Introduction
Traumatic lesions of the axillary artery are
relatively rare, representing 15 to 20% of the arterial injuries of
the upper limbs. Of the traumas, 94% are due to penetrating wounds,
while the remaining 6% are caused by blunt traumas following
shoulder fracture-dislocations (1). The axillary artery is commonly
ruptured in high-energy injuries around the shoulder girdle, which
are associated with multiple ruptures of nerves whose incidence
ranges between 27 and 44% (2). The
injured axillary artery may cause a distal ischemia. Consequently,
it is hypothesized that vascular repair by interposition grafting
should be the treatment of choice (3–8). For
those patients with perfectly viable distal limbs due to an
extensive anastomotic network of collateral vessels, it remains
uncertain whether the injured axillary artery should be
reconstructed. The present study reports three cases of proximal
humeral fractures associated with axillary artery injury which were
treated with or without artery reconstruction.
Patients and methods
Case 1
A 22-year-old male fell on his outstretched
left-upper limb with severe pain in the shoulder area. Two hours
after the fall the patient progressively developed coolness,
numbness and weakness extending from the fingers to the elbow of
the left arm. Physical examination revealed soft-tissue swelling
and tenderness around the shoulder. The subclavian pulse was
palpable, but the brachial, radial or ulnar pulses were impalpable.
The hand and forearm were cool and pale and the capillary refill
was slow. The blood pressure of the right arm was 56/46 mmHg, lower
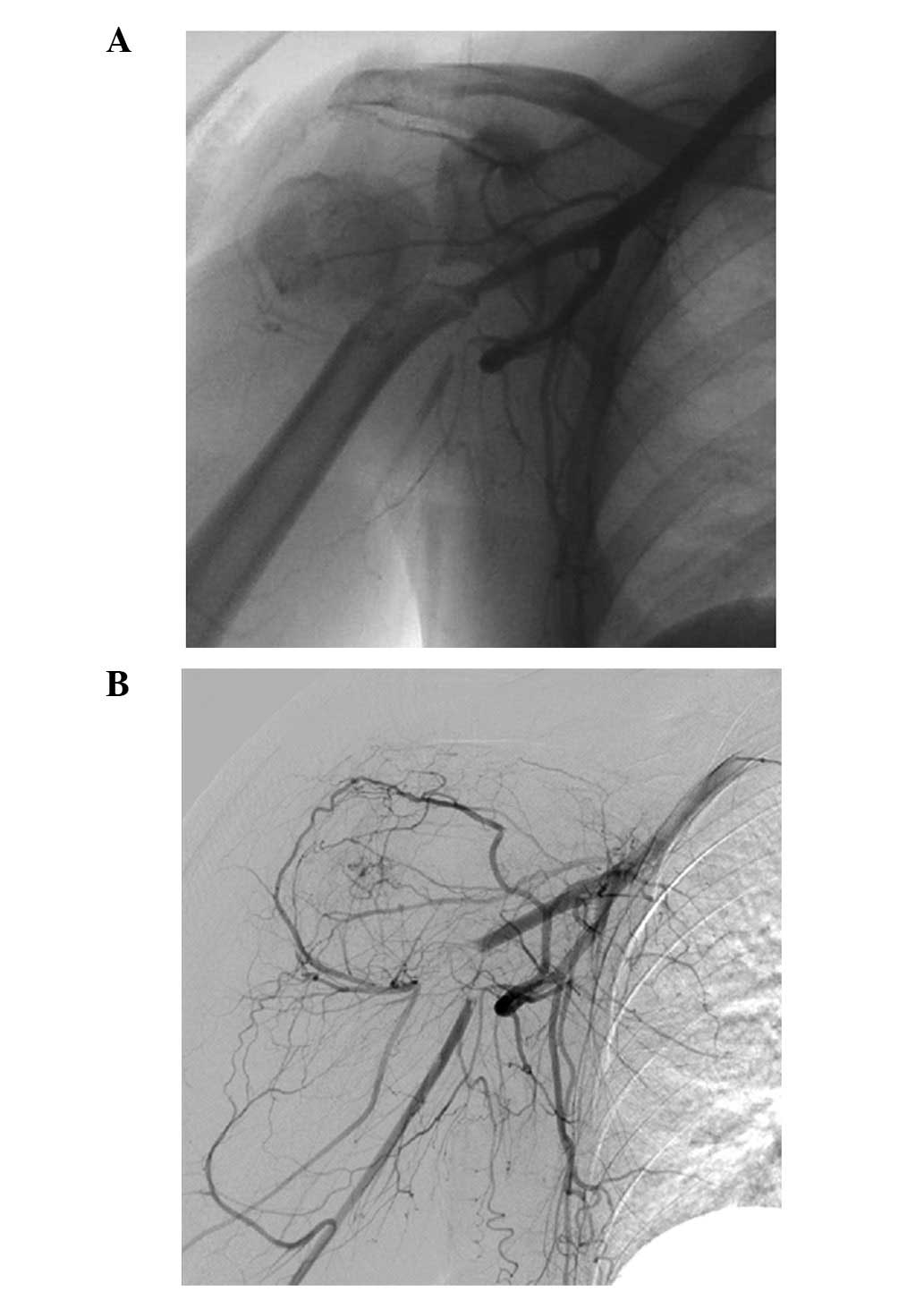
than left side which was 116/70 mmHg. Initial radiography of the
shoulder revealed a displaced comminuted fracture of the humeral
surgical neck (Fig. 1).
Computerized tomography angiography (CTA) of the left-upper
extremity showed an occluded axillary artery just under the level
of glenoid cavity with a 3-cm filling deficiency which was caused
by protrusion of the distal segment of the fracture (Fig. 2). The surgical treatment was
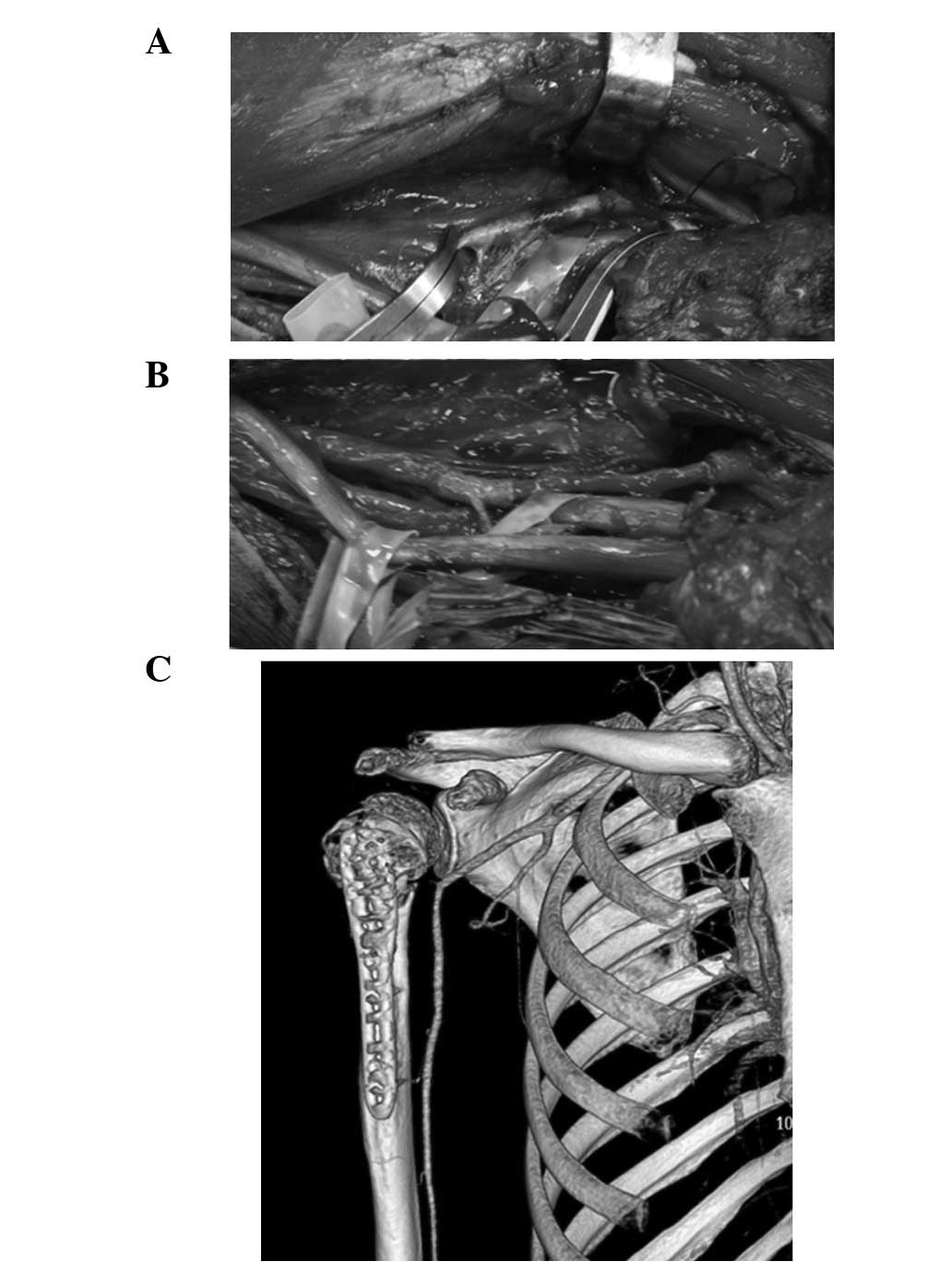
performed through an extended deltopectoral groove incision. The
