Introduction
The normal coronary artery and its main branch are
mostly located in the epicardial adipose tissue. If the original
trabecular artery network fails to move outward in the coronary
artery development process, any one segment of the coronary artery
or its branch is covered by cardiac muscle fiber. This segment of
vessel is called a mural coronary artery (MCA), while the
bridge-like myocardial fiber bundle covering the artery is called a
myocardial bridge (MB). In addition, ‘MB-MCA’ is a complex and is
usually called ‘MB’ in the clinic (1). Previously it was understood that
MB-MCA was a benign anatomical variant and patients may have no
clear symptoms for a long time. At present, a number of patients
present with myocardial ischemia and the symptom becomes
aggravated, particularly in the case of tiredness, movement and
agitation. This may cause stenocardia, ventricular tachycardia,
atrioventricular block, acute coronary syndrome, myocardial
stunning and even sudden cardiac failure. It is clear that a MB may
cause changes to the MCA stressed by it and hemodynamic
abnormalities and may cause cardiac events to occur to different
extents (2). In the clinic, MB-MCA
diagnosis mainly depends on the conventional coronary angiography
(CAG) examination. The characteristics of MCA include stenosis in
systole and its restoration to the normal level in diastole,
presenting a typical ‘milking effect’. However, CAG only
demonstrates the persistence of MB-MCA indirectly by observing
changes in vessel diameter size at systole and diastole, but it
does not directly show the internal and external situations of
blood vessel lumen. Only MB-MCA with an marked stenosis may be
identified, while a case with superficial stenosis is easily
missed. Therefore, the detection rate of CAG is low, only 0.5–16%
(3,4). In recent years, the advanced CT
technology has improved MB detectability. Certain scholars have
used l6- and 64-slice CT to investigate the MB detection rate, and
these studies have shown that multiple-slice spiral CT is an
effective measure for detecting MB and intuitively shows the
thickness, length and imaging characteristics of MB-MCA (5–7). In
the present study, a retrospective analysis was conducted of the
data from 580 patients with suspected coronary artery lesions
receiving 128-slice spiral CT coronary artery angiography (MSCTCA)
and the detection rate of MB-MCA was determined. In addition, the
left anterior descending branch (LAD) was investigated to observe
the correlations of MCA compression extent in systole with MB
length and thickness to provide clinical scientific imaging
data.
Materials and methods
Patients
Data from 580 cases of outpatients and inpatients
who received 128-SCTCA in The First Affiliated Hospital of Liaoning
Medical University between January, 2011 and December, 2011 were
collected. The ages of the patients ranged from 38 to 88 years old
and the mean age was 57±12.5 years old. There were 316 male and 264
female cases. Inclusion criteria: patients with clinically
suspected coronary heart disease and patient with symptoms of chest
tightness, precordial discomfort and effort angina. Disease
histories ranged from 1 month to 10 years and written informed
consent was obtained from all patients. The present study was
approved by the ethics committee of The First Affiliated Hospital
of Liaoning Medical University, Jinzhou, China
Scanning method and parameters
A Definition AS+ scanner (64-detector 128-slice CT;
Siemens, Munich, Germany) was used to conduct calcium scoring plain
multislicespiral CT (MSCT) scanning. Subsequently, non-ionic
contrast agent (iobitridol, 350 mgI/ml, 65–70 ml) was injected with
a high pressure injector via the antecubital vein at a rate of
3.5–5.0 ml/sec and 40 ml normal saline was injected to reduce
contrast agent dosage and streak artifacts caused by the
concentration of the contrast agent being too high in the superior
vena cava and right atrium. The aortic root was set as the region
of interest (ROI) and the trigger threshold was set as 100 HU.
Contrast agent automatic tracking film scanning (timing bolus) was
conducted to generate a time-density curve (TDC) and calculate scan
delay time. Enhanced scanning of the coronary artery was conducted
from the tracheal carina to the diaphragmatic surface of heart
under the retrospective electrocardiographically-gated control for
6–11 sec. The scanning parameters were as follows: voltage, 120 kV;
current, automatic mA; field of vision (FOV), 160–220 mm; screw
pitch, 0.2–0.5; detector collimating value, 64x0.6 mm; acquisition
slice thickness, 0.6 mm; rotation speed, 0.33 sec/r; matrix,
512x512; convolution kernel, B26f. In addition, the heart rate was
controlled at 75 bpm. For patients with a heart rate >75 bpm,
metoprolol (25–50 mg) was provided by sublingual administration 30
min prior to examination to reduce the heart rate.
