Introduction
Granulomatous mastitis (GM) is a rare inflammatory
disorder of the breast, which typically develops in women of
childbearing age who have a history of breastfeeding (1). GM is classified into two types:
Idiopathic GM or primary GM, as well as secondary GM. Infections
such as histoplasmosis and actinomycosis, along with autoimmune
conditions such as granulomatosis with polyangiitis, IgG4-related
diseases like mastitis, sarcoidosis, fat necrosis and foreign body
reactions, are all potential triggers for secondary GM (2). In 1972, Kessler and Wolloch (3) initially documented GM, but it was
Cohen (4) who provided a more
comprehensive description of the condition in 1977. Despite being a
benign disease, it is frequently difficult to detect, and its
locally aggressive character causes long-term discomfort and
distress for affected patients (5).
It is a serious condition, since it clinically mimics cancer
(6). Ethnic diversity has a role in
the distribution of this condition, as GM occurrences are more
prevalent in Middle Eastern nations compared to Western countries
(7). GM in accessory breast tissue
is rare. There have been only a small number of cases of GM
identified in axillary accessory breast tissue that have been
documented in the medical literature (2,8-10),
excluding those published in predatory journals.
The present case report reports on a rare clinical
presentation of GM in accessory breast tissue, providing
information on the diagnosis and therapeutic challenges of this
unusual disease.
Case report
Patient information
A 39-year-old female patient presented with right
axillary discomfort and swelling for ~5 days, associated with
redness, fever and chills. The patient had three children and she
had breastfed two of them for ~17 months each; the last child was
breastfed only three months intermittently from the right breast.
The last time the patient lactated was approximately two years
prior to the current presentation. She was non-diabetic with a past
