Introduction
Unilateral massive exudate is usually related with a
malignant or infectious (parapneumonic or tuberculosis) origin.
Subdiaphragmatic diseases, such as hepatic or subdiaphragmatic
abscess, acute and chronic pancreatitis, are rarely noted in
clinical practice, as shown in Table
I (1,2). Herein, we present a patient with
symptoms leading to a misdiagnosis of pleuropneumonia.
 | Table I.Causes of unilateral, massive and
exudative pleural effusions. |
Table I.
Causes of unilateral, massive and
exudative pleural effusions.
| Common causes | Less common
causes | Rare causes |
|---|
| Malignancy | Pulmonary
embolism | Yellow-nail syndrome
(and other lymphatic disorders, lymphangioleiomyomatosis) |
| Parapneumonic
effusions | Rheumatoid arthritis
and other autoimmune pleuritis |
| Tuberculosis | Benign asbestos
effusion | Drugs |
| Pancreatitis | Fungal
infections |
| Post-myocardial
infarction | |
| Post-coronary artery
bypass graft | |
Case report
A 40 year-old man presented with chest and right
shoulder pain, cough, sputum and sweating symptoms, for a period of
1 month. Two weeks earlier, the patient had been examined in the
emergency room due to epigastric pain and abdominal distension. He
had smoked 40 pack-years of cigarettes and consumed 140 ml
alcohol/day for 20 years. The patient complained of delirium-like
symptoms due to alcohol withdrawal. His vital signs were normal.
Expansion of the right hemi-thorax was delayed. Percussion tone was
dull and breath sounds were diminished at the right lung base.
Laboratory analysis showed a high level of
hemoglobin (18.2 g/dl), hematocrit (54.2%) and white blood cells
(12.1×103/ μl). Glucose (190 mg/dl), total bilirubin
(2.34 mg/dl), direct bilirubin (0.3 mg/dl) and lactate
dehydrogenase (691 U/l) levels were also found to be high. Platelet
count (237×103/μl), erythrocyte sedimentation rate (14
mm/h) and the remaining routine biochemical parameters were normal.
Pulmonary function tests revealed a restrictive defect. On the
chest X-ray the right hemi-diaphragm was elevated and the right
costophrenic sinus was obliterated. The right hilus was widened and
heterogeneous opacity was observed on the right inferior zone.
Pleuropneumonia most probably due to the aspiration
was first considered as a possible diagnosis. Alcohol consumption
was restricted, and antibiotics (cefuroxime axetyl 500 mg, p.o.,
BID) were administered. Diazepam and vitamin B6 were also
supplemented in order to control any potential alcohol withdrawal
symptoms. A diabetic diet was recommended to sustain the blood
glucose level within an acceptable range. A few days later the
patient developed severe dyspnea. Common dullness appeared on the
right hemi-thorax. Right parabolic opacity was detected on the
chest X-ray (Fig. 1). Computed
tomography (CT) of the thorax demonstrated massive pleural effusion
on the right hemi-thorax. Thoracentesis and biochemical analysis of
the pleural fluid were performed (Table II). Serosanguineous exudate was
sampled.
 | Table II.Patient biochemical results of the
pleural fluid analysis |
Table II.
