Introduction
The liver is the second most commonly injured organ
following blunt abdominal trauma and associated injuries contribute
significantly to mortality and morbidity (1). Early diagnosis of the nature and
extent of intra-abdominal organ injuries may result in significant
reduction of morbidity and mortality (1). Focused abdominal sonography for
trauma (FAST) is able to sensitively detect free fluid in the
abdomen and pelvis, but its numerous limitations have been
recognized (2–4). The overall sensitivity of emergency
FAST for detection of blunt liver injury was reported to be as low
as 64% (5). When there are
parenchymal injuries of the liver only, with no free fluid, the
sensitivity is even lower (6).
Computed tomography (CT) is the standard diagnostic modality for
stable trauma patients with a suspected abdominal injury (7,8).
However, accurate diagnosis of significant injuries could be
delayed as not all health institutions worldwide have ready access
to CT scans. In addition, a CT scan suite, at times, may not
provide a safe environment for resuscitation and additionally has
limitations for patients who are too unstable for transportation.
The high cost of a CT scan does not permit its widespread use in
screening all patients with blunt abdominal trauma.
In view of the above issues, small-scale studies
carried out in pediatric patients with trauma have revealed varied
threshold admission levels of liver enzymes below which no
clinically significant liver injury was observed (9–13).
Should an association between laboratory tests and liver injuries
exist, early identification of patients with liver injuries could
be achieved. The usefulness of these tests in predicting
intra-abdominal and liver injury in adults has not been intensively
investigated. The present study was undertaken to determine the
accuracy of selected laboratory tests in predicting the presence of
liver injury and its severity following blunt abdominal trauma.
Materials and methods
Study population
The 101st Hospital of the Chinese People’s
Liberation Army is a 1,000-bed hospital in Southeastern China that
provides medical care to approximately 1 million individuals within
the Wuxi metropolitan area and has more than 10,000 visits to the
emergency department annually. It admits an average of 600 serious
trauma cases yearly, of which 96% are blunt injuries.
A review of a retrospective electronic database of
all patients with traumatic blunt abdominal injuries to our
institution over a three-year period (January 2008 to December
2010) was performed. Patients were excluded if they suffered
penetrating injuries, died in the emergency department or if the
required laboratory tests were not performed within 24 h of the
trauma.
Patients were then subdivided into two groups:
patients with and without liver injuries. Liver injury grade was
determined using the organ injury scale (1994 revision) described
by the American Association of Surgery for Trauma (AAST). In this
study, minor liver injuries were classified as AAST Grades I–III,
while major liver injuries were classified as AAST Grades IV–VI.
The information was obtained from either surgery or CT scans. The
results of the CT scans were abstracted from attending radiology
reports if the CT scan was performed at our hospital or from review
of progress notes if the scan was obtained at another institution
prior to transfer.
Test results for aspartate aminotransferase (AST),
alanine aminotransferase (ALT), alkaline phosphatase (ALP), lactate
dehydrogenase (LDH), bilirubin, γ-glutamyl transpeptidase (GGT),
C-reactive protein (CRP) and white blood cell (WBC) levels were
collected. The values were compared with reference ranges for our
institution (Table I). Data
collection forms also included age, gender, trauma mechanisms,
injury severity score (ISS), the AAST grade of liver injury, length
of stay (LoS) in an intensive care unit (ICU), total inpatient LoS
and the eventual outcome.
 | Table I.Reference ranges for laboratory
tests. |
Table I.
Reference ranges for laboratory
tests.
| Laboratory test | Reference range |
|---|
| Aspartate
aminotransferase (AST) | 0–50 U/l |
| Alanine
aminotransferase (ALT) | 0–50 U/l |
| Alkaline phosphatase
(ALP) | 32–135 U/l |
| Bilirubin | 4–25 μmol/l |
| Lactate dehydrogenase
(LDH) | 50–250 U/l |
| γ-glutamyl
transpeptidase (GGT) | 0–50 U/l |
| White blood cell
(WBC) |
4–10×109/l |
| C-reactive protein
(CRP) | 0–5 mg/l |
Median and range were calculated for continuous
variables. The selected laboratory test levels in patients with
liver injuries were compared with patients with abdominal non-liver
injury by plotting the receiver operating characteristic (ROC)
curves for threshold in the presence or absence of liver injury.
