Introduction
The head computed tomography perfusion (CTP)
technique is an important method for cerebral blood flow assessment
(1–4). This technique visually represents the
blood flow perfusion in various parts of the brain tissue. In the
application of CTP, time to peak (TTP) is the most sensitive and
specific index for brain ischemia (5). Stenting is a technique which has been
applied in cerebrovascular disease treatment, particularly for
ischemic cerebrovascular diseases (6–10).
The effect of stenting on ischemic cerebrovascular disease may be
evaluated visually using the CTP technique (11,12).
In the present study, the Alberta stroke program
early computed tomography scoring (ASPECTS) scale was used to
quantitatively analyze CTP in 25 patients with ischemic
cerebrovascular disease caused by middle cerebral artery solitary
stenosis prior to and following stenting. The factors affecting CTP
prior to and following stenting were further analyzed (13,14).
Patients and methods
Clinical data
A total of 25 patients with cerebrovascular disease
caused by unilateral middle cerebral artery solitary stenosis that
received treatment at Tiantan Hospital (Beijing, China) between
January 1, 2004 and March 1, 2007 were enrolled. All patients were
subjected to percutaneous stent implantation (stenting). Head CTP
imaging was performed within 7 days before and after stenting. Of
the 25 patients, 12 had transient ischemic attack (TIA) and 13 had
cerebral infarction (CI). The patient’s ages ranged between 34 and
71 years with an average of 49.4±8.4 years. Of the patients, 19
were male and 6 were female. The degree of stenosis ranged between
60 and 99% with an average of 80.1±11.4%. This study was conducted
with approval from the Ethics Committee of Capital Medical
University. Written informed consent was obtained from all
participants.
Pre-stenting evaluation
Preoperative evaluation included angiographic
classification of the cerebral arterial stenosis based on Mori’s
method (15,16), clinical typing of the cerebral
arterial stenosis (6) and
classification based on whether apparent cerebral blood flow
collateral circulation existed (17).
CTP examination
CT scanning was performed using a GE Lightspeed
spiral CT system. The scanning matrix was 512x512 and the exposure
conditions were 120 kV and 100 mA. Successive scanning of the
layers of interest began when a high pressure injector was started
for rapid intravenous injection of the contrast medium. The slice
thickness was 10 mm and the scanning lasted 60 sec at a 1 slice/sec
scanning rate (60 slices in total). Iohexol (300 mg/ml) was used as
the contrast medium, with a volume of 40 ml at an 8 ml/sec flow
rate. The layers of interest included the basal and coronal
radiation layers. The regional cerebral blood flow (rCBF), regional
cerebral blood volume (rCBV), mean transit time (MTT) and TTP
parameters were calculated using professional software. Color maps
were obtained.
Pre- and post-stenting CTP scoring
criteria
The CT parameter color maps prior to and following
stenting were compared and the head CTP TTP prior to and following
stenting was scored using the ASPECTS scale (13,14).
The highest possible mark of the scale is 10 points. Higher scores
indicates greater cerebral perfusion. The TTP improvement degree
was then calculated based on the following formula: TTP improvement
degree = (post-stenting ASPECTS score - pre-stenting ASPECTS
score)/10x100(%).
Statistical analysis
The χ2 test was used to compare
categorical data, and t-tests or paired t-tests were used to
compare continuous data. Correlation analysis and linear regression
were performed to calculate the correlation coefficient and
regression equation. All data were analyzed using SPSS 11.5
statistical software.
