Introduction
The distal femur and proximal tibia which constitute
the knee joint are mainly cancellous bone covered by cartilage.
Once comminuted fracture occurs, compression bone defects and
massive broken bones often follow, usually involving the cartilage
surface. Therefore, post-traumatic osteomyelitis at this region may
easily cause cancellous bone and cartilage surface infection and
necrosis. Purulent fluid flow into the articular cavity through
fracture gaps, which may easily cause bone and joint infection, and
the treatment remains difficult. The current study describes our
experience of 11 cases of metaphyseal osteomyelitis, which involved
4 femurs and 7 tibiae, treated with debridement, bone graft and
sealing of the articular cavity using the synovium.
Patients and methods
Patient data collection
From 1999 to 2003, 11 patients with metaphyseal
osteomyelitis involving the knee joint were treated in our
hospital. Ten of the patients were male and one was female, with a
mean age of 38 years (range, 27–56). Four cases involved the distal
femur (3 cases at the lateral condyle and 1 at the medial condyle),
of which 2 cases resulted in bone nonunions. Seven cases involved
proximal tibiae (4 cases at the lateral plateau and 3 at the medial
plateau) and the bones healed fully. Three of the 11 cases remained
with an implant (1 case with a retrograde locking nail in the femur
and 2 with a lateral plate in the tibia) and an average of 2
surgical procedures (range, 1–4) had been undertaken by patients
prior to administration (Table
I).
 | Table IDemographic and clinical
characteristics of the patients. |
Table I
Demographic and clinical
characteristics of the patients.
| Case | Gender | Age (years) | Infection site | Time interval
(months)a | No. of surgeries
before administration | Follow-up Bacterium
species | (months) | Status of the knee (2
years following surgery) |
|---|
| 1 | M | 56 | LCF | 9 | 3 | MRSA | 82 | Lateral instability,
walks with crutch, ROM: 0–90° |
| 2 | M | 47 | LTP | 12 | 2 | Pseudomonas
aeruginosa | 96 | Normal |
| 3 | M | 27 | LCF | 7 | 2 | Staphylococcus
aureus | 74 | Normal |
| 4 | M | 33 | MCF | 6 | 1 | Staphylococcus
aureus | 80 | Lateral instability,
walks freely, ROM: 0–100° |
| 5 | M | 35 | LCF | 2 | 1 | MRSA | 90 | Stable, ROM:
0–90° |
| 6 | M | 36 | MTP | 5 | 2 | Staphylococcus
aureus | 64 | Stable, ROM:
0–130° |
| 7 | M | 29 | LTP | 7 | 4 | Bacillus cloacae,
Pseudomonas aeruginosa, Serratia marcescens | 73 | Normal |
| 8 | F | 42 | MTP | 12 | 1 | Staphylococcus
aureus | 70 | Normal |
| 9 | M | 34 | MTP | 3 | 1 | Staphylococcus
aureus | 67 | Normal |
| 10 | M | 39 | LTP | 9 | 2 | MRSA | 61 | Stable, valgus 15°,
ROM: 0–90° |
| 11 | M | 43 | LTP | 11 | 2 | Bacillus
cloacae | 58 | Valgus 15°, walks
freely, ROM: 0–100° |
After the patients were admitted, X-ray radiography,
contrast fistulography, MRI, CT and emission computed tomography
(ECT) examination were performed to assess the extent of the foci;
the size and position of the dead bone and the strength and
stability of the involved bone were also assessed. Bacteriological
tests of pus and tissues from the foci were examined routinely
(Table I).
Procedures
According to the lesion sites, a medial or lateral
incision was made, extending 12 cm proximal or distal to the knee
joint. After internal fixation appliances were removed, necrotic
granulation, fibrous cicatrix tissue and sequestra in the involved
bone cavity were cleared thoroughly, and the sclerotic bone was
also mechanically removed, followed by repeated compressive
flushing of the focus and articular cavity with isotonic saline.
Following debridement, the knee joint lateral stability was
evaluated as follows: if the residual bone was able to resist varus
or valgus stress and there was no obvious lateral movement in the
joint, the joint was classified as stable (2 cases involving the
lateral femoral condyle and 5 cases involving the tibia, of which 3
affected the medial plateau and 2 affected the lateral plateau).
Otherwise, the joint was classified as unstable (2 cases involving
the distal femur, of which 1 affected the lateral condyle and the
other the medial condyle, and 2 cases involving the lateral tibial
plateau).