humeral neck fracture was anatomically reduced and stabilized with
a plate and screws. The axillary artery was exposed and observed to
be contused and thrombosed between the thoracoacromial artery and
circumflex humeral branches (Fig.
3A). The occlusion was caused by an intimal tear with
sub-adventitial dissection and secondary thrombosis. The contused
segment of the axillary artery was replaced with a greater
saphenous vein interposition graft in a reversed fashion (Fig. 3B). The cords of the brachial plexus
appeared to be partly injured. Postoperative neurological recovery
was incomplete with residual weakness of the wrist and finger
extension. The radial pulse was palpable and the blood pressure was
almost equal in each arm (right arm was 110/85 mmHg and left arm
was 118/82 mmHg). Another CTA confirmed the patency of the arterial
repair (Fig. 3C) three months
after the operation.
Case 2
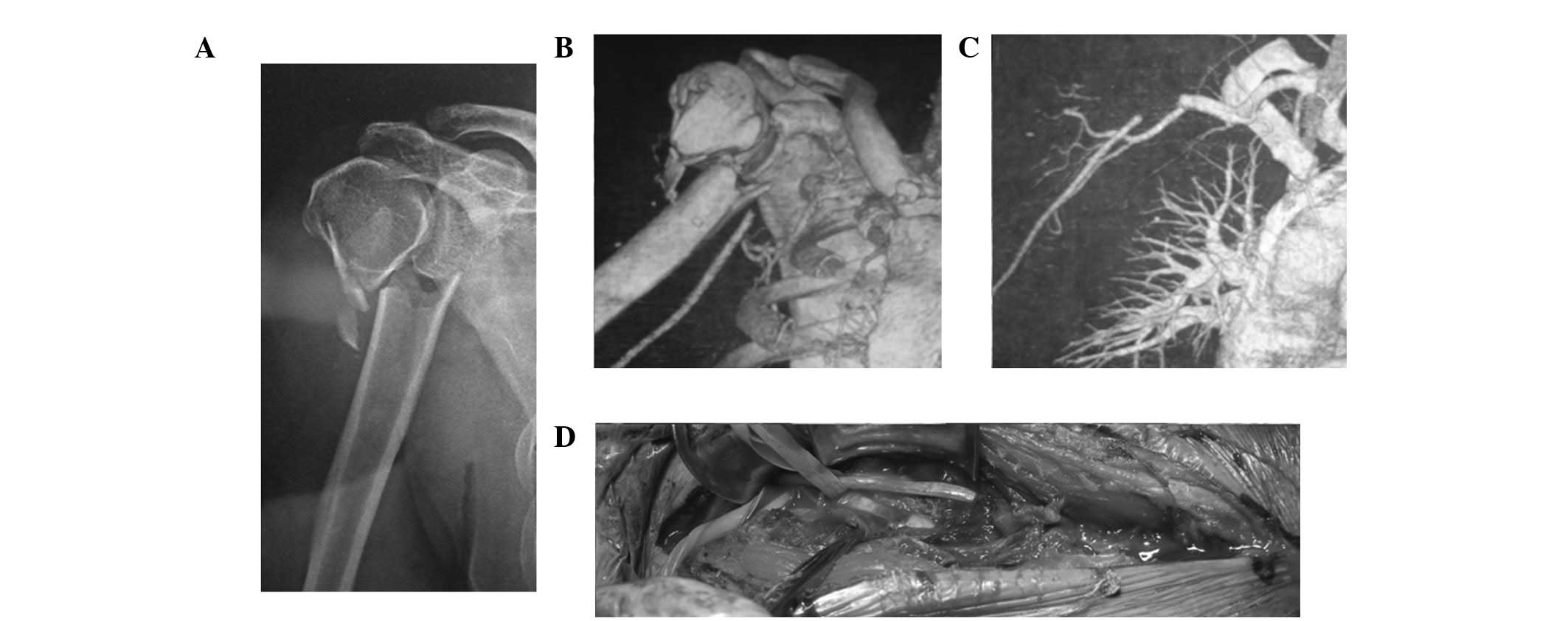
A male 45-year-old received a right-humeral surgical
fracture during a bicycle accident (Fig. 4A). The patient’s right forearm was
