Introduction
Ankle joint injuries are common in clinical practice
(1,2) and lateral malleolar fractures have
the highest incidence (3,4). The Danis-Weber classification is a
commonly used system for classifying distal fibular fractures. The
classification concerns the association of the fracture line with
the distal tibiofibular syndesmosis. Type A fractures have a
fracture line in the distal fibula which is lower than the
syndesmosis level. The fracture line in type B is the same as the
syndesmosis level while in type C the syndemosis level is higher
(5).
Ankle fractures involving posterior malleolus
fractures account for 14–44% of all ankle fractures (6). In 1932, Henderson (8) first defined posterior malleolus
fractures and proposed the trimalleolar concept. However, this
definition was based on an imaging view from an upper lateral film
and was not a truly anatomical concept. Since the average lateral
rotation angle of the lateral ankle joint is 27.5°, the majority of
the fracture lines are irregular, meaning that the angle between
the posterior malleolus fracture line and the lateral axis of the
ankle joint detected by a lateral X-ray varies. It is almost
impossible to accurately assess the size and orientation of
posterior malleolus fracture fragments via X-ray films (8).
In 2006, Haraguchi et al(16) classified posterior malleolus
fractures into three types based on computed tomography (CT) scans.
The type I fractures involved wedge-shaped bone fragments at the
posterolateral end of the tibia with transverse fracture lines. The
type II fractures included fractures with a fracture line extending
from the fibular notch at the lower end of the tibia to the medial
malleolus and the type III fractures included solitary or multiple
cortical fractures at the posterior lip of the tibia. The ratio of
the posterior malleolus fracture fragments to the entire surface
area of the tibial distal joint (based on CT scans) was calculated
for each type of fracture. Haraguchi et al(16) observed that 11.7% of the joint
surface was affected in type I fractures, 29.8% in type II
fractures and only an extremely small area in type III
fractures.
The optimal intervention for posterior malleolus
fractures has long been controversial. Certain clinicians believe
that additional treatment for posterior malleolus fractures is not
necessary since resetting the fracture fragments may be achieved
with the reduction of the lateral malleolus fracture due to the
mechanical stretch from the ligament behind the distal tibiofibular
syndesmosis (10). By contrast,
others support the view that incomplete reduction of posterior
fractures may alter the contact area and the biomechanics of the
tibiotalar joint. These surgeons recommend an incision in the
posterior joint capsule which allows the doctor to reset the
fracture fragments and fix the screws within a direct view
(9). At present, it is commonly
accepted that fractures in which >10% (25% in previous criteria)
of the joint surface is affected and >2 mm of displacement of
the posterior malleolus fracture fragments is evident should be
actively treated since fractures involving the posterior malleolus
result in osteoarthritis in the ankle joint more frequently than
bimalleolar fractures (11,12).
Similarly, dispute remains in terms of the incision
selection for fibular fractures accompanied by posterior malleolus
fractures. The lateral approach is performed between the
superficial peroneal and sural nerves (in front of the peroneus
longus and peroneus brevis) and provides good access to the ankle
joint, allowing for easy placement of a distal tibiofibular
syndesmotic screw (13). The
posterolateral incision is performed on the medial side of the
posterior edge of the fibula and the point of entry is between the
peroneal and flexor hallux longus tendons. Peroneal tendons are
usually stretched toward the medial side to expose the fracture
fragments at the corner of the posterolateral side of the fibula
and the posterolateral side of the posterior malleolus (14). The posterior incision is performed
between the Achilles tendon and the distal fibula and the peroneal
tendon is stretched toward the lateral side, which protects the
sural nerve and the small saphenous vein on the lateral side, while
exposing the fibular fracture line and the posterolateral corner of
the posterior malleolus between the peroneal and flexor hallucis
longus tendons. The present study aimed to quantitatively analyze
the anatomical characteristics of the lateral, postero-lateral and
posterior approaches to the fibula. Furthermore, the advantages of
the operative approaches and the anatomical issues that affect the
selection of an operative approach for fibula fractures involving
the posterior malleolus were analyzed according to the Danis-Weber
classification and the Haraguchi classification for CT scans of
posterior malleolus fractures.