Management of the bone defect and
articular cavity following debridement
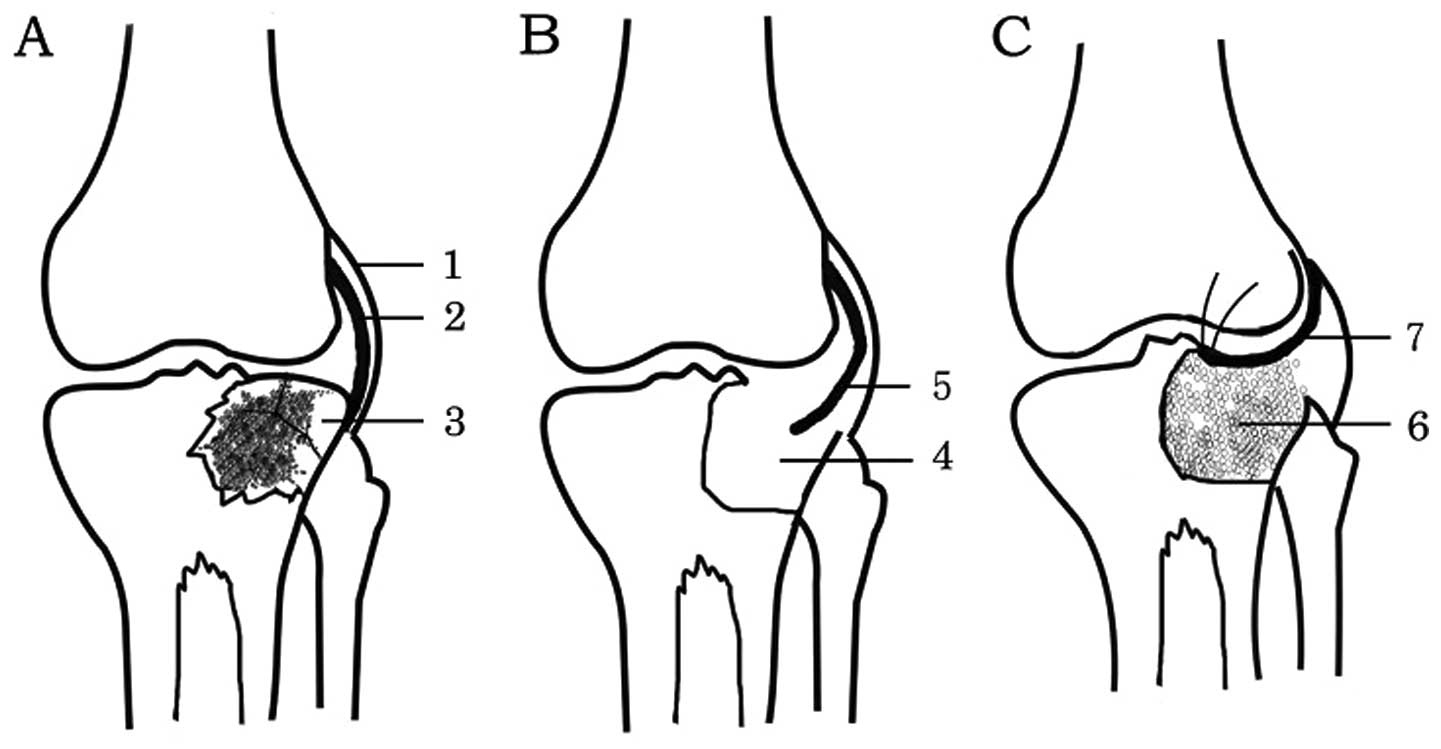
The following techniques were used after
debridement: i) Single-stage bone graft and articular cavity
sealing with synovium: of the 7 cases with stable knees, 4 cases (3
tibial and 1 femural) underwent a bilateral iliac granular
cancellous autograft and the other 3 cases (2 tibial and 1
femoral), due to bone defects >40 ml, underwent a granular
cancellous allograft. Of the 4 patients with unstable knees, 3
received primary bulk cancellous allografts (50, 65 and 110 ml)
from which the cartilage surface had been removed prior to
grafting, and cancellous allograft particles were implanted in
order to bridge the gap between the host bone and allograft, and
were fixed by a strut plate. The adjacent synovium was dissociated
and sutured to seal the synovial articular cavity (Fig. 1). ii) Two-stage bulk allograft: 1
patient retained a femoral retrograde interlocking intramedullary
nail and had an infection which affected the whole lateral condyle
and resulted in the formation of a sequestrum. Infection spread to
the distal medullary cavity and medial condyle along the locking
nail. After debridement, the synovium was sutured to seal the
articular cavity and a vancomycin cement bead was placed in the
bone defect area. After 8 weeks, the vancomycin cement bead was
removed, then, a femoral condyle allograft from which the cartilage
surface had been removed was implanted and fixed using a strut
plate. However, 8 months later, nonunion and displacement of the
femoral condyle was observed in an X-ray, and a dynamic condylar
screw plate was used to strengthen the fixation (Fig. 2). iii) Negative pressure drainage
was used at the articular cavity and bone graft area.
