Introduction
Ureteral obstruction is one of the most common
urological emergencies, the etiology of which can be benign (in
case of ureteral stones or strictures secondary to surgery or
radiotherapy) or malign (when a urothelial cancer affects the
ureteral lumen or when an abdominal advanced neoplastic disease
compresses the ureter ‘ab estrinseco’) (1). Effective treatment should be
immediately carried out, in order to avoid the complications of
long-term obstruction (such as pain, infection and ultimately renal
failure). The scope of this treatment is to alleviate the patient
pain and to protect its renal function (2). To date, the most commonly used
existing surgical methods for ureteral obstruction include
percutaneous nephrostomy (PCN) and Double J stenting (DJS)
(3,4). PCN is performed under both sonographic
and fluoroscopy guidance. This procedure requires the patient to be
in the prone position and moderate sedation is needed. PCN
placement is associated with a risk of hemorrhage, urinary tract
infection and catheter dislodgement. On the other hand, DJS
placement is performed concomitantly with cystoscopy for the
visualization of the ureteral orifice, with the patient who is in
the supine position during the procedure. Early complications of
DJS placement include irritative bladder symptoms, hematuria and
stent discomfort; meanwhile, stent migration and encrustation are
among the common complications in the late period. The selection of
the drainage method is multifactorial and may be influenced by the
nature of each case, considering different factors such as
complexity, local technique expertise, availability of medical
equipment and patient features. For example, the classical ureteral
obstruction is due to stones; about this, we have to consider that
in certain health systems the waiting time for stone removal
surgery is long. For this reason, it was observed that an expected
long period time for definitive treatment biased the treating
urologist to prefer a ureteral stent over nephrostomy tube,
assuming the patient would be less bothered by the stent during the
waiting period. Currently, no existing guidelines suggest to the
urologist the ideal treatment for the obstructive uropathy. On one
hand, DJS placement is commonly considered as the best surgical
method, but it can occasionally be difficult to apply in patients
with cancer. On the other hand, the numerous complications
associated with the PCN procedure must be considered. The treatment
choice for patients with obstructive uropathy is, therefore, still
an open question. Both procedures have advantages and disadvantages
in regard to complications, costs and post-operative management.
Therefore, it is important to select the appropriate technique, as
each has its own unique impact on the patients' outcomes. For this
reason, it was assessed which of the two main methods is superior
in this type of patients according to normalization of renal
function indices, post-operative complication and the perception of
the quality of life by the patient's point of view.
Materials and methods
In a period between 2019 and 2023, a total of 317
consecutive patients (198 males and 119 females) presenting to the
emergency room of our hospital with a ureteral obstruction, which
was resolved surgically by DJ stent placement or nephrostomy tube,
were enrolled in the present study. All patients signed a written
informed consent. All data analyzed were collected as part of
routine diagnosis and treatment. Patients were treated according to
national and international guidelines and agreements. Surgical
drainage was performed when definitive treatment was not possible
immediately or when a two-stage procedure was considered a safer
approach. Inclusion criteria were: Ureteral obstruction with fever
(>38˚C), acute renal failure (indicated by an increase in
creatinine and urea nitrogen blood values), risk of sepsis
(suspected based on an increase in WBC count) or intractable pain.
Diagnosis of the ureteral obstruction was made by either a
non-contrast CT and/or renal ultrasound. Pregnant women and
patients with a contraindication to either form of drainage (for
example uncorrected coagulopathy excluding percutaneous tube,
hemodynamic instability precluding anesthesia for DJS placement or
abnormalities of the urinary tract) were excluded from the
analysis. Patients received either a DJS or a PCN according to the
surgeon's preference and to the availability of anesthetic support.
PCN was routinely performed in local anesthesia (1% Lidocaine, 10
cc), positioning a percutaneous pigtail polyurethane 8 or 10-French
catheter (Cook medical). Ureteral stents were placed under
loco-regional anesthesia and according to the commonly validated
technique; a 6 or 7 FR, Percuflex (Boston Scientific) stent of the
appropriate length (most commonly from to 24-28 cm) was used.