medical history of left breast GM in November 2018. The patient was
a nonsmoker and her other medical history was unremarkable. Her
diet consisted of eating daily meals of low-fat and low-salted food
with high amounts of vegetables. She ate less fruit and fried food,
and a lot of sweet or sweetened food.
Clinical findings
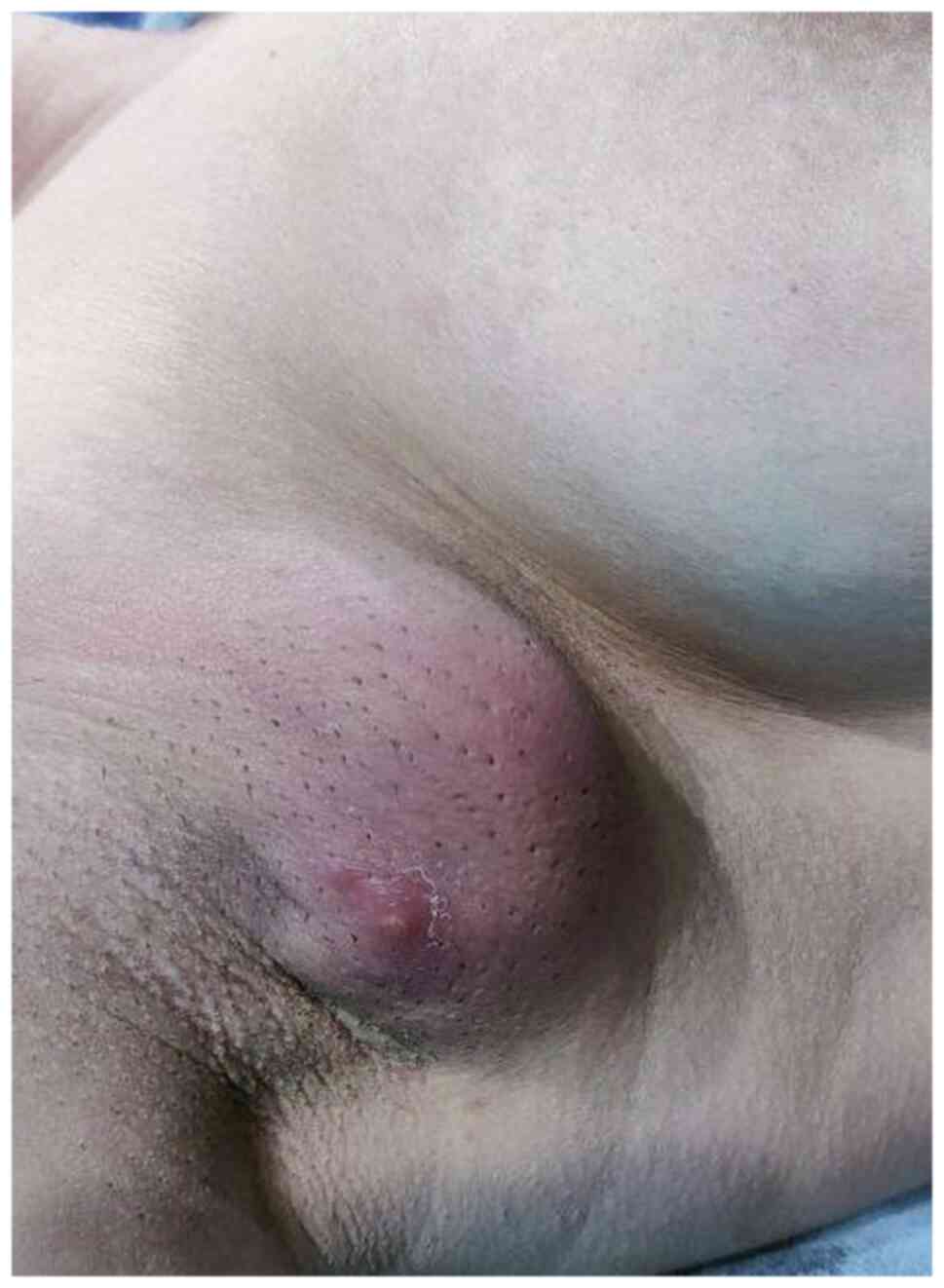
During the clinical examination, a tender, firm lump
was detected in the right axillary region. The lump displayed signs
of inflammation, including redness and warmth, and there were also
palpable lymph nodes in the axilla (Fig. 1).
Diagnostic approach
The breast ultrasound (US) was performed externally
at Breast Center on Malik Mahmud Ring Road (HCMR+46H; Sulaymaniyah,
Iraq). Unfortunately, the US image is not available. It revealed
bilateral normal breasts with normal left accessory breast. The
right accessory breast showed diffuse parenchymal heterogeneity and
surrounding edema associated with reactive axillary lymph nodes.
There was no evidence of fluid accumulation, implying a diagnosis
of mastitis. The complete blood count results fell within the
normal range.
Therapeutic interventions
Initially, conservative treatment commenced with a
five-day course of antibiotics, specifically oral amoxicillin and
clavulanic acid. However, during the follow-up, the patient did not
show any improvement with the medication. Consequently, surgical
excision was proposed as an alternative, considering the patient's
history of successfully treating left breast GM through surgical
intervention when medication proved ineffective. After obtaining
informed consent, the surgical procedure was performed in the form
of an excisional biopsy. This procedure was conducted under general
anesthesia and involved a seven-centimeter elliptical incision with
no drain placed.
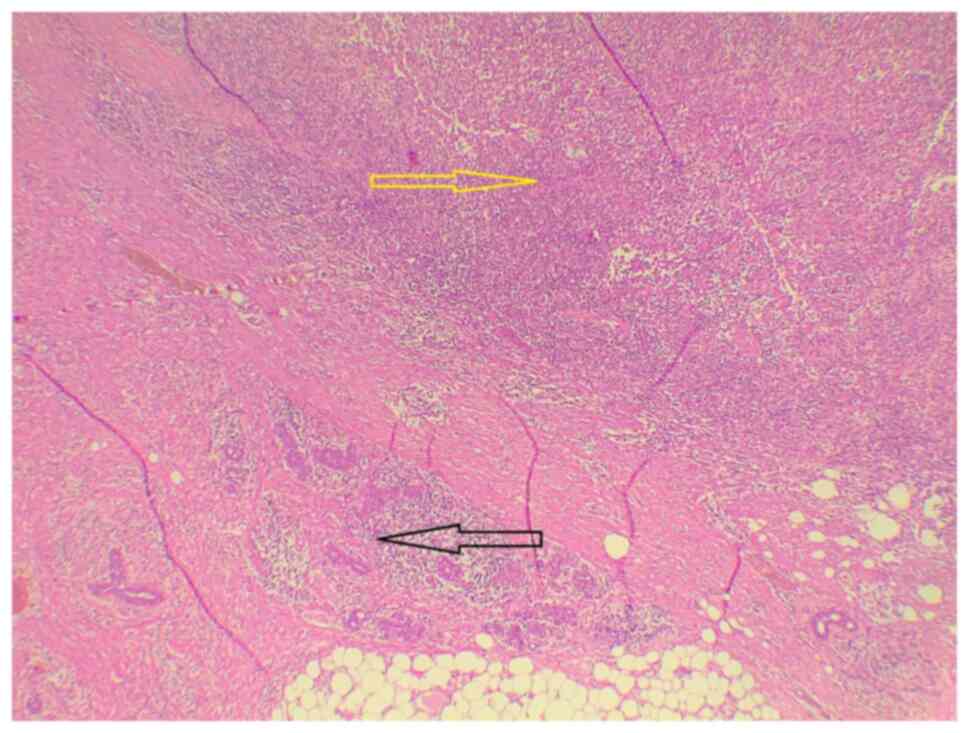
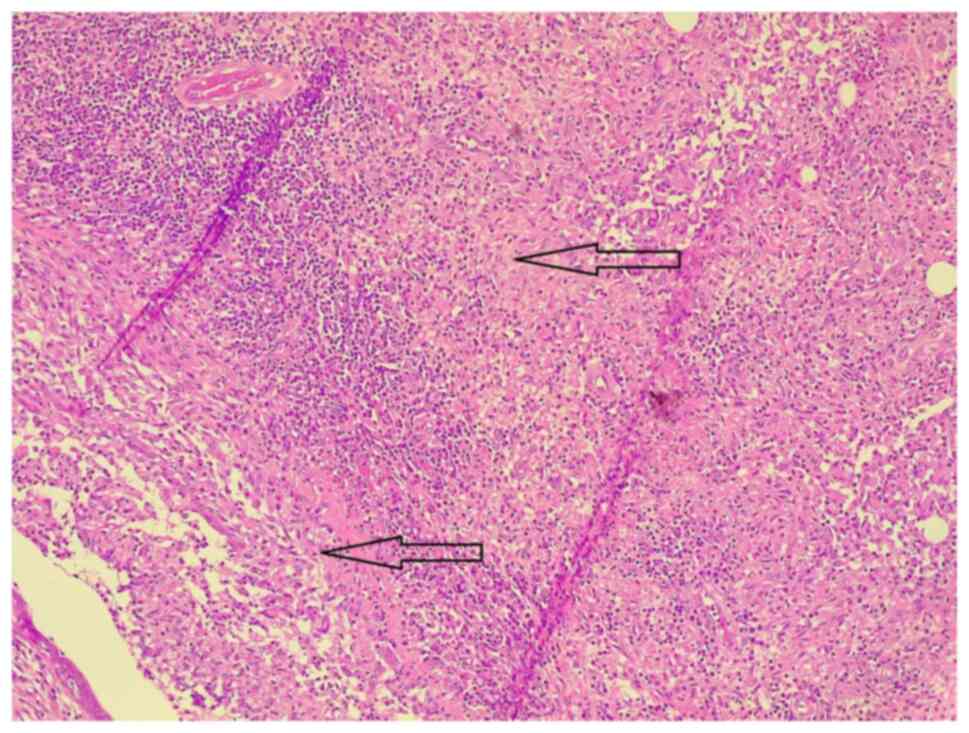
The excised tissue was sent for histopathological
