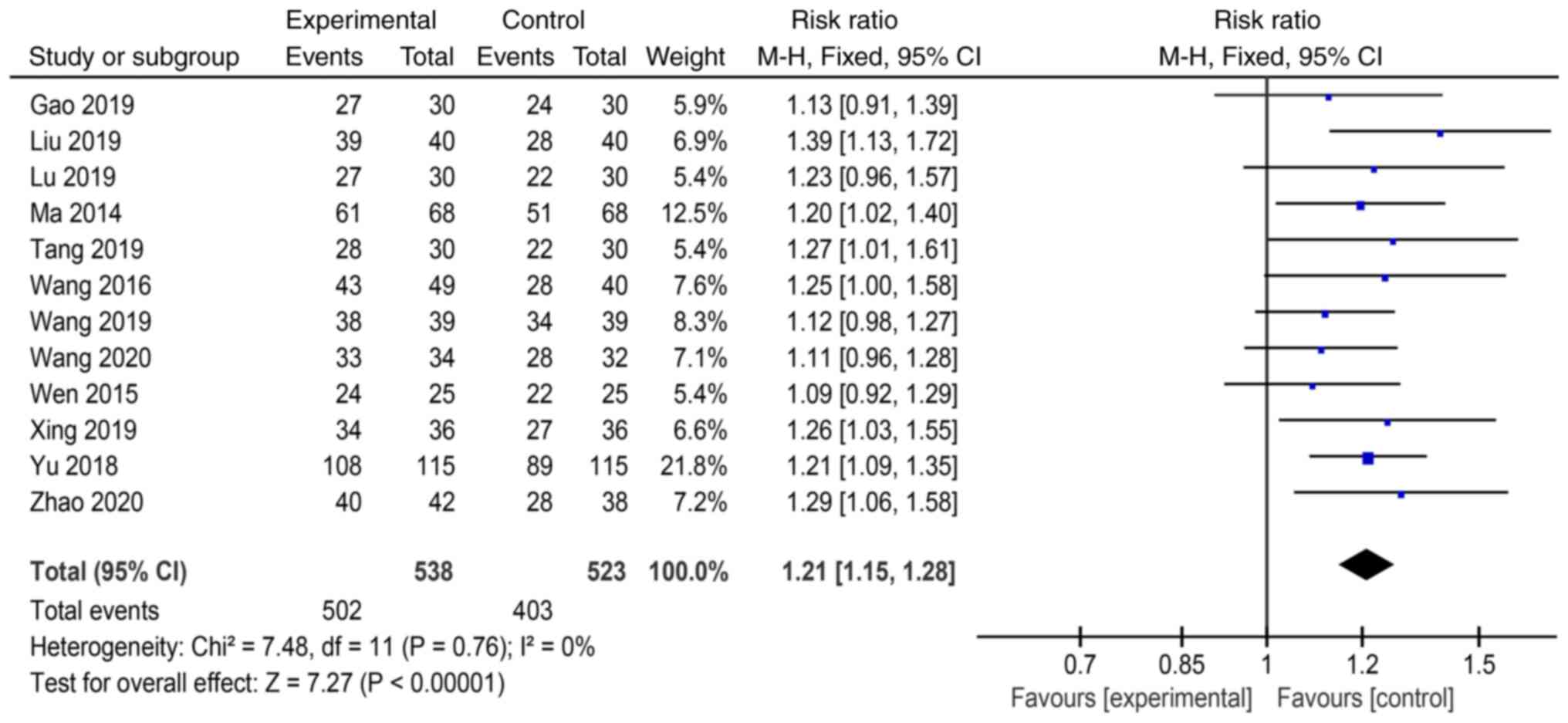
Meta-analysis. Overall efficacy
The overall treatment efficacy in the experimental
and control groups was reported in 12 studies. There were 1,061
patients, including 538 in the experimental group and 523 in the
control group. Heterogeneity was low among the studies (P=0.76,
I2=0%). The results showed that the overall efficacy was