Data analysis was performed by comparing the selected laboratory
tests to the threshold using the Chi-square test. All P-values were
2-sided and considered significant at P<0.05. All statistical
operations were performed using SPSS Statistics 13 for Windows
(SPSS Inc, Chicago, IL, USA).
Results
Characteristics of the study sample
During the three-year study period, 182 patients
with blunt abdominal trauma had the relevant laboratory tests
performed and were included in our study. Table II summarizes the general
characteristics of the two groups. In the two groups there was a
preponderance of males. Patients with abdominal non-liver injury
were, on average, older than those with liver injury. The majority
of the patients underwent CT scans. The road traffic accident was
the most common mechanism of injury. Patients with liver injury
tended to be significantly more severely injured than those with
non-liver injury in terms of their median ISS, LoS in ICU and
total. However, more patients (67.4%) with abdominal non-liver
injury underwent exploratory laparotomy than those (41.1%) with
liver injury.
 | Table II.Characteristics of the 182 patients
with blunt abdominal trauma. |
Table II.
Characteristics of the 182 patients
with blunt abdominal trauma.
| Liver injury
(n=90) | Abdominal non-liver
injury (n=92) |
|---|
| Age, median
(range) | 39.0 (8–73) | 45.7 (10–83) |
| Gender, n (%) | | |
| Male | 75 (83.3) | 72 (78.3) |
| Female | 15 (16.7) | 20 (21.7) |
| Mechanism, n (%) | | |
| Road traffic
accident | 57 (63.3) | 58 (63.0) |
| Fall | 21 (23.3) | 16 (17.4) |
| Assault | 7 (7.8) | 12 (13.0) |
| Crush | 5 (5.6) | 6 (6.5) |
| CT scans, n (%) | | |
| Performed | 89 (98.9) | 84 (91.3) |
| Not performed | 1 (1.1) | 8 (8.7) |
| Surgical
intervention, n (%) | | |
| Performed | 37 (41.1) | 62 (67.4) |
| Not performed | 53 (58.9) | 30 (32.6) |
| ISS, median
(range) | 32.0 (9–75) | 24.6 (9–75) |
| ICU LoS, median
(range) | 6.9 (0–30) | 5.0 (1–30) |
| Total LoS, median
(range) | 30.3 (2–215) | 22.1 (2–93) |
| Outcome, n (%) | | |
| Alive | 85 (94.4) | 83 (90.2) |
| Dead | 5 (5.6) | 9 (9.8) |
Patients with liver injuries
The grading of the 90 patients with liver injuries
is shown in Table III. In those
patients with liver injuries, patients were graded according to the
severity of their liver injury as follows: grade I, 23 patients;
grade II, 27 patients; grade III, 23 patients; grade IV, 6
patients; and grade V, 11 patients. There were no patients with
grade VI liver injuries. Grouped according to severity, there were
73 patients (81.1%) with minor (grades I–III) injuries and 17
patients (18.9%) with major (grades IV–V) injuries.
 | Table III.Grading of liver injury for the 90
patients. |
Table III.
