Introduction
The typical late presentation of pancreatic
adenocarcinoma, its early systemic dissemination and its poor
response to chemoor radiation therapy, render prognosis and chance
of a cure under present management poor. The dearth of conventional
therapeutic options motivates the search for novel
immuno-therapeutic approaches to pancreatic cancer, including the
development of monoclonal antibodies, cytokines, cellular
immunotherapy and vaccines (1).
The risk of developing cancer may be increased by
poorly regulated local inflammatory responses to pathogenic
challenge. Although the etiology of pancreatic adenocarcinoma is
not entirely clear, in vivo and in vitro studies show
that inflammation is important in its carcinogenesis (2). Whereas acute inflammatory responses
may be beneficial to the host, as it eliminates cancer cells, if
this response becomes chronic it may hinder antitumor immune
responses, enhancing tumor growth, angiogenesis, invasion and
metastasis.
Natural CD25+CD4+ regulatory
T-cells (Tregs) in the human peripheral bloodstream (identified by
high CD25 expression and the IL-2 receptor α chain), alongside
transcriptional factor forkhead box P3 (FoxP3) (3), have been implicated in regulating
immune responses affecting tumor growth. Normally, Tregs maintain
self-tolerance by suppressing immune responses against autoantigens
and restore immune homeostasis during chronic inflammatory
disorders (4). Although Tregs may
reduce the risk of inflammation-associated cancer by downregulating
inflammation, it is believed that, in cancer, they mainly function
by suppressing the antitumor immune response. However, under poorly
regulated pro-inflammatory conditions, Tregs fail to inhibit, and
may stimulate, a pro-inflammatory T helper 17 (Th17) response,
driving the pro-carcinogenic process (5).
Tregs, which promote tolerance, and Th17 cells,
which induce inflammation (6),
appear to arise from common naïve CD4+ T precursor
cells. During activation of human precursor CD4+ T
cells, interleukin-6 (IL-6) and transforming growth factor β
(TGF-β) promote differentiation toward Th17 cells, whereas TGF-β
alone promotes differentiation of Tregs and suppresses Th17
(7). Furthermore, IL-23, a
heterodimer produced by dendritic cells (DC) comprising the unique
p19 subunit plus the p40 subunit in common with IL-12, also
contributes to differentiation and maintenance of Th17 cells
(8). Moreover, recent data
indicate late-stage plasticity of a subpopulation of Tregs, which
can be selectively induced to adopt a Th17 phenotype, suggesting
that Tregs may do more to modulate cancer than simply block
constructive anticancer responses (5).
Tregs and Th17 are involved in opposing immune
responses critically involved in modulating inflammation in several
diseases, including cancer. IL-6, TGF-β1, IL-23 and IL-17A are key
contributors to the Th17/Treg balance; the present study
concentrated on these factors.
Materials and methods
Patients
The cohort comprised 62 patients (39 males, 23
females; median age 64.5 years, range 31–80) diagnosed with locally
advanced or metastatic pancreatic adenocarcinoma at Centro
Oncologico Ematologico Subalpino (COES), San Giovanni Battista
Hospital, Turin, Italy, between March 2007 and March 2010. None of
the patients had undergone anticancer treatment and all provided
informed consent prior to entering the study. Study procedures
complied with the Helsinki Declaration. Tumors were classified
according to the International Union Against Cancer (UICC) Staging
System at the start of chemotherapy; Table I presents the clinicopathological
features of the patients. Of the 62 patients, 15 underwent radical
surgery, only entering chemotherapy at disease progression and
seven underwent palliative surgery, entering chemotherapy
immediately afterwards. Four patients received no chemotherapy due
to rapid progression. Protocols were: gemcitabine (GEM, 1250
mg/m2 on days 1 and 8 every 21 days; 28 patients); GEM
(1000 mg/m2 on day 1) plus oxaliplatin (OX, 100
mg/m2 on day 2 every 14 days; 23 patients); bevacizumab
(BEV, 5 mg/kg every 14 days) plus capecitabine (CAPE, 825
mg/m2/b.i.d.) and concomitant radiotherapy (RT, 50.4 Gy
in 28 cycles, following the study protocol; six patients);
5-fluorouracil (5-FU, 500 mg/m2) plus levofolinate
calcium (250 mg/m2 on days 1, 8, and 15 every 28 days;
one patient). After the first restaging, responses (by RECIST
criteria) were: no complete responses, one partial response
(patient with locally advanced carcinoma treated with
chemo-radiotherapy in combination with BEV followed by radical
surgery), 30 stabilizations and 26 disease progressions (clinical
progression in eight cases, not documented radiologically). In two
cases the response was not evaluable: one patient succumbed to
unrelated causes after a single dose of chemotherapy and one
patient discontinued therapy after two cycles due to toxicity and
poor compliance. Follow-up continued until death or May 2010. A
total of 44 patients died and the median survival time was 7.2
months. Seventeen patients survived to the end of the study: with
four being in follow-up and 13 being in chemotherapy. Survival was
34.4% at one year after diagnosis, 11.5% at two years.
 | Table I.Clinicopathological features of the
patients. |
Table I.
Clinicopathological features of the
patients.