Materials and methods
The present study was conducted in accordance with
the Declaration of Helsinki and with approval from the Ethics
Committee of Huashan Hospital, Fudan University (Shanghai, China).
Written informed consent was obtained from all participants.
Leg specimens from below the knee joint were
obtained from 10 fresh cadavers which were provided by the Foot and
Ankle Surgeon Training Center of the Chinese Medical Association
(Applied Anatomy and Training Center, Huashan Hospital, Fudan
University). None of the specimens had any evidence of prior injury
or surgery to the leg. All specimens were fresh-frozen and stored
at −18°C until they were thawed for use.
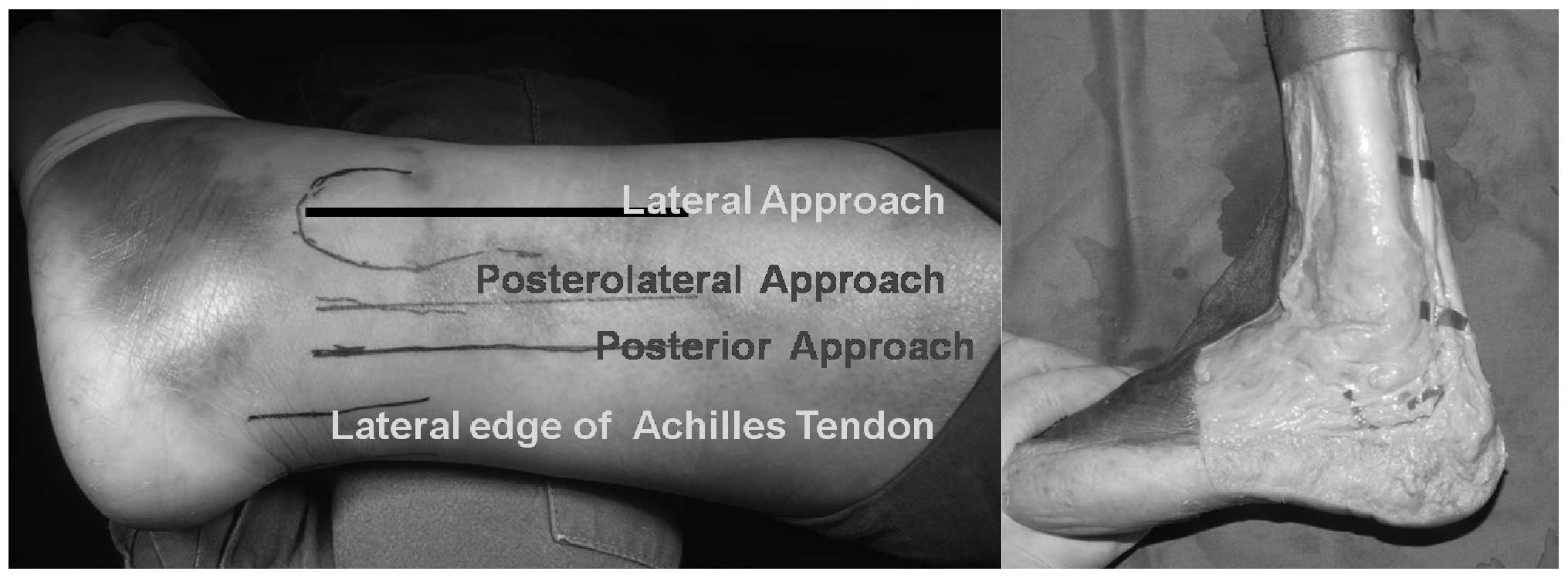
Firstly, the skin and superficial fascia were
dissected in the posterolateral region of the ankle joint while the
sural nerve and superficial peroneal nerve were preserved for
further measurements. Then, the posterior, lateral and
posterolateral approaches to the fibula were simulated in this
region (Fig. 1) and steel plates
were placed on the corresponding exposed fibular surface in order
to test whether they injured the adjacent structures.