cool and two ulnar fingers were numb. The systolic blood pressure
of the right arm was 51 mmHg lower than that of left arm. The CTA
revealed that the distal humeral segment had trapped the axillary
artery, with a 2-cm blood filling deficiency (Fig. 4B). The fracture was reduced and
fixed with a lock plate. The axillary artery was explored and an
embolism was observed at the contused segment (Fig. 4C). The patient’s permission to
repair the artery was not received. As a result, the wound was
closed without administering further treatment to the artery. The
patient returned home following the surgery. On a follow-up visit
three months later, the patient’s right arm was observed to have
become significantlay warmer since the patient left the hospital.
The same temperature was recorded in both arms. The patient was
able to move his hand freely, but the two ulnar fingers remained
feeling numb.
Case 3
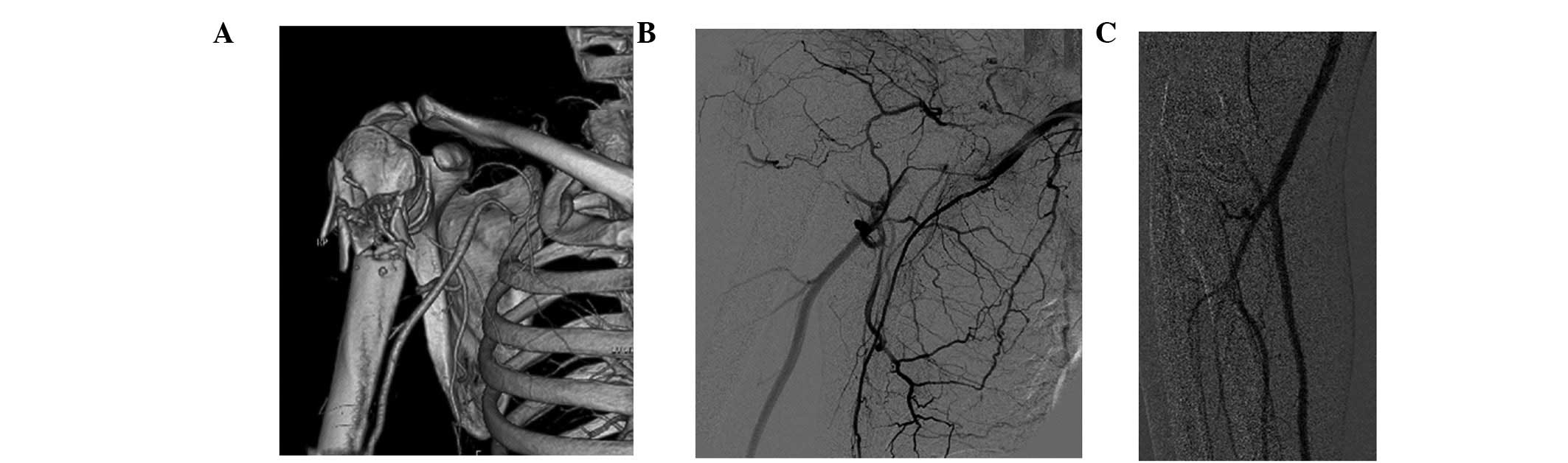
A 47-year-old male construction worker was hit on
his right shoulder by a heavy object while working on scaffolding.
