Introduction
Ischemic stroke, a commonly encountered and
frequently occurring clinical disease, is a complication of
hypertension, heart disease and diabetes mellitus (1), which occurs when the blood supply to
a part of brain is interrupted or severely reduced, resulting in
oxygen and nutrient deprivation in brain tissues (2). Acupuncture, a medicinal methodology
originating in ancient China, has long been used as a complementary
and alternative therapy in a number of East Asian countries as well
as more recently in Western society (3). The clinical efficacy of acupuncture
in stroke rehabilitation has been demonstrated in numerous studies
(4–9) and the Zusanli (ST36) and Quchi (LI11)
acupoints are the acupoints most commonly used to clinically treat
stroke in China (10,11). However, the precise mechanism of
the neuroprotective effect remains to be elucidated.
The pathogenic mechanisms of ischemic stroke are
complex. During ischemia/reperfusion (I/R) injury, cells undergo
rapid changes which lead to perturbations in signaling pathways,
resulting in an imbalance between cell proliferation and apoptosis
(12,13). Extracellular signal-regulated
kinase (ERK) signaling is one of the major cell-survival and
proliferation pathways. As a major subfamily of the
mitogen-activated protein kinases (MAPKs), the activation of ERKs
is regulated by a central three-tiered kinase core consisting of a
MAPK kinase kinase (e.g., Raf), MAPK kinase (e.g., MEK) and MAPK,
wherein Raf phosphorylates MEK which in turn phosphorylates and
activates the ERK (14). By
altering the levels and activities of transcription factors, the
activation of the ERK pathway regulates the expression of various
cell cycle-regulatory genes, including cyclin D1 and
cyclin-dependent kinase (CDK)4, thus mediating the promotion of
cell proliferation (15,16). The role of the ERK pathway in
cerebral I/R injury has been studied intensively (17–19),
suggesting that the activation of ERK signaling is a promising
target for stroke treatment.
In present study, a focal cerebral I/R-injured rat
model was used to elucidate the neuroprotective mechanism of
electroacupuncture (EA) at the Quchi and Zusanli acupoints,
evaluate the therapeutic efficacy of EA against ischemic stroke and
investigate its effect on the ERK pathway.
Materials and methods
Materials and reagents
Ras, ERK1/2, phospho-p44/42
(Thr202/Thr204), cyclin D1 and horseradish
peroxidase (HRP)-conjugated secondary antibodies were obtained from
Cell Signaling Technology, Inc. (Beverly, MA, USA). Mouse
proliferating cell nuclear antigen (PCNA) immunohistochemical (IHC)
kits were purchased from Beijing Golden Bridge Biotechnology Co.,
Ltd. (Beijing, China), while rat CDK4 antibody was obtained from
Abcam (Cambridge, MA, USA). All other chemicals, unless stated
otherwise, were obtained from Sigma-Aldrich (St. Louis, MO,
USA).
Animals
Male Sprague-Dawley rats (initial body weights ∼250
g) were obtained from Shanghai SLAC Laboratory Animal Co., Ltd.
(Shanghai, China) and housed under pathogen-free conditions with a
12 h light/dark cycle. Food and water were provided ad
libitum throughout the experiment. All animal treatments were
strictly in accordance with the international ethical guidelines
and National Institutes of Health guide concerning the Care and Use
of Laboratory Animals. The study was approved by the Institutional
Animal Care and Use Committee of Fujian University of Traditional
Chinese Medicine (Fuzhou, China).
Establishment of the cerebral I/R-injured
rat model and animal groups
The I/R-injured model was established by middle
cerebral artery (MCA) occlusion (MCAO) as described previously
(20). Briefly, after each rat was
anesthetized by intraperitoneal injection of 10% chloral hydrate
(300 mg/kg), the left common carotid artery (CCA), left external
carotid artery (ECA) and internal carotid artery (ICA) were
carefully exposed via a midline neck incision. The left MCA was
occluded by introducing an embolus through the ICA. The CCA and the
ECA were permanently blocked. Focal cerebral ischemia was induced
by occluding the left common carotid artery (MCA) when the tip of
catheter reached the origin of MCA (18–22 mm). Reperfusion was
achieved by removing the thread after 2 h of occlusion to restore
the blood supply to the MCA area. Heat preservation was considered
throughout the process. The rectal temperatures of the rats were
maintained at 37°C throughout the surgical procedures.
Sham-operated control (SC) animals underwent the same surgical
procedure, but no arterial occlusion was performed and no embolus
used.