Specifically, 155 patients of the study sample were treated with
nephrostomy, whereas 217 individuals underwent to stenting
procedure. The standardized Clavien-Dindo classification of
surgical complications was used to assess and report post-operative
complications (5). According to
Clavien classification, post-operative complications were
subdivided in three grades as shown in Table I. The PCN group was composed of 79
men (mean age ± standard deviation: 58.17±16.21 years, min-max:
39-92 years) and 76 women (mean age ± standard deviation:
60.18±14.34 years, min-max=29-90 years), whereas the DJS group
constituted of 116 men (mean age ± standard deviation: 68.53±10.88
years, min-max=18-92 years) and 101 women (mean age ± standard
deviation: 64.01±15.94 years, min-max=23-85 years). Notably, the
legal age of adulthood in Italy is 18 years. For each participant,
data concerning the creatinine (mg/dl), azotemia (mg/dl), potassium
(mEq/l), WBC count (103/mm3), core
temperature (˚C), pain in the side (yes or not), anti-inflammatory
therapy (yes or not) and ASA score were evaluated. The pre- and
post-drainage data of creatinine, azotemia, potassium, WBC count
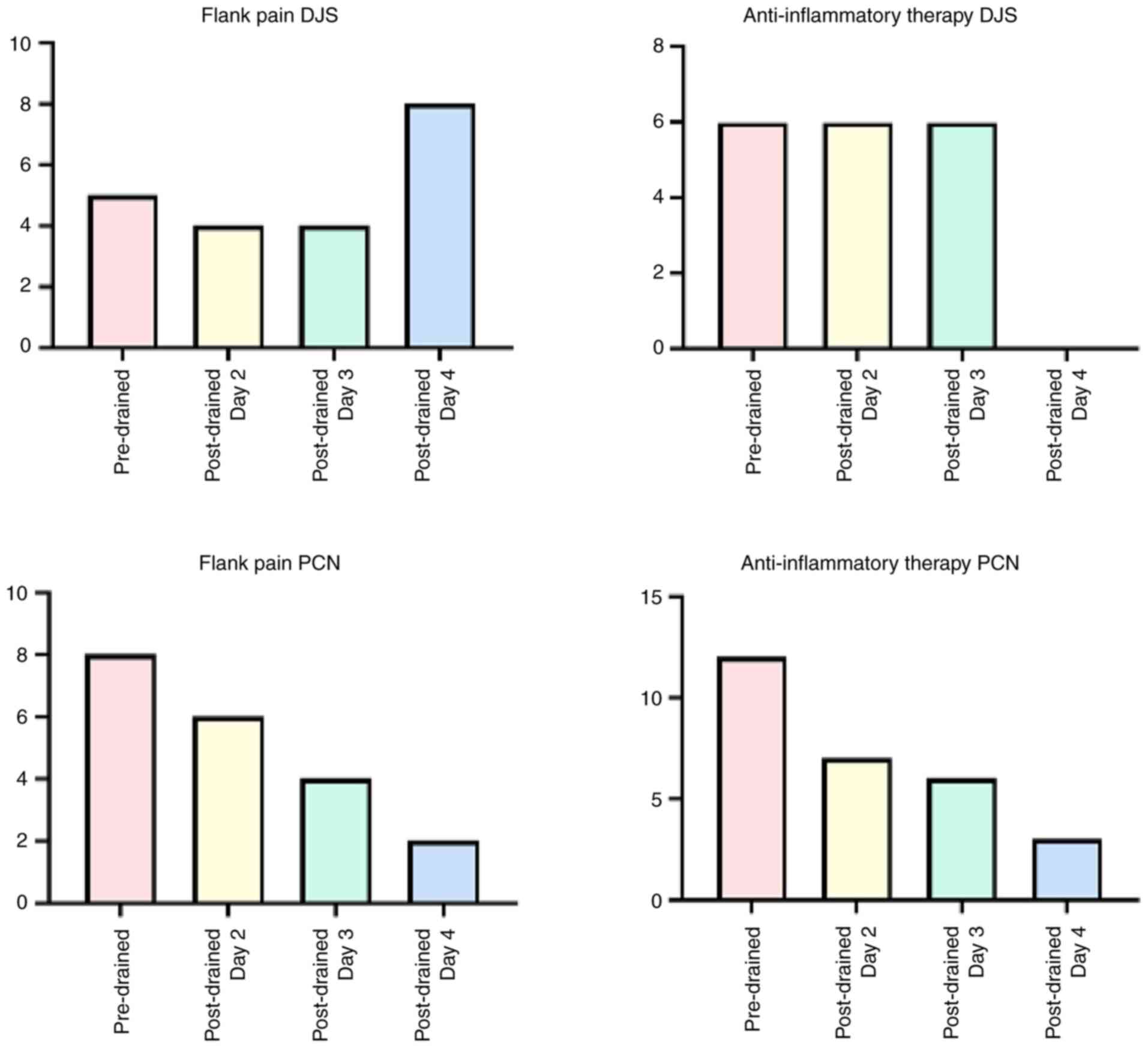
and core temperature are reported in Table II. The distribution of the flank
pain and of the anti-inflammatory therapy pre- and post-drainage
until 4 days after the intervention separately for the DJS and PCN
groups are reported in Fig. 1. In
both groups the post-procedural pain was measured with VAS scale,
suggesting a higher pain in patients with DJS. The VAS scale
corresponds to the visual representation of the extent of the pain
felt by the patient and is made up of a predetermined line 10 cm
long, where the left end corresponds to ‘no pain’ while the right
end corresponds to ‘worst possible pain’. Patients in the present
study were asked to draw a mark on the line representing the level
of pain they felt. The scale line can be oriented horizontally or
vertically, without this affecting its sensitivity; however, the
horizontal orientation was preferred. The scale was administered to
patients 24 h after the surgical procedure and in the following
days, until discharge. Thereafter, measurement was performed weekly
for a 6-month follow-up. The score was calculated in mm, measuring
with a ruler the length of the line between the end corresponding
to the minimum intensity and the mark placed by the patient. Based
on several studies, the following cut-off values were used: 0 to 4
mm: ‘no pain’; from 5 to 44 mm: ‘mild pain’; from 45 to 74 mm:
‘moderate pain’; and from 75 to 100 mm: ‘severe pain’.
 | Table IClavien-Dindo classification of
surgical complications. |
Table I
Clavien-Dindo classification of
surgical complications.
| GRADE I | Fever | Hematuria | Pain | Urgency | Urge
incontinence |
|---|
| GRADE II | Septicemia | Bleeding | Encrustation | Pyelonephritis | Infection |
| GRADE III | Percutaneous
nephrostomy dislodgement | Ureteral
perforation | Migration | Slippage | Tube obstruction |
 | Table IIThe pre- and post-drainage data of
creatinine, azotemia, potassium, WBC count and core temperature for
the group of patients with DJS and the group of patients with
PCN. |
Table II
The pre- and post-drainage data of
creatinine, azotemia, potassium, WBC count and core temperature for
the group of patients with DJS and the group of patients with
PCN.