| Feature | Group A (n=27) | Group B (n=35) | Total (n=62) |
|---|
| Gender [n (%)] | | | |
| Female | 11 (40.74) | 12 (34.29) | 23 (37.1) |
| Male | 16 (59.26) | 23 (65.71) | 39 (62.9) |
| Age [mean
(median)], in years | 63.81 (66) | 64.69 (62) | 64.30 (64.5) |
| Disease stage at
start of chemotherapy [n (%)] | | | |
| II | 2 (7.41) | 5 (14.29) | 7 (11.29) |
| III | 3 (11.11) | 12 (34.29) | 15 (24.19) |
| IV | 22 (81.48) | 18 (51.43) | 40 (64.52) |
| Surgery [n
(%)] | | | |
| None | 20 (74.07) | 20 (57.14) | 40 (64.52) |
| Palliative | 1 (3.7) | 6 (17.14) | 7 (11.29) |
| Radical | 6 (22.22) | 9 (25.71) | 15 (24.19) |
| Metastases [n
(%)] | | | |
| No | 5 (18.52) | 17 (48.57) | 22 (35.48) |
| Yes | 22 (81.48) | 18 (51.43) | 40 (64.52) |
| Metastatic site [n
(%)] | | | |
| Liver | 13 (59.09) | 7 (38.89) | 20 (50) |
| Peritoneum | 4 (18.18) | 4 (22.22) | 8 (20) |
| Lung | 2 (9.09) | 2 (11.11) | 4 (10) |
| Liver,
peritoneum | 1 (4.55) | 4 (22.22) | 5 (12.5) |
| Liver, lung | 1 (4.55) | 0 (0) | 1 (12.5) |
| Lung,
peritoneum | 1 (4.55) | 1 (5.56) | 2 (5) |
| Chemotherapy [n
(%)] | | | |
| No | 4 (14.81) | 0 (0) | 4 (6.45) |
| Yes | 23 (85.19) | 35 (100) | 58 (93.55) |
| Type of
chemotherapy [n (%)] | | | |
| GEM | 13 (56.52) | 15 (42.86) | 28 (48.28) |
| GEMOX | 9 (39.13) | 14 (40) | 23 (39.66) |
| BEV+CAPE+RT | 0 (0) | 6 (17.14) | 6 (10.34) |
| 5-FU+levofolinate
calcium | 1 (4.35) | 0 (0) | 1 (1.72) |
| Response [n
(%)] | | | |
| Complete
remission (CR) | 0 (0) | 0 (0) | 0 (0) |
| Partial remission
(PR) | 0 (0) | 1 (2.86) | 1 (1.72) |
| Stable disease
(SD) | 8 (34.78) | 22 (62.86) | 30 (51.72) |
| Disease
progression (DP) | 14 (60.87) | 12 (34.29) | 26 (44.83) |
Cell isolation and plasma collection
Peripheral blood was collected from the patients in
heparinized tubes at admission (time 0, prior to chemotherapy) and
at first restaging (after 2–3 months, depending on chemotherapy
regime) in parallel with evaluation of clinical course, and from
the controls (20 age- and gender-matched volunteers). Peripheral
blood mononuclear cells (PBMCs) and plasma were collected at
interface and upper phase, respectively, after centrifugation of
blood over a Ficoll-Hypaque density gradient. Plasma was stored at
−20°C until use.
Flow cytometry
Circulating
CD4+/CD25high/FoxP3+ Tregs were
enumerated by three-color flow cytometry. PBMCs were incubated with
anti-CD4-FITC (Caltag Laboratories, Burlingame, CA, USA) and
anti-CD25-PC5 (Beckman Coulter, Immunotech, France) mAb for 30 min
at 4°C. Subsequent to washing with PBS, PBMCs were fixed and
permeabilized with fixation/permeabilization buffer for 30 min at
4°C, washed twice with permeabilization buffer and stained with
anti-human FoxP3-PE mAb, following the manufacturer’s instructions
(eBioscience, San Diego, CA, USA). Following a 30-min incubation at
4°C, cells were washed and analyzed by flow cytometry in a Coulter
Epics IV Cytometer (Beckman Coulter, Inc, Fullerton, CA, USA)
employing Expo32 Software (Beckman Coulter). Cells were gated on
viable lymphocytes, following standard forward and sideways
scattering parameters. Among cells included in this gate, we
evaluated Treg subpopulations as FoxP3+ within the
CD4+/CD25bright subset. The results are
expressed as percentages of triple-positive cell values, calculated
subtracting the autofluorescence of unstained cells (morphology)
from the fluorescence-intensity of antibody-labeled cells.
Statistical analyses involved ≥30,000 events gated on the
population of interest.
ELISA determination of IL-23, IL-17A,
IL-6 and TGF-β1 plasma levels
IL-23, IL-17A, IL-6 and TGF-β1 plasma concentrations
were determined using commercially available ELISA kits. For
TGF-β1, plasma samples were tested after transient acidification
(reducing pH to 1.5 by adding 1 N HCl for 10 min at room
temperature and neutralizing with 1.2 N NaOH in 0.5 M HEPES). All
evaluations were carried out in duplicate. The lower detection
limits of the assays were: 4 pg/ml for IL-17A (eBioscience), 44.7
pg/ml for IL-23 and 4.61 pg/ml for TGF-β1 (R&D, Minneapolis,
MN, USA) and 7 pg/ml for IL-6 (Orgenium Laboratories-Ani Biotech
Oy, Vantaa, Finland).
Statistics
Patient features were presented using mean and
median for continuous variables and absolute and percentage
frequency for categorical variables. To compare the Treg count and
cytokine levels of patients with those of the healthy donors, we
used the non-parametric Mann-Whitney two-sample statistic.
Correlations among Tregs, IL-23, IL-17A, IL-6 and TGF-β1 were
assessed by Spearman’s correlation coefficient. Overall survival
was defined as the interval from diagnosis to death or last
follow-up. Hazard ratios were estimated using the semi-parametric
Cox model. The Wilcoxon matched-pairs signed-ranks test was used to
compare Treg counts and cytokine levels pre- and post-treatment.
Statistical analysis was carried out with Stata 9.2 (StataCorp LP,
College Station, TX, USA) and SigmaStat 3.1 (Jandel Scientific, San
Rafael, CA, USA].
Results
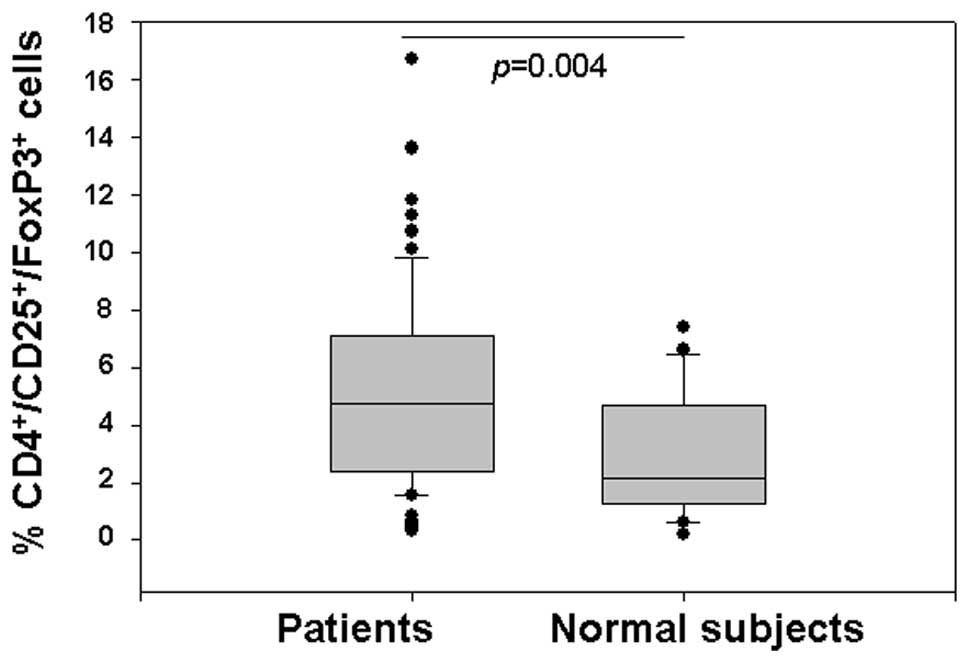
Pre-chemotherapy circulating Treg counts
in pancreatic cancer patients versus healthy donors
Tregs were characterized by flow cytometry, based on
coexpression of CD4/CD25high/FoxP3, in PBMCs from 62
patients with locally advanced or metastatic pancreatic cancer
prior to chemotherapy, and from 20 healthy donors. Patients had a
statistically significantly higher percentage of Tregs than
controls [median (range): 4.72 (0.34–16.7) vs. 2.13 (0.2–7.4),
p=0.004] (Fig. 1).