The humeral neck was broken and the whole arm completely lost
motion and feeling (Fig. 5A),
although the hand remained warm. The right brachial pulse and
radial pulse were palpable, but markedly weaker than than those on
the left. The capillary refill was good and the temperature in both
arms was the same. However, the systolic blood pressure in the
right arm was 60 mmHg, much lower than in the left arm which was
108 mmHg. A Doppler ultrasound scan was performed on the axillary,
brachial, radial and ulnar arteries but no vascular injury was
observed, although the artery blood-flow speed was slower (19–22
cm/s). Digital subtraction angiography (DSA) revealed that the
axillay artery was injured badly at the first and second segments
but with extensive collaterals circulation (Fig. 5B) and the brachial, radial and
ulnar arteries were engorged (Fig.
5C). This case was discussed carefully with regard to the
vessel surgery and neurosurgery and the decision was made not to
reconstruct the axillary artery due to three reasons: i) the
patient had a warm hand and good capillary refill, meaning that the
collateralization was rich; ii) the artery was injured by plucking
just below the clavicle and blunted without hematoma. It may have
been dangerous to repair it and the iatrogenic trauma would have
been large; iii) the patient had total brachial plexus injury from
the root, resulting in motion and sensory defects. The function of
the arm may not have been able to recover. The proximal humeral
fracture was reduced and fixed without artery reconstruction.
Results
The present study reports three cases of axillary
artery injury associated with humeral neck fractures. The patients
were all male and injured in right-upper extremity. The mean age
was 38 years (22–47 years). In two cases, the axillary artery was
injured at the third segment due to the bony segment, while in one
case it was injured at the first and second segments which may have
been caused by hard plucking. All the fractures were reduced and
fixed with plates and healed completely. In one patient (case 1)
the axillary artery was repaired with a greater saphenous vein
interposition graft in a reversed fashion. Following surgery, the
pulse, temperature and blood pressure in the injured arm recovered
completely to those of the normal side. In the remaining two cases,
the axillary artery lesion was not repaired. The injured arm became
warmer in the long-term and no patients developed ischemia.
However, the radial pulse was markedly weaker and the blood
pressure was notably lower. As for the brachial plexus lesions, all
three patients were left with motor or sensory deficiencies.
Discussion
Vascular injuries of the upper extremity occur in 30
to 50% of vascular extremity traumas (9–11).
There is a rare subgroup of patients with an associated vascular
injury to the axillary artery and an incidence of 5%. Penetrating
trauma is the primary cause of upper extremity vascular injury (90
to 95% of cases). Blunt trauma due to motor vehicle accidents,
industrial accidents and falls account for the remaining 5 to 10%
(3). The location of the axillary
artery, surrounded by the bones and muscles of the shoulder girdle,
explains the low incidence of trauma suffered by this arterial
segment. Axillary artery injury due to blunt trauma resulting in
proximal humeral fractures is even more uncommon. Humeral neck
fractures with hyper abduction and traction injuries to the
shoulder are a well known cause. The axillary artery is divided
into three segments by the pectoralis minor muscle. The first
segment of the axillary artery is often injured by clavicular
fractures and severe hyper abduction and traction of the shoulder.