| Group | | Pre-renal
drainage | Post renal drainage,
Day 2 | Post-renal drainage,
Day 3 | Post-renal drainage,
Day 4 |
|---|
| DJS | creatinine
(mg/dl) | 1.574±1.758 | 1.533±2.618 | 2.156±1.976 | 1.882±2.062 |
| | azotemia (mg/dl) | 56.019±38.291 | 49.973±33.565 | 65.230±44.827 | 54.814±43.686 |
| | WBC
(103/mm3) | 7.698±2.523 | 8.813±3.548 | 8.857±4.250 | 8.220±3.599 |
| | Body temperature
(˚C) | 36.327±2.051 | 36.286±2.581 | 36.468±2.291 | 36.171±3.179 |
| PCN | creatinine
(mg/dl) | 3.673±3.003 | 3.196±2.648 | 3.233±2.460 | 2.882±2.209 |
| | azotemia (mg/dl) | 102.540±69.099 | 100.383±67.741 | 104.50±67.891 | 100.539±64.899 |
| | WBC
(103/mm3) | 11.078±9.228 | 10.7498±7.174 | 10.576±8.745 | 9.783±6.061 |
| | Body temperature
(˚C) | 36.479±0.290 | 36.467±0.244 | 36.467±0.177 | 36.463±0.178 |
Consistently, patients with DJ stents reported
values on the VAS scale, which oscillated between moderate pain and
severe pain. By contrast, a greater number of patients with PCN
reported not complaining of any pain. Furthermore, quality of life
(QoL) was assessed weekly after the surgical procedure for a
6-month follow-up period. Patients were requested to fill out the
‘Tube symptoms’ questionnaire' which included six questions
regarding pain, analgesics use, hematuria, urinary discomfort,
discomfort associated with movement and discomfort associated with
personal hygiene. Answers to these questions were based on a
four-point rating scale; a higher score is associated with worse
symptoms. At each measurement, the DJS group more frequently
reported pain, analgesics use and presence of hematuria.
Furthermore, the severity of these symptoms increased over time in
the DJS group, while patients with PCN showed greater adaptation to
the surgical device, which did not impede their personal hygiene or
carrying out their daily activities.
The medial length to defervescence was 2.06 days,
while the median length of white blood count (WBC) normalization
was 1 day. After discharge, none of the patients undergoing DJS
placement required readmission to the hospital; conversely, 10
patients (6,4%) required readmission to the hospital due to PCN
dislocation. More patients with DJS presented to the emergency room
with complaints related to their procedure compared with patients
with PCN, mostly due to flank pain and dysuria. The post-drainage
complication rate was not similar, being higher in PCN group. The
majority of patients in both groups underwent ureteroscopy as the
definitive treatment. The length of time between the urgent
drainage and the definitive treatment was higher in the DJS group
compared with the PCN group; this meant that a greater number of
patients with DJS were admitted to the emergency room due to
infection, malfunction of the stent or calcification of the same in
both the bladder and the kidney (with the consequent need for a
double operation, percutaneous nephrolithotomy and laser
cysto-lithotripsy, to remove the stent in those patients).
Inferential statistical analysis
A Chi-square test was used to evaluate the
difference in the incidence of complications according to sex and
to the type of intervention. Moreover, 2-way ANOVA, considering the
time (that is, pre-intervention, 2, 3, and 4 days after the
intervention) as within factor and the groups as between factor,
was implemented separately for the creatinine, azotemia, WBC and
body temperature values to assess differences between the PCN and
DJS groups. Multiple comparisons were performed through t-tests
comparing the values pre-operation and the values at 2, 3 and 4
days after the intervention for each group. Moreover, independent
samples t-tests were computed to identify differences between the
two groups. Importantly, the multiple comparisons results were
Bonferroni corrected. Finally, in order to assess a possible effect
of the age on the variations of the creatinine, azotemia, WBC and
body temperature for the two groups considered, a MANCOVA was
performed, considering the age as a covariate. Finally, an
independent sample t-test was performed between the hospitalization
time of the two groups; differences between the two sides were also
investigated with a preliminary analysis, not proving any
difference between the two sides; for this reason, the side of the
intervention was not considered as a regressor for the ML
algorithms.
Machine learning analysis
A Support Vector Regressor was employed to estimate
the values of the creatinine and azotemia until to 4 days after the
interventions for both the PCN and DJS groups. The input features
were age, creatinine, azotemia, potassium, WBC, body temperature,
flank pain and anti-inflammatory therapy before the intervention.
Specifically, three different models were developed by splitting
the study sample in three classes of age: patients with age <55
years, patients between 55-70 years-old, and patients aged >70
years. Moreover, a Support Vector Machine classifier was fed using
the same regressors to estimate whether the hospitalization time of
the patients is lower or higher than 3 days. Importantly, the input
features were normalized (z-score) and, in order to assess the
generalizability of the models' performance, a nested
cross-validation (nCV) was implemented. In the nCV approach, the
dataset is partitioned into numerous folds. The model is then
trained repeatedly and in a nested manner, excluding 1-fold at a
time, on the remaining data. In contrast to the outer loop, which
assesses the model's performance over iterations (test), the inner
loop is responsible for identifying the ideal hyperparameter
(validation). In the present study, the 5-fold CV was utilized and,
in addition, a portion of the study sample (10%) was used as test
set to further confirm the generalization performance of the models
and to reduce overfitting effects. The data analysis was conducted
using the MATLAB 2023b software (MathWorks, Inc.).