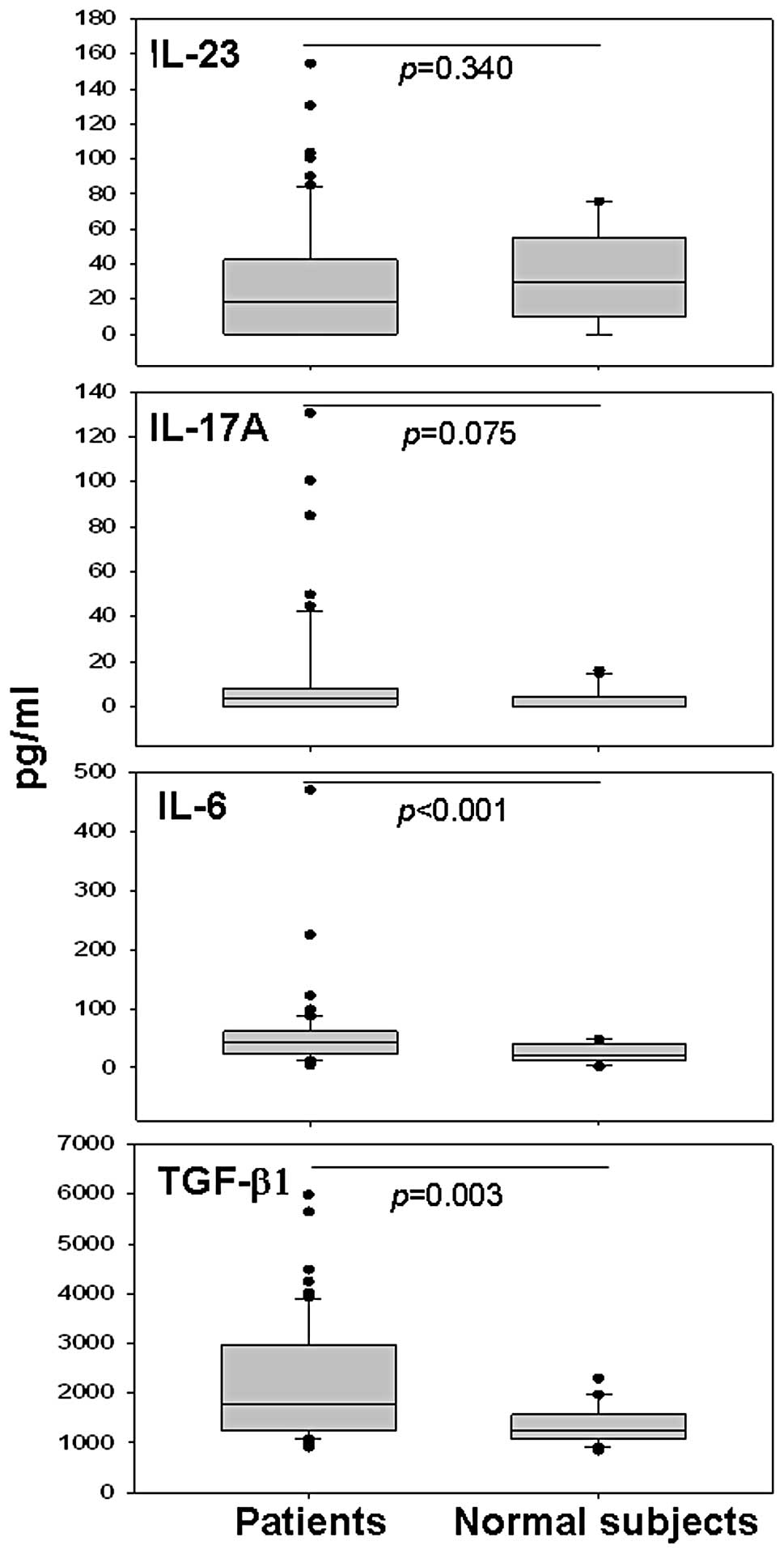
Pre-chemotherapy plasma levels of IL-23,
IL-17A, IL-6 and TGF-β1 in pancreatic cancer patients versus
healthy donors
To investigate whether the tumor microenvironment
perturbs Treg generation or function via soluble factors, for the
first time for pancreatic cancer, we simultaneously analyzed the
profile of all the circulating cytokines involved in these complex
regulatory mechanisms. Patient plasma concentrations of IL-23,
IL-17A, IL-6 and TGF-β1 were measured by ELISA prior to
chemotherapy and compared with corresponding healthy levels. There
was no significant difference between patients and controls for
levels of IL-23 [median (range) pg/ml: 18.72 (0–154.4) vs. 29.54
(0–75.67), p=0.340]. Levels of IL-6 [median (range) pg/ml: 43.42
(4.54–470.58) vs. 20.41 (1.34–48.1), p<0.001] and TGF-β1 [median
(range) pg/ml: 1762.90 (907.60–5986.40) vs. 1247.70
(847.20–2290.00), p=0.003] were higher in cancer patients than
those in the controls (Fig. 2).
The patient-control difference in IL-17A was at the limit of
statistical significance [median (range) pg/ml: 3.60 (0–130.61) vs.
0 (0–15.94), p=0.075].
Correlation among Tregs, IL-23, IL-17A,
IL-6 and TGF-β1
To assess any correlation between Tregs and
cytokines, we looked at the relationship between pre-chemotherapy
Treg counts and the plasma concentrations of IL-23, IL-17A, IL-6
and TGF-β1. There was no correlation between Treg counts and levels
of IL-23, IL-17A, IL-6 or TGF-β1 (r=0.128, p=0.322; r=0.099,
p=0.444; r=−0.066, p=0.609; r=0.072, p=0.578, respectively).