examination (HPE). The examined tissue underwent a pathological
staining process according to standard procedures (Data S1).
The HPE indicated the presence of breast tissue with
duct ectasia and suppurative granulomatous inflammation leading to
abscess formation (Figs. 2 and
3). Importantly, no malignancy was
detected in the histopathological findings.
Follow-up
The postoperative course was uneventful. In zero-day
postoperative care, nearly 12 h after surgery, the patient was
discharged home without any complications. During the six-month
follow-up, the breast US showed no signs of recurrence, and the
patient was not symptomatic; therefore, she was kept on one-year
follow up.
Discussion
GM is a rare and clinically challenging inflammatory
breast disorder characterized by the formation of granulomas within
the breast tissue. It predominantly affects the mammary gland but
may, in rare cases, occur within accessory breast tissue (8). Accessory breast tissues can be seen
along the embryonic mammary ridge, which runs from the axilla to
the pubic region. The disease processes affecting axillary breast
tissue are the same as those affecting the tissue of the main
breast (9). While GM is most
frequently observed in women who are in their third and fourth
decades of life, it is often identified within a few years after
childbirth, and most individuals affected by this condition have
experienced at least one live birth and have breastfed (11).
The exact cause of GM remains uncertain and the
etiology within accessory breast tissue is even less understood.
Proposed mechanisms suggest that it may result from an exaggerated
immune response triggered by various factors, such as infection,
autoimmunity or hormonal fluctuations. However, no single
etiological factor has been consistently identified (1). Only a few cases of GM in accessory
breast tissue have been documented in the English literature. Two
of these occurred in women of childbearing age after giving birth
and one during pregnancy (2,8,9).