Results
Inferential statistical results
The chi-square test showed a not significant
difference in the incidence of complications according to sex
(Chi-squared=0.692; P=0.4054), whereas a significant difference was
assessed regarding the incidence of the complications according to
the type of intervention (Chi-squared=13.000; P=3x10-4),
highlighting a higher incidence of complications in the nephrostomy
group. Concerning the creatinine, the ANOVA showed significant
differences for the groups [F(1,370)=42.39, P<0.0001], the time
[F(1.203,445,3)=23.52; P<0.0001] and their interaction
[F(3,1110)=19.26, P<0.0001]. Regarding the azotemia no
significant differences were assessed for the groups
[F(1,370)=0.5853, P=0.4447], for the time [F(1,369.7)=0.3574,
P=0.5503], and for their interaction [F(3,1109)=1.116, P=0.3415].
As far as it concerns the WBC, significant differences were
identified for the groups [F(1,370)=14.42, P=0.0002], for the time
[F(1.716,630)=4.383, P=0.173] and for their interaction
[F(3,1101)=7.310, P<0.0001]. Regarding the body temperature, no
significant differences were assessed for the groups
[F(1,370)=0.7451, P=0.3886], time [F(1.375,507.8)=1.003, P=0.3418]
and for their interaction [F(3,1108)=0.2213, P=0.8817]. The paired
t-tests demonstrated a statistically significant improvement of the
patients' condition after the intervention for both nephrostomy and
stenting, as reported in Table
III. Moreover, the independent samples t-test showed a
significant difference between the variations of the several
metrics considered when comparing the nephrostomy and the DJS
operations, highlighting a higher effect of the nephrostomy
(Table IV). The MANCOVA showed a
significant interaction between the group and the age of the
participant regarding the creatinine (P=0.0021) and the azotemia
(P=0.0089), whereas no significant interaction was found for the
WBC (P=0.0611) and for the body temperature (P=0.1354). The t-test
between PCN and DJS demonstrated a greater hospitalization time for
the PCN group with respect to the DJS (t-stat=7.3075, d.f.=394,
P<0.0001).
 | Table IIIResults of the comparison between the
values of the creatinine, azotemia, WBC count, and body temperature
before and until four days after the intervention. The comparisons
have been performed for both nephrostomy and stenting. |
Table III
Results of the comparison between the
values of the creatinine, azotemia, WBC count, and body temperature
before and until four days after the intervention. The comparisons
have been performed for both nephrostomy and stenting.
| | Day 2 | Day 3 | Day 4 |
|---|
| Intervention | Metric | T-stat | P-value | T-stat | P-value | T-stat | P-value |
|---|
| Nephrostomy | creatinine | 4.778 |
4.088x10-6 | 6.468 |
1.244x10-9 | 7.41 |
7.812x10-12 |
| | azotemia | 3.031 | 0.003 | 4.711 |
5.49x10-6 | 5.808 |
3.537x10-8 |
| | WBC count | 0.147 | 0.883 | 1.004 | 0.316 | 1.952 | 0.053 |
| | Body
temperature | 1.077 | 0.282 | 1.203 | 0.231 | 1.263 | 0.208 |
| Stenting | creatinine | 0.313 |
0.754∙10-7 | 0.454 | 0.650 | 0.330 | 0.7411 |
| | azotemia | 5.353 | 2.201 | 6.225 |
2.470x10-9 | 5.991 |
8.620x10-9 |
| | WBC count | -4.594 |
7.396x10-6 | -4.523 |
1.007x10-5 | -3.112 | 0.002 |
| | Body
temperature | -0.947 | 0.344 | -0.903 | 0.367 | 0.074 | 0.941 |
 | Table IVResults of the comparison between the
variations of the values of the creatinine, azotemia, WBC count,
and body temperature in response to nephrostomy and stenting until
four days after the intervention. |
Table IV
Results of the comparison between the
variations of the values of the creatinine, azotemia, WBC count,
and body temperature in response to nephrostomy and stenting until
four days after the intervention.