The animals were randomly divided into 3 groups
(n=8) as follows: i) in the SC group, the rats underwent neck
dissection and the exposure of the blood vessels, but no arterial
occlusion; ii) in the ischemic control (IC) group, the left MCA was
blocked for 2 h and then recanalized, iii) in the EA group, the
surgical procedure was same as that in the IC group. After recovery
from the I/R surgery and 2 h of reperfusion, EA treatment was
performed daily for 30 min. Acupuncture needles (0.3 mm diameter)
were inserted 2–3 mm deep into the Quchi (LI11) and Zusanli (ST36)
acupoints on the right paralyzed limb. Stimulation was then
generated with the EA apparatus (Model G6805; SMIF, Shanghai,
China) and the stimulation parameters were set as disperse waves of
1 and 20 Hz.
Evaluation of neurological deficit
scores
At 2 or 24 h after I/R, the neurological deficit
score was examined in a blinded manner as described previously
(20): a score of 0 indicated no
neurological deficits; 1 (failure to fully extend right forepaw)
indicated mild focal neurological deficits; 2 (circling to the
right) and 3 (falling to the right) indicated moderate focal
neurological deficits; rats with a score of 4 were not able to walk
independently and exhibited a depressed level of consciousness.
Mice that scored 0 or 4 were eliminated from the experiment.
Measurement of cerebral infarct
volume
After cerebral I/R injury for 24 h, the rats were
anesthetized with 10% chloral hydrate by intraperitoneal injection.
Each rat was perfused transcardially with 0.9% NaCl and the brain
was removed. The brain was sectioned in the coronal plane into 2-mm
thick slices. The slices were placed in 2%
2,3,5-triphenyltetrazolium chloride (TTC) in phosphate-buffered
saline (PBS) at 37°C for 20 min and fixed by immersion in 4%
buffered formaldehyde solution (21). The normal area of the brain was
stained dark red based on intact mitochondrial function, whereas
the infarct area remained unstained. Each brain slice was scanned
with a high-resolution digital camera (Canon SX20; Canon Inc.,
Tokyo, Japan) and the infarct was quantified as a percentage of the
total brain volume using a Motic 6.0 system (Motic, Xiamen,
China).
Immunohistochemistry of PCNA, cyclin D1
and CDK4
Each rat was anesthetized and perfused
transcardially with 0.9% NaCl and 4% paraformaldehyde through the
left ventricle and the brain was removed. Samples were fixed in
cold 4% paraformaldehyde and processed into 5-μm thick
sections. PCNA, cyclin D1 and CDK4 levels were analyzed with an
immunohistochemistry assay kit (DS-005; Beijing Golden Bridge
Biotechnology Co., Ltd.) according to the manufacturer’s
instructions. For staining, the slides were placed in 3% hydrogen
peroxide and normal serum for 10 min at 37°C, to block nonspecific
protein activity. This was followed by an incubation at 4°C
overnight with the primary antibodies, rabbit anti-CDK4 (1:50;
Abcam), rabbit anti-cyclin D1 (1:400; Cell Signaling Technology,
Inc.) and mouse anti-PCNA (Beijing Golden Bridge Biotechnology Co.,
Ltd.). After incubation with primary antibodies, the sections were
washed three times in PBS and incubated with the secondary
antibodies. The brain sections were stained with alkaline
phosphatase (AP)-red or diaminobenzidine (DAB) staining solutions.
PCNA-positive cells were stained red, while cyclin D1 and
CDK4-positive cells were stained sepia. Positive cells were counted
in four randomly selected microscopic fields at ×400 magnification.
The positive rate was expressed as the ratio of red- or
sepia-stained cells.
Western blotting analysis
Ischemic cerebral tissues were homogenized in
nondenaturing lysis buffer and centrifuged at 12,000 × g for 15
min. The supernatants were collected and frozen at −80°C until
immunoblotting. The protein concentration of each homogenate was
determined. Equal amounts of protein (50 μg) were loaded
onto 12% SDS-PAGE gels for electrophoresis, then transferred to a
PVDF membrane. After blocking in 5% non-fat dry milk in 0.1 M
Tris-buffered saline (TBS)-0.1% Tween-20 (TBST), the proteins were
detected with primary antibodies against Ras, ERK1/2, p-ERK1/2 and
β-actin (dilution, 1:1,000). The proteins were incubated overnight
with primary antibodies at 4°C, then with appropriate
HRP-conjugated secondary antibodies for 50 min. Blots were
developed using enhanced chemiluminescence and images were analyzed
using a Bio-Image Analysis System (Bio-Rad, Hercules, CA, USA).
Statistical analysis
All data were processed using SPSS 16.0.
Quantitative data were expressed as the mean ± standard deviation.
Differences among the three groups were compared using one-way
analysis of variance (ANOVA) and Student’s t-tests. P<0.05 was
considered to indicate a statistically significant difference.