The second segment is often injured by this type of injury. The
injury reported in case 3 belonged to this group of injuries and
the first and second segments were damaged. The majority (89%) of
traumatic injuries to the axillary artery occur at the level of the
third segment of the vessel (12).
It is considered to be due to the fact that this segment of the
artery is tethered by the anterior and posterior circumflex vessels
and it is more susceptible to contusion and laceration from the
bony fragments of the humeral neck. The contusion is able to cause
an intimal tear with secondary thrombosis. A hematoma dissecting
the arterial wall has also been described previously (13) and a similar finding was observed in
two of the cases (cases 1 and 2), which were injured by the
contusion of the humeral surgical neck and caused a short-segment
occlusion in the second and third segments of the axillary
artery.
Axillary artery injury due to humeral neck fractures
may be identified early with a physical examination. Yagubyan and
Panneton (3) reported that pulses
were abnormal in 89% involved limbs and 75% had no distal pulse,
whereas 14% had decreased pulses. Two of the three patients (cases
1 and 2) had no radial pulse and case 3 had a weak radial pulse.
The temperature of the limb was another important physical sign.
The majority of the patients with axillary artery injuries reported
previously had cold or cool upper extremities (3–10).
These patients also exhibited pale fingers and poor capillary
refill. Of the limbs of the present cases, case 1 was cold, case 2
was cool and case 3 was as warm as the uninjured arm. The the
brachial blood pressure was recorded. All three cases had lower
systolic blood pressure than the uninjured arm. The right systolic
blood pressure of case 1 was difficult to measure and was 60 mmHg
lower. In case 2, it was 51 mmHg lower. Even in case 3 the systolic
blood pressure was also was 48 mmHg lower despite the normal
temperature. So if a patient with a humeral surgical neck fracture
has a cool, pulseless, lower blood pressure arm, this suggests that
the axillary artery may be injured and further examination should
be performed.
Doppler ultrasound, DSA and venous contrast CTA are
useful for to making a definitive diagnosis of axillary artery
injuries (3,8,13).
Ultrasound requires no wound, is convenient and cheap and is widely
used to detect the integrity of the vessels (6). However, it may sometimes provide
false-negative results if the patient has rich collateral
circulation and it may not detect the right injured segment of the
axillary artery due to the fracture. In case 3, the embolized
segment of the axillary artery was not identified with ultrasound,
but the DSA clearly showed that the axillary artery was injured and
a filling deficiency had occurred at the third segment. CTA was
used in all three cases. It easily identified the location and the
degree to which the artery was damaged. It also clearly showed the
association between the artery and the bony segment. In case 1, CTA
was used to evaluate the result of the injured artery being
replaced by a greater saphenous vein segment. Vessel angiography is
usually considered to be necessary in performing a diagnosis of the
axillary artery injury (3–6,8).
The broken humeral surgical neck and injured
axillary artery may be treated at the same time. The deltopectoral
groove approach is advocated, since it exposes the humeral neck and
the axillary artery excellently. As in case 1, using a
deltopectoral groove incision the fractured fragments of the
humeral neck were reduced and fixed with a locked plate and screws.
The injured artery was exposed and repaired with a greater
saphenous vein interposition graft. In cases of axillary arteries
with blunt injuries, the orthopedic procedure is often required
before vascular repair is undertaken since the reduction and
stabilization of the humeral neck fracture may allow the vessel
repair to be performed conveniently and prevent the repaired artery
from being injured again.
Whether the injured axillary artery should be
reconstructed is not clear. It is usually (3–8,11,13,14)
considered to be necessary to repair the artery as soon as possible
and even in those with adequate distal perfusion, fracture
stabilization and vascular repair is likely to improve the
long-term outcome and posttraumatic cold intolerance (15). Conservative management is clearly
advised against in an ischemic limb (13). When the artery is broken or
blocked, the distal segment of the limb has a lower systolic blood
pressure, meaning that the tissue perfusion pressure is lower and
ischemia is likely to occur. In the present cases of axillary
artery injuries, all had lower blood pressures. Case 1 underwent a
formal arterial reconstruction and the upper extremity recovered
normal temperature, strong radial pulse, normal blood pressure and
good capillary refill. This is beneficial for injured limb
recovery. When reviewing the literature, >70% of the patients
underwent reconstruction, including end-to-end anastomosis and
interposition or bypass grafts with saphenous veins or vascular
prostheses. A simple primary repair involving intimal excision and
tacking down with or without a thrombectomy was performed in a
number of patients. Shalhub et al describe an endovascular
technique utilizing combined brachial and femoral access to create
a through-and-through brachial-femoral wire and repair the arterial
injury with a covered stent (16).