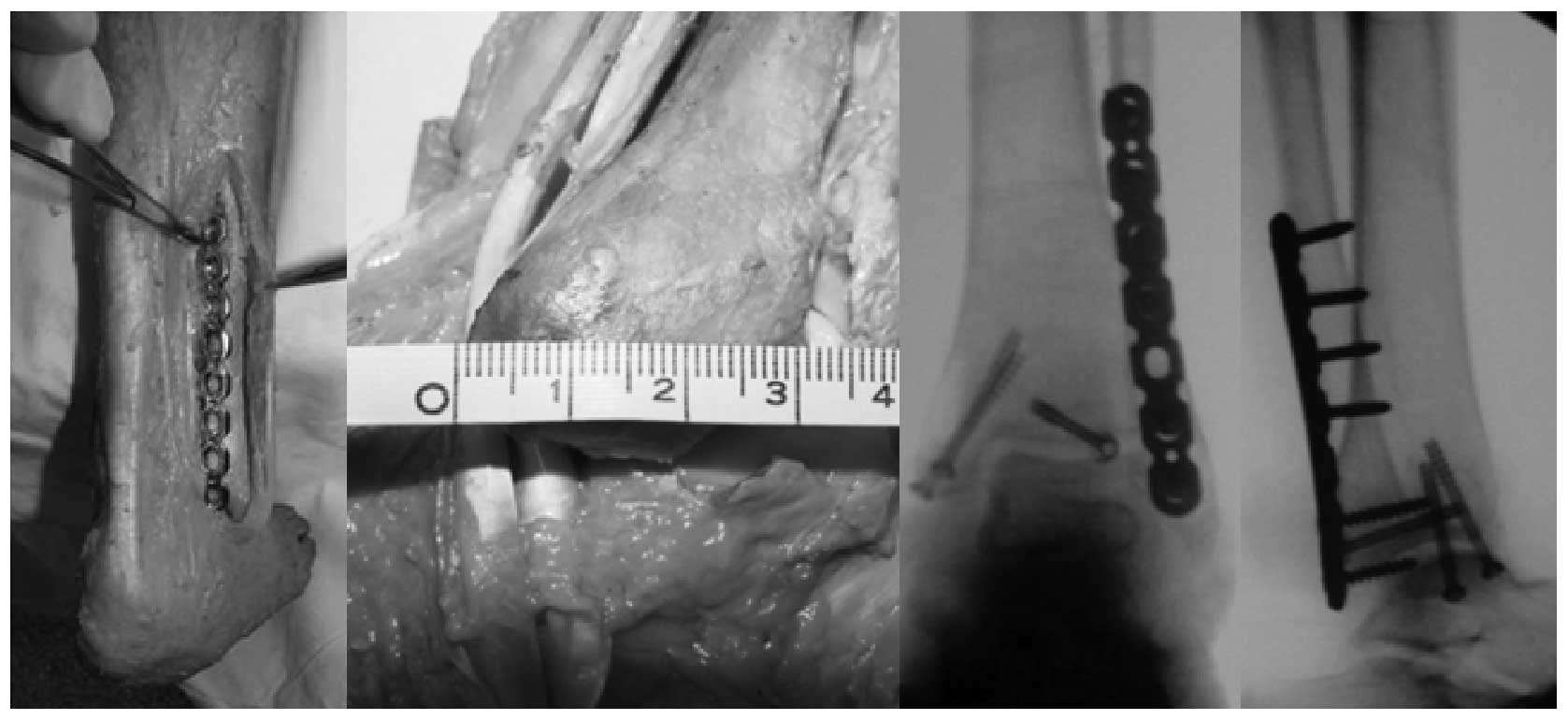
During the procedure, several measurements were
taken for each of the specimens, including the distances between
the lateral malleolus tip and the location of the transition from a
tubular to a triangular shape in the fibula, between the lateral
malleolus tip and the muscle belly of the jointed peroneal and
flexor hallux longus muscles (Fig.
2) and between the sural nerve and the posterior section of the
fibula and the anteroposterior diameter at the widest point of the
distal fibula.
Results
Distance between the sural nerve and
posterior section of the fibula
The distance between the sural nerve and most
prominent section of the posterior edge of the lateral malleolus
was 7.2±4.1 mm.
Distance between the lateral malleolus
tip and lower fibula
The average distance between the lateral malleolar
tip and the point where the shape changes in the lower fibula was
79.2±23.5 mm.