Results
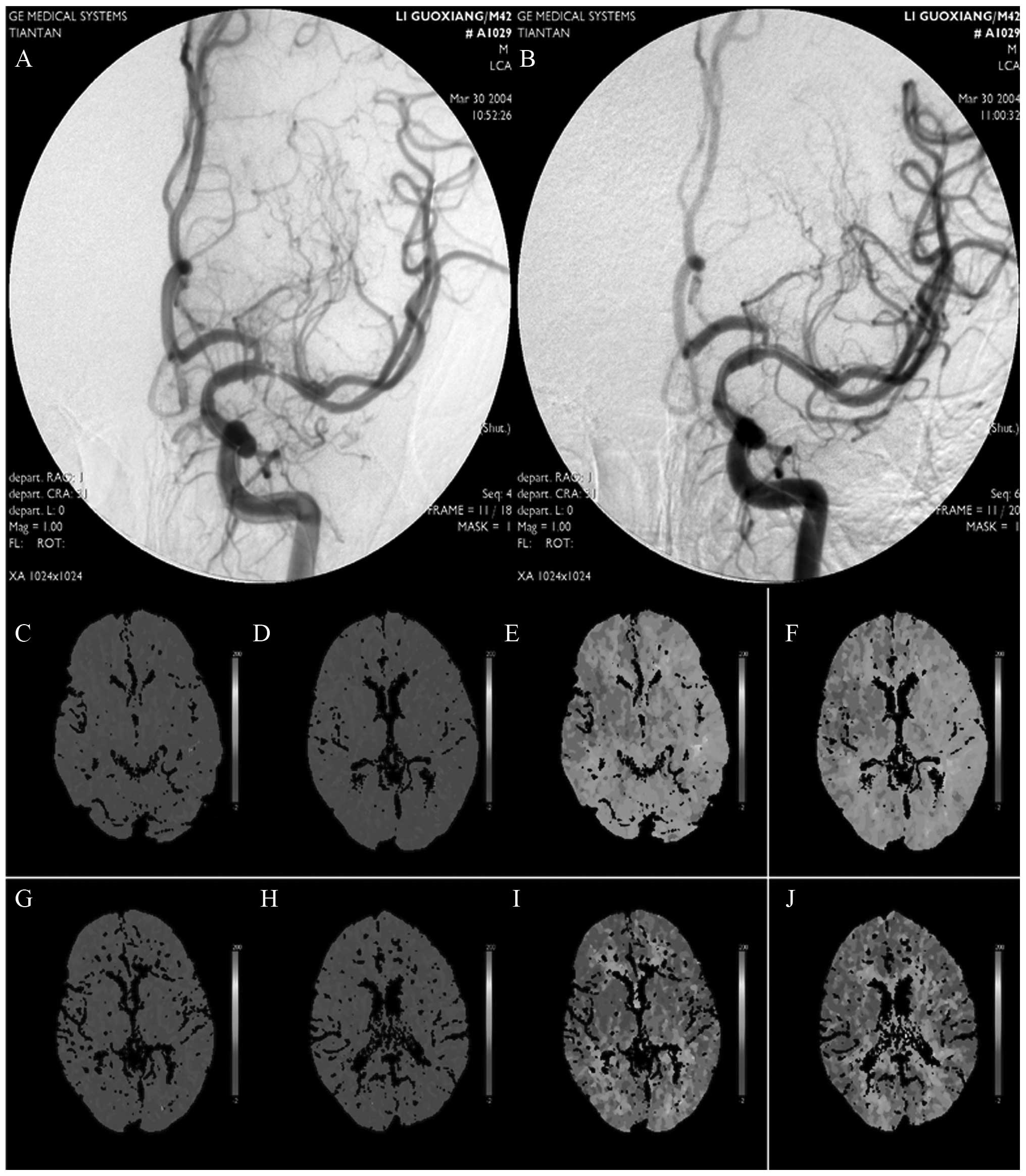
The CTP color maps revealed that the TTP values in
all the 25 patients were significantly prolonged prior to surgery,
while following surgery, all these values improved by various
degrees. The ASPECTS score (mean ± SD) prior to surgery was
2.32±1.31, whereas that following surgery was 8.28±1.65, indicating
a significant difference (P<0.01). The preoperative ASPECTS
score was negatively correlated with the degree of middle cerebral
artery solitary stenosis with a correlation coefficient of −5.78
(Fig. 1).