Concerning relationships among cytokines, there was no correlation
between IL-23 and IL-6 levels (r= −0.031, p=0.809) nor between
IL-23 and TGF-β1 (r=0.232, p=0.070), IL-17A and IL-6 (r=0.242,
p=0.058), IL-17A and TGF-β1 (r=0.211, p=0.099) nor IL-6 and TGF-β1
(r=0.023, p=0.856). However, there was a statistically-significant
positive correlation between IL-23 and IL-17A (r=0.261,
p=0.041).
Correlation between disease stage, Treg
count and levels of plasma IL-23, IL-17A, IL-6 and TGF-β1
To clarify the clinical significance of these
findings in locally advanced or metastatic pancreatic cancer,
pre-chemotherapy levels of circulating Tregs and cytokines were
compared between patients categorized as being at stages II/III
(n=22) and stage IV (n=40). Levels of peripheral Tregs did not
differ significantly between early (II/III) and late (IV) stage
disease [median (range) %: 5.13 (0.41–16.7) vs. 3.86 (0.34–13.60),
p=0.162]. Furthermore, circulating levels of IL-23, IL-17A or
TGF-β1 did not differ significantly between early and late stage
disease [median (range] IL-23 pg/ml: 15.44 (0–130.61) vs. 18.72
(0–154.40), p=0.881; median (range) IL-17A pg/ml: 0.40 (0–130.61)
vs. 4.35 (0–49.76), p=0.465; median (range) TGF-β1 pg/ml: 1580.80
(943.60–5643.50) vs. 1842.30 (907.60–5986.40), p=0.431].
Conversely, early-stage patients had significantly lower median
levels of IL-6 vs. late-stage patients [median (range) pg/ml: 23.72
(10.68–225.07) vs. 52.61 (4.54–470.58), p=0.008].
Overall survival
The Cox model, adjusting for age, radical surgery,
metastasis and gender, showed that the Treg counts, IL-23, and IL-6
plasma levels were not prognostic for overall survival (p=0.75,
p=0.133, p=0.246, respectively). However, IL-17A, and especially
TGF-β1, were significantly associated with increased risk of poor
prognosis (p=0.050 and p=0.001, respectively) (Table II).
 | Table II.Hazard ratio estimated by Cox
model. |
Table II.
Hazard ratio estimated by Cox
model.
| Variables | Hazard
ratioa | 95% CI | P-value |
|---|
| Tregs | 1.015 | 0.320–1.110 | 0.75 |
| IL-23 | 1.007 | 0.998–1.015 | 0.133 |
| IL-17A | 1.019 | 0.998–1.040 | 0.050 |
| IL-6 | 1.002 | 0.998–1.007 | 0.246 |
| TGF-β1 | 1.050 | 1.021–1.079 | 0.001 |
Effect of different treatment protocols
on the percentage of Tregs and plasma levels of IL-23, IL-17A, IL-6
and TGF-β1
Percentages of circulating Tregs pre- (Time 0) and
post-chemotherapy were analyzed comparatively at first restaging
(Time 1) in 15 patients treated with GEM, 14 with GEMOX and 6
treated with BEV+CAPE+RT. As Table
III shows, following the stratification of patients by
treatment protocol, there was no significant pre- or post-treatment
difference in the percentages of peripheral Tregs in those who
received GEMOX and BEV+CAPE+RT treatment. However, those receiving
GEM alone showed a statistically significant reduction in Tregs
(p=0.021).
 | Table III.Treg and plasma levels of IL-23,
IL-17A, IL-6 and TGF-β1 pre- and post-treatment. |
Table III.
Treg and plasma levels of IL-23,
IL-17A, IL-6 and TGF-β1 pre- and post-treatment.
| Chemotherapy | % Trega | IL-23 | IL-17A | IL-6 | TGF-β1 |
|---|
|
|
|---|
| median (range) | pg/mlb median (range) |
|---|
| GEM (n=15) | |
| Time 0c | 4.90
(0.87–16.7) | 34.21 (0–85) | 0 (0–85) | 40.70
(10.68–225.07) | 1691.80
(907.6–5643.5) |
| Time 1d | 2.80
(0.33–7.9) | 24.88
(0–120.24) | 0 (0–6.2) | 17.19
(3.24–160.21) | 1469.80
(690.3–3256.3) |
| p-value | 0.021 | 0.842 | 0.161 | 0.001 | 0.100 |
| GEMOX (n=14) | |
| Time 0 | 3.95
(0.57–11.8) | 31.10
(0–103.61) | 0 (0–130.61) | 29.67
(4.54–470.58) | 1502.90
(1127.4–5986.4) |
| Time 1 | 3.6 (0.4–10) | 21.77
(0–80.85) | 0 (0–50.7) | 20.58
(3.24–230.91) |
1855.65(1074.8–3753.3) |
| p-value | 0.638 | 0.059 | 0.046 | 0.088 | 0.683 |
| BEV+CAPE+RT
(n=6) | |
| Time 0 | 5.10
(0.41–11.3) | 4.15 (0–81.89) | 0 (0–2.07) | 24.08
(20.27–37.62) | 1548.85
(1069.4–3269.2) |
| Time 1 | 6.36 (1.5–13) | 23.32
(0–40.43) | 0 (0–0) | 12.70
(4.54–25.60) | 1964.95
(1056–3134.8) |
| p-value | 0.753 | 0.518 | 0.159 | 0.028 | 0.463 |
Pre- and post-therapy plasma levels of IL-23 and
TGF-β1 did not differ significantly with GEM or BEV+CAPE+RT. Only
GEMOX significantly reduced levels of IL-17A (p= 0.046) and IL-23
levels but only at the limit of statistical significance (p=0.059).
IL-6 was significantly reduced by treatment with GEM or BEV+CAPE+RT
(p=0.001, p=0.028, respectively).
Among the patients who passed first restaging after
pharmacological treatment (n=57), 55.6% of those receiving GEM had
stable disease (SD) with median (range) survival 457 (106–2005)
days, whereas 44.4% had disease progression (DP) with median
(range) survival 158.5 (43–601) days; of patients receiving GEMOX,
43.5% showed SD with median (range) survival 375 (112–836) days,
whereas 56.5% had DP, with median (range) survival 118 (73–957)
days; 83.4% of patients receiving BEV+CAPE+RT (n=5) had SD with
median (range) survival 406 (126–770) days and 16.6% (n=1) were in
partial remission (PR) with median survival of 728 days.
Objective tumor response rate, percentage
of Tregs, plasma levels of IL-23, IL-17A, IL-6 and TGF-β1
Overall chemotherapy response rate was 54.3% (31
responders comprising 1 PR and 30 SD, and 26 non-responders with
DP). No statistically significant responder/non-responder
difference was found between pre-treatment Treg percentages and
IL-6 plasma levels [median (range) % Treg: 5.06 (0.34–16.70) vs.