Grading of liver injury for the 90
patients.
| Grading of liver
injury | n (%) |
|---|
| Minor liver
injuries | 73 (81.1) |
| I | 23 (25.6) |
| II | 27 (30.0) |
| III | 23 (25.6) |
| Major liver
injuries | 17 (18.9) |
| IV | 6 (6.7) |
| V | 11 (12.2) |
| VI | 0 (0.0) |
Main results
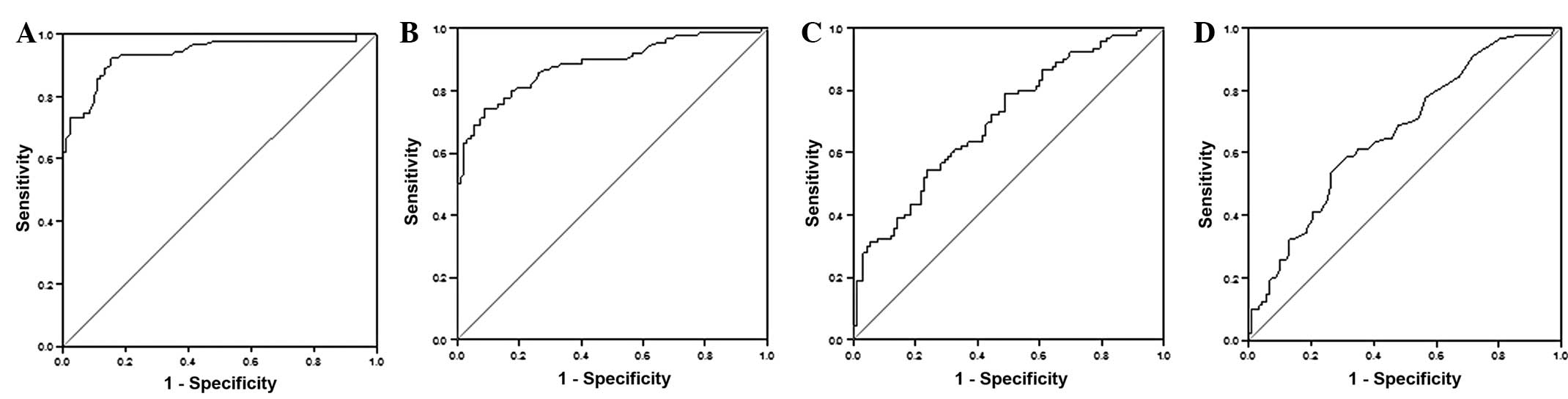
Patients with non-liver injury and grades of liver
injury from I to V were significantly different in regards to
levels of ALT (P<0.001), AST (P<0.001), LDH (P<0.001) and
GGT (P=0.001) (Table IV). Fig. 1 shows the ROC curves generated for
the sensitivity and specificity comparison for the association
between ALT, AST, LDH, GGT levels and the presence of liver injury.
The area under the curve demonstrated that the test was a good
discriminator for identification of liver injury. Using ROC curve
assessment, optimum ALT, AST, LDH, GGT thresholds were determined
to be >57 U/l, 113 U/l, 595 U/l and 50 U/l.
 | Table IV.Relationship between the various
laboratory tests and liver injuries. |
Table IV.
Relationship between the various
laboratory tests and liver injuries.
| Laboratory test | No liver injury | Grade of liver injury
| F-value | P-value |
|---|
| I | II | III | IV | V |
|---|
| ALT | 35± 23 | 96±64 | 306±274 | 263±206 | 628±448 | 681±440 | 39.01 | <0.001 |
| AST | 59±42 | 126±90 | 309±261 | 292±230 | 777±482 | 695±368 | 43.40 | <0.001 |
| LDH | 483±379 | 637±509 | 879±1084 | 775±652 | 2023±1715 | 1581±1011 | 10.27 | <0.001 |
| ALP | 57±39 | 57±36 | 65±27 | 60±28 | 52±15 | 60±31 | 0.28 | 0.923 |
| GGT | 25±37 | 28±35 | 83±138 | 32±36 | 73±62 | 29±14 | 4.12 | 0.001 |
| Bilirubin | 17±10 | 18±13 | 17±11 | 14±7 | 18±6 | 25±24 | 1.20 | 0.310 |
| WBC | 14±6 | 13±7 | 14±6 | 13±5 | 17±6 | 11±2 | 0.97 | 0.439 |
| CRP | 54±80 | 52±84 | 53±87 | 31±32 | 16±29 | 40±67 | 0.63 | 0.681 |
ALT >57 U/l (OR, 66.1; P<0.001) and AST
>113 U/l (OR, 30.6; P<0.001) were significantly associated
with the presence of liver injuries. This was also observed in
patients with LDH >595 U/l (OR, 3.8; P<0.001) and GGT >50
U/l (OR, 3.0; P<0.05) (Table
V).