significantly higher in the experimental group (including BLP-C
alone and BLP-C + acupuncture or TCM) than in the control group
(drug treatments) [RR=1.21, 95% CI: 1.15-1.28, P<0.00001]
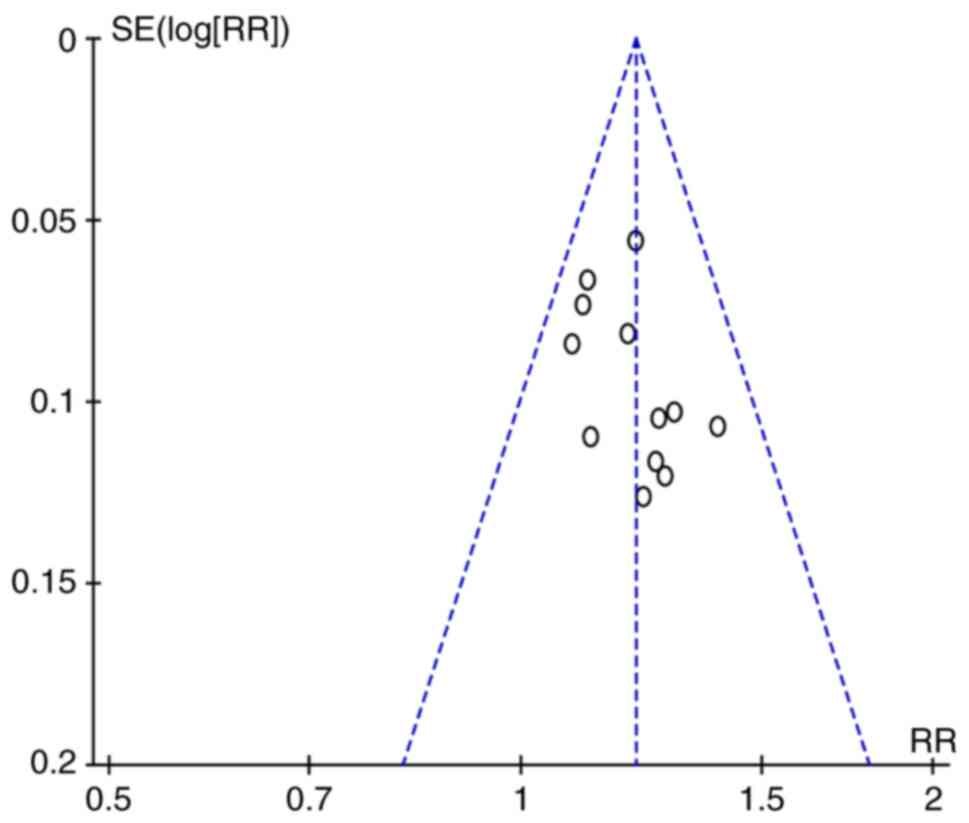
(Fig. 3). There was low publication
bias in the results (Fig. 4).
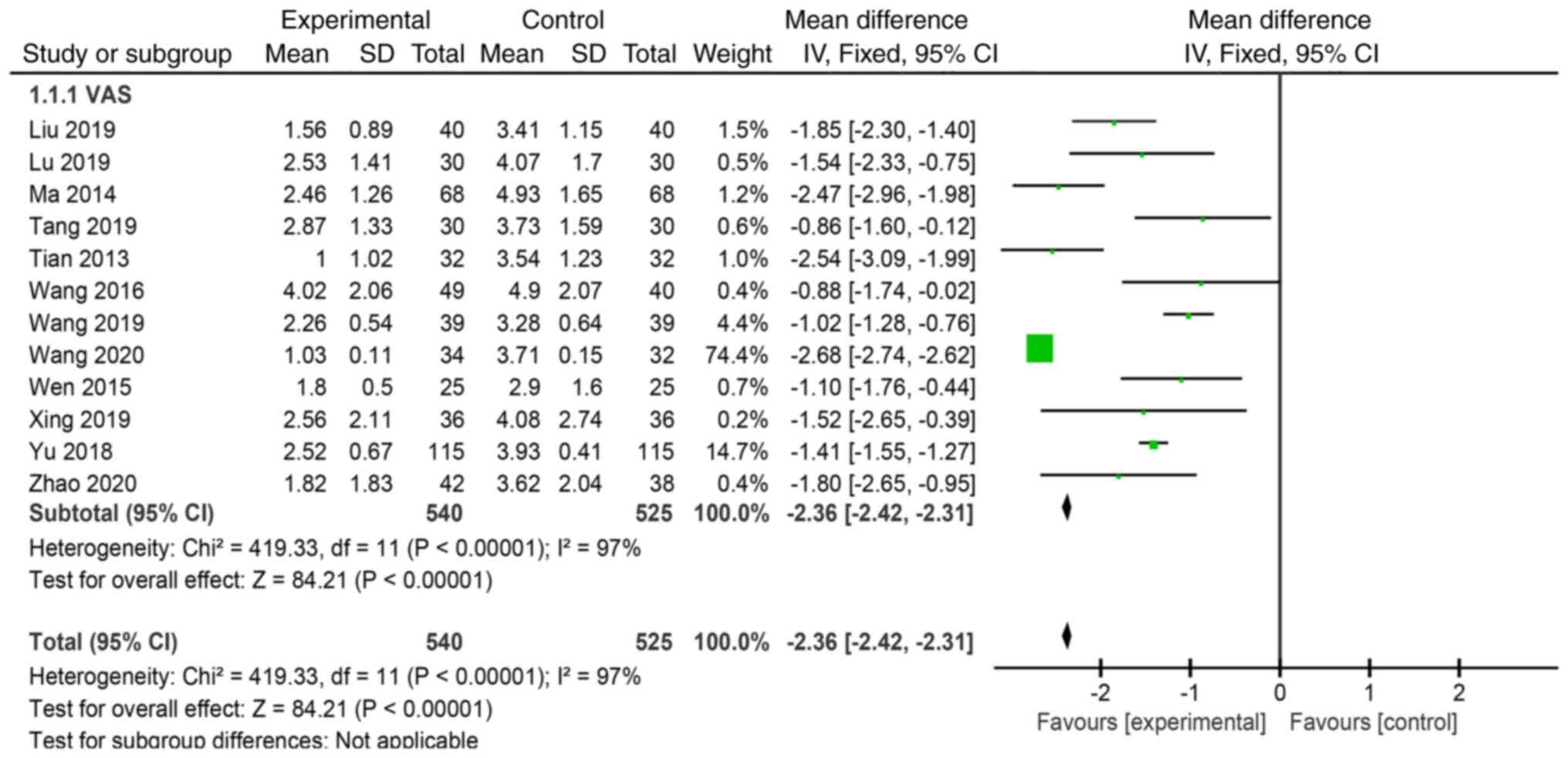
VAS score. Post-treatment VAS scores were
reported in 12 studies (15-26).