Results
EA treatment at the Zusanli (ST36) and
Quchi (LI11) acupoints alleviates neurological deficits in cerebral
I/R-injured rats
The neuroprotective effect of EA was first evaluated
by measuring the neurological deficit scores. As shown in Table I, all MCAO rats exhibited clear
manifestations of neurological deficits compared with rats in the
SC group (P<0.05), indicating successful model construction.
Although no significant differences were observed between the IC
and EA groups in the clinical evaluation before electric
stimulation, EA at Zusanli and Quchi was observed to significantly
improve the neurological deficits (P<0.05).
 | Table INeurological deficit score |
Table I
Neurological deficit score
| Group (n=8) | 2 h after I/R | 24 h after I/R |
|---|
| SC | 0 | 0 |
| IC | 2.50±0.76 | 2.25±0.71 |
| EA | 2.37±0.74 | 1.50±0.53a |
EA treatment at the Quchi and Zusanli
acupoints decreases the infarct volume in cerebral I/R-injured
rats
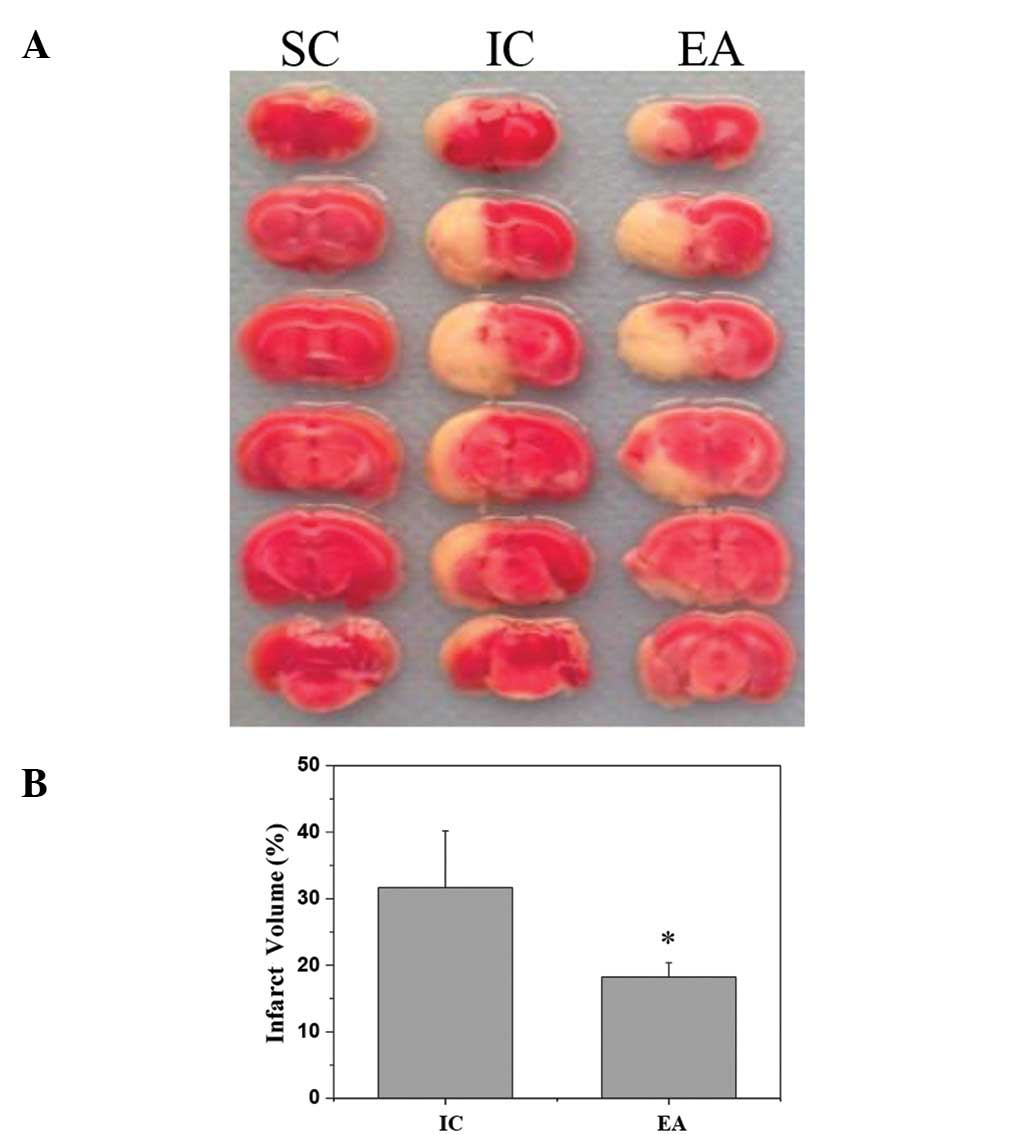
To further investigate the therapeutic efficacy of
EA against cerebral I/R injury, its effect on cerebral infarct
volume was evaluated using TTC staining. As shown in Fig. 1, EA at Quchi and Zusanli
significantly reduced the cerebral infarct volumes. The total
infarct volumes were 31.66±8.53 and 18.25±2.11% of the total brain
volume in the IC and EA groups, respectively (P<0.05).