Distance between the lateral malleolus
and the tendons
The distance between the lateral malleolus and
jointed tendons of the peroneal and flexor hallux longus muscles
was 66.4±17.4 mm.
Diameter of distal fibular
The anteroposterior diameter at the widest point of
the distal fibula was 27.3±3.5 mm (Fig. 5).
Distance between the fibular tip and
superficial peroneal nerve
The distance between the point where the superficial
peroneal nerve crossed through the deep fascia and anterior edge of
the fibula was 3±3 mm. The height of the point had large variations
between individuals. The lowest position occurred at ∼5 cm from the
proximal end of the fibula tip.
Discussion
The lateral incision is the most commonly used
approach to access and expose distal fibula in the surgical
treatment of malleolar fractures. The measurements taken in the
current study showed that the mean distance between the penetration
point of the superficial peroneal nerve and anterior edge of the
fibula was 3±3 mm, while the horizontal distance between the sural
nerve and the most prominent section of the posterior edge of the
lateral malleolus was 7.2±4.1 mm. These results demonstrated that
the lateral incision was located exactly between these two
vulnerable nerves and the exposure area was a relatively safe area
in which to place a steel plate (Fig.
1).
However, the height of the penetrating position of
the superficial peroneal nerve varied greatly. The lowest position
was ∼5 cm proximal to the fibula tip. This result was similar to
that of Kim et al(15) who
also reported a 5-cm distance to where the nerve penetrated the
deep fascia. Thus, if a steel plate placed on the lateral side of
the fibula is too long, the plate may stimulate the superficial
peroneal nerve in individuals with a low penetrating point
(Fig. 3).
The distal end of the posterolateral incision is
adjacent to the sural nerve and the small saphenous vein and the
surgeon should be careful in this area (16). The majority of the posterior
malleolus may be exposed with the separation of the flexor hallucis
longus tendon from the posterior malleolus (Fig. 4), although perforators of the
peroneal artery and the accompanying veins were occasionally
observed at the distal part of this incision.
The Danis-Weber classification system not only
indicates the injuries relative to the distal tibiofibular
syndesmosis, but also aids surgeons in selecting the location of
the fibular incision (7,17). For type A and B fractures, the
steel plate is placed on the lateral side of the fibula using a
lateral incision and the distal end is usually fixed with one or
two unicortical cancellous bone screws. The lateral placement of
the steel plate on the lateral side of the fibula facilitates the
screw placement in the tibiofibular syndesmosis and stabilizes the
reduced tibiofibular syndesmosis. However, it does not provide a
direct visual field for reduction and fixation under the conditions
of combined posterior malleolus fractures.
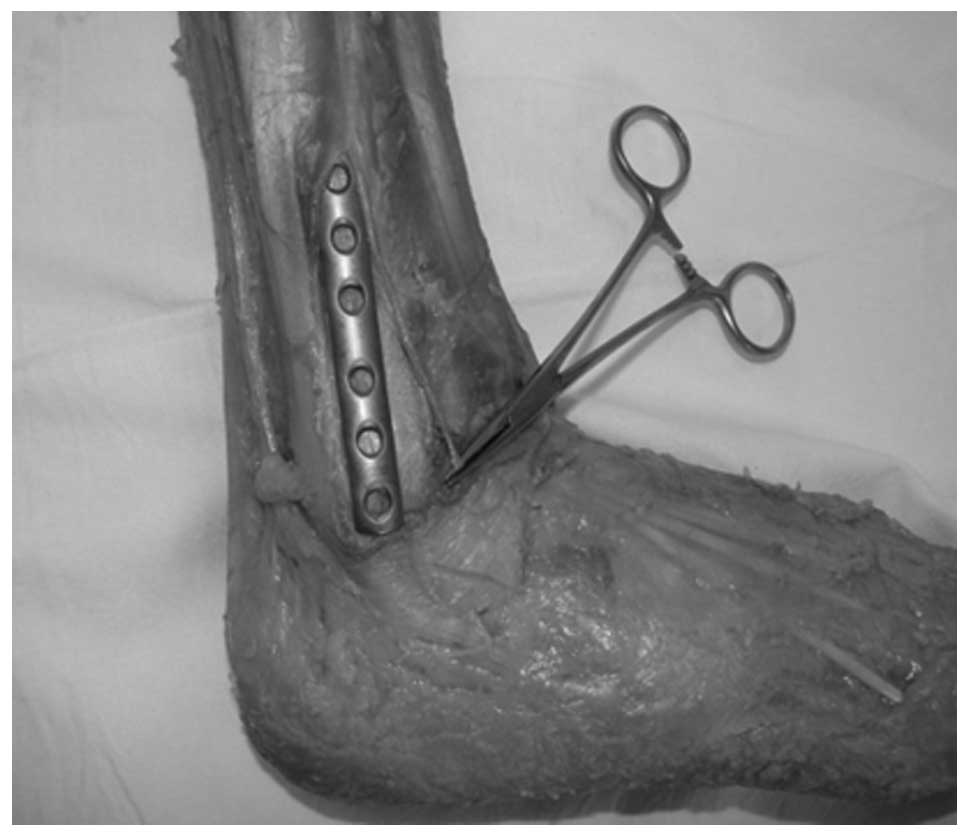
The distal fibula and the ligament behind the distal
tibiofibular syndesmosis were directly visible for anatomical
reduction through a posterior incision and it was possible to place