Patient biochemical results of the
pleural fluid analysis
| Variable | Serum (U/l) | Pleural fluid
(U/l) | Urine (U/l) | Pleura/serum
ratio |
|---|
| Amylase | 369.0 | 44,900 | 4,751 | >1 |
| Lipase | 465.0 | 173,000 | - | >1 |
| ADA | 8.3 | 11 | - | >1 |
High levels of serum amylase and lipase, and a high
pleura to serum ratio of these enzymes were detected. The urine
amylase level was also very high. Adenosine deaminase (ADA) levels
of serum and pleural fluid were unremarkable ruling out
tuberculosis. Cytopathological examination of the fluid revealed
mesothelial reaction. Pleural biopsy was reported as non-specific
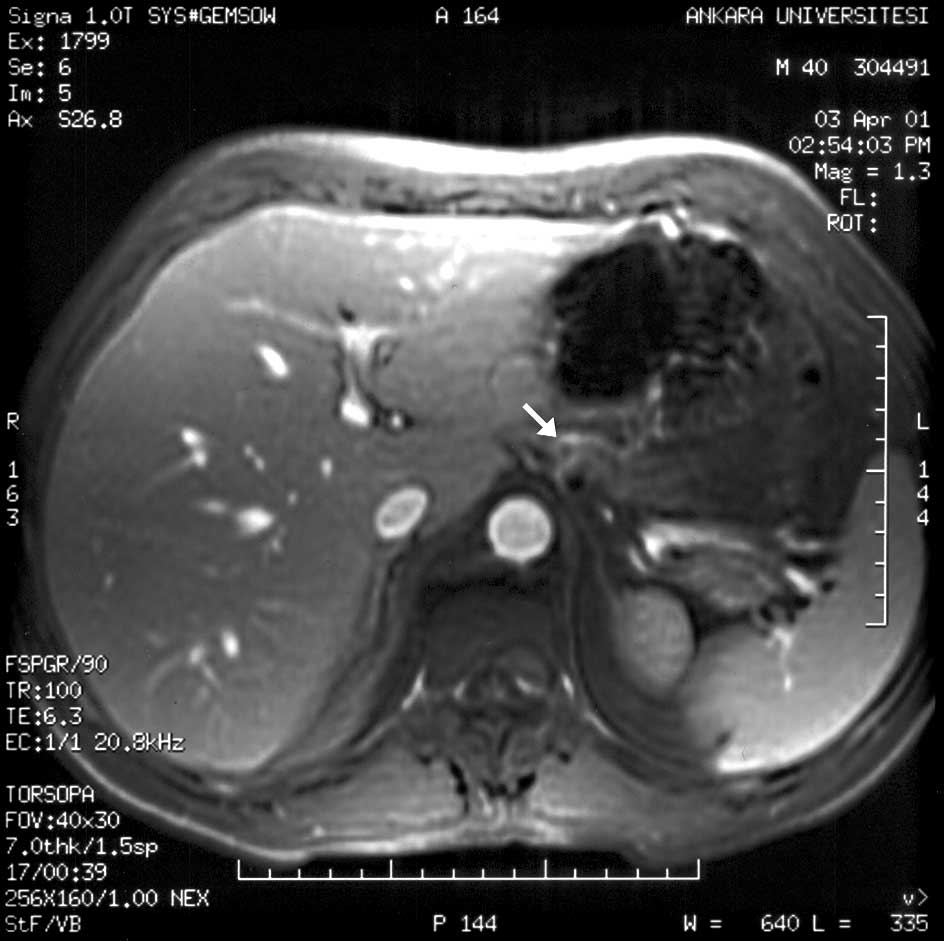
pleuritis. On abdominal CT, a right paragastric lesion was
detected. Endoscopic retrograde cholangiopancreatography was
non-diagnostic. Magnetic resonance imaging (MRI) of the pancreas
revealed a pseudocyst close to the left diaphragmatic crus
(Fig. 2).
Four thousand milliliters of pleural fluid was
drained through an intercostal drain (Pleurocane®)
during a 4-day interval, and chest symptoms were relieved. By
antibiotherapy and intravenous feeding, clinical and radiological
improvement was achieved. Upon follow-up, the patient was in good
health, and his physical examination, laboratory and radiological
findings progressively normalized.
Discussion
Pleural effusion associated with pancreatitis is
usually symptomatic and inflammatory in nature. It is noted in
approximately 3–17% of cases of pancreatitis. Pleural effusion is
uncommon in chronic pancreatitis (<1%) and occurs as a
consequence of a fistula or pseudocyst (3). Chronic pancreatitis occurs most often
in patients with alcoholism (70–80% of all cases). Ethanol is
implicated in the secretion of insoluble pancreatic proteins that
calcify and occlude the pancreatic duct (2,4).