VAS scores were decreased after intervention and were significantly
different between the experimental group and control group
(WMD=-2.31, 95% CI: -2.42-2.31, P<0.00001] (Fig. 5). However, there was high
heterogeneity among the studies (P<0.00001, I2=97%).
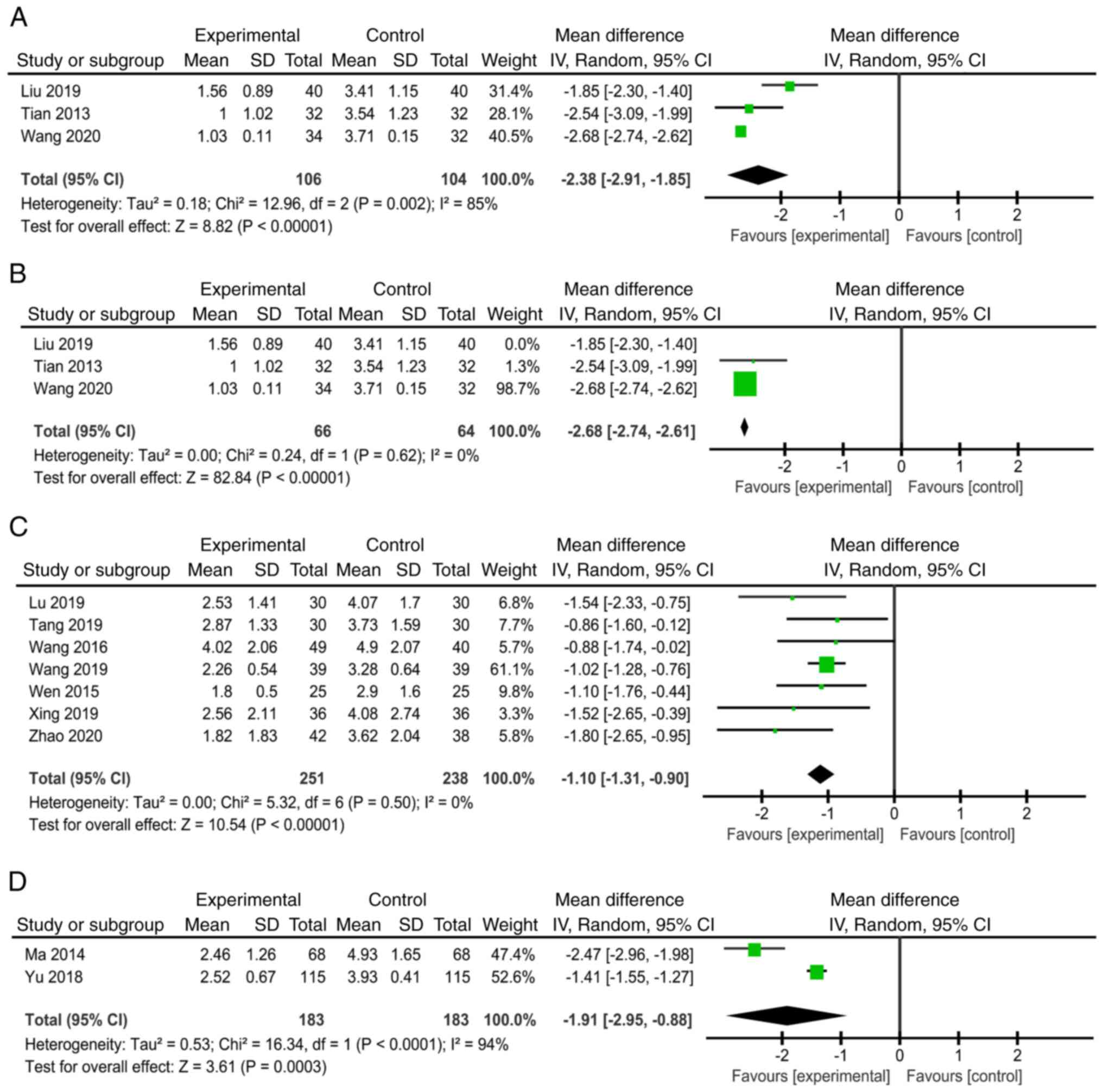
Therefore, a subgroup analysis was conducted according to different
interventions.