Image processing
Circulation software (Siemens) was used to conduct
post processing of the optimum images in diastole and systole, and
included multiple planar reconstruction (MPR), curve planar
reconstruction (CPR), volume rendering technology (VRT), maximum
intensity projection (MIP) and Angioview DSA tumbling technology
which were used to evaluate the coronary artery. At the 10% R-R
interval (the interval between two QRS complexs), a 0–100% R-R
interval image was reconstructed. In addition, the Inspace software
4D movie mode was used to observe whether the ‘milking effect’ in
systole existed in the MCA segment.
Image analysis and measurement
The location of the coronary artery with respect to
the cardiac muscle was observed. When one segment of the coronary
artery was embedded in cardiac muscle or >1/2 the diameter of a
segment was surrounded by cardiac muscle or fibrous tissue, while
its proximal and distal segments ran in epicardial fat tissues,
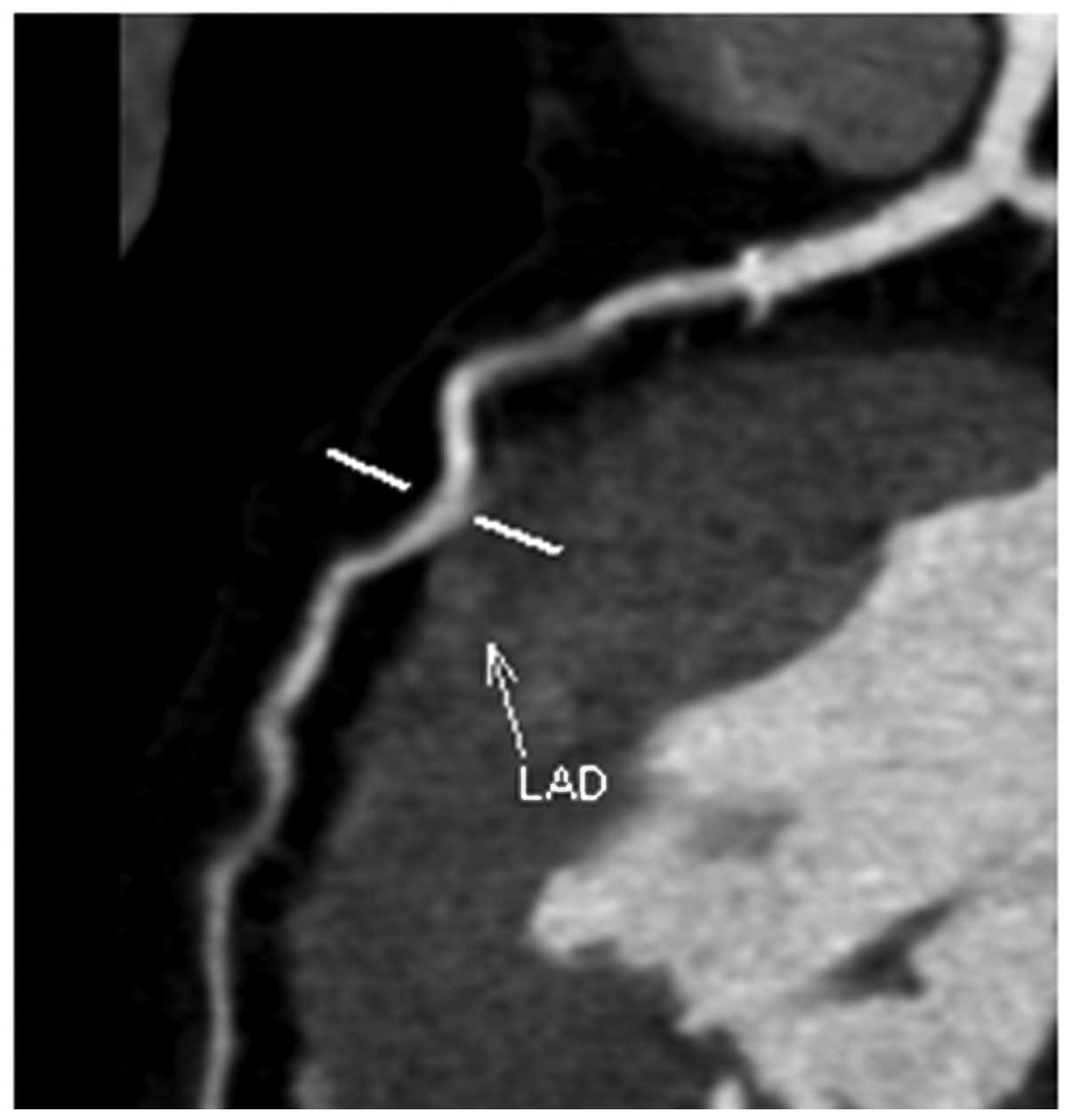
this segment of coronary artery was evaluated as MCA (8). CPR images of MCA showed ‘step up-step
down’ or ‘cosine curve’-like changes on the myocardial surface
after running in cardiac muscle for a certain distance (Fig. 1). In addition, MB position, length,