 | Table V.Relationship between selected
laboratory tests and the presence of liver injuries (part I). |
Table V.
Relationship between selected
laboratory tests and the presence of liver injuries (part I).
| Laboratory test | Liver injury (n) | No liver injury
(n) | OR | 95% CI | P-value |
|---|
| Median ALT
(range) | 309 (13–1500) | 35 (8–118) | 66.1 | 25.33–172.27 | <0.001 |
| ALT ≤57 | 7 | 78 | | | |
| ALT >57 | 83 | 14 | | | |
| Median AST
(range) | 336 (17–1637) | 59 (15–228) | 30.6 | 12.86–72.73 | <0.001 |
| AST ≤113 | 23 | 84 | | | |
| AST >113 | 67 | 8 | | | |
| Median LDH
(range) | 953 (173–5787) | 482 (49–2875) | 3.8 | 2.02–7.17 | <0.001 |
| LDH ≤595 | 41 | 70 | | | |
| LDH >595 | 49 | 22 | | | |
| Median GGT
(range) | 49 (4–551) | 25 (3–319) | 3.0 | 1.25–7.22 | 0.014 |
| GGT ≤50 | 70 | 84 | | | |
| GGT >50 | 20 | 8 | | | |
Further analysis of selected laboratory tests also
revealed that ALT >57 U/l is perhaps most suitable for detecting
hepatic injuries. Its sensitivity (92.2%), specificity (84.8%),
positive predictive value (85.6%) and negative predictive value
(91.8%) are all favorable for its role as a screening tool compared
to the other markers (Table VI).
However, in patients with liver injuries, none of the selected
laboratory tests were related to the severity of the liver injuries
(Table VII).
 | Table VI.Relationship between selected
laboratory tests to presence of liver injuries (part II). |
Table VI.
Relationship between selected
laboratory tests to presence of liver injuries (part II).
| Laboratory
test | Liver injury
(n) | No liver injury
(n) | |
|---|
| ALT >57 | 83 | 14 | Positive predictive
value = 85.6% |
| ALT ≤57 | 7 | 78 | Negative predictive
value = 91.8% |
| Sensitivity =
92.2% | Specificity =
84.8% | |
| AST >113 | 67 | 8 | Positive predictive
value = 89.3% |
| AST ≤113 | 23 | 84 | Negative predictive
value = 78.5% |
| Sensitivity =
74.4% | Specificity =
91.3% | |
| LDH >595 | 49 | 22 | Positive predictive
value = 69.0% |
| LDH ≤595 | 41 | 70 | Negative predictive
value = 63.1% |
| Sensitivity =
54.4% | Specificity =
76.1% | |
| GGT >50 | 20 | 8 | Positive predictive
value = 71.4% |
| GGT ≤50 | 70 | 84 | Negative predictive
value = 54.5% |
| Sensitivity =
22.2% | Specificity =
91.3% | |
 | Table VII.Relationship between selected
laboratory tests and severity of liver injuries. |
Table VII.