The patient of the present case study had three children and
breastfed for a total of three years. She had a history of GM of
the contralateral breast in 2018.
GM is often unilateral, with few reports of
bilateral involvement. A large, tender lump, frequently several
centimeters in diameter, is the most common presenting symptom.
This is usually associated with skin abnormalities such as erythema
and ulceration. Sinuses can occur, with discharge from the lesions.
Multiple lumps and ulcers in one or more quadrants of the breast
are common. Systemic features such as fever are uncommon (5,11). The
current patient presented with right axillary pain and swelling for
~5 days, associated with fever and chills. On examination, there
was a hard, palpable lump in the right axilla; it was tender and
exhibited evidence of inflammation, such as redness and pain, as
well as palpable axillary lymph nodes.
Diagnosing GM is often challenging due to its rarity
and the absence of specific clinical or radiological features.
Mammography often shows nonspecific features that do not provide a
definitive diagnosis, such as asymmetric density (12). In cases where an abscess is present,
US can be a valuable diagnostic tool. It is able to display an
irregular mass with mixed heterogeneity. However, these findings
are non-specific and may overlap with other breast pathologies
(5). In the current case, the US
revealed the normal features of both the main breasts and the left
accessory breast. However, there were notable irregularities in the
tissue of the right accessory breast, parenchymal heterogeneity
with preserved architecture without associated mass or ductal
distortion, marked by significant variation in density, along with
edema in the surrounding area, which was more evident than in
malignancy. Importantly, there was no sign of fluid accumulation,
which typically suggests mastitis. In addition, reactive lymph
nodes were observed in the adjacent axillary region. The axillary
lymph nodes showed concentric regular outline cortical thickening
and the vascularity was going from the hilum towards the cortices,
not vice versa as it occurs in malignancy.
Definitive diagnosis often relies on
histopathological examination, typically obtained through
fine-needle aspiration cytology (FNAC) or core needle biopsy (CNB).
Although FNAC may aid in a quicker diagnosis, it is not as specific
as CNB. As a result, in the literature, CNB is regarded as the gold
standard preoperative diagnostic modality (1,5,13). The
condition is distinguished by the formation of granulomas in
conjunction with localized infiltration of multi-nucleated giant
cells, lymphocytes, epithelioid histiocytes and plasma cells
(1).
Regarding the management, there is no agreement on
the optimum treatment for GM; however, medical therapy, surgical
excision, abscess drainage or only close observation are now the
most popular choices. Antibiotics, systemic steroids, nonsteroidal
anti-inflammatory drugs and immunosuppressive medicines, such as
methotrexate and azathioprine, have been documented as medical
therapies (14). Corticosteroids,
while commonly employed by numerous clinicians and yielding
positive results, have a restricted role primarily due to the
absence of consensus regarding their optimal timing, duration and
dosage. Commencing steroid therapy can be complicated by concerns
about the presence of an infectious cause (15). Furthermore, the use of
corticosteroids may lead to potential adverse effects, including
Cushing syndrome, hyperglycemia, weight gain and susceptibility to
opportunistic infections (8). The
period required for complete remission typically spans from six
weeks to eleven months, necessitating prolonged patient follow-up,
which may pose challenges when patients are non-compliant with
follow-up appointments (16).
In the present case, surgical excision was performed
and no signs of recurrence were observed during a six-month
follow-up period. Surgery was chosen for this patient due to her
previous successful surgery on the contralateral breast, the
favorable cosmetic outcomes associated with surgery in this region,
the potential for a precise diagnosis and the prospect of faster
recovery. After surgery, recurrence rates of 5.5-50% have been
reported (17).
Healthcare providers should be aware of the
possibility of GM occurring in accessory breast tissue,
particularly when evaluating patients with axillary masses. Prompt
diagnosis is crucial to avoiding delays in appropriate treatment
and minimizing patient discomfort. Given the rarity of this
condition, a high index of suspicion is essential. Treatment
options should be individualized, taking into account the patient's
symptoms and the extent of the disease. In cases of GM in accessory
breast tissue, surgical excision may be a suitable option,
considering the potential for favorable cosmetic outcomes and a
definitive diagnosis. Long-term follow-up is vital to monitor for
disease recurrence, complications and treatment efficacy.
In conclusion, GM in accessory breast tissue is a
rare and challenging clinical condition to diagnose. Due to the
rarity of this condition, it highlights the importance of including
GM in the differential diagnosis of axillary masses, particularly
when clinical and radiological characteristics are abnormal.