Furthermore, the correlation factors possibly
affecting pre- and post-stenting CTP improvement were analyzed and
compared between the subgroups. These factors included gender,
discharge diagnosis of manifestations and vessels (including CI and
TIA), collateral circulation, histories of high blood pressure,
diabetes, coronary heart disease and smoking, as well as
dyslipidemia and hyperhomocysteinemia. The comparisons revealed
that only the collateral circulation subgroups exhibited a
significant difference (P=0.033). The results are shown in Table I. Correlations of age, the
preoperative vascular stenosis rate, postoperative residual
stenosis rate and pre- and post-operative scores based on the
National Institutes of Health stroke scale (NIHHS) with CTP
improvement were analyzed. The results revealed that only the
preoperative vascular stenosis rate was positively correlated with
the CTP ASPECTS score improvement with a correlation coefficient of
1.137 (P=0.01; Table II).
 | Table I.T-test analysis of the factors
affecting pre- and post-operative CTP. |
Table I.
T-test analysis of the factors
affecting pre- and post-operative CTP.
| Factor | Pre-stenting
ASPECTS | Post-stenting
ASPECTS | Improvement degree
(%) | P-value |
|---|
| Gender | | | | 0.121 |
| Male | 2.26±1.33 | 8.58±1.50 | 63.16±17.34 | |
| Female | 2.50±1.38 | 7.33±1.86 | 48.33±26.40 | |
| High blood
pressure | | | | 0.782 |
| Yes | 2.36±1.03 | 8.45±1.75 | 60.91±20.72 | |
| No | 2.29±1.54 | 8.14±1.61 | 58.57±20.70 | |
| Diabetes | | | | 0.462 |
| Yes | 1.50±0.71 | 8.50±2.12 | 70.00±14.14 | |
| No | 2.39±1.34 | 8.26±1.66 | 58.70±20.74 | |
| Coronary heart
diseasea | | | | 0.315 |
| Yes | 2.00 | 10.00 | 80.00 | |
| No | 2.33±1.34 | 8.21±1.64 | 58.75±20.28 | |
| Smoking | | | | 0.426 |
| Yes | 2.17±1.10 | 8.33±1.50 | 61.67±18.23 | |
| No | 2.71±1.80 | 8.14±2.12 | 54.29±25.73 | |
| Drinking | | | | 0.384 |
| Yes | 2.50±1.17 | 8.08±1.51 | 55.83±18.32 | |
| No | 2.15±1.46 | 8.46±1.81 | 63.08±22.13 | |
| Dyslipidemia | | | | 0.190 |
| Yes | 2.00±0.93 | 8.40±1.80 | 64.00±19.57 | |
| No | 2.80±1.69 | 8.10±1.45 | 53.00±20.58 | |
|
Hyperhomocysteinemia | | | | 0.484 |
| Yes | 2.43±1.27 | 8.86±1.21 | 64.29±19.02 | |
| No | 2.28±1.36 | 8.06±1.76 | 57.78±21.02 | |
| Discharge
diagnosis | | | | 0.286 |
| TIA | 2.83±1.47 | 8.33±1.61 | 55.00±21.95 | |
| CI | 1.84±0.99 | 8.23±1.74 | 63.85±18.50 | |
| Collateral
circulation | | | | |
| Yes | 2.91±1.38 | 7.91±2.02 | 50.00±21.91 | 0.033 |
| No | 1.86±1.10 | 8.57±1.28 | 67.14±15.90 | |
 | Table II.Correlation analysis of the factors
possibly affecting pre- and post-stenting CTP. |
Table II.
Correlation analysis of the factors
possibly affecting pre- and post-stenting CTP.
| Factor | P-value |
|---|
| Age | 0.839 |
| Preoperative vascular
stenosis rate | 0.001 |
| Postoperative
residual stenosis rate | 0.923 |
| Pre-stenting NIHHS
score | 0.668 |
| Post-stenting NIHHS
score | 0.596 |
Discussion
Cerebral arterial stenosis is a significant
pathological mechanism leading to ischemic cerebrovascular disease.
Theoretically, the removal of stenosis and improvement of the
cerebral blood flow is likely to decrease the incidence of CI.