Relationship between selected
laboratory tests and severity of liver injuries.
| Laboratory
test | Minor liver
injury | Major liver
injury | OR | 95% CI | P-value |
|---|
| Median ALT
(range) | 227 (13–1123) | 663 (13–1500) | 0.1 | 0.01–0.90 | 0.040 |
| ALT ≤100 | 26 | 1 | | | |
| ALT >100 | 47 | 16 | | | |
| Median AST
(range) | 246 (17–1131) | 724 (28–1636) | 0.2 | 0.02–1.16 | 0.069 |
| AST ≤113 | 22 | 1 | | | |
| AST >113 | 51 | 16 | | | |
| Median LDH
(range) | 770 (173–5787) | 1737
(240–5189) | 0.1 | 0.01–0.41 | 0.005 |
| LDH ≤595 | 40 | 1 | | | |
| LDH >595 | 33 | 16 | | | |
| Median GGT
(range) | 50 (4–551) | 45 (9–148) | 0.8 | 0.15–4.22 | 0.788 |
| GGT ≤100 | 66 | 15 | | | |
| GGT >100 | 7 | 2 | | | |
Discussion
The liver continues to be the second most commonly
injured organ in blunt abdominal trauma (1). Physicians dealing with blunt
abdominal trauma often use biochemical tests and radiographic
imaging to aid in clinical assessment. Outcome of liver trauma has
been shown to be related to several important factors: increased
ISS, worse grading of hepatic injury, advanced age, operative blood
loss and hemodynamic instability on admission (14,15).
Patients with blunt abdominal trauma resulting in
liver injury may present with unstable hemodynamics and obvious
hemoperitoneum. These patients usually do not represent a
diagnostic challenge since the strategy is clear. They generally
receive either prompt abdominal imaging (ultrasound or CT scan) or
laparotomy or both. Usually the more difficult diagnosis is that of
lesser, but still significant, liver injury in the stable patient
with minimal physical findings following blunt abdominal trauma.
Abdominal CT scan has proved to be a valuable diagnostic tool for
evaluating intra-abdominal injury (8). However, it may only be carried out if
available and in patients who are hemodynamically stable.
Furthermore, it is costly, requires radiation exposure, and removes
patients from direct clinical care. Another useful tool for initial
survey is FAST. Yet, FAST is not always available in all healthcare
institutions and one of the major limitations is the technical
expertise of the operator (3,4).
Furthermore, FAST has limited value if the blunt abdominal trauma
does not result in hemoperitoneum, and it may miss nearly one third
of the cases of abdominal injuries when used as the sole diagnostic
tool in evaluating victims of blunt abdominal trauma.
Elevation of the serum liver enzymes AST and ALT is
known to be associated with blunt traumatic liver injury.
Presumably, as these transaminases are present in high
concentrations in hepatocytes, they are released into the
circulation in large quantities following acute traumatic
hepatocellular injury. AST and ALT have been previously reported to
indicate liver injury (12,16).
One previous observational cohort study has reported serum ALT to
be a sensitive diagnostic marker when evaluating harm caused by
blunt hepatic injuries (17).
From our study, the authors preferred ALT to AST as
a screening tool for hepatic injuries due to its associated high
sensitivity, specificity, positive predictive value and negative
predictive value. Although 7 (7.8%) and 23 (25.6%) of the patients
with liver injuries had ALT and AST levels less than their
thresholds in our study, most of them only had grades I and II
injuries. We also found a trend that the more severe the liver
injury of the patients, the higher the liver enzyme levels, but our
study further demonstrates that patients with elevated ALT >100
U/l, AST >113 U/l, LDH >595 U/l and GGT >100 U/l did not
necessarily have major liver injury. Therefore, even where patients
whose liver enzyme levels are at lower levels and liver injury
cannot be completely ruled out, they may still provide clues
concerning liver injury, particularly in patients with high-grade
liver injury.
There are several limitations to this study.
Firstly, it is a retrospective chart review; therefore, data may
not be present or properly recorded on the medical record.
Secondly, the time interval between injury and the procurement of
the blood test could not be standardized. This was predominantly
due to the highly variable timing and location of the accident.