a steel plate at the outer posterior peroneal tendon groove. Since
the anteroposterior diameter of the lateral malleolus was 27.3±3.5
mm according to the present measurements, it was possible to place
two 25–30-mm cancellous bone screws at the distal fracture line for
bicortical fixation. Commonly used large-end screws should be
avoided in such conditions since they may cause peroneal tendon
irritation (Fig. 6).
Posterolateral incisions are not appropriate for type A or B
fractures due to the blockage of the peroneal tendon.
For type C fractures, the incision choice should be
based on the height of the fracture line. If the fracture line is
located below one-third of the distal end of the fibula, we suggest
a posterior approach as the preferred choice and a steel plate may
be placed under such conditions by properly rotating the lower
fibula. This suggestion is mostly based on the present measurement
results. The cross-section of the distal fibula diaphysis gradually
transforms from a round shape to a triangular shape at a height of
79.2±23.5 mm relative to the tip. Thus, plates placed on either the
posterior or the lateral side may encounter a ridge. However, a
flat plane may be obtained on the posterior side after the distal
fibula is appropriately rotated. If the fracture line is above
one-third of the distal end of the fibula, a lateral fibular
incision would be more suitable for these patients. This suggestion
is mainly due to the observation that the fibers between the
peroneal and flexor hallux longus muscles were intertwined with
each other at this segment. Therefore, the posterior approach,
which requires a separation of the peroneal and flexor hallux
longus muscles, may aggravate the injury and cause hemorrhaging in
the flexor hallux longus muscle.
Furthermore, in patients with trimalleolar
fractures, a posterior approach to the fibula requires the surgeon
to change the patient’s position during surgery, increasing the
complexity of the procedure.
Since the majority of posterior malleolus fracture
fragments are reset with the lateral malleolus using the pulling
tension from the ligament behind the distal tibiofibular
syndesmosis, clinicians commonly use hollow screws for
anteroposterior fixation. However, this is an indirect reset and
does not completely confirm the anatomical reduction and
stabilization of the fracture. The conventional lateral approach to
the fibula has its limitations in the exposure of posterior
malleolus fracture fragments as it cannot provide a direct view of
them. However, the posterolateral as well as the posterior approach
may achieve an improved exposure.
According to the Haraguchi classification system,
the posterolateral approach is suitable for type I posterior
malleolus fractures due to its complete exposure of the
posterolateral corner of the posterior malleolus. For the type II
fractures commonly observed in clinical practice, the
postero-lateral approach provides limited exposure of the fracture
fragments on the medial side. The posterior approach is able to
completely expose the posterior malleolus fracture line and provide
a direct view of the resetting.