As shown in Fig. 6,
three studies (15,19,22)
compared BLP-C vs. Western medicine (Fig. 6A). Furthermore, seven studies
(16,18,20,21,23,24,26)
compared BLP-C plus acupuncture or TCM vs. Western medicine
(Fig. 6C). In addition, two studies
(17,25) compared BLP-C plus acupuncture and
TCM vs. Western medicine. BLP-C was superior to pharmacological
therapy in relieving pain in all three subgroups; however, there
was high heterogeneity among the studies (I2 =85%,
P=0.002, Fig. 6A; I2 =
94%, P<0.00001, Fig. 6D). Thus,
a sensitivity analysis was further conducted. As shown in Fig. 6B, heterogeneity was decreased upon
removal of the study by Liu (15)
(I2=0%, P=0.62), but VAS scores were still significantly
different between the BLP-C plus acupuncture and TCM group and the
pharmacological therapy group. It was suspected that the observed
heterogeneity may be attributed to variations in the duration of
treatment and the specific Western medicines employed in the
control group across the included studies. The differences in the
duration of treatment may have influenced the treatment outcomes
and given rise to heterogeneity. Each study may have adopted a
different duration or frequency of treatment, leading to variations
in patient response and overall treatment effects.
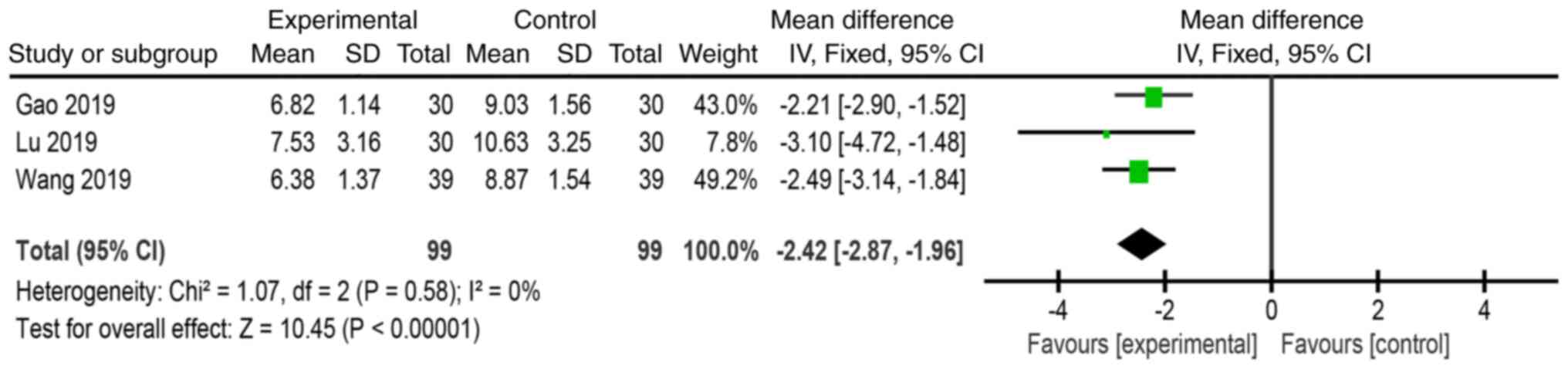
PSQI. The PSQI was reported by three studies
(14,16,21).