depth and compression extent in systole were recorded. i) Position:
the coronary artery modification 17-segment model of the American
Heart Association (AHA) (9) was
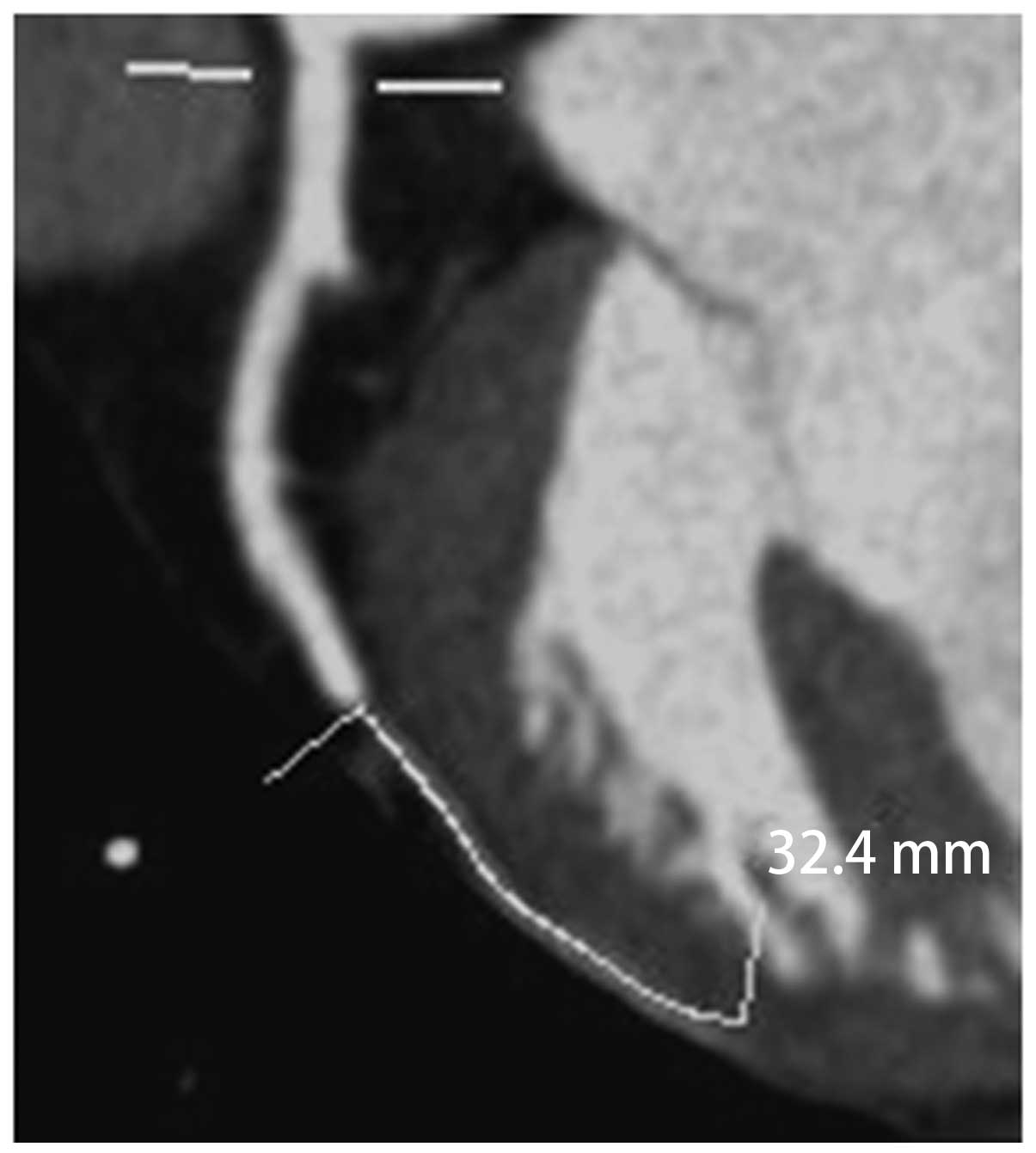
used to identify the location. ii) MB length: curved surface length
of MCA surrounded by cardiac muscle (Fig. 2); iii) MB thickness: the shortest
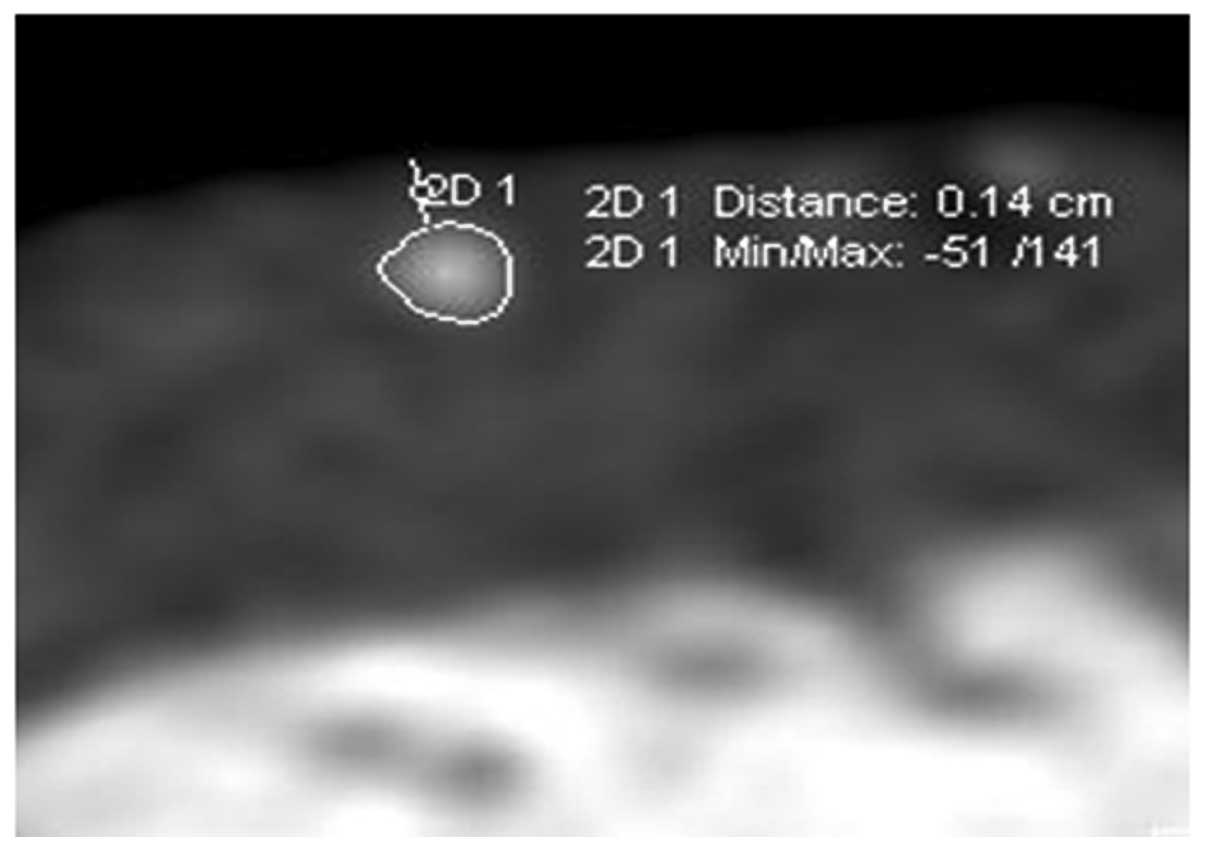
distance from the vascular wall of the MCA to the myocardial
membrane, which was measured at the thickest myocardial cover on
MCA cross section (adjust the optimum width and position for