External fixation
Of the 11 cases, 10 underwent fixation for 2 months,
7 with a lateral and medial cast and 3 with a plastic brace. One
patient who received a femoral medial condyle bulk bone graft
underwent fixation by an external fixator with articulation for 6
months due to the uncertainty of plate fixation.
The removal time of the drainage tube was determined
by the final volume of drainage (<5 ml/24 h). The average
drainage times were 8 days for the articular cavity and 16 days for
the bone graft area.
Medication with antibiotics
Appropriate antibiotics were primarily selected
according to the preoperative bacterial culture result and
subsequently selected according to the culture result of the tissue
obtained during surgery. Antibiotics were administered
intravenously for 2–3 weeks from the day of surgery and then orally
for 4 weeks. The patients underwent regular clinical and
radiological evaluation. The average follow-up period was 74 months
(range, 58–96).
Results
Infection recurrence was not observed for 10 of the
11 cases in the joint and bone graft area. In one patient (no. 7 in
Table I), who underwent a lateral
granular cancellous bone allograft in the right tibial plateau,
infection recurred 2 weeks later in the graft area. The patient
underwent debridement and a bilateral ilium bone graft to eliminate
the dead space, and 3 months later, the infection was arrested.
Of the 2 bone nonunion patients, bone union was
achieved in 1 case while the other case (no. 1, in Table I) presented bone nonunion at 11
months after surgery. In this case, a revision surgery was
performed to replace the implant with a dynamic condylar screw
plate and an iliac autograft, and bone union was observed at the
final follow-up. Slight bone reabsorption was observed in the
granular cancellous bone autograft or allograft in the articular
cavity surface, with no sign of bone loss in bulk allograft
patients.
Two of the 11 (18%) cases developed a frontal
misalignment of 15°, but were able to walk without crutches.
Lateral instability of the knee joint was reported in 3 cases, of
which 2 cases walked freely and 1 with crutches. The range of
motion in all cases was >90°. No leg length discrepancy (>2
cm) was observed in the current study (Table I).
Discussion
In metaphyseal osteomyelitis involving the knee
joint, the primary infection usually originates from bone tissue.
Therefore dead bone and the attached cartilage should be thoroughly
removed during debridement, to eliminate the source of infection
(1,2). Precise bone debridement is most
effectively carried out with high speed burs and is performed until
the ‘paprika sign’ (defined as scattered pinpoint bleeding
indicating a good vasculature) is encountered (3).
Since the joint infection is secondary to the bone
infection, after the granulation tissue on the cartilage surface
and the synovial membrane had been removed, the articular cavity is
able to resume normal metabolism and immune function. With the aid
of effective antibiotics, the small quantity of bacteria remaining
following debridement may be eliminated (4). No joint infection recurred in the 11
patients in this study, which demonstrated that the management
option was reasonable and effective.
Bone defects resulting from debridement were
reconstructed using granular cancellous bone grafts instead of
other techniques, including vascularized bone grafting, distraction
osteogenesis, bone graft substitutes and prosthetic devices
(5–8).
Granular cancellous bone grafts have the following
advantages: i) they are easily molded to fill any shape of bone
defect, ii) the blood vessels of the defect cavity wall easily
permeate the bone graft due to the abundant bone intergranular
lattice channels, which may result in higher incorporation and
union rates and, consequently, superior results (9,10).
iii) Antibiotics and immuno-active substances exuded from the blood
vessels are able to distribute well into the bone grafts, resulting
in a strong ability to resist infection (11). Granular cancellous bone grafts also
have disadvantages, for example, particulate bone grafts clearly
have poorer mechanical properties than structural allografts
(12). In 7 of the patients in the
current study, the residual bone after debridement had the ability
to resist lateral stress and therefore the joint was stable, with
no need for stabilizing bone grafts.
Large osseous defects require bone for stability and
are usually managed with a vascularized bone flap (13,14).