PSQI scores were decreased after intervention in both groups and
were significantly lower in the experimental group than in the
control group (WMD=-2.42, 95% CI: -2.87 to -1.96, P<0.00001,
Fig. 7), which suggests that BLP-C
is superior to Western medicine in improving sleep quality.
However, PSQI scores were only reported by 3 RCTs with a small
sample size. Therefore, further investigations are warranted to
confirm this conclusion.
Safety. Adverse reactions were mostly caused
by drugs, which resolved after treatment discontinuation. Of the 13
studies included, 3 studies (17,25,26)
reported stomach discomfort in the pharmacological therapy group,
including 2 cases receiving vitamin B1 injection, mecobalamin and
Fenbid (n=30) (17), 4 cases
receiving paracetamol and codeine (n=12) (25) and 2 cases receiving carbamazepine
(n=12) (26). Furthermore, one
study reported 11 cases of adverse reactions of the nervous system
in the control group (paracetamol and codeine, n=12) (25). Conversely, only 4 cases (17,25) of
adverse reactions were reported in the BLP-C group (Table SII).
Discussion
The present systematic review and meta-analysis were
performed on 13 RCTs (14-26)
published between 2013 and 2020. The findings showed that the BLP-C
group had a better VAS score, PSQI score and safety profile than
the Western medicine group. VAS and PSQI scores were used as
outcome measures to quantify improvements in pain and sleep
disorders, which are the most common symptoms of PHN. In addition,
two studies (14,22) reported the start time of pain relief
and the results showed that the BLP-C group had earlier pain relief
than the Western medicine group. The duration of disease in the
experimental group was 20.04±1.68 and 4.00±0.00 months,
respectively, which indicates that BLP-C may be more effective for
both a short and long disease duration.
The pathogenesis of PHN is highly complex and
involves both peripheral and central sensitization, which makes
treatment challenging (27). There
is compelling evidence from skin biopsies, along with subcutaneous
and cutaneous drug challenges, showing that the peripheral
afferents may be a significant pain generator in a subset of
patients with PHN (28).
Furthermore, a previous clinical trial indicated that inhibiting
inflammation of locally injured nerves may help reduce the
intensity of pain in patients with PHN (29). These findings suggest that
inhibiting peripheral nociceptor stimulations and inflammatory
responses may contribute to PHN pain.
Patients with PHN are often troubled by debilitating
pain of various sensations (e.g., burning pain or paroxysmal severe
pain) in the region of damaged innervation. The current
meta-analysis results indicated that the analgesic effect of BLP-C
was superior to that of Western medicine. BLP-C combines both
acupuncture and cupping to treat the painful area. After the
cupping site is disinfected, it is punctured by a three-edged
needle to release blood, henceforth blood-letting. Cupping is then
performed at the bloodletting site, and the negative pressure
inside the glass jar creates suction on the local skin and thus
induces bleeding at the puncture site. It was recently reported
that BLP-C may improve hemorheological abnormalities and local
microcirculation, reduce proinflammatory factors and eliminate
nerve root edema (30). Hence,
BLP-C of the painful region of the skin may modulate the
inflammatory microenvironment of the affected side of cases with
PHN, effectively reduce the transmission of peripheral noxious
stimuli to the spinal cord and inhibit the establishment of central
sensitization, thereby successfully reducing pain.
Elderly individuals with a weakened immune system
are most susceptible to PHN and related symptoms. It was shown that
BLP-C therapy is closely related to endocrine and immunological
regulation (31). Thus, controlling
the activity of the immune and endocrine systems may be the
therapeutic mechanism of BLP-C in PHN. Human nerve endings can
release ‘endorphin-like chemicals’ when the acupoint is stimulated,
increasing the pain threshold and decreasing susceptibility to pain
(32). Signals triggered by the
needles during BLP-C may reach the brain and induce the release of
several central neurotransmitters, including acetylcholine,
morphine and 5-hydroxytryptamine, thereby enhancing the analgesic
effects (33). Cupping after
puncture may help discharge blood stasis and dredge the meridians
and Qi, which can effectively improve the local blood circulation
and maintain nutritional supply.
BLP-C exerts neuromodulatory effects by controlling
the release of neurotransmitters, such as endorphin (34) and substance P (19,22).
The present meta-analysis showed that the serum level of substance
P is decreased after treatment. Substance P can induce the
accumulation of pain-causing and inflammatory substances, thereby
leading to neurogenic inflammation and persistent or worsening
pain. BLP-C may lead to higher oxygen saturation (35), which can remove oxidants, reduce
oxidative stress and damage caused by free radicals, and protect
cells and tissues. These effects are all associated with pain
relief and the improvement of sleep quality. In addition, it was
shown that substance P can influence sleep physiology through
neurokinin receptors (36).