Percutaneous endovascular stenting has been demonstrated to be an
effective treatment method for intracranial cerebral arterial
stenosis (6–8), although evaluations of the
effectiveness of stenting are often based on long-term stroke and
preoperative event incidence rates (6,7). CTP
is highly sensitive to the improvement effect of stenting on
cerebral perfusion. CTP color maps visually represent the cerebral
perfusion improvement following stenting (12,18)
but are not contributory to scientific research statistics. The
ASPECTS scale was an early tool for evaluating the effect of
thrombolytic therapy on CI (13,14).
Since the radiological layers involved in the ASPECTS scale are the
same as the CT scanning layers involved in the CTP technique, the
scale may also be used for evaluating middle cerebral arterial
blood supply.
All 25 patients in the present study had middle
cerebral artery solitary stenosis. The CTP color maps revealed that
their TTP was prolonged prior to stenting, whereas following
stenting, the values were improved significantly. These findings
were consistent with those reported previously (11,12).
The ASPECTS score also revealed a significant difference in the
cerebral perfusion prior to and following stenting (P<0.01),
which indicated a perfusion improvement following stenting. This
result suggests that the evaluation of CTP improvement using the
ASPECTS scale is feasible. However, although the ASPECTS score bore
a negative correlation with the degree of severity of middle
cerebral stenosis prior to stenting, a correlation was not observed
between the ASPECT score and residual stenosis following stenting.
When the middle cerebral stenosis was between 60% and 99%, the more
serious stenosis led to a lower ASPECT score, whereas when residual
stenosis fell below 30%, the ASPECT score did not appear to vary
according to the severity of stenosis. This suggests that the
ASPECTS scale has statistical significance only within certain
degrees of stenosis.
Furthermore, the correlation factors which may
affect CTP prior to and following stenting were also analyzed in
the present study. The studied factors included age, gender,
histories of high blood pressure, smoking, drinking, diabetes and
coronary heart disease, as well as hyperlipidemia,
hyperhomocysteinemia, postoperative residual stenosis rate, NIHHS
score prior to and following surgery and discharge diagnosis (TIA
and CI). The analysis revealed that the preoperative vascular
stenosis rate and collateral circulation were the only factors
correlated with the degree of CTP improvement. This result suggests
that the non-correlated factors are negligible in surgical patient
selection and prognosis assessment. The preoperative vascular
stenosis rate was markedly correlated with the degree of
postoperative CTP improvement. A more serious degree of stenosis
indicated a more marked improvement effect of stenting for cerebral
perfusion and cerebral ischemia. In addition, whether there was
good collateral circulation in the blood supply region prior to
stenting also greatly affected the degree of postoperative CTP
improvement. Patients without good collateral circulation exhibited
greater degrees of CTP improvement. This suggests that patients
without good collateral circulation benefit more from stenting,
which is in agreement with the reported literature (7).
Based on the findings of the present study, the
degree of vascular stenosis and whether good collateral circulation
exists should be considered first when stenting is selected for
patients with intracranial arteriostenosis, in order to achieve
satisfactory cerebral perfusion improvement. The considerations of
age, gender, drinking, high blood pressure, diabetes, coronary
heart disease, lipid disorders and hyperhomocysteinemia should then
be considered. However, the present study had a significant
limitation. In order to remove the effects of external factors, all
the recruited patients were those with single cerebral artery
disease. The patients received CTP detection prior to and following
stenting. Due to the strict selection criteria, the sample size in
the present study was small with only 25 subjects enrolled.
References
|
1.
|
Gasparotti R, Grassi M, Mardighian D, et
al: Perfusion CT in patients with acute ischemic stroke treated
with intra-arterial thrombolysis: predictive value of infarct core
size on clinical outcome. AJNR. 30:722–727. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
d’Esterre CD, Aviv RI and Lee TY: The
evolution of the cerebral blood volume abnormality in patients with
ischemic stroke: a CT perfusion study. Acta Radiol. 53:461–467.