The 4 patients in our study with large bone defects had joint
instability; structural allografts from which cartilage had been
removed beforehand and strut plate fixation were chosen in order to
withstand a certain pressure, and stability of the joints was
achieved.
The exposure of necrotic cartilage to the articular
cavity is likely to increase the chances of infection recurring.
The exposure of the bone graft to the articular cavity easily
permits the bacteria remaining in the bone tissue to enter the
articular cavity, or the inflammatory joint fluid to infiltrate the
bone graft, both of which are counter to infection control. In
addition, grafted bone extensively exposed to the articular cavity
is not easily vascularized, requires a long time to be able to
resist infection, may easily become a new source of infection and
is likely to accelerate joint wear and degeneration.
Sealing the articular cavity with the highly
vascularized synovium separates the articular cavity from the
outside structures. The grafted bone may easily obtain a blood
supply from the synovial membrane, which shortens the time taken to
achieve revascularization (15).
In conclusion, the results of the 11 patients
demonstrated that bone grafting combined with the sealing of the
articular cavity using the synovium is an effective treatment
option for metaphyseal osteomyelitis involving the knee joint.
However, further study should be performed to investigate the
long-term outcomes of the synovial tissue and the reconstructed
joint using structural cortical allografts covered by the synovial
membrane.
Acknowledgements
This study was supported by the China
Postdoctoral Science Foundation (CPSF #2004036111).
References
|
1
|
Lew DP and Waldvogel FA: Osteomyelitis.
Lancet. 364:369–379. 2004. View Article : Google Scholar
|
|
2
|
Eckardt JJ, Wirganowicz PZ and Mar T: An
aggressive surgical approach to the management of chronic
osteomyelitis. Clin Orthop Relat Res. 298:229–239. 1994.PubMed/NCBI
|
|
3
|
Cierny G III, Mader JT and Penninck JJ: A
clinical staging system for adult osteomyelitis. Clin Orthop Relat
Res. 414:7–24. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lazzarini L, Mader JT and Calhoun JH:
Osteomyelitis in long bones. J Bone Joint Surg Am. 86:2305–2318.
2004.
|
|
5
|
Garcia-Cimbrelo E and Marti-Gonzalez JC:
Circular external fixation in tibial nonunions. Clin Orthop Relat
Res. 419:65–70. 2004. View Article : Google Scholar
|
|
6
|
McKee MD, Yoo D and Schemitsch EH: Health
status after Ilizarov reconstruction of post-traumatic lower-limb
deformity. J Bone Joint Surg Br. 80:360–364. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mekhail AO, Abraham E, Gruber B and
Gonzalez M: Bone transport in the management of posttraumatic bone
defects in the lower extremity. J Trauma. 56:368–378. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Green SA: Skeletal defects: a comparison
of bone grafting and bone transport for segmental skeletal defects.
Clin Orthop Relat Res. 301:111–117. 1994.PubMed/NCBI
|
|
9
|
Sporer SM, O’Rourke M, Chong P and
Paprosky WG: The use of structural distal femoral allografts for
acetabular reconstruction: Average ten-year follow-up. J Bone Joint
Surg Am. 87:760–765. 2005.PubMed/NCBI
|
|
10
|
Sporer SM, O’Rourke M, Chong P and
Paprosky WG: The use of structural distal femoral allografts for
acetabular reconstruction: Surgical technique. J Bone Joint Surg
Am. 88(Suppl 1): 92–99. 2006.PubMed/NCBI
|
|
11
|
Schimmel JW, Buma P, Versleyen D, Huiskes
R and Slooff TJ: Acetabular reconstruction with impacted morselized
cancellous allografts in cemented hip arthroplasty: a histological
and biomechanical study on the goat. J Arthroplasty. 13:438–448.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bolder SB, Schreurs BW, Verdonschot N,
Veth RP and Buma P: Wire mesh allows more revascularization than a
strut in impaction bone grafting: an animal study in goats. Clin
Orthop Relat Res. 423:280–286. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cierny G III: Chronic osteomyelitis:
results of treatment. Instr Course Lect. 39:495–508. 1990.
|
|
14
|
Weiland AJ, Moore JR and Daniel RK: The
efficacy of free tissue transfer in the treatment of osteomyelitis.
J Bone Joint Surg Am. 66:181–193. 1984.PubMed/NCBI
|
|
15
|
McNally MA, Small JO, Tofighi HG and
Mollan RA: Two stage management of chronic osteomyelitis of the
long bones: the Belfast technique. J Bone Joint Surg Br.
75:375–380. 1993.PubMed/NCBI
|