4.10 (1.60–13.60), p=0.773; median (range) IL-6 pg/ml: 40.7
(4.54–225.07) vs. 50.73 (4.54–470.57), p=0.178]. However, IL-23,
IL-17A and TGF-β1 levels were significantly lower in responders
than non-responders [median (range) IL-23 pg/ml: 4.68 (0–103.66)
vs. 33.17 (0–130.61), p=0.030; median (range) IL-17A pg/ml: 0
(0–85) vs. 5.65 (0–130.61), p=0.040; median (range) TGF-β1 pg/ml:
1469.8 (907.6–5643.5) vs. 1912.85 (934.7–5986.4), p=0.032].
Discussion
Tregs are significant in tumor immune evasion,
operating both by blocking generation of immunity to tumor antigens
in the periphery and by neutralizing tumor-infiltrating effector T
cells. They are therefore a significant obstacle to successful
tumor immunotherapy (9). However,
it has recently emerged that, in the tumor microenvironment, Treg
cells can undergo aberrant conversion, producing the
pro-inflammatory IL-17 instead of the immunosuppressive IL-10
(5). Thus, the role of Tregs may
be dual, helping the tumor to survive and expand – Tregs fail to
inhibit, and may contribute to, a Th17-driven pro-carcinogenic
process.
Concurrently, alongside DC activation, local and
systemic alterations of the effector T cell response have been
reported in pancreatic cancer patients (10,11).
However, in pancreatic cancer little is known regarding the effects
of host Treg switch from protecting to suppressing the antitumor
immune response.
This study analyzed the frequency of circulating
Tregs and, for the first time, concomitant levels of IL-23, IL-17A,
IL-6 and TGF-β1, cytokines implicated in the complex mutual
regulation mechanism of Treg/Th17 subpopulations. Patients with
locally advanced or metastatic pancreatic carcinoma were evaluated
prior and subsequent to palliative chemo-therapy. Three-color flow
cytometry was employed for Tregs, and ELISA was carried out to
assess levels of cytokines. The results were compared with those of
matched controls, investigating correlation with clinical
features.
Treg levels were approximately twice the normal
level in pancreatic carcinoma patients, consistent with other
studies reporting increased Treg levels in various cancer patients
(12–15), including pancreatic carcinoma
(16).
According to the physiological-steady-state theory,
Tregs in tumor patients may increase to the highest level
compatible with prolonged tumor-host interaction, allowing the
tumor to escape immune-mediated rejection, while protecting the
host from excessive and indiscriminate immunosuppression. However,
this equilibrium is temporary, and the host eventually surrenders
to the overwhelming tumor burden. Animal studies have demonstrated
that during tumor progression, the initial concomitant immunity is
progressively lost as suppressor CD4+ T cells are
generated (17). In vitro
studies have revealed that suppressor T cells generated in
tumor-draining lymph nodes to abrogate antitumor reactivity possess
the same functional properties and FoxP3 expression levels
as Tregs naturally present in the thymus in order to maintain
self-tolerance (18). Tumor cells
may actively recruit, activate, and expand Tregs by directly or
indirectly presenting self-antigenic peptides for their
recognition. Although they are refractory to T cell receptor
stimulation in vitro, Tregs are able to proliferate in
response to self-antigens in vivo in the presence of IL-2
(19). Moreover, suppressive
cytokines such as IL-10 and TGF-β and chemokines such as CCL22, all
secreted by tumor cells, tumor-infiltrating macrophages, myeloid
suppressor cells and by DC, not only recruit Tregs to tumor sites,
but also favor the conversion of non-suppressive T cells into
suppressive-function Tregs (20).
Since the percentage of Tregs was not correlated
with disease stage in our series of advanced pancreatic carcinoma
patients, it is tempting to speculate that pancreatic tumor-induced
Treg expansion occurs early in tumorigenesis and, once established,
remains constant during the late phase of tumor progression. This
has been reported to occur in ovarian, breast, head and neck
cancers and gastrointestinal carcinomas (16,21–24).
However, due to late presentation and delayed diagnosis, the timing
of Treg expansion in pancreatic cancer is difficult to assess.
Moreover, in contrast to findings in ovarian carcinoma and breast
cancer (21,22), Treg frequency appears not to be
correlated with poor survival in pancreatic carcinoma patients.
However, since our study only investigated patients with locally
advanced or metastatic cancer, the significance of Tregs as
potential prognostic and predictive indicators must be evaluated
prospectively, in a large cohort of patients with operable
tumors.
There is mounting evidence that the composition of
CD4+ cell functional subsets is dynamic and is
controlled by several key cytokine networks, which play pivotal
roles in promoting T regulatory or inflammatory responses upon
microenvironment request. Naturally occurring
CD4+CD25+FoxP3+ suppressor cells
(nTregs), which govern self-tolerance, derive from the thymus, but
CD4+FoxP3+ immunoregulatory cells (iTregs)
related to IL-10 and/or to TGF-β can be induced in the periphery
during immune response.
The conversion of CD4+FoxP3−
to CD4+FoxP3+ Treg occurs at
immune-privileged sites and has been shown in vivo to depend
on TGF-β (25). Tumor cells
themselves, including pancreatic cancer cells (26), and tumor-educated immune cells, can
locally produce abundant TGF-β. It is therefore likely that the
Treg pool in tumor bearers includes newly generated Tregs,
alongside proliferating nTregs. However, it has recently been shown
that TGF-β, under inflammatory conditions, is important in inducing
Treg and IL-17-producing cells (Th17) from T CD4+ naïve
cells, firmly linking these two subsets, which possess opposing
functions (27). A T-cell
activation state, which produces IL-17 as principle effector
cytokine, can be promoted by the combined action of TGF-β and IL-6
(7); IL-23, a cytokine produced by
myeloid DC and activated macrophages, is required for their
expansion and maintenance (8).
We addressed the relationship between Tregs and the
third arm of the CD4+ T-cell effectors, Th17, in
pancreatic cancer patients, simultaneously investigating plasma
levels of IL-23, IL-17A, IL-6 and TGF-β1, the crucial soluble
factors orchestrating the Treg/Th17 balance (28). We found a significant elevation in
the levels TGF-β1 and IL-6 and slightly elevated IL-17A levels in
advanced pancreatic carcinoma patients compared to normal donors;
levels of IL-23 did not differ significantly. Circulating cytokine
levels were not correlated with the percentage of Tregs. However,
the finding that IL-6 levels reflect disease status suggests that
its overexpression may be crucial, not only in determining tumor
growth, invasion, angiogenesis and cachexia, but also in
controlling the Th17/Treg balance in this tumor type. IL-6
participates in differentiation of both T-cell subsets, whereas it
induces Th17 differentiation, acting jointly with TGF-β, and
inhibits TGF-β-induced Treg differentiation (28).