| | Day 2 | Day 3 | Day 4 |
|---|
| Metric | T-stat | P-value | T-stat | P-value | T-stat | P-value |
|---|
| Creatinine | 3.767 | 0.003 | 3.968 |
2.17x10-5 | 4.091 |
6.696x10-7 |
| Azotemia | 0.516 | 0.606 | 1.947 | 0.052 | 2.508 | 0.012 |
| WBC count | 2.361 | 0.018 | 3.093 | 0.002 | 3.39 |
7.748x10-4 |
| Body
temperature | 1.44 | 0.151 | 1.508 | 0.132 | 0.714 | 0.475 |
Machine learning results
The prediction results of the values of creatinine
and azotemia until day 4 are reported in Table V. Specifically, the correlation
coefficient between the measured value of the metrics considered
and the predicted one is reported. The results reported in Table V refers to the test set. In fact, in
the present study, together with a 5-fold cross validation, the 10%
of the study sample was used as test set to further investigate the
generalization performance of the models and to reduce the
overfitting. Concerning the prediction of the hospitalization time,
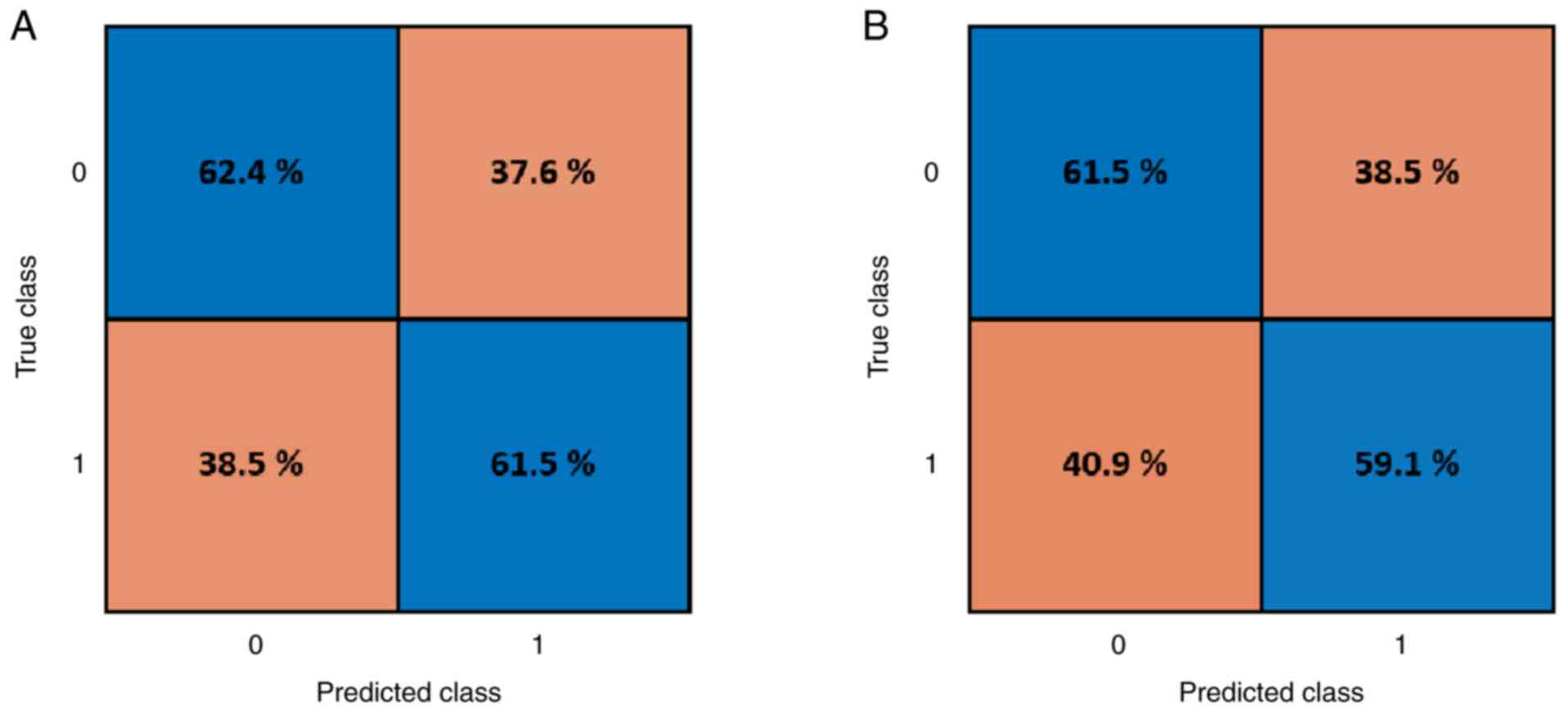
the results of the two-class classification (that is,
hospitalization time lower or higher than 3 days) for both DJS and
PCN are reported in Fig. 2.
Specifically, the confusion matrices associated to the test set are
reported in Fig. 2, demonstrating
the correct classification in the main diagonal (blue background)
and the wrong classification in the secondary diagonal (orange
background). The test accuracy of the prediction was 61.9% for DJS
and 60.2% for PCN, whereas the validation accuracy of the
prediction was 62.4% for DJS and 61.6% for PCN. These results
demonstrate the feasibility of predicting the hospitalization time
for the patients based on their pre-drained condition. Although the
results are preliminary and the accuracies are not high, this
approach could help the surgeon choose the right kind of
intervention for each patient.
 | Table VResults of the Support Vector
Regressor based prediction of the values of creatinine and azotemia
until day 4 relying on age, creatinine, azotemia, potassium, white
blood cell count, body temperature, flank pain, and
anti-inflammatory therapy before the intervention, for both
nephrostomy and stenting. In the table, the correlation
coefficients obtained between the measured and predicted values for
each metric considered. |
Table V
Results of the Support Vector
Regressor based prediction of the values of creatinine and azotemia
until day 4 relying on age, creatinine, azotemia, potassium, white
blood cell count, body temperature, flank pain, and
anti-inflammatory therapy before the intervention, for both
nephrostomy and stenting. In the table, the correlation
coefficients obtained between the measured and predicted values for
each metric considered.