observations; Fig. 3); iv) MCA
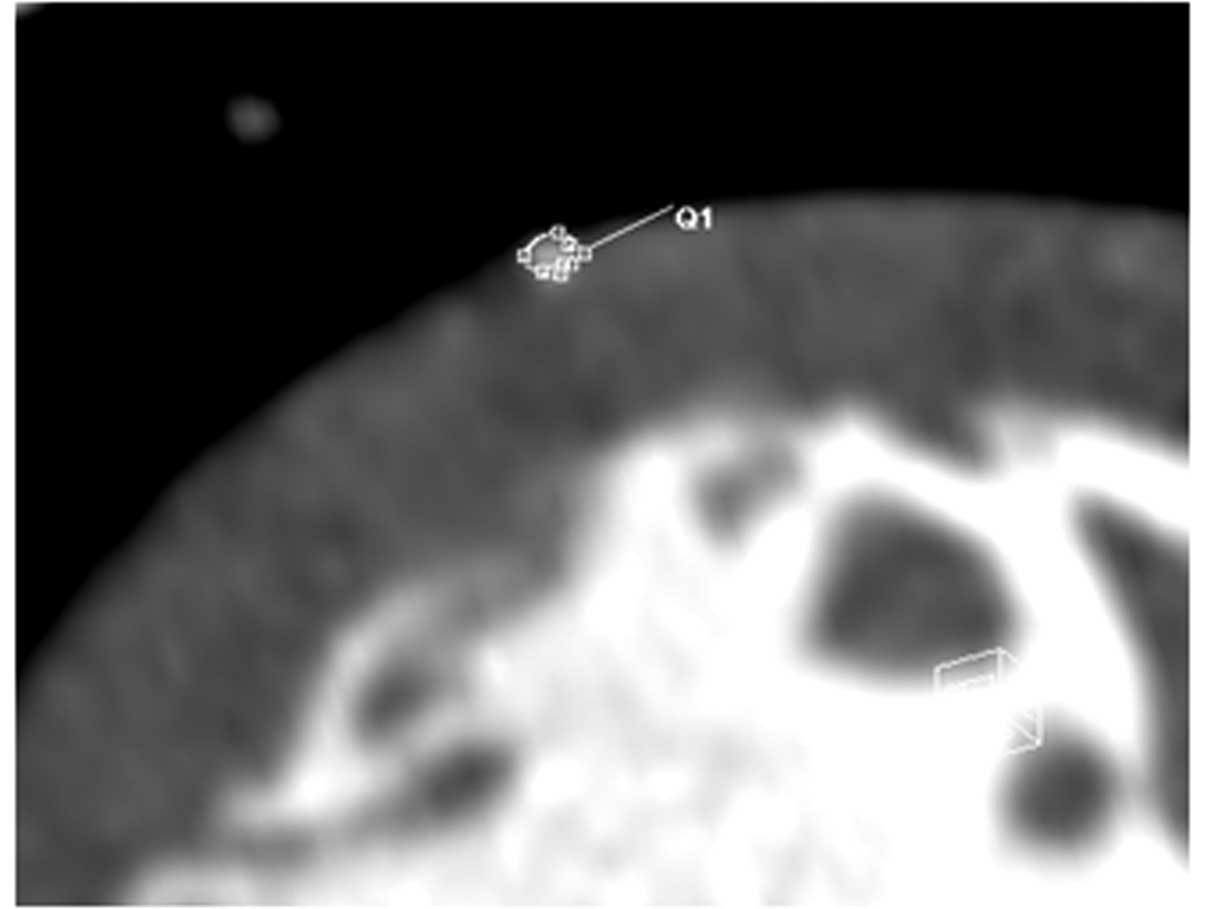
compression extent in systole: the cross-sectional area method was
used for evaluation. Rotation was conducted in a vascular CPR image
to identify the narrowest position and the short axis lumen areas
in diastole and systole (Fig. 4),
and the following calculation was performed: MCA compression extent
= vascular area of MCA in diastole - vascular area of this segment
of MCA in systole / vascular area of MCA in diastole. This process
was completed by two physicians with the title of associate chief
physician or above.