Andersen et al (37)
revealed that a certain dose of substance P led to decreased sleep
efficiency and increased sleep onset latency.
PHN is often accompanied by sleep disorders
(38). In addition to the
improvement of pain, BLP-C is also better than Western medicine in
improving sleep quality. There is a bidirectional relationship
between sleep disturbance and pain (39). Chronic pain can interfere with sleep
depth and continuity, as well as reduce sleep duration and quality
(40). Furthermore, decreased sleep
quality can increase pain sensitivity and severity (41). On the other hand, pain in patients
with PHN often occurs in the chest, back, waist and abdomen
(2). Compression of certain body
parts during sleep may aggravate the patients' pain perception,
increase their physiological stress response and thus affect their
sleep quality. Altogether, this suggests that BLP-C may improve
sleep quality by reducing pain.
The findings of the present review support that
BLP-C is a safe and effective treatment for PHN. Western medicines
generally have hepatorenal toxicity and elderly patients are less
likely to tolerate long-term medication. Compared with Western
medicine, BLP-C is performed directly on the skin and does not
cause hepatorenal toxicity, which makes this treatment approach
favorable for patients with weak gastrointestinal function or renal
insufficiency. Collectively, the present results demonstrated that
BLP-C is a promising complementary and alternative therapy for
addressing pain and sleep loss in patients with PHN, particularly
in those who are elderly and have poor liver and renal
functions.
Although the literature on BLP-C treatment for PHN
was comprehensively reviewed for the present study, certain
limitations remain. First, the studies included in the present
meta-analysis were of medium quality and there may be biases in the
results due to language restriction. Furthermore, the subjectivity
of assessors may have introduced bias. Finally, the duration of
treatment varied among studies, which in turn may affect the
accuracy of the results. Further studies with better design or
higher quality are warranted to confirm the present findings.
In conclusion, the present systematic review showed
that BLP-C is an effective therapy for reducing pain intensity and
improving sleep quality in patients with PHN. The therapeutic
effects of BLP-C are mediated through multiple targets and
pathways, whereas Western medicine usually addresses a single
target, which may explain the superior efficacy of BLP-C compared
with Western medicine. Therefore, BLP-C is an effective external
therapy worthy of further application in the treatment of PHN. Due
to the limited quantity and quality of the included studies, more
high-quality studies are needed to ascertain these findings.
Supplementary Material
Search strategy for PubMed.
Incidence of adverse reactions.
Acknowledgements
Not applicable.
Funding
Funding: The current study was supported by the Shanghai Science
and Technology Planning Project (grant no. 20Y21903100), Clinical
Research Plan of Shanghai Shenkang Hospital Development Center
(grant no. SHDC2020CR3102B), Shanghai Three-year Action Plan for
Further Accelerating the Development of TCM [grant no.
ZY(2018-2020)-ZYBZ-06] and Shanghai University of TCM Excellent
Talents Training Program [grant no. TCM(2020)10].
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author upon reasonable
request.
Authors' contributions
KW and CX conceived and designed the study and set
the direction of the manuscript. WK and LX performed the literature
search and KW made the final decision regarding study inclusion. WK
and LX prepared the original manuscript, as well as figures and
tables. YL and ZG analyzed the study data. SL visualized the study
data. CX and KW reviewed and proofread the manuscript. All authors
contributed to editorial changes to the manuscript. All authors
have read and approved the final version of the manuscript. CX and
KW have checked and approved the authenticity of the raw data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sampathkumar P, Drage LA and Martin DP:
Herpes zoster (shingles) and postherpetic neuralgia. Mayo Clin
Proc. 84:274–280. 2009.PubMed/NCBI View
Article : Google Scholar
|
|
2
|
Johnson RW and Rice AS: Clinical practice.
Postherpetic neuralgia. N Engl J Med. 371:1526–1533.
2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Bollea-Garlatti ML, Bollea-Garlatti LA,
Vacas AS, Torre AC, Kowalczuk AM, Galimberti RL and Ferreyro BL:
Clinical characteristics and outcomes in a population with
disseminated herpes zoster: A retrospective cohort study. Actas
Dermosifiliogr. 108:145–152. 2017.PubMed/NCBI View Article : Google Scholar : (In English,
Spanish).
|
|
4
|
Yang F, Yu S, Fan B, Liu Y, Chen YX, Kudel
I, Concialdi K, DiBonaventura M, Hopps M, Hlavacek P, et al: The
Epidemiology of herpes zoster and postherpetic neuralgia in China:
Results from a cross-sectional study. Pain Ther. 8:249–259.