| Age class | Metric | Intervention | Day 2 | Day 3 | Day 4 |
|---|
| <55 | Creatinine | Stenting | 0.89 | 0.92 | 0.94 |
| | Creatinine | Nephrostomy | 0.69 | 0.68 | 0.72 |
| | Azotemia | Stenting | 0.76 | 0.63 | 0.63 |
| | Azotemia | Nephrostomy | 0.82 | 0.82 | 0.81 |
| >55 and
<70 | Creatinine | Stenting | 0.51 | 0.35 | 0.36 |
| | Creatinine | Nephrostomy | 0.66 | 0.65 | 0.41 |
| | Azotemia | Stenting | 0.51 | 0.69 | 0.33 |
| | Azotemia | Nephrostomy | 0.77 | 0.64 | 0.53 |
| >70 | Creatinine | Stenting | 0.87 | 0.85 | 0.90 |
| | Creatinine | Nephrostomy | 0.52 | 0.50 | 0.48 |
| | Azotemia | Stenting | 0.69 | 0.65 | 0.37 |
| | Azotemia | Nephrostomy | 0.66 | 0.58 | 0.49 |
Discussion
The incidence of ureteral obstruction has risen in
last decades for causes that differ depending on the age group of
the patients: Ureteral stones in young and middle age (6) while, for the elderly, advanced
urological malignant diseases (such as bladder cancer which
involves ureteral orifice or ureteral neoplasms) or non-urological
abdominal cancer with compression of the ureter are more common
(7). Those patients require
emergency treatment in order to avoid different adverse events such
as pain unresponsive to medical therapy, urinary infections, acute
renal failure, urosepsis and even death (1). Despite the commonness of these
situations, only few studies compared renal drainage methods
(8-12).
The placement of PCN or DJS represents the mainstream surgical
drainage method for temporary relief of obstruction (13). However, the dilemma of choosing
between these two drainage methods remains extremely relevant and
current in urological daily practice; this is where the idea of our
research was born. In the present study, all patients were
potential candidates for both procedures and they showed similar
characteristics. The goal of the aforementioned systems is to
obtain ureteral drainage, in order to maintain renal function,
waiting for the resolution surgery. Regarding this, some studies
reported a difference in time to second procedure (9), which was 2-fold longer in DJS patients
compared with those with PCN (probably because a patient with a DJS
is mistakenly considered less debilitated compared with a patient
with a PCN). Furthermore, both PCN and DJS placements have some
complications such as the risk of infection and displacement, as
well as the discomfort of nephrostomy catheter and stent. Moreover,
ureteral stents should be exchanged every 6 to 8 weeks in order to
avoid the risk of encrustation and bacterial colonization (14). Generally, stent placement has a high
success rate and it is minimally traumatic using the natural
ureteral orifice. In addition, it does not require an external
tube, resulting in no effect on the aesthetic appearance of
patients. However, the review of Ramsey et al (15) suggested that retrograde stent
placement leads to increased bacteremia. PCN placement reduces
renal pelvis pressure and the risk of bacteremia (16). It is commonly performed under local
anesthesia by a urologist using ultrasonographic guidance (16) and, in part for this reason,
urologists consider PCN to be superior to DJS (17). Likewise, oncologists were more
likely to recommend PCN as the next step after stent failure in
unilateral obstruction (18). In
another study a more rapid return of serum creatinine to normal
levels with PCN tubes than DJS was also reported (19). Moreover, unstable patients with
larger stones being severely ill should be treated with PCN under
local anesthesia (12). Despite
this, in clinical practice, the proper surgical option is affected
by numerous factors. In recent decades, studies (evaluating the
superiority of one drainage method over the other) reported
inconclusive results, probably due to too small study samples.
Thus, PCN and DJS were compared to understand which of the two was
the best drainage method for resolving urinary tract obstruction.
The Chi-square test showed a not significant difference in the
incidence of complications according to sex (Chi-square=0.692;
P=0.4054), whereas a significant difference was assessed regarding
the incidence of the complications according to the type of
intervention (Chi-square=13.000; P=3x10-4), highlighting
a higher incidence of complications in the nephrostomy group. The
paired t-tests demonstrated a statistically significant improvement
of the patients' condition after the intervention for both
nephrostomy and stenting, as reported in Table I. Moreover, the independent samples
t-test showed a significant difference between the variations of
the several metrics considered (values of the creatinine, azotemia,
WBC count and body temperature) when comparing the nephrostomy and
the stenting operations, highlighting a higher effect of the
nephrostomy, as showed in Table
II. On the other hand, compared with DJS, PCN showed a
relatively higher rate of post-operative complications. Another
aspect that was evaluated is the QoL of patients undergoing DJS
placement or nephrostomy tube. Both surgical methods caused pain or
discomfort to a significant number of patients. Generally, while
the number of patients with PCN complaining of pain remain similar
over time and with an ever-decreasing use of analgesics, more
patients with DJS report of pain, requiring greater and more
frequent use of painkillers (20).