Grouping and statistical processing
The cases of LAD with MB were divided into three
groups according to the MB-MCA compression extent 3-grade
classification method of Noble et al(9,10):
the mild group (compression extent <50%), the moderate stenosis
group (compression extent 50–75%) and the severe stenosis group
(compression extent >75%). SPSS 17.0 software (SPSS, Chicago,
IL, USA) was used for statistical processing, and measurement data
are expressed as the mean ± standard deviation (mean ± SD). The
Student’s t-test was used for comparison of measurement data and
the Chi-square test was used for comparison of enumerated data.
P<0.05 was considered to indicate a statistically significant
result.
Results
General data
Among the 580 cases who were analyzed, 140 cases
presented with MB-MCA and the detection rate was 24.14%. The
occurrence sites and constituent ratios are shown in Table I. Among them, 120 cases in which
the MB-MCA was located in the LAD, (104 in the middle segment + 16
in the distal segment) were investigated. The MB length ranged
between 8 and 46 mm, the mean length was 21.80±5.98 mm, the
thickness ranged between 0.7 and 4.4 mm and the mean thickness was
2.15±0.74 mm. The range of the compression extent was between 0 and
69.4% and the mean compression extent was 38.5±19.6%. There were 86
cases of mild stenosis, 26 cases of moderate stenosis and 8 cases
of severe stenosis. Among the different groups, no significant
difference in MB length was observed (P>0.05) but there were
significant differences in MB thickness (P<0.05; Table II).
 | Table I.MB-MCA locations and constituent
ratios. |
Table I.
MB-MCA locations and constituent
ratios.
| Incidence | Middle segment of
LAD | Distal segment of
LAD | LCX-OM | 1st D | Intermediate
branch | RCA-PD | Total |
|---|
| No. of cases | 104 | 16 | 8 | 7 | 3 | 2 | 140 |
| Constituent ratios
(%) | 74.3% | 11.4% | 5.7% | 5.0% | 2.1% | 1.5% | 100% |
 | Table II.Correlations of the MCA systolic
compression extent with the length and thickness of the MB. |
Table II.
Correlations of the MCA systolic
compression extent with the length and thickness of the MB.
| Muscle bridge | Mild stenosis group
(n=86) | Moderate stenosis
group (n=26) | Severe stenosis group
(n=8) | F | P-value |
|---|
| Length (mm) | 21.18±5.85 | 23.91±5.48 | 21.81±5.97 | 2.139 | 0.122 |
| Thickness (mm) | 1.94±0.63 | 2.51±0.71 | 3.24±0.76 | 19.213 | 0.000 |
Correlation analysis
Pearson’s correlation analysis was conducted for the
correlations of MCA compression extent in systole with MCA length
and thickness. The extent of MCA compression was linearly
correlated with MB thickness (r=0.408, P<0.05) but was unrelated
to MB length (r=0.076, P>0.05; Table II, Figs. 3 and 4). This suggests that the thicker the MB,
the more marked the MB stress to the MCA, and that the MCA
compression extent was not influenced by the MB length.
Discussion
As a new noninvasive technique, MSCTCA has been
widely applied in the clinic, and markedly increases the detection
rate of MB. In the present study, the detection rate of 128-slice
SCTCA was 24.14% which is comparable to the detection rate (15–85%)
of autopsy and higher than that of CAG (0.5–16%). This may be due
to the ability of MSCTCA imaging to directly show coronary artery
segments that run in cardiac muscle or are partly covered by
cardiac muscle. MSCTCA also directly reveals the MB, measures the
MB thickness and length, and evaluates the extent of MB lumen
compression in systole and the presence of plaques before and after
the MCA vessel segment. A ‘milking effect’ may be observed by use
of a 4D movie mode. MB-MCA often occurs in the middle and distal
segments of the LAD and the coronary artery of left ventricular
anterior wall, including the left circumflex-obtuse marginal
branch, intermediate branch and diagonal branch. They respectively
account for 74.3, 11.4, 5.7, 2.1 and 5.0% of cases, while MB-MCA
occurs less frequently in the right coronary artery; the number of
right coronary artery cases only accounts for 1.5% of those in the
present study, which is almost in agreement with literature values
(9–11).