2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Attal N, Cruccu G, Baron R, Haanpää M,
Hansson P, Jensen TS and Nurmikko T: EFNS guidelines on the
pharmacological treatment of neuropathic pain: 2010 revision. Eur J
Neurol. 17:1113–e1188. 2010.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Dubinsky RM, Kabbani H, El-Chami Z,
Boutwell C and Ali H: Quality Standards Subcommittee of the
American Academy of Neurology. Practice parameter: Treatment of
postherpetic neuralgia: An evidence-based report of the Quality
Standards Subcommittee of the American Academy of Neurology.
Neurology. 63:959–965. 2004.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Massengill JS and Kittredge JL: Practical
considerations in the pharmacological treatment of postherpetic
neuralgia for the primary care provider. J Pain Res. 7:125–132.
2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Mehta P and Dhapte V: Cupping therapy: A
prudent remedy for a plethora of medical ailments. J Tradit
Complement Med. 5:127–134. 2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Saha FJ, Schumann S, Cramer H, Hohmann C,
Choi KE, Rolke R, Langhorst J, Rampp T, Dobos G and Lauche R: The
effects of cupping massage in patients with chronic neck pain-a
randomised controlled trial. Complement Med Res. 24:26–32.
2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Emerich M, Braeunig M, Clement HW, Lüdtke
R and Huber R: Mode of action of cupping-local metabolism and pain
thresholds in neck pain patients and healthy subjects. Complement
Med Res. 22:148–158. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Guo Y, Chen B, Wang DQ, Li MY, Lim CH, Guo
Y and Chen Z: Cupping regulates local immunomodulation to activate
neural-endocrine-immune worknet. Complement Ther Clin Pract.
28:1–3. 2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Price DD, McGrath PA, Rafii A and
Buckingham B: The validation of visual analogue scales as ratio
scale measures for chronic and experimental pain. Pain. 17:45–56.
1983.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Buysse DJ, Reynolds CF III, Monk TH,
Berman SR and Kupfer DJ: The Pittsburgh sleep quality index: A new
instrument for psychiatric practice and research. Psychiatry Res.
28:193–213. 1989.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Gao J, Lou Z and Yu L: Therapeutic effects
of acupuncture and pricking blood with cupping combined with
Taohong Siwu decoction on herpes zoster and its effect on sequelae
neuralgia. Shi Jie Zhong Yi Yao. 14:2163–2165. 2019.(In
Chinese).
|
|
15
|
Liu F: A clinical analysis of treating
post-herpetic neuralgia by blood-letting puncture and cupping.
Zhong Guo Lin Chuang Yan Jiu. 11:72–73. 2019.
|
|
16
|
Lu Y, Xiao H and Chen R: Clinical study of
acupuncture checkpoint combined with lancet cupping in the
treatment of postherpetic neuralgia in elderly people. Hubei Zhong
Yi Yao Za Zhi. 41:49–51. 2019.(In Chinese).
|
|
17
|
Ma X and Zhang W: Effects of Xuefuzhuyu
tablets combined with acupuncture and pricking and cupping therapy
in treating postherpetic neuralgia. Yi Xue Yan Jiu Yu Jiao Yu.
30:47–50. 2013.(In Chinese).
|
|
18
|
Tang Q, Wang L and Zhao Z: Silver needle
combined with needle cupping for the treatment of postherpetic pain
in 30 cases. Shanxi Zhong Yi Yao Da Xue Xue Bao. 42:100–106.
2019.(In Chinese).
|
|
19
|
Tian H, Tian Y, Wang B, Yang L, Wang YY
and Yang JS: Moxibustion, impacts of bleeding and cupping therapy
on serum P. substance in patients of postherpetic neuralgia. Zhong
Guo Zhen Jiu. 33:678–681. 2013.PubMed/NCBI(In Chinese).
|
|
20
|
Wang S: Tonic Yang also five decoctions
combined with blood pricking cupping for the treatment of
postherpetic neuralgia. Jilin Zhong Yi Yao. 36:844–846. 2016.(In
Chinese).
|
|
21
|
Wang N, Ceng S and Yu M: Clinical
observation of 39 cases of postherpetic neuralgia with fire
acupuncture combined with pricking cupping. Hunan Zhong Yi Yao Za
Zhi. 35:73–74. 2019.(In Chinese).
|
|
22
|
Wang L, Fang Y and Li Q: Effect of
pricking and cupping on serum substance P and IL-6 in patients with
postherpetic neuralgia. Zhong Guo Zhong Yi Yao Xian Dai Yuan Cheng
Jiao Yu. 18:92–94. 2020.(In Chinese).
|
|
23
|
Wen B, Li X and Deng X: Acupuncturing
umbilical ring acupoints in Zhuang medicine and lotus needle
cupping stasis on AIDS patients with postherpetic neuralgia a
clinical observation. Shizhen Guo Yi Guo Yao. 26:2175–2177.