The most troublesome symptoms in the DJS group are irritative
symptoms of the lower urinary tract (10,21),
inflicting ~70% of these patients who require over time a higher
number of emergency room visit due to the unchanged frequency and
severity of the bother symptoms. In distinct opposition, patients
with PCN suffered at first mostly from discomfort during daily
activities and personal hygiene but, over time, they adjusted to
this condition. This result is corroborated by the study of de
Sousa Morais et al (10) and
in other studies which compared PCN drainage vs. DJS in other
clinical scenarios (22,23). Although according to the current
results PCN is superior to DJS for temporary urinary diversion in
terms of renal function preservation (with also an improved QoL for
the patients, as demonstrated by the results of the VAS scale and
of the ‘Tube symptoms' questionnaire’), the choice of treatment
depends on the individual situation. For example, PCN represents
the choice treatment in case of advanced malignancies, after failed
retrograde stent placement (24)
and in patients who might not be able to tolerate general
anesthesia (25). Thus, the
decision on the appropriate method of drainage is multifactorial;
furthermore, a discussion with the patient is extremely important
because the urologist might explain the clinical advantages and the
complications of each procedure, not forgetting what is expected
regarding tube symptoms and their impact on QoL. To quote Dr Louis
R Kavoussi (26), ‘traditionally,
urologists have placed stents because … that's what we do’, but his
experience is that ‘patients are more comfortable with a
nephrostomy than a stent’. The results of the present study support
superior QoL of nephrostomy tube over time, inducing some
urologists to reconsider their choice of renal drainage, especially
in health systems in which definitive treatment might be delayed.
There are several limitations to the present study. Selection bias
may have been introduced through choice of drainage procedure
according to surgeon's preference, with a higher probability of
performing PCN in patients suspected of long-standing obstruction.
Furthermore, as different imaging modalities were used (CT scan
and/or ultrasonography exam), hydronephrosis severity could not be
assessed as a possible confounder. Nevertheless, the authors
consider that the present study has a fundamental strength. To the
best of our knowledge, the current research represents the first
single-center study with the highest number of patients enrolled,
which allows for a more accurate assessment of the problem of
ureteral obstruction.
In conclusion, according to the present results, PCN
is an improved method compared with DJS for management of ureteral
obstruction in terms of renal function preservation, also ensuring
an improved QoL (as demonstrated by the results of the VAS scale
and of the ‘Tube symptoms' questionnaire’). Moreover, patients with
PCN have a higher rate of postoperative complications. Then,
concerning the prediction of the hospitalization time (according to
the two-class classification: hospitalization time lower or higher
than 3 days), the test accuracy of the prediction was 61.9% for DJS
and 60.2 for PCN. These results demonstrate the feasibility of
predicting the hospitalization time for the patients based on their
pre-drained condition. Although the results are preliminary and the
accuracies are not high, this approach could help the surgeon
choose the right kind of intervention for each patient. In fact,
predicting hospitalization time is directly related to post-surgery
complications, which can significantly impact patient outcomes and
healthcare resource management. To improve the accuracies obtained,
it could be possible to include more regressors for the machineries
(for example, detailed patient demographics, comorbidities, lab
results, imaging findings and intraoperative details). Furthermore,
increasing the sample size can enable models to learn improved
patterns and generalize well to unseen data. Additionally,
increasing the sample size would allow to employ more sophisticated
ML algorithms or ensemble methods that can capture more complex
patterns in the data.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
RB was the major contributor in writing the
manuscript. RB and GM performed the DJS placement and nephrostomy
tube. DP and EB performed the statistical analysis of the data. RC,
VF and RDA performed the data collection. RB and GM confirm the
authenticity of all the raw data. RS, UDM, OI, UP and MB
interpreted the patient data regarding urological disease. All
authors read and approved the final version of the manuscript.
Ethics approval and consent to
participate
The present study was conducted according to the
guidelines of the Declaration of Helsinki. The present study is
part of the checks that patients routinely carry out as part of
pre-operative screening programs when they enter the emergency room
and is not a clinical study. The data presented in this manuscript
were produced by the Umberto I Hospital of Nocera Inferiore,
belonging to the ASL Salerno, as part of the routine emergency
medicine program for the monitoring of patients referred to the
emergency room, according to good practices laboratory
municipalities. No further sampling was performed for the analyses
reported. For this reason, the opinion of the Ethics Committee was
not necessary as it is not a clinical study or a pharmacological
treatment. Patients had already been informed by written
communication that these analyses were part of normal emergency
medicine evaluation practice. Patient data has been processed in
accordance with current privacy protection laws and in accordance
with the procedures of the General Data Protection Regulation
(GDPR) n. 2016/679; the patients’ informed consent was acquired for
the processing of their data, both personal and medical.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Use of artificial intelligence tools
During the preparation of this work, artificial
intelligence tools were used to improve the readability and
language of the manuscript or to generate images, and subsequently,
the authors revised and edited the content produced by the
artificial intelligence tools as necessary, taking full
responsibility for the ultimate content of the present
manuscript.
References
|
1
|
Tabib C, Nethala D, Kozel Z and Okeke Z:
Management and treatment options when facing malignant ureteral
obstruction. Int J Urol. 27:591–598. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Yoon JH, Park S, Park S, Park S, Moon KH,
Cheon SH and Kwon T: Renal function is associated with prognosis in
stent-change therapy for malignant ureteral obstruction. Investig
Clin Urol. 59:376–382. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Netsch C, Becker B and Gross AJ:
Management of ureteral obstruction: Value of percutaneous
nephrostomy and ureteral stents. Urologe A. 55:1497–1510.
2016.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
4
|
Hardie EM and Kyles AE: Management of
ureteral obstruction. Vet Clin North Am Small Anim Pract.
34:989–1010. 2004.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Clavien PA, Sanabria JR and Strasberg SM:
Proposed classification of complications of surgery with examples
of utility in cholecystectomy. Surgery. 111:518–526.