However, we tried to confine our patients to the group having their
blood drawn within 24 h to reduce study bias. Thirdly, as the
threshold for undertaking CT scans varies greatly from one
institution to another, our findings may not be applicable to the
entire population of patients with blunt abdominal trauma.
In conclusion, this study suggests that, in patients
with blunt abdominal trauma, abnormal transaminase levels are
associated with liver injury. Patients with ALT >57 U/l and AST
>113 U/l are strongly associated with liver injury and require
further imaging studies and close management.
Acknowledgements
This research was supported by the
Army Medicine Technology Fund (10MA008).
References
|
1.
|
Piper GL and Peitzman AB: Current
management of hepatic trauma. Surg Clin North Am. 90:7752010.
View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Nural MS, Yardan T, Guven H, et al:
Diagnostic value of ultrasonography in the evaluation of blunt
abdominal trauma. Diagn Interv Radiol. 11:41–44. 2005.PubMed/NCBI
|
|
3.
|
Scalea TM, Rodriguez A, Chiu WC, et al:
Focused assessment with sonography for trauma (FAST): results from
an international consensus conference. J Trauma. 46:466–472. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Chiu WC, Cushing BM, Rodriguez A, et al:
Abdominal injuries without hemoperitoneum: a potential limitation
of focused abdominal sonography for trauma (FAST). J Trauma.
42:617–623. 1997. View Article : Google Scholar
|
|
5.
|
Kirkpatrick AW, Sirois M, Laupland KB, et
al: Prospective evaluation of hand-held focused abdominal
sonography for trauma (FAST) in blunt abdominal trauma. Can J Surg.
48:453–460. 2005.PubMed/NCBI
|
|
6.
|
Richards JR, McGahan JP, Pali MJ, et al:
Sonographic detection of blunt hepatic trauma: hemoperitoneum and
parenchymal patterns of injury. J Trauma. 47:1092–1097. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Richards JR and Derlet RW: Computed
tomography for blunt abdominal trauma in the ED: a prospective
study. Am J Emerg Med. 16:338–342. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Kreimeyer S and Grenacher L: Modern
imaging techniques for liver trauma. Chirurg. 80:8962009.(In
German).
|
|
9.
|
Sola JE, Cheung MC, Yang R, et al:
Pediatric FAST and elevated liver transaminases: an effective
screening tool in blunt abdominal trauma. J Surg Res. 157:103–107.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Capraro AJ, Mooney D and Waltzman ML: The
use of routine laboratory studies as screening tools in pediatric
abdominal trauma. Pediatr Emerg Care. 22:480–484. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Karaduman D, Sarioglu-Buke A, Kilic I, et
al: The role of elevated liver transaminase levels in children with
blunt abdominal trauma. Injury. 34:249–252. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Puranik SR, Hayes JS, Long J, et al: Liver
enzymes as predictors of liver damage due to blunt abdominal trauma
in children. South Med J. 95:203–206. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Karam O, La Scala G, Le Coultre C, et al:
Liver function tests in children with blunt abdominal traumas. Eur
J Pediatr Surg. 17:313–316. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Scollay JM, Beard D, Smith R, et al:
Eleven years of liver trauma: the Scottish experience. World J
Surg. 29:744–749. 2005.PubMed/NCBI
|
|
15.
|
Sikhondze WL, Madiba TE, Naidoo NM, et al:
Predictors of outcome in patients requiring surgery for liver
trauma. Injury. 38:65–70. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Stassen NA, Lukan JK, Carrillo EH, et al:
Examination of the role of abdominal computed tomography in the
evaluation of victims of trauma with increased aspartate
aminotransferase in the era of focused abdominal sonography for
trauma. Surgery. 132:642–646. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Srivastava AR, Kumar S, Agarwal GG, et al:
Blunt abdominal injury: serum ALT-A marker of liver injury and a
guide to assessment of its severity. Injury. 38:1069–1074. 2002.
View Article : Google Scholar : PubMed/NCBI
|