EA at the Quchi and Zusanli acupoints
activates the ERK pathway in cerebral I/R-injured rats
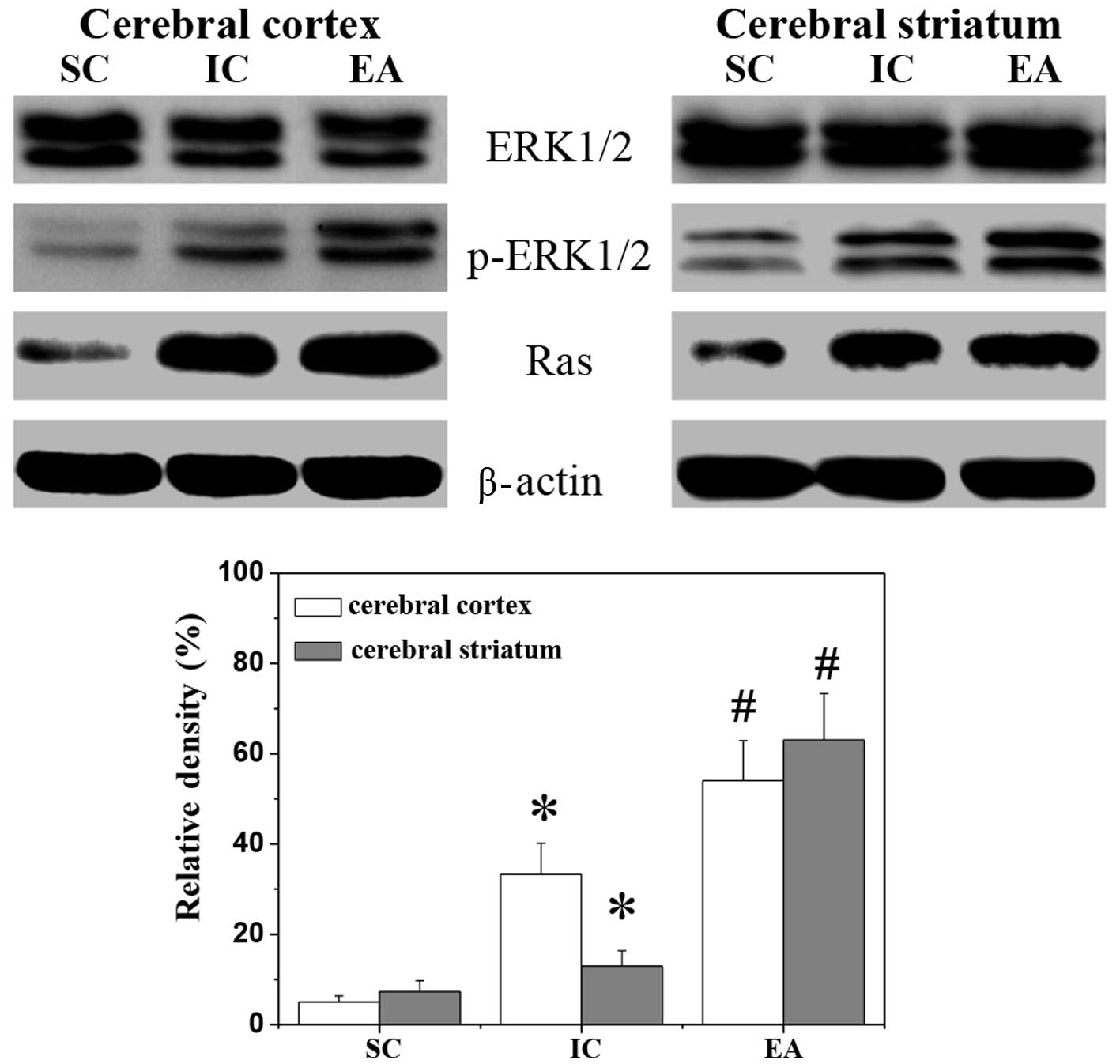
To investigate the effect of EA on the ERK pathway,
western blotting was performed to examine the expression of Ras and
the phosphorylation of ERK in the ischemic cerebral cortex and
striatum. As shown in Fig. 2, I/R
injury increased the Ras protein expression and the phosphorylation
level of ERK. This was consistent with previous studies of the
transient focal ischemia model which showed that ERK was activated
following I/R and persisted for 24 h (22,23).