Massive pleural effusion related to pancreatic pseudocyst is very
rare and the incidence remains unknown (5). Recurrent pleural effusions may
develop. Although effusions are generally on the left, they may
also be observed on the right or bilateral side (3,5–8). In
chronic pancreatitis, the cause of pleural effusion is attibuted to
the direct extension of a pseudocyst across the diaphragm. or by
the formation of a fistulous tract between the pancreas and pleural
spaces (9). Although a
pleuropancreatic fistula was not documented, pleural effusion may
have been the complication of this pseudocyst in this case.
Alcoholic pancreatitis is generally the most common
cause of massive pleural fluid. There are several explanations for
the pathogenesis of pancreatic duct disruption. Alcohol ingestion
induces focal acute inflammation on a single branch of the
pancreatic duct system and elicits the protein plug formation. If
transient obstruction occurs with protein plugs, pleural collection
can be observed due to leakage of the pancreatic fluid. From the
retroperitoneal space, it usually moves upward due to the
transdiaphragmatic pressure gradient between the abdominal and
pleural cavities (10).
Pancreatic pseudocysts are localized collections of
pancreatic fluid resulting from disruption of the duct or acinus.
Approximately 25% of patients with chronic pancreatitis develop a
pseudocyst. Patients should be administered intravenous or jejunal
enteral feeding to rest the bowel and minimize pancreatic
stimulation, somatostatin infusion and repeated aspiration. The
cyst resolves in 70% of cases after 2 or 3 weeks. Persistent leaks
to the abdominal cavity require endoscopic stenting of the
pancreatic duct or surgery to drain the site of leakage if it is
proximal or resection if distal (11,12).
In cases with pleuropancreatic fistula, chronic massive and/ or
recurrent pleural effusions may develop (9,12).
Sometimes, chronic pancreatitis may present only with pleural
effusions (5). In such cases, CT
is recommended to show pancreatic parenchymal atrophy, in addition
to dilatation of the pancreatic ducts, calcifications and
pseudocysts (3). The pleural fluid
due to chronic pancreatitis is usually bloody and contains a high
level of amylase, which is predominantly a pancreatic type of
isoenzymes (10). Adenocarcinoma
of the lung and female genital tract, other solid neoplasms and
esophageal perforation or rupture can also be the reason for high
amylase levels in the fluid (9).
The pancreatic pseudocyst of the present case could be detected by
pancreatic MRI. Magnetic resonance cholangiopancreatography,
ultrasonography and ERCP are also advocated to scan
pleuropancreatic fistula (3,13–15).
In chronic pancreatitis, medical treatment is mainly
based on alcohol withdrawal, analgesics and restoration of normal
nutritional status. Pain can be decreased, but sometimes
endoscopic, radiologic or surgical procedures are required. Surgery
is performed in a small group of patients when other therapeutic
approaches fail. Insulin is often given for diabetes, while
exocrine insufficiency is substituted by gastroresistant
microgranule pancreatic extracts (16,17).
Briefly, in the present case, ADA levels in serum or
pleural fluid and microscopic examination for acid fast bacilli or
other bacterias ruled out tuberculosis and empyema. There was no
sign reflecting malignancy on thorax or abdominal CT and MRI. The
patient denied any trauma or accident during the last 2 weeks.
Radiological findings were prominent for pancreatic pseudocyst
formation. High amylase and lipase levels detected in serum and
pleural fluid indicated pancreatic inflammation. In conclusion,
chronic pancreatitis, including a pseudocyst, should be considered
in patients developing massive pleural effusion in case of alcohol
abuse. Although it is extremely less common, chronic pancreatitis
including pseudocyst should be included in the list of differential
diagnosis for massive pleural effusion.