2015.(In Chinese).
|
|
24
|
Xing Y, Yuan J and Zhang S: Clinical study
of double surround needling combined with pricking-cupping
bloodletting in the treatment of senile postherpetic neuralgia.
Hebei Zhong Yi. 41:587–591. 2019.(In Chinese).
|
|
25
|
Yu Z, Yao X and Liang R: Clinical study on
the treatment of postherpetic neuralgia by traditional Chinese
medicine comprehensive therapy under the guidance of the theory of
dissolving stasis communication. Hebei Zhong Yi Yao Xue Bao.
40:1021–1024. 2018.(In Chinese).
|
|
26
|
Zhao Y and Li C: The efficacy of Da Chai
Hu Tang and Gui Zhi Zhuo Ling Pills combined with spiny cupping in
the treatment of postherpetic neuralgia was observed. Shi Yong
Zhong Yi Yao Za Zhi. 29:809–810. 2013.(In Chinese).
|
|
27
|
Mallick-Searle T, Snodgrass B and Brant
JM: Postherpetic neuralgia: Epidemiology, pathophysiology, and pain
management pharmacology. J Multidiscip Healthc. 9:447–454.
2016.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Fields HL, Rowbotham M and Baron R:
Postherpetic neuralgia: Irritable nociceptors and deafferentation.
Neurobiol Dis. 5:209–227. 1998.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Sommer C, Leinders M and Üçeyler N:
Inflammation in the pathophysiology of neuropathic pain. Pain.
159:595–602. 2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Wang X, Yuan A and Yuan L: Research
progress on the functional mechanism of Blood-letting collateral
puncture and cupping therapy and its clinical application. N Chin
Med. 52:128–130. 2020.
|
|
31
|
Ahmed SM, Madbouly NH, Maklad SS and
Abu-Shady EA: Immunomodulatory effects of Blood Letting cupping
therapy in patients with rheumatoid arthritis. Egypt J Immunol.
12:39–51. 2005.PubMed/NCBI
|
|
32
|
Patil S, Sen S, Bral M, Reddy S, Bradley
KK, Cornett EM, Fox CJ and Kaye AD: The role of acupuncture in pain
management. Curr Pain Headache Rep. 20(22)2016.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Chen T, Zhang WW, Chu YX and Wang YQ:
Acupuncture for pain management: Molecular mechanisms of action. Am
J Chin Med. 48:793–811. 2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Subadi I, Nugraha B, Laswati H and
Josomuljono H: Pain relief with wet cupping therapy in rats is
mediated by heat shock protein 70 and ß-endorphin. Iran J Med Sci.
42:384–391. 2017.PubMed/NCBI
|
|
35
|
Tagil SM, Celik HT, Ciftci S, Kazanci FH,
Arslan M, Erdamar N, Kesik Y, Erdamar H and Dane S: Wet-cupping
removes oxidants and decreases oxidative stress. Complement Ther
Med. 22:1032–1036. 2014.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Zielinski MR and Gerashchenko D:
Sleep-inducing effect of substance P-cholera toxin A subunit in
mice. Neurosci Lett. 659:44–47. 2017.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Andersen ML, Nascimento DC, Machado RB,
Roizenblatt S, Moldofsky H and Tufik S: Sleep disturbance induced
by substance P in mice. Behav Brain Res. 167:212–218.
2006.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Zilliox LA: Neuropathic pain. Continuum
(Minneap Minn). 23 (2, Selected Topics in Outpatient
Neurology):512–532. 2017.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Shyen S, Amine B, Rostom S, E L Badri D,
Ezzahri M, Mawani N, Moussa F, Gueddari S, Wabi M, Abouqal R, et
al: Sleep and its relationship to pain, dysfunction, and disease
activity in juvenile idiopathic arthritis. Clin Rheumatol.
33:1425–1431. 2014.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Melikoglu MA and Celik A: Does neuropathic
pain affect the quality of sleep? Eurasian J Med. 49:40–43.
2017.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Covarrubias-Gomez A and Mendoza-Reyes JJ:
Evaluation of sleep quality in subjects with chronic nononcologic
pain. J Pain Palliat Care Pharmacother. 27:220–224. 2013.PubMed/NCBI View Article : Google Scholar
|