1992.PubMed/NCBI
|
|
6
|
Zhang Z, Wang X, Chen D, Peng N, Chen J,
Wang Q, Yang M and Zhang Y: Minimally invasive management of acute
ureteral obstruction and severe infection caused by upper urinary
tract calculi. J Xray Sci Technol. 28:125–135. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kumar A, Mynderse L, Patel K, Grudem M,
Bakkum-Gamez J, Longenbach S, Block MS, Pitot HC, Garovic V, Weroha
SJ and Jatoi A: Ureteral obstruction in cancer patients: A
qualitative study. Psychooncology. 25:605–609. 2016.PubMed/NCBI View
Article : Google Scholar
|
|
8
|
Joshi HB, Adams S, Obadeyi OO and Rao PN:
Nephrostomy tube or ‘JJ’ ureteric stent in ureteric obstruction:
Assessment of patient perspectives using quality-of-life survey and
utility analysis. Eur Urol. 39:695–701. 2001.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mokhmalji H, Braun PM, Martinez Portillo
FJ, Siegsmund M, Alken P and Köhrmann KU: Percutaneous nephrostomy
versus ureteral stents for diversion of hydronephrosis caused by
stones: A prospective, randomized clinical trial. J Urol.
165:1088–1092. 2001.PubMed/NCBI
|
|
10
|
de Sousa Morais N, Pereira JP, Mota P,
Carvalho-Dias E, Torres JN and Lima E: Percutaneous nephrostomy vs
ureteral stent for hydronephrosis secondary to ureteric calculi:
Impact on spontaneous stone passage and health-related quality of
life-a prospective study. Urolithiasis. 47:567–573. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Pearle MS, Pierce HL, Miller GL, Summa JA,
Mutz JM, Petty BA, Roehrborn CG, Kryger JV and Nakada SY: Optimal
method of urgent decompression of the collecting system for
obstruction and infection due to ureteral calculi. J Urol.
160:1260–1264. 1998.PubMed/NCBI
|
|
12
|
Goldsmith ZG, Oredein-McCoy O, Gerber L,
Bañez LL, Sopko DR, Miller MJ, Preminger GM and Lipkin ME: Emergent
ureteric stent vs percutaneous nephrostomy for obstructive
urolithiasis with sepsis: Patterns of use and outcomes from a
15-year experience. BJU Int. 112:E122–E128. 2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Hsu L, Li H, Pucheril D, Hansen M,
Littleton R, Peabody J and Sammon J: Use of percutaneous
nephrostomy and ureteral stenting in management of ureteral
obstruction. World J Nephrol. 5:172–181. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Loughlin KR and Bailey RB Jr: Internal
ureteral stents for conservative management of ureteral calculi
during pregnancy. N Engl J Med. 315:1647–1679. 1986.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ramsey S, Robertson A, Ablett MJ, Meddings
RN, Hollins GW and Little B: Evidence-based drainage of infected
hydronephrosis secondary to ureteric calculi. J Endourol.
24:185–189. 2010.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Xu ZH, Yang YH, Zhou S and Lv JL:
Percutaneous nephrostomy versus retrograde ureteral stent for acute
upper urinary tract obstruction with urosepsis. J Infect Chemother.
27:323–328. 2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Lynch MF, Anson KM and Patel U:
Percutaneous nephrostomy and ureteric stent insertion for acute
renal deobstruction: Consensus-based guidance. Br J Med Surg Urol.
1:120–125. 2008.
|
|
18
|
Hyams ES and Shah O: Malignant extrinsic
ureteral obstruction: A survey of urologists and medical
oncologists regarding treatment patterns and preferences. Urology.
72:51–56. 2008.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Elgammal MA, Abdel-Kader MS, Kurkar A,
Mohammed OA and Hammouda HM: Management of calculus anuria in
children: Experience of 54 cases. J Pediatr Urol. 5:462–465.
2009.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Shoshany O, Erlich T, Golan S, Kleinmann
N, Bensel J, Rosenzweig B, Eisner A, Mor Y, Ramon J, Winkler H and
Lifshitz D: Ureteric stent versus percutaneous nephrostomy for
acute ureteral obstruction-clinical outcome and quality of life: A
bi-center prospective study. BMC Urol. 19(79)2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Dellis A, Joshi HB, Timoney AG and Keeley
FX Jr: Relief of stent related symptoms: Review of engineering and
pharmacological solutions. J Urol. 184:1267–1272. 2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Zhao PT, Hoenig DM, Smith AD and Okeke Z:
A randomized controlled comparison of nephrostomy drainage vs
ureteral stent following percutaneous Nephrolithotomy using the
wisconsin StoneQOL. J Endourol. 30:1275–1284. 2016.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Jiang H, Huang D, Yao S and Liu S:
Improving drainage after percutaneous Nephrolithotomy based on
health-related quality of life: A prospective randomized study. J
Endourol. 31:1131–1138. 2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Lau MW, Temperley DE, Mehta S, Johnson RJ,
Barnard RJ and Clarke NW: Urinary tract obstruction and nephrostomy
drainage in pelvic malignant disease. Br J Urol. 76:565–569.
1995.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Bres-Niewada E: Ureteral obstruction in
pregnancy-the ‘stone mountain’ for the urologist. Cent European J
Urol. 70:101–102. 2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Practice update, comment by Kavoussi LR,
2016: http://www.practiceupdate.com/content/inferior-wisconsin-stoneqol-results-observed-with-ureteral-stent-vs-nephrostomy-drainage-following-percutaneous-nephrolithotomy/47216.
Accessed at 21 July 2018.
|