Further research is warranted to better understand the pathogenesis
and optimal treatment strategies. Increased awareness among
healthcare providers, along with collaborative efforts in research
and clinical care, will ultimately enhance the ability to diagnose
and manage this noteworthy and rare manifestation of GM.
Supplementary Material
Supplementary data
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
AMS and HOA were major contributors to the
conception of the study, as well as the literature search for
related studies. FHK, SHH, SHM and MNH were involved in the
literature review, study design and in writing the manuscript.
LRAP, SL, JIH, MLA and HOB were involved in the literature review,
the design of the study, critical revision of the manuscript and
processing of the figures. FHK and SHH confirm the authenticity of
all the raw data. AMA was the pathologist who performed the
histopathological diagnosis. All authors have read and approved the
final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient for participation in the present study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wolfrum A, Kümmel S, Theuerkauf I, Pelz E
and Reinisch M: Granulomatous mastitis: A therapeutic and
diagnostic challenge. Breast Care (Basel). 13:413–418.
2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Alvand S, Hessami A, Makhmalbaf AO and
Elahi A: Uncommon location of idiopathic granulomatous mastitis: A
case report. Arch Breast Cancer. 9 (3-SI):320–324. 2022.
|
|
3
|
Kessler E and Wolloch Y: Granulomatous
mastitis: A lesion clinically simulating carcinoma. Am J Clin
Pathol. 58:642–646. 1972.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Cohen C: Granulomatous mastitis-a review
of 5 cases. S Afr Med J. 52:14–16. 1977.PubMed/NCBI
|
|
5
|
Brennan ME, Morgan M, Heilat GB and
Kanesalingam K: Granulomatous lobular mastitis: Clinical update and
case study. Aust J Gen Pract. 49:44–47. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Carmalt HL and Ramsey-Stewart G:
Granulomatous mastitis. Med J Aust. 1:356–359. 1981.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Deng Y, Xiong Y, Ning P, Wang X, Han XR,
Tu GF and He PY: A case management model for patients with
granulomatous mastitis: A prospective study. BMC Womens Health.
22(143)2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Nakamura J, Tanaka F, Ohtaka K, Sato K and
Iyama A: A rare case of granulomatous mastitis in the accessory
axillary breast of a pregnant woman successfully treated by
surgery. Eur J Breast Health. 18:195–198. 2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Yılmaz MA, Kaya TI, Demirel M and Yuyucu
Karabulut Y: Pregnancy-associated granulomatous mastitis of
accessory breast: A novel clinical presentation. Dermatol Ther.
34(e14729)2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Muhialdeen AS, Ahmed JO, Baba HO, Abdullah
IY, Hassan HA, Najar KA, Mikael TM, Mustafa MQ, Mohammed DA, Omer
DA, et al: Kscien's list; a new strategy to discourage predatory
journals and publishers (second version). Barw Med J. 1:30–32.
2023.
|
|
11
|
Altintoprak F, Kivilcim T and Ozkan OV:
Aetiology of idiopathic granulomatous mastitis. World J Clin Cases.
2:852–858. 2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Camargo MD PhD A, F B, B DF, L S, J M,
Ramilo MD T and Balcarce MD TG: Is it possible to avoid the late
diagnosis of idiopathic granulomatous mastitis? Obstet Gynecol Int
J. 12:408–413. 2021.
|
|
13
|
Kumar MA, Pankaja S, Kumar NG and Sunayana
K: Varied clinical presentation of granulomatous mastitis-a
retrospective cohort study. Int J Anat Radiol Surg. 11:SO19–SO24.
2022.
|
|
14
|
Chirappapha P, Thaweepworadej P,
Supsamutchai C, Biadul N and Lertsithichai P: Idiopathic
granulomatous mastitis: A retrospective cohort study between 44
patients with different treatment modalities. Ann Med Surg (Lond).
36:162–167. 2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Bani-Hani KE, Yaghan RJ, Matalka II and
Shatnawi NJ: Idiopathic granulomatous mastitis: Time to avoid
unnecessary mastectomies. Breast J. 10:318–322. 2004.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Diesing D, Axt-Fliedner R, Hornung D,
Weiss JM, Diedrich K and Friedrich M: Granulomatous mastitis. Arch
Gynecol Obstet. 269:233–236. 2004.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kiyak G, Dumlu EG, Kilinc I, Tokaç M,
Akbaba S, Gurer A, Ozkardes AB and Kilic M: Management of
idiopathic granulomatous mastitis: Dilemmas in diagnosis and
treatment. BMC Surg. 14(66)2014.PubMed/NCBI View Article : Google Scholar
|