EA at Zusanli and Quchi further upregulated the protein expression
of Ras, as well as ERK phosphorylation, whereas the levels of
nonphosphorylated ERK remained unchanged in all three animal
groups.
Electroacupuncture at the Quchi and
Zusanli acupoints promotes cell proliferation in cerebral
I/R-injured rats
ERK activation is important in cell proliferation
and therefore, the pro-proliferative activity of EA was
investigated using IHC staining for PCNA. As shown in Fig. 3, I/R injury increased the
percentage of PCNA-positive cells in the ischemic cerebral cortex
and striatum of the IC rats compared with the SC group. The
percentages of PCNA-positive cells in the ischemic cerebral cortex
and striatum of the SC rats were 2.00±0.27 and 5.17±1.61%,
respectively, while those in the IC group were 11.48±1.15 and
13.01±1.17% (P<0.05). However, EA at Zusanli and Quchi was
observed to significantly promote cell proliferation. The
PCNA-positive cell rates of the ischemic cerebral cortex and
striatum in the EA group were 19.11±0.77 and 19.77±0.42%,
respectively (P<0.05, vs. IC group).
Electroacupuncture at Quchi and Zusanli
increases the expression of cyclin D1 and CDK4 in cerebral
I/R-injured rats
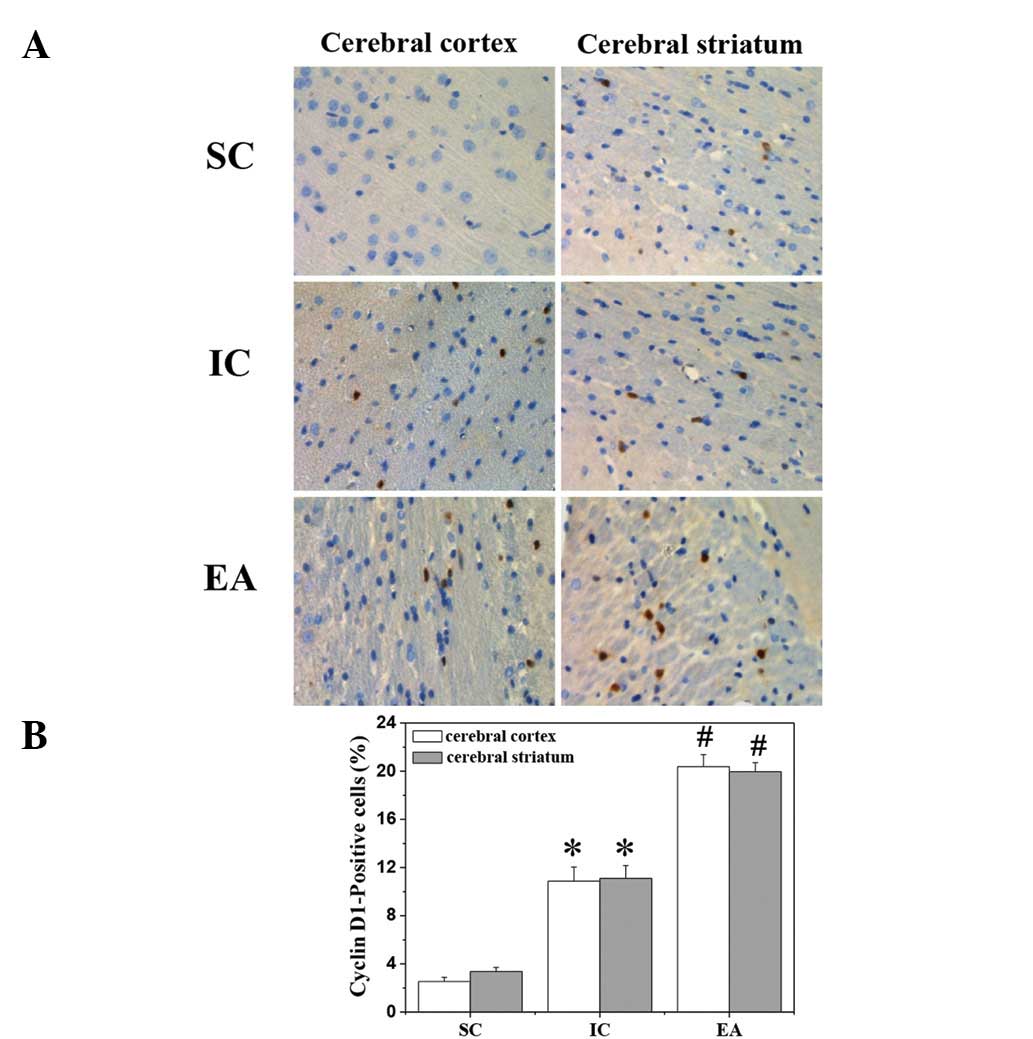
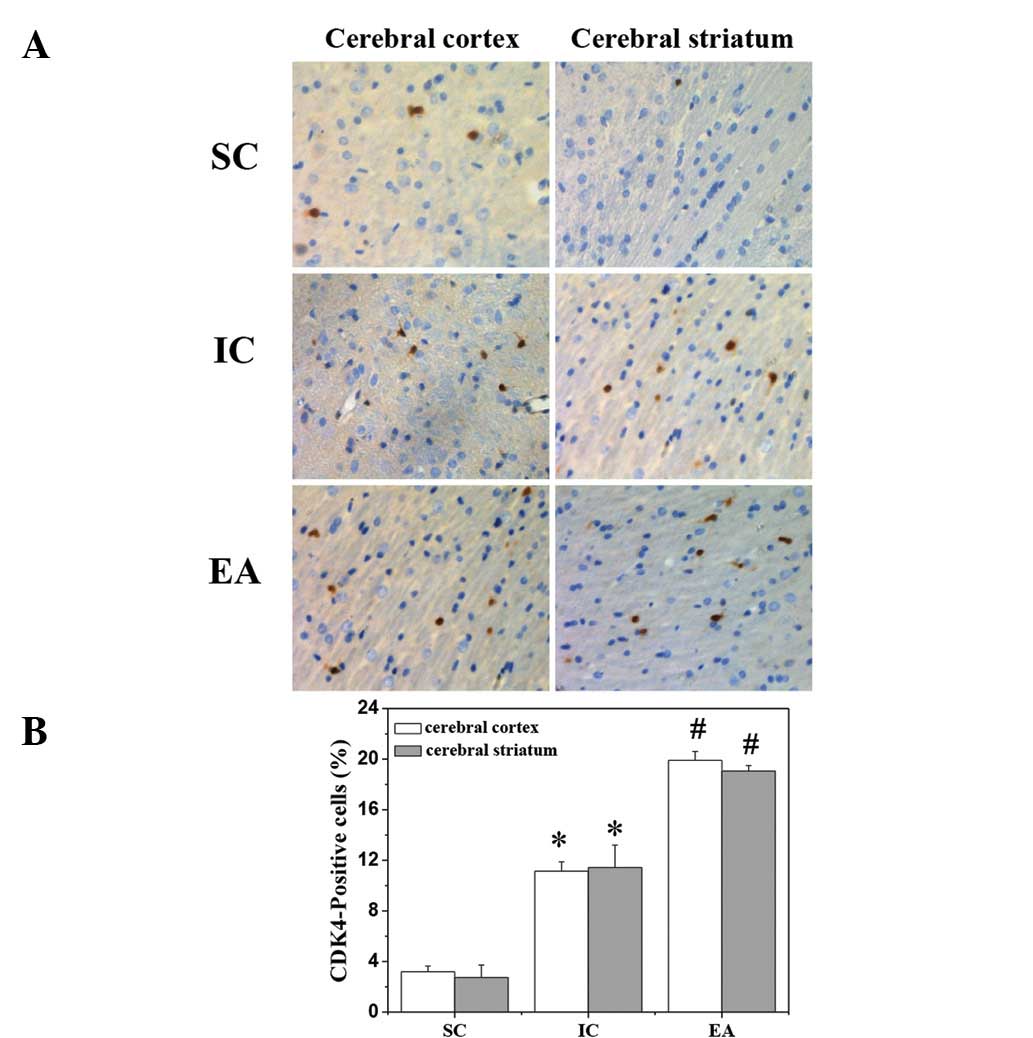
To further investigate the mechanism of the
pro-proliferative activity of EA, its effect on the protein
expression of cyclin D1 and CDK4 was evaluated using IHC staining
(Figs. 4 and 5). Consistent with the previous findings,
the protein expression levels of cyclin D1 and CDK4 in the ischemic
cerebral cortex and striatum were increased by I/R injury and
further upregulated by EA treatment.
Discussion
The ERK1/2 pathway is a critical mediator of cell
proliferation, which is activated in response to growth factors
(24,25), oxidative stress (26) and glutamate receptor stimulation
(19,27), and promotes progression from the G1
to the S-phase by regulating the cyclin D1-CDK4 complex (15,16,28).