Notably, among the cytokines studied, TGF-β1 and
IL-17A were significantly associated with poor prognosis. In the
case of IL-17A, this is the first report of such an association in
cancer. Whereas, during early tumor formation, TGF-β can function
as a tumor suppressor and tends to prevent tumorigenesis, in
established tumors overproduction of TGF-β is often associated with
poor prognosis (29). TGF-β can
suppress or alter the activation, maturation, and differentiation
of innate and adaptive immune cells, including natural killer (NK)
cells, DC, macrophages, neutrophils, and CD4+ and
CD8+ T effector cells (29), thus promoting an overall
tolerogenic state. However, depending on the cytokine milieu, TGF-β
can also control the ratio between Tregs and Th17 cells in the
tumor microenvironment (30).
Since IL-17A was an independent factor that negatively affected
prognosis in our patients, and since Th17 cells are the sole
cellular source of IL-17 in the human tumor microenvironment, we
may speculate that, at a certain point during tumor development,
Tregs are converted to Th17, stimulated by high levels of IL-6 and
TGF-β1; this contributes to tumor progression in advanced
pancreatic carcinoma. A similar event has been reported in
hepatocellular carcinoma and non-small cell lung carcinoma patients
(31,32), whereas in ovarian carcinoma, high
levels of IL-17 predict improved patient survival (33). This contradiction may be accounted
for by the intensity and nature of IL-17-producing cells and the
other inflammatory and immune cells infiltrated in the tumor
microenvironment. The precise situations in which IL-17 has
pro-tumor or antitumor activity remain to be fully explored.
However, increasing evidence points to the ability of IL-17 to
induce IL-6 and promote chemotaxis of inflammatory cells,
angiogenesis and invasion in cancer (34). Importantly, we found a significant
association between IL-23 and IL-17A plasma concentrations in
support of the hypothesis that, in advanced pancreatic carcinoma,
Th17-polarizing (TGF-β, IL-6) and/or stabilizing (IL-23) cytokines
are important molecular links between tumor-promoting
pro-inflammatory processes and the failure of adaptive immune
surveillance to infiltrate tumors. In chemical carcinogenesis and
transplantable tumor models, and through genetic deletion in mice,
IL-23 has been shown to directly participate in triggering a
pro-inflammatory cytokine cascade and sustaining proliferation
and/or survival of IL-17-producing Th17 cells (35), but reducing CD8+ T-cell
infiltration, activation and function (36). Significant upregulation of IL-23
mRNA has been found in the overwhelming majority of carcinoma
types, as has expression of IL-17 transcript (37) as the result of the tumor-induced
pro-inflammatory environment.
Like IL-12, IL-23 is efficiently produced by
activated macrophages and DC; secretion of these cytokines is
reciprocally regulated and affects the nature and evolution of the
initial innate and immune responses. It was recently reported that
Stat3 signaling, operative in the tumor microenvironment, shifts
inflammation from an antitumor IL-12 program to a tumor-enhancing
IL-23 program, suggesting that preponderant production of IL-23
over IL-12 by antigen-presenting cells in tumor-draining lymph
nodes ultimately skews the differentiation of tumor-specific T
cells, possibly leading to dominance of Treg and Th17 responses
over antitumor Th1 responses (38).
Further investigation is needed, as information
concerning the relevance of the IL-23/IL-17A axis in cancer biology
is scant and contradictory. However, since it has been shown that
IL-18 participates in the differentiation of Th17 cells in synergy
with IL-23 (39), and since
elevated levels of free active IL-18 can play a paradoxically
detrimental role in pancreatic carcinoma (40), it is tempting to hypothesize a
functional link with the present findings, envisaging a new
important mechanism whereby the Th17 effector function is augmented
in cancer.
As curative surgery is only practicable in a small
group of pancreatic carcinoma patients, systemic palliative
chemotherapy remains the standard-of-care for patients with locally
advanced or metastatic cancer. This study employed standard
single-therapy (GEM), two-drug combination therapy (GEMOX), or a
newer therapeutic approach consisting of BEV+CAPE+RT. At the time
of first restaging, GEM administered alone significantly reduced
the percentage of Treg cells, as well as IL-6 levels. By contrast,
GEMOX significantly reduced IL-17A plasma levels and induced
downregulation of IL-23. Combined administration of BEV+CAPE+RT
produced no change in the frequency of Treg, nor IL-23 or IL-17A
levels, but caused a statistically significant decrease in
IL-6.
The apparently contradictory effect of GEM as a
single agent and GEM combined with OX is unsurprising, since
metabolic and biological interactions between drugs are possible
and may result in synergistic, additive, or antagonistic actions.
Elsewhere we report an antagonistic interaction between GEM and
5-FU in some pancreatic cancer cases (41).
Very few data exist regarding the effects of the
chemotherapeutics used here on the levels of circulating Tregs, or
on plasma levels of IL-23, IL-17A, IL-6 and TGF-β1. In colon
carcinoma patients, GEM in association with other
chemotherapeutics, including OX, has been shown to reduce Tregs in
the peripheral blood (42).
However, these analyses were performed at early time points,
whereas ours were after 2–3 months, depending on the chemotherapy
regime; this difference may account for the discrepancy in
findings. GEM has, moreover, been found to cause a significant
decrease in the number of myeloid suppressor cells, one of the
major sources of TGF-β1 in the cancer microenvironment, present in
the spleens of tumor-bearing animals (43). CAPE and/or RT were probably
responsible for the effects observed here, since these two
treatments have been shown to decrease circulating IL-6 and TGF-β1
levels in human and in animal models (44,45),
whereas BEV is a humanized neutralizing monoclonal antibody that
acts against vascular endothelial growth factor A.
Considering the relation of immunological parameters
to clinical response, irrespective of the chemotherapeutic regimen,
responders (PR/SD) had lower IL-23, IL-17A, and TGF-β1 levels than
non-responders, indirectly suggesting that inflammatory status may
play a role in inducing chemotherapy resistance. Potential
limitations of these findings could be the different types of
chemotherapy employed and the limited cohort. However, some
preliminary conclusions may be drawn. GEM as a single agent and the
combined treatment BEV+CAPE+RT reduced plasma levels of IL-6 (a
cytokine that, in association with TGF-β1, induces pro-Th17
development) and produced more favorable effects in terms of
overall survival (BEV+CAPE+RT: 100% of patients with SD, median
overall survival 406 days; GEM: 69% with SD, 31% with DP, median
overall survival 360 days) than did GEMOX (42% with SD, 31% with
DP, median overall survival 186.5 days).