Only ∼10% of the patients were treated conservatively, including an
elderly patient with an old fracture. The injured limb may be alive
due to the presence of extensive collateral circulation (3).
The axillary artery has 5 major branches which form
multiple anastomoses and develop a web-like network, supplying the
thoracic and scapular/humeral areas and providing excellent
collateral circulation around the shoulder girdle. A short-segment
occlusion of the axillary artery between the origins of these
arterial branches that prevents the flow through them may be
effectively bypassed by these collaterals. A discussion with the
vascular surgeons suggested that the vascular injury may be treated
conservatively by relying on collateral circulation, as the limb
was warm and the brachial plexus injury was not due to a pressure
effect from a large hematoma (8).
In cases 2 and 3, although the axillary arteries were occluded or
ruptured and the patients did not undergo reconstruction, the
extremity did not experience ischemia in the long-term due to the
rich collateralization. The artery in case 3 was not reconstructed
based on three factors: i) the patient had a warm arm and good
capillary refill, meaning that the collateralization was rich; ii)
the artery was injured by plucking just below the clavicle and
blunted without hematoma. It may have been dangerous to repair it
and the iatrogenic trauma would have been large; iii) the patient
had total brachial plexus injured from the root, resulting in
motion and sensory defects. The function of the arm may not have
been able to recover. This case was discussed carefully with regard
to the vessel surgery and the decision was made to reduce and fix
the fracture only. Although two of the present cases and a number
reported previously (3) had
non-ischemic limbs without artery reconstruction, it is necessary
to evaluate the long-term outcome.
The intimate association of the brachial plexus and
the axillary artery is so close that it is a notable feature of
axillary artery trauma associated with brachial plexus injury
(3,7). The brachial plexus and axillary
artery lie in a common fascial sheath. Damage to the artery, which
may cause only minimal swelling, is capable of leading to early
compression of the brachial plexus and its components. The main
cause of injury is the direct damage resulting from the broken
humeral bone segment. Axillary sheath hematomas may be another
reason for delayed ischemia. Of these patients, 46% exhibited a
neurological deficit (17).
Johnson et al(17) reported
a 43.5% incidence of brachial plexus injury occurring in patients
with subclavian and axillary artery vascular trauma. Other studies
have also reported a similarly high incidence of nerve injury in
upper extremity vascular trauma, between 35 and 70% (3,18–21).
In the present cases, all patients had different brachial complex
injuries and were left with neurological motion and sensory
defects.
Axillary artery injury resulting from humeral neck
fractures is a rare but disabling traumatic event (3). Special attention should be payed to
fractures with abduction and severe medial displacement. The
patients’ pulse, temperature and blood pressure are highly
sensitive physical signs of axillary artery injuries. Angiograms,
including DSA and CTA, are the best method for diagnosing arterial
injuries and evaluating the condition of the collateral
circulation. The majority of these patients should undergo artery
reconstruction while the humeral neck fracture is reduced and
fixed, with the exception of certain special cases. Recognition of
concomitant brachial plexus injury is also important for decreasing
the neurological morbidity. The orthopedic surgery, vessel surgery
and neurosurgery should work together to treat these patients
(21).