Numerous studies have reported that the activation of the ERK1/2
pathway is markedly associated with protection from cerebral I/R
injury, decreasing the infarct size and promoting cerebral cell
proliferation (29–32). Therefore, promoting cerebral cell
proliferation via the activation of ERK signaling is a promising
strategy for the treatment of ischemic stroke. Acupuncture is an
alternative medicine methodology that has long been used in China
to treat various diseases. Previous studies have demonstrated the
clinical efficacy of acupuncture in stroke rehabilitation. On the
basis of data in the literature, the Zusanli (ST36) and Quchi
(LI11) acupoints have commonly been used in China to clinically
treat stroke. However, the mode of action of the neuroprotective
activities of EA remain poorly understood.
In the present study, a focal cerebral I/R rat model
was used to demonstrate that EA at Zusanli and Quchi for only 24 h
had a neuroprotective effect as evidenced by improved neurological
deficits and reduced cerebral infarct volume. In addition, it was
observed that the ERK1/2 pathway was activated 24 h after cerebral
I/R injury, which was consistent with the findings of previous
studies (22,23). However, EA significantly further
upregulated ERK1/2 in I/R-injured brain tissues. The pattern of
cyclin D1 and CDK4 protein expression was consistent with that of
ERK activation in the present study. Consequently, the regulatory
effect of EA on ERK activation resulted in the promotion of
cerebral cell proliferation.
In conclusion, to the best of our knowledge, the
present study reported for the first time that EA at the Quchi
(LI11) and Zusanli (ST36) acupoints exerts a neuroprotective effect
in ischemic stroke via the activation of the ERK1/2 pathway. These
results suggest that EA may be a potential therapeutic approach for
the treatment of cerebral ischemia.
Abbreviations:
|
ERK
|
extracellular signal-regulated
kinase;
|
|
I/R
|
ischemia/reperfusion;
|
|
MCAO
|
middle cerebral artery occlusion;
|
|
EA
|
electroacupuncture;
|
|
PCNA
|
proliferating cell nuclear
antigen;
|
|
TTC
|
2,3,5-triphenyltetrazolium
chloride;
|
|
CDK4
|
cyclin-dependent kinase 4;
|
|
MAPKs
|
mitogen-activated protein kinases
|
Acknowledgements
This study was sponsored by the
Special Program for Key Basic Research Project of the China
Ministry of Science and Technology (973 Program, No. 2010CB534900)
and National Natural Science Foundation of China (No.
81273835).
References
|
1.
|
Luitse MJ, Biessels GJ, Rutten GE and
Kappelle LJ: Diabetes, hyperglycaemia, and acute ischaemic stroke.
Lancet Neurol. 11:261–271. 2012. View Article : Google Scholar
|
|
2.
|
Szydlowska K and Tymianski M: Calcium,
ischemia and excitotoxicity. Cell Calcium. 47:122–129. 2010.
View Article : Google Scholar
|
|
3.
|
Wu JN: A short history of acupuncture. J
Altern Complement Med. 2:19–21. 1996. View Article : Google Scholar
|
|
4.
|
Kim SK and Bae H: Acupuncture and immune
modulation. Auton Neurosci. 157:38–41. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Zhang GC, Fu WB, Xu NG, et al: Meta
analysis of the curative effect of acupuncture on post-stroke
depression. J Tradit Chin Med. 32:6–11. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Hu HH, Chung C, Liu TJ, et al: A
randomized controlled trial on the treatment for acute partial
ischemic stroke with acupuncture. Neuroepidemiology. 12:106–113.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Jansen G, Lundeberg T, Kjartansson J and
Samuelson UE: Acupuncture and sensory neuropeptides increase
cutaneous blood flow in rats. Neurosci Lett. 97:305–309. 1989.
View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Johansson K, Lindgren I, Widner H, et al:
Can sensory stimulation improve the functional outcome in stroke
patients? Neurology. 43:2189–2192. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Magnusson M, Johansson K and Johansson BB:
Sensory stimulation promotes normalization of postural control
after stroke. Stroke. 25:1176–1180. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Pavlikova M, Kovalska M, Tatarkova Z, et
al: Response of secretory pathways Ca(2+) ATPase gene expression to
hyperhomocysteinemia and/or ischemic preconditioning in rat
cerebral cortex and hippocampus. Gen Physiol Biophys. 30:S61–S69.
2011.
|
|
11.
|
Urban P, Pavlíková M M, Sivonová M, et al:
Molecular analysis of endoplasmic reticulum stress response after
global forebrain ischemia/reperfusion in rats: effect of
neuroprotectant simvastatin. Cell Mol Neurobiol. 29:181–192. 2009.