Current theories indicate a role of chronic
inflammation in generating conditions that contribute to malignant
transformation, e.g., the progressive accumulation of genetic
mutations consequent on repeated DNA damage and cell regeneration
in an environment favoring proliferation and neovascularization.
The present data provide novel insight into the significance of the
pro-inflammatory response in human pancreatic carcinoma
progression. We may speculate that, under pathophysiological
conditions, the persistence of a still-unidentified inflammatory
trigger in a particular context, may transform potentially
protective cytokines, such as IL-17A, IL-18 and IL-23 into
procancer cytokines.
These observations support our hypothesis that, in
pancreatic carcinoma, during chronic inflammatory processes linked
to tumor development, Tregs may augment rather than suppress
Th17-mediated immune responses. This pro-inflammatory switch may
play a crucial role in determining tumor progression, and
paradoxically appears to be associated with a less favorable
outcome. We may assume that the tumor microenvironment converts
inflammation, from an IL-12-type program with strong antitumor
effects, due to activation of NK cells and cytotoxic
CD8+ T lymphocytes, to a tumor-promoting IL-23-type
program. It is known that the prevailing production of IL-23
(rather than IL-12) by DC and tumor antigen-stimulated macrophages
in tumor-draining lymph nodes and microenvironment, respectively,
may result in subversion of tumor-specific T-cell differentiation,
with a prevalence of Treg and Th17-type responses over the
antitumor Th1 response (35).
Moreover, IL-23, acting in an autocrine/paracrine manner on DC and
activated macrophages, induces production of IL-1, IL-6 and TNF-α,
responsible for the marked cachexia in patients with advanced
pancreatic carcinoma (36).
Aberrant Tregs have been reported in polyp-ridden
mice. By promoting inflammation and suppressing Th functions, these
provide a dual advantage for tumor growth (46). The discovery of the two opposing
cellular and signal networks (Treg/Th17, IL-23/IL-17), critically
involved in modulating inflammation, induced not only by
autoimmunity or bacterial infection but also by the tumor
microenvironment, has dramatically changed the view of
cell-mediated immune responses. Importantly, and for the first
time, our results show the impact of the Treg/Th17 balance in
pancreatic carcinoma in a new perspective, highlighting the
significance of IL-17A as a potential prognostic and predictive
indicator and showing that chemotherapy, if appropriately
associated with immunotherapy, may amplify antitumor effects.
Due to its control of tumor-promoting inflammatory
and angiogenic pathways and its immunoregulatory effects on tumor
immune surveillance, IL-17A may be an attractive target for tumor
treatment. As the underlying mechanism regulating the Th17/Treg
balance is better understood, it may lead to the development of
effective pancreatic cancer vaccine strategies that circumvent
these tumor-related mechanisms.
Acknowledgements
We thank Dr Manuela Ceccarelli and Dr
Anna Castiglione [Unit of Cancer Epidemiology (CPO-Piemonte),
Azienda Ospedaliera Universitaria San Giovanni Battista, Turin,
Italy] for their assistance with statistical analysis and for
critical reading of the manuscript. This study was supported by
research funds from the Piedmont Regional Government (Regione
Piemonte, Italy) to G.B.
References
|
1
|
Laheru D and Jaffee EM: Immunotherapy for
pancreatic cancer - science driving clinical progress. Nat Rev
Cancer. 5:459–467. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Greer JB and Whitcomb DC: Inflammation and
pancreatic cancer: an evidence-based review. Curr Opin Pharmacol.
9:411–418. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sakaguchi S, Sakaguchi N, Asano M, Itoh M
and Toda M: Immunologic self-tolerance maintained by activated T
cells expressing IL-2 receptor alpha-chains (CD25). Breakdown of a
single mechanism of self-tolerance causes various autoimmune
diseases. J Immunol. 155:1151–1164. 1995.
|
|
4
|
Sakaguchi S and Powrie F: Emerging
challenges in regulatory T cell function and biology. Science.
317:627–629. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Erdman SE, Rao VP, Olipitz W, et al:
Unifying roles for regulatory T cells and inflammation in cancer.
Int J Cancer. 126:1651–1665
|
|
6
|
Chen Z and O’Shea JJ: Th17 cells: a new
fate for differentiating helper T cells. Immunol Res. 41:87–102.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bettelli E, Carrier Y, Gao W, et al:
Reciprocal developmental pathways for the generation of pathogenic
effector TH17 and regulatory T cells. Nature. 441:235–238. 2006.
View Article : Google Scholar
|
|
8
|
Boniface K, Blom B, Liu YJ and de Waal
Malefyt R: From interleukin-23 to T-helper 17 cells: human T-helper
cell differentiation revisited. Immunol Rev. 226:132–146. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ferrone S and Whiteside TL: Tumor
microenvironment and immune escape. Surg Oncol Clin N Am.
16:755–774. viii2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bellone G, Turletti A, Artusio E, et al:
Tumor-associated transforming growth factor-beta and interleukin-10
contribute to a systemic Th2 immune phenotype in pancreatic
carcinoma patients. Am J Pathol. 155:537–547. 1999. View Article : Google Scholar
|
|
11
|
Bellone G, Carbone A, Smirne C, et al:
Cooperative induction of a tolerogenic dendritic cell phenotype by
cytokines secreted by pancreatic carcinoma cells. J Immunol.
177:3448–3460. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wolf AM, Wolf D, Steurer M, Gastl G,
Gunsilius E and Grubeck-Loebenstein B: Increase of regulatory T
cells in the peripheral blood of cancer patients. Clin Cancer Res.
9:606–612. 2003.PubMed/NCBI
|
|
13
|
Ichihara F, Kono K, Takahashi A, Kawaida
H, Sugai H and Fujii H: Increased populations of regulatory T cells
in peripheral blood and tumor-infiltrating lymphocytes in patients
with gastric and esophageal cancers. Clin Cancer Res. 9:4404–4408.
2003.PubMed/NCBI
|
|
14
|
Ormandy LA, Hillemann T, Wedemeyer H,
Manns MP, Greten TF and Korangy F: Increased populations of
regulatory T cells in peripheral blood of patients with
hepatocellular carcinoma. Cancer Res. 65:2457–2464. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Viguier M, Lemaitre F, Verola O, et al:
Foxp3 expressing CD4+CD25(high) regulatory T cells are
overrepresented in human metastatic melanoma lymph nodes and
inhibit the function of infiltrating T cells. J Immunol.