According to the depth (2 mm) by which the MCA is
embedded by cardiac muscle, MB is divided into superficial and deep
types. The majority of MB cases belong to the superficial type
which generally do not cause marked stenosis of the MB segment of
the coronary artery in systole, but the deep type may stress and
twist vessels, which not only causes MCA stenosis in systole and
blood perfusion, but also influences the blood perfusion in the
early and medium diastole to cause a clear decrease of coronary
flow reserve. In addition, the MCA readily undergoes spasm and
secondary atherosclerosis and develops plaque rapture, hemorrhage
and thrombosis, thus causing myocardial ischemia and even acute
coronary syndrome (ACS). In the present study, 120 cases of
patients with MB occurring in the anterior descending branch were
grouped according to the MCA compression extent in systole.
Comparisons among various groups indicate that that extent of MCA
compression correlates with MB thickness but not with MB length,
which is in agreement with literature findings (9–13).
If the MB thickness is increased, the MCA compression caused by the
MB in systole is more evident, and myocardial ischemia symptoms are
more severe. Myocardial ischemia is closely correlated with the
extent of compression of the MCA, while the latter directly
influences the internal diameter of the MCA lumen. According to
Poiseuille’s law, blood flow resistance is inversely proportional
to the biquadratic of vascular radius. Therefore, MCA compression
extent is a main factor causing hemodynamic change. Recent studies
also suggest that pressure increases and vortex generation in
proximal segments of the MB are the main factors causing atherosis
(14,15). As MB-MCA is stressed in systole,
long-term compression inevitably causes local vessels to generate
high shear stress changes. In addition, electron microscopy and
intravascular ultrasound (IVUS) examinations show that endothelial
cells of the MB are elongated and almost cover the basal lamina
surface. The basal lamina surface is covered with microvilli. While
the endothelial cells of the coronary artery in the proximal MB
mostly present flap or oval shapes, the cell surfaces present rough
worm-eaten-like defects. The vessels in the distal segment of the
MB are in a relatively low pressure state and the surfaces present
fewer worm-eaten-like defects, which is possibly associated with
the anti-atherosclerosis effect of high shear stress. As high shear
stress usually induces endothelial cells of the MCA to express
vascular relaxing factor, growth inhibiting factor, fibrinolysis
substance and antioxidant, and inhibits the expression of vascular
contraction factor, growth factor, inflammatory mediator and
adhesion factor, it cannot easily damage endothelial cells and is
detrimental for cellular proliferation, lipid uptake and blood cell
adhesion. Thus, high shear stress has an anti-AS effect. In
addition, the position of the MB has a certain influence on
myocardial ischemia. If it is closer to the coronary sinus,
particularly for thicker MB, its stress to vessels is marked
(14–16).
In summary, 128-slice SCTCA directly reveals the
positions of MCA and cardiac muscle, but also dynamically evaluates
the presence of MCA-MB and dynamically shows changes of MCA lumen
size by exhibiting the ‘milking effect’ with a 4D movie mode. In
particular, 128-slice SCTCA is more sensitive for the detection of
superficial MBs. In addition, 128-slice SCTCA further enables the
determination of MB thickness and length and compression extent in
systole. Therefore, 128-slice SCTCA may provide extensive imaging
information for the preoperative evaluation of surgical muscle
bridge lysis and thereby guide surgery. Furthermore, 128-slice
SCTCA may provide a basis for the preoperative judgement of MB
position, thickness, length and compression extent in
interventional treatment and the accurate and effective selections
of stent type and length, which increases the treatment success
rate (17–20). However, this study also shows
certain shortcomings (the diagnosis results are not comparable with
those of the pathological gold standard and the technique is unable
to calculate to high sensitivity and specificity) due to the
spatio-temporal resolution limitations of MSCT and the influence of
motion artifacts on compression extent accuracy. Therefore, it is
necessary to conduct further modifications and studies.
References
|
1.
|
Goitein O and Lacomis JM: Myocardial
bridging: noninvasive diagnosis with multidetector CT. J Comput
Assist Tomogr. 29:238–240. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Argyriou M, Filippatos GS, Antonellis J
and Kranidis A: Myocardial infarction and ventricular septal
rupture caused by myocardial bridging. Eur J Cardiothorac Surg.