View Article : Google Scholar
|
|
12.
|
Riedemann NC and Ward PA: Complement in
ischemia reperfusion injury. Am J Pathol. 162:363–367. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Lehotský J, Urban P, Pavlíková M, et al:
Molecular mechanisms leading to neuroprotection/ischemic tolerance:
effect of preconditioning on the stress reaction of endoplasmic
reticulum. Cell Mol Neurobiol. 29:917–925. 2009.PubMed/NCBI
|
|
14.
|
Seger R and Krebs EG: The MAPK signaling
cascade. FASEB J. 9:726–735. 1995.PubMed/NCBI
|
|
15.
|
Lavoie JN, Rivard N, L’Allemain G and
Pouysségur J: A temporal and biochemical link between growth
factor-activated MAP kinases, cyclin D1 induction and cell cycle
entry. Prog Cell Cycle Res. 2:49–58. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Whitmarsh AJ and Davis RJ: A central
control for cell growth. Nature. 403:255–256. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Gu Z, Jiang Q and Zhang G: Extracellular
signal-regulated kinase 1/2 activation in hippocampus after
cerebral ischemia may not interfere with postischemic cell death.
Brain Res. 901:79–84. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Hu BR and Wieloch T: Tyrosine
phosphorylation and activation of mitogen-activated protein kinase
in the rat brain following transient cerebral ischemia. J
Neurochem. 62:1357–1367. 1994.PubMed/NCBI
|
|
19.
|
Kurino M, Fukunaga K, Ushio Y and Miyamoto
E: Activation of mitogen-activated protein kinase in cultured rat
hippocampal neurons by stimulation of glutamate receptors. J
Neurochem. 65:1282–1289. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Longa EZ, Weinstein PR, Carlson S and
Cummins R: Reversible middle cerebral artery occlusion without
craniectomy in rats. Stroke. 20:84–91. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Bederson JB, Pitts LH, Germano SM, et al:
Evaluation of 2,3,5-triphenyltetrazolium chloride as a stain for
detection and quantification of experimental cerebral infarction in
rats. Stroke. 17:1304–1308. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Hu X, Wu X, Xu J, et al: Src kinase
up-regulates the ERK cascade through inactivation of protein
phosphatase 2A following cerebral ischemia. BMC Neurosci.
10:742009. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Sugino T, Nozaki K, Takagi Y, et al:
Activation of mitogen-activated protein kinases after transient
forebrain ischemia in gerbil hippocampus. J Neurosci. 20:4506–4514.
2000.PubMed/NCBI
|
|
24.
|
Boulton TG, Nye SH, Robbins DJ, et al:
ERKs: a family of protein-serine/threonine kinases that are
activated and tyrosine phosphorylated in response to insulin and
NGF. Cell. 65:663–675. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Nishida E and Gotoh Y: The MAP kinase
cascade is essential for diverse signal transduction pathways.
Trends Biochem Sci. 18:1281993. View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Aikawa R, Komuro I, Yamazaki T, et al:
Oxidative stress activates extracellular signal-regulated kinases
through Src and Ras in cultured cardiac myocytes of neonatal rats.
J Clin Invest. 100:1813–1821. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
Fiore RS, Murphy TH, Sanghera JS, et al:
Activation of p42 mitogen-activated protein kinase by glutamate
receptor stimulation in rat primary cortical cultures. J Neurochem.
61:1626–1633. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
Jirmanova L, Afanassieff M, Gobert-Gosse
S, et al: Differential contributions of ERK and PI3-kinase to the
regulation of cyclin D1 expression and to the control of the G1/S
transition in mouse embryonic stem cells. Oncogene. 21:5515–5528.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
29.
|
Tian HP, Huang BS, Zhao J, et al:
Non-receptor tyrosine kinase Src is required for
ischemia-stimulated neuronal cell proliferation via Raf/ERK/CREB
activation in the dentate gyrus. BMC Neurosci. 10:1392009.
View Article : Google Scholar : PubMed/NCBI
|
|
30.
|
Zhou L and Miller CA: Mitogen-activated
protein kinase signaling, oxygen sensors and hypoxic induction of
neurogenesis. Neurodegener Dis. 3:50–55. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
31.
|
Zhou L, Del Villar K, Dong Z and Miller
CA: Neurogenesis response to hypoxia-induced cell death: map kinase
signal transduction mechanisms. Brain Res. 1021:8–19. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
32.
|
Luo WS, Yu HB, Yang ZX, et al: Influence
of Ren and Du meridian electro-acupuncture on neural stem cell
proliferation and extracellular signal-regulated kinase pathway in
a rat model of focal cerebral ischemia injury. Neural Regen Res.
5:433–438. 2010.
|