2012.PubMed/NCBI
|
|
3.
|
König M: Brain perfusion CT in acute
stroke: current status. Eur J Radiol. 45(Suppl 1): S11–S22.
2003.
|
|
4.
|
Galvez M, York GE 2nd and Eastwood JD: CT
perfusion parameter values in regions of diffusion abnormalities.
AJNR Am J Neuroradiol. 25:1205–1210. 2004.PubMed/NCBI
|
|
5.
|
Smith WS, Roberts HC, Chuang NA, et al:
Safety and feasibility of a CT protocol for acute stroke: combined
CT, CT angiography, and CT perfusion imaging in 53 consecutive
patients. AJNR Am J Neuroradiol. 24:688–690. 2003.PubMed/NCBI
|
|
6.
|
Jiang WJ, Wang YJ, Du B, et al: Stenting
of symptomatic M1 stenosis of middle cerebral artery: an initial
experience of 40 patients. Stroke. 35:1375–1380. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Chimowitz MI, Lynn MJ, Derdeyn CP, et al:
Stenting versus aggressive medical therapy for intracranial
arterial stenosis. N Engl J Med. 365:993–1003. 2011. View Article : Google Scholar
|
|
8.
|
Gröschel K, Schnaudigel S, Pilgram SM,
Wasser K and Kastrup A: A systematic review on outcome after
stenting for intracranial atherosclerosis. Stroke. 40:e340–e347.
2009.PubMed/NCBI
|
|
9.
|
SSYLVIA Study Investigators: Stenting of
Symptomatic Atherosclerotic Lesions in the Vertebral or
Intracranial Arteries (SSYLVIA): study results. Stroke.
35:1388–1392. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Suh DC, Kim JK, Choi JW, et al:
Intracranial stenting of severe symptomatic intracranial stenosis:
results of 100 consecutive patients. AJNR Am J Neuroradiol.
29:781–785. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Roberts HC, Dillon WP and Smith WS:
Dynamic CT perfusion to assess the effect of carotid
revascularization in chronic cerebral ischemia. AJNR Am J
Neuroradiol. 21:421–425. 2000.PubMed/NCBI
|
|
12.
|
Trojanowska A, Drop A, Jargiello T,
Wojczal J and Szczerbo-Trojanowska M: Changes in cerebral
hemodynamics after carotid stenting: evaluation with CT perfusion
studies. J Neuroradiol. 33:169–174. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Barber PA, Demchuk AM, Zhang J and Buchan
AM: Validity and reliability of a quantitative computed tomography
score in predicting outcome of hyperacute stroke before
thrombolytic therapy. ASPECTS Study Group Alberta Stroke Programme
Early CT Score. Lancet. 355:1670–1674. 2000. View Article : Google Scholar
|
|
14.
|
Pexman JH, Barber PA, Hill MD, et al: Use
of the Alberta Stroke Program Early CT Score (ASPECTS) for
assessing CT scans in patients with acute stroke. AJNR Am J
Neuroradiol. 22:1534–1542. 2001.PubMed/NCBI
|
|
15.
|
Mori T, Fukuoka M, Kazita K and Mori K:
Follow-up study after intracranial percutaneous transluminal
cerebral balloon angioplasty. AJNR Am J Neuroradiol. 19:1525–1533.
1998.PubMed/NCBI
|
|
16.
|
Feldman RL, Trigg L, Gaudier J and Galat
J: Use of coronary Palmaz-Schatz stent in the percutaneous
treatment of an intracranial carotid artery stenosis. Cathet
Cardiovasc Diagn. 38:316–319. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Higashida RT, Furlan AJ, Roberts H, et al:
Trial design and reporting standards for intra-arterial cerebral
thrombolysis for acute ischemic stroke. Stroke. 34:e109–e137. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Kalia J, Wolfe T and Zaidat OO:
Limb-shaking transient ischemic attack masquerading as lumbar
radiculopathy from pericallosal artery stenosis treated
successfully with intracranial angioplasty and stenting. J Stroke
Cerebrovasc Dis. 19:169–173. 2010. View Article : Google Scholar
|