25:6432004. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Duygu H, Zoghi M, Nalbantgil S, et al:
Myocardial bridge: a bridge to atherosclerosis. Anadolu Kardiyol
Derg. 7:12–16. 2007.PubMed/NCBI
|
|
4.
|
Mollet NR, Cademartiri F, van Mieghem CA,
et al: High-resolution spiral computed tomography coronary
angiography in patients referred for diagnostic conventional
coronary angiography. Circulation. 112:2318–2323. 2005. View Article : Google Scholar
|
|
5.
|
Zeina AR, Odeh M, Blinder J, Rosenschein U
and Barmeir E: Myocardial bridge: evaluation on MDCT. AJR Am J
Roentgenol. 188:1069–1073. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Kantarci M, Duran C, Durur I, et al:
Detection of myocardial bridging with ECG-gated MDCT and
multiplanar reconstruction. AJR Am J Roentgenol. 186(Suppl 2):
S391–S394. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Hazirolan T, Canyigit M, Karcaaltincaba M,
et al: Myocardial bridging on MDCT. AJR Am J Roentgenol.
188:1074–1080. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Liu SH, Yang Q, Chen JH, Wang XM, Wang M
and Liu C: Myocardial bridging on dual-source computed tomography:
degree of systolic compression of mural coronary artery correlating
with length and depth of the myocardial bridge. Clin Imaging.
34:83–88. 2010.
|
|
9.
|
Kawawa Y, Ishikawa Y, Gomi T, et al:
Detection of myocardial bridge and evaluation of its anatomical
properties by coronary multislice spiral computed tomography. Eur J
Radiol. 61:130–138. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Lee Y, Naseem RH, Park BH, et al:
Alpha-lipoic acid prevents lipotoxic cardiomyopathy in acyl
CoA-synthase transgenic mice. Biochem Biophys Res Commun.
344:446–452. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Leschka S, Koepfli P, Husmann L, et al:
Myocardial bridging: depiction rate and morphology at CT coronary
angiography - comparison with conventional coronary angiography.
Radiology. 246:754–762. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Kurisu S, Inoue I, Kawagoe T, et al: Acute
myocardial infarction associated with myocardial bridging in a
young adult. Intern Med. 43:1157–1161. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Jodocy D, Aglan I, Friedrich G, et al:
Left anterior descending coronary artery myocardial bridging by
multislice computed tomography: correlation with clinical findings.
Eur J Radiol. 73:89–95. 2010. View Article : Google Scholar
|
|
14.
|
Atar E, Kornowski R, Fuchs S, Naftali N,
Belenky A and Bachar GN: Prevalence of myocardial bridging detected
with 64-slice multidetector coronary computed tomography
angiography in asymptomatic adults. J Cardiovasc Comput Tomogr.
1:78–83. 2007. View Article : Google Scholar
|
|
15.
|
Kim PJ, Hur G, Kim SY, et al: Frequency of
myocardial bridges and dynamic compression of epicardial coronary
arteries: a comparison between computed tomography and invasive
coronary angiography. Circulation. 119:1408–1416. 2009. View Article : Google Scholar
|
|
16.
|
Chen YD, Wu MH, Sheu MH and Chang CY:
Myocardial bridging in Taiwan: depiction by multidetector computed
tomography coronary angiography. J Formos Med Assoc. 108:469–474.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Ko SM, Kim NR, Kim DH, Song MG and Kim JH:
Assessment of image quality and radiation dose in prospective
ECG-triggered coronary CT angiography compared with retrospective
ECG-gated coronary CT angiography. Int J Cardiovasc Imaging.
26(Suppl 1): 93–101. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Kim SS, Ko SM, Song MG and Hwang HG:
Systolic luminal narrowing and morphologic characteristics of
myocardial bridging of the mid-left anterior descending coronary
artery by dual-source computed tomography. Int J Cardiovasc
Imaging. 27(Suppl 1): 73–83. 2011.
|
|
19.
|
Hwang JH, Ko SM, Roh HG, et al: Myocardial
bridging of the left anterior descending coronary artery: depiction
rate and morphologic features by dual-source CT coronary
angiography. Korean J Radiol. 11:514–521. 2010.PubMed/NCBI
|
|
20.
|
Kim SY, Lee YS, Lee JB, et al: Evaluation
of myocardial bridge with multidetector computed tomography. Circ
J. 74:137–141. 2010. View Article : Google Scholar : PubMed/NCBI
|