References
|
1.
|
Hooper C, Lee YC and Maskell N; BTS
Pleural Guideline Group: Investigation of a unilateral pleural
effusion in adults: British Thoracic Society Pleural Disease
Guideline 2010. Thorax. 65(Suppl 2): ii4–ii17. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Shan SA: The pleura. Am Rev Respir Dis.
138:184–234. 1988. View Article : Google Scholar
|
|
3.
|
Materne R, Vranckx P, Pauls C, Coche EE,
Deprez P and van Beers BE: Pancreatico-pleural fistula: diagnosis
with magnetic resonance pancreatography. Chest. 117:912–914. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Tierney LM Jr, McPhee SJ and Papadakis MA:
Current Medical Diagnosis and Treatment 2003. 42nd edition. Lange
Medical Books/McGraw-Hill; pp. 6692003
|
|
5.
|
Molinuevo JL, Moitinho E, Font MC, et al:
Massive pleural effusion secondary to pancreatic-pleural fistula as
first manifestation of chronic pancreatitis. Report of three cases.
Med Clin. 109:222–224. 1997.
|
|
6.
|
Kiewiet JJ, Moret M, Blok WL, Gerhards MF
and de Wit LT: Two patients with chronic pancreatitis complicated
by a pancreaticopleural fistula. Case Rep Gastroenterol. 3:36–42.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Vyas S, Gogoi D, Sinha SK, Singh P, Yadav
TD and Khandelwal N: Pancreaticopleural fistula: an unusual
complication of pancreatitis diagnosed with magnetic resonance
cholangiopancreatography. JOP. 10:671–673. 2009.PubMed/NCBI
|
|
8.
|
Reechaipichitkul W, Bowornkitiwong T and
Utchariyaprasit E: Chronic pancreatitis presenting with right
pleural effusion: a case report. J Med Assoc Thai. 93:378–382.
2010.PubMed/NCBI
|
|
9.
|
Iglesias JI, Cobb J, Levey J and Rosiello
RA: Recurrent left pleural effusion in a 44-year-old woman with a
history of alcohol abuse. Chest. 110:547–549. 1996.PubMed/NCBI
|
|
10.
|
Akahane T, Kuriyama S, Matsumoto M, et al:
Pancreatic pleural effusion with a pancreaticopleural fistula
diagnosed by magnetic resonance cholangiopancreatograpy and cured
by somatostatin analogue treatment. Abdom Imaging. 28:92–95. 2003.
View Article : Google Scholar
|
|
11.
|
Bornman C and Beckingham IJ: ABC of
diseases of liver, pancreas, and biliary system. Chronic
pancreatitis. BMJ. 322:660–663. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Bhasin DK, Rana SS, Chandail VS, Nanda M,
Sinha SK and Nagi B: Successful resolution of a mediastinal
pseudocyst and pancreatic pleural effusion by endoscopic
nasopancreatic drainage. JOP. 6:359–364. 2005.PubMed/NCBI
|
|
13.
|
Siwezynski H: Chronic pleural effusion
from the pancreas. Wiad Lek. 51:190–195. 1998.
|
|
14.
|
Kumar A, Upreti L, Bhargava SK and Gupta
S: Sonographic demonstration of a pancreaticopleural fistula. J
Clin Ultrasound. 30:503–505. 2002. View Article : Google Scholar
|
|
15.
|
Safadi BY and Marks JM: Pancreatic-pleural
fistula: the role of ERCP in diagnosis and treatment. Gastrointest
Endosc. 51:213–215. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Buscail L: Diagnosis and management of
chronic pancreatitis. Rev Prat. 52:1561–1566. 2002.
|
|
17.
|
Olakowski M, Mieczkowska-Palacz H,
Olakowska E and Lampe P: Surgical management of pancreaticopleural
fistulas. Acta Chir Belg. 109:735–740. 2009.PubMed/NCBI
|