The anatomy of the distal fibula indicates that the
selection of an incision is affected by multiple factors for the
commonly observed fibular fractures accompanied by posterior
malleolus fractures. Although the fracture site, the fracture shape
and the internal fixation must be considered, so too must the
surgical techniques that the surgeon is familiar with and able to
perform. Moreover, other conditions associated with ankle joint
stabilization should be considered, such as whether to explore and
repair the medial triangular ligament and whether to use a distal
tibiofibular syndesmosis screw. The goal is to restore the
stability of the ankle joint and provide good ankle joint function.
The clinical application of new types of internal fixation material
is also likely to promote progress in the treatment of ankle
fractures.
References
|
1.
|
Salai M, Dudkiewicz I, Novikov I, Amit Y
and Chechick A: The epidemic of ankle fractures in the elderly - is
surgical treatment warranted? Arch Orthop Trauma Surg. 120:511–513.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Sanders DW, Tieszer C and Corbett B;
Canadian Orthopedic Trauma Society: Operative versus nonoperative
treatment of unstable lateral malleolar fractures: A randomized
multicenter trial. J Orthop Trauma. 26:129–134. 2012. View Article : Google Scholar
|
|
3.
|
Smith G: The isolated lateral malleolar
fracture: Where are we and how did we get here? Surgeon. Mar
27–2012.(Epub ahead of print).
|
|
4.
|
Lin CW, Moseley AM and Refshauge KM:
Effects of rehabilitation after ankle fracture: a Cochrane
systematic review. Eur J Phys Rehabil Med. 45:431–441.
2009.PubMed/NCBI
|
|
5.
|
Harper MC: Ankle fracture classification
systems: a case for integration of the Lauge-Hansen and
AO-Danis-Weber schemes. Foot Ankle. 13:404–407. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Talbot M, Steenblock TR and Cole PA:
Posterolateral approach for open reduction and internal fixation of
trimalleolar ankle fractures. Can J Surg. 48:487–490.
2005.PubMed/NCBI
|
|
7.
|
Koval KJ, Lurie J, Zhou W, et al: Ankle
fractures in the elderly: what you get depends on where you live
and who you see. J Orthop Trauma. 19:635–639. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Henderson MS: Trimalleolar fractures of
the ankle. J Surg Clin North Am. 12:867–872. 1932.
|
|
9.
|
Forberger J, Sabandal PV, Dietrich M,
Gralla J, Lattmann T and Platz A: Posterolateral approach to the
displaced posterior malleolus: functional outcome and local
morbidity. Foot Ankle Int. 30:309–314. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Hersh IR and Fleming JJ: Considerations of
a midline posterior approach to the ankle and subtalar joints. J
Foot Ankle Surg. 51:482–486. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Ferries JS, DeCoster TA, Firoozbakhsh KK,
Garcia JF and Miller RA: Plain radiographic interpretation in
trimalleolar ankle fractures poorly assesses posterior fragment
size. J Orthop Trauma. 8:328–331. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Gardner MJ, Brodsky A, Briggs SM, Nielson
JH and Lorich DG: Fixation of posterior malleolar fractures
provides greater syndesmotic stability. Clin Orthop Relat Res.
447:165–171. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Sen T, Basarir K, Esmer AF, Armangil M,
Tuccar E and Karahan ST: Lateral approach to the ankle and distal
leg. Folia Morphol (Warsz). 70:91–94. 2011.PubMed/NCBI
|
|
14.
|
Abdelgawad AA, Kadous A and Kanlic E:
Posterolateral approach for treatment of posterior malleolus
fracture of the ankle. J Foot Ankle Surg. 50:607–611. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Kim HJ, Oh JK, Oh CW, Hwang JH and Biswal
S: Anterior transposition of the superficial peroneal nerve branch
during the internal fixation of the lateral malleolus. J Trauma.
68:421–424. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Haraguchi N, Haruyama H, Toga H and Kato
F: Pathoanatomy of posterior malleolar fractures of the ankle. J
Bone Joint Surg Am. 88:1085–1092. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Fitzpatrick DC, Otto JK, McKinley TO,
Marsh JL and Brown TD: Kinematic and contact stress analysis of
posterior malleolus fractures of the ankle. J Orthop Trauma.
18:271–278. 2004. View Article : Google Scholar : PubMed/NCBI
|