References
|
1
|
Gallucci G, Ranalletta M, Gallucci J, De
Carli P and Maignon G: Late onset of axillary artery thrombosis
after a nondisplaced humeral neck fracture: a case report. J
Shoulder Elbow Surg. 16:e7–e8. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Birch R and Bonney G: Compound nerve
injuries: the vascular lesion. Surgical Disorders of the Peripheral
Nerves. Birch R, Bonney G and Wynn Parry CB: 1st edition. Churchill
Livingstone; London: pp. 125–134. 1998
|
|
3
|
Yagubyan M and Panneton JM: Axillary
artery injury from humeral neck fracture: a rare but disabling
traumatic event. Vasc Endovascular Surg. 38:175–184. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Matheï J, Depuydt P, Parmentier L, Olivie
F, Harake R and Janssen A: Injury of the axillary artery after a
proximal humeral fracture: a case report and overview of the
literature. Acta Chir Belg. 108:625–627. 2008.PubMed/NCBI
|
|
5
|
Zarkadas PC, Throckmorton TW and Steinmann
SP: Neurovascular injuries in shoulder trauma. Orthop Clin North
Am. 39:483–490. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Modi CS, Nnene CO, Godsiff SP and Esler
CN: Axillary artery injury secondary to displaced proximal humeral
fractures: a report of two cases. J Orthop Surg (Hong Kong).
16:243–246. 2008.PubMed/NCBI
|
|
7
|
Stenning M, Drew S and Birch R: Low-energy
arterial injury at the shoulder with progressive or delayed nerve
palsy. J Bone Joint Surg Br. 87:1102–1106. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Seagger RM and Kitson J: A rare
combination of an axillary artery and brachial plexus injury due to
a proximal humeral fracture. J Shoulder Surg. 3:71–73. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mattox KL, Feliciano DV, Burch J, Beall
AC, Jordan GL and De Bakey ME: Five thousand seven hundred sixty
cardiovascular injuries in 4459 patients. Epidemiologic evolution
1958 to 1987. Ann Surg. 209:698–705. 1989. View Article : Google Scholar
|
|
10
|
Keen RR, Meyer JP, Durham JR, et al:
Autogenous vein graft repair of injured extremity arteries: early
and late results with 134 consecutive patients. J Vasc Surg.
13:664–668. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ender Topal A and Nesimi Eren M:
Management of axillosubclavian arterial injuries and predictors of
outcome. Minerva Chir. 66:307–315. 2011.PubMed/NCBI
|
|
12
|
Hayes JM and Van Winkle GN: Axillary
artery injury with minimal displaced fracture of neck of the
humerus. J Trauma. 23:431–433. 1983. View Article : Google Scholar
|
|
13
|
Jensen BV, Jacobsen J and Andreasen H:
Late appearance of arterial injury caused by fracture of the neck
of the humerus. J Trauma. 27:1368–1369. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
McLaughlin JA, Light R and Lustrin I:
Axillary artery injury as a complication of proximal humerus
fractures. J Shoulder Elbow Surg. 7:292–294. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Klocker J, Peter T, Pellegrini L, et al:
Incidence and predisposing factors of cold intolerance after
arterial repair in upper extremity injuries. J Vasc Surg.
56:410–414. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Shalhub S, Starnes BW and Tran NT:
Endovascular treatment of axillosubclavian arterial transection in
patients with blunt traumatic injury. J Vasc Surg. 53:1141–1144.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Johnson SF, Johnson SB, Strodel WE, Barker
DE and Kearney PA: Brachial plexus injury: association with
subclavian and axillary vascular trauma. J Trauma. 31:1546–1550.
1991. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Carlsen BT, Bishop AT and Shin AY: Late
reconstruction for brachial plexus injury. Neurosurg Clin N Am.
20:51–64. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Myers SI, Harward TR, Maher DP, Melissinos
EG and Lowry PA: Complex upper extremity vascular trauma in an
urban population. J Vasc Surg. 12:305–309. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wenger JD and Olsson CJ: Acute limb
ischemia after a proximal humeral epiphyseal fracture:
intraoperative findings of an illustrative vascular lesion. J
Shoulder Elbow Surg. 20:e1–e3. 2011. View Article : Google Scholar
|
|
21
|
Syed AA and Williams HR: Shoulder
disarticulation: a sequel of vascular injury secondary to a
proximal humeral fracture. Injury. 33:771–774. 2002. View Article : Google Scholar : PubMed/NCBI
|