173:1444–1453. 2004.
|
|
16
|
Liyanage UK, Moore TT, Joo HG, et al:
Prevalence of regulatory T cells is increased in peripheral blood
and tumor microenvironment of patients with pancreas or breast
adenocarcinoma. J Immunol. 169:2756–2761. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
North RJ and Bursuker I: Generation and
decay of the immune response to a progressive fibrosarcoma. I.
Ly-1+2- suppressor T cells down-regulate the generation of Ly-1-2+
effector T cells. J Exp Med. 159:1295–1311. 1984.
|
|
18
|
Hiura T, Kagamu H, Miura S, et al: Both
regulatory T cells and antitumor effector T cells are primed in the
same draining lymph nodes during tumor progression. J Immunol.
175:5058–5066. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Walker LS, Chodos A, Eggena M, Dooms H and
Abbas AK: Antigen-dependent proliferation of CD4+
CD25+ regulatory T cells in vivo. J Exp Med.
198:249–258. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yamagiwa S, Gray JD, Hashimoto S and
Horwitz DA: A role for TGF-beta in the generation and expansion of
CD4+CD25+ regulatory T cells from human
peripheral blood. J Immunol. 166:7282–7289. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Curiel TJ, Coukos G, Zou L, et al:
Specific recruitment of regulatory T cells in ovarian carcinoma
fosters immune privilege and predicts reduced survival. Nat Med.
10:942–949. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
22
|
Merlo A, Casalini P, Carcangiu ML, et al:
FOXP3 expression and overall survival in breast cancer. J Clin
Oncol. 27:1746–1752. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Schaefer C, Kim GG, Albers A, Hoermann K,
Myers EN and Whiteside TL: Characteristics of
CD4+CD25+ regulatory T cells in the
peripheral circulation of patients with head and neck cancer. Br J
Cancer. 92:913–920. 2005.
|
|
24
|
Kono K, Kawaida H, Takahashi A, et al:
CD4(+)CD25high regulatory T cells increase with tumor stage in
patients with gastric and esophageal cancers. Cancer Immunol
Immunother. 55:1064–1071. 2006.
|
|
25
|
Stein-Streilein J and Taylor AW: An eye’s
view of T regulatory cells. J Leukoc Biol. 81:593–598. 2007.
|
|
26
|
Bellone G, Smirne C, Mauri FA, et al:
Cytokine expression profile in human pancreatic carcinoma cells and
in surgical specimens: implications for survival. Cancer Immunol
Immunother. 55:684–698. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Lee YK, Mukasa R, Hatton RD and Weaver CT:
Developmental plasticity of Th17 and Treg cells. Curr Opin Immunol.
21:274–280. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kimura A and Kishimoto T: IL-6: regulator
of Treg/Th17 balance. Eur J Immunol. 40:1830–1835. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wrzesinski SH, Wan YY and Flavell RA:
Transforming growth factor-beta and the immune response:
implications for anticancer therapy. Clin Cancer Res. 13:5262–5270.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Veldhoen M, Hocking RJ, Atkins CJ,
Locksley RM and Stockinger B: TGFbeta in the context of an
inflammatory cytokine milieu supports de novo differentiation of
IL-17-producing T cells. Immunity. 24:179–189. 2006. View Article : Google Scholar
|
|
31
|
Zhang JP, Yan J, Xu J, et al: Increased
intratumoral IL-17-producing cells correlate with poor survival in
hepatocellular carcinoma patients. J Hepatol. 50:980–989. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chen X, Wan J, Liu J, et al: Increased
IL-17-producing cells correlate with poor survival and
lymphangiogenesis in NSCLC patients. Lung Cancer. 69:348–354
|
|
33
|
Kryczek I, Banerjee M, Cheng P, et al:
Phenotype, distribution, generation, and functional and clinical
relevance of Th17 cells in the human tumor environments. Blood.
114:1141–1149. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Gaffen SL: An overview of IL-17 function
and signaling. Cytokine. 43:402–407. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Langowski JL, Zhang X, Wu L, et al: IL-23
promotes tumour incidence and growth. Nature. 442:461–465. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Langowski JL, Kastelein RA and Oft M:
Swords into plowshares: IL-23 repurposes tumor immune surveillance.
Trends Immunol. 28:207–212. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Numasaki M, Fukushi J, Ono M, et al:
Interleukin-17 promotes angiogenesis and tumor growth. Blood.
101:2620–2627. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Kortylewski M, Xin H, Kujawski M, et al:
Regulation of the IL-23 and IL-12 balance by Stat3 signaling in the
tumor micro-environment. Cancer Cell. 15:114–123. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Weaver CT, Harrington LE, Mangan PR,
Gavrieli M and Murphy KM: Th17: an effector CD4 T cell lineage with
regulatory T cell ties. Immunity. 24:677–688. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Carbone A, Vizio B, Novarino A, et al:
IL-18 paradox in pancreatic carcinoma: elevated serum levels of
free IL-18 are correlated with poor survival. J Immunother.
32:920–931. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Bellone G, Carbone A, Busso V, et al:
Antagonistic interactions between gemcitabine and 5-fluorouracil in
the human pancreatic carcinoma cell line Capan-2. Cancer Biol Ther.
5:1294–1303. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Correale P, Rotundo MS, Del Vecchio MT, et
al: Regulatory (FoxP3+) T-cell tumor infiltration is a
favorable prognostic factor in advanced colon cancer patients
undergoing chemo or chemoimmunotherapy. J Immunother.
33:435–441
|
|
43
|
Suzuki E, Kapoor V, Jassar AS, Kaiser LR
and Albelda SM: Gemcitabine selectively eliminates splenic
Gr-1+/CD11b+ myeloid suppressor cells in
tumor-bearing animals and enhances antitumor immune activity. Clin
Cancer Res. 11:6713–6721. 2005.PubMed/NCBI
|
|
44
|
Fengming K, Anscher MS, Zhiping X and
Jirtle RL: Elevated circulating transforming growth factor beta1
(TGFβ1) levels decreased after radiotherapy in patients with lung
cancer, cervical cancer and Hodgkin’s disease: a possible tumor
marker. Int J Radiat Oncol Biol Phys. 32:2391995.
|
|
45
|
Fujimoto-Ouchi K, Onuma E, Shirane M, Mori
K and Tanaka Y: Capecitabine improves cancer cachexia and
normalizes IL-6 and PTHrP levels in mouse cancer cachexia models.
Cancer Chemother Pharmacol. 59:807–815. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Gounaris E, Blatner NR, Dennis K, et al:
T-regulatory cells shift from a protective anti-inflammatory to a
cancer-promoting proinflammatory phenotype in polyposis. Cancer
Res. 69:5490–5497. 2009. View Article : Google Scholar : PubMed/NCBI
|