Introduction
Cataract is the main cause of avoidable blindness
worldwide and accounts for approximately half of all cases of
blindness in China (1–4). It is necessary to evaluate
post-surgical outcomes not only on the basis of visual acuity, but
also on self-reported visual function (VF) and vision-related
quality of life (QOL). These assessments may elucidate the full
spectrum of disabilities associated with visual impairment from
cataracts and improve the treatment approach and rehabilitation of
patients.
Several previous studies evaluated the status of
cataract patients, based on the population studied in rural areas
of Northern and Southern China (5–7). The
cataract surgery in those studies included intracapsular cataract
extraction with aphakic glasses (ICCE-AG) and extracapsular
cataract extraction with posterior chamber intraocular lens
(ECCE/PC-IOL). Zhao et al observed that the mean QOL and VF
scores for the patients who underwent surgery were 61.9±30.0 and
71.0±31.8, respectively, which were similar to those in patients
who had not undergone surgery and had moderate bilateral blindness
(<6/60 to ≥3/60 in the better eye). The VF and QOL scores
closely correlate with the visual acuity of the two patient
populations (for the ICCE-AG group, r=0.64 and r=0.61,
respectively, and for the ECCE/PC-IOL group, r=0.68 and r=0.59,
respectively) (5). He et al
also revealed that mean VF and QOL scores for the cataract surgery
population were 41.6 and 54.5, respectively (6). These studies generally agree that
cataract surgeries do not consistently produce favourable VF and
QOL outcomes (7). The improvement
of outcome should be given greater emphasis (5) and certain remedial efforts are
required to improve the performance of local eye surgeons (6). Fletcher et al observed that
ICCE-AG and ECCE/PC-IOL were associated with substantial benefits
in improved daily VF and QOL. The patients who received ECCE/PC-IOL
reported greater benefits and fewer problems with vision than the
patients who received ICCE-AG (9).
Small incision cataract surgery (SICS) was recently
introduced into China and performed widely in a series of rural
blindness prevention activities conducted by Sight First China
Action, while phacoemulsification is used widely in other
developed areas and countries. Yao et al reported that
microincision cataract surgery generated significantly less corneal
astigmatism and improved the optical quality of the cornea by
modulation transfer function (MTF) evaluation, compared with SICS.
However, microincision cataract surgery showed no significant
advantage in reducing corneal high order aberrations compared with
SICS (10). Lam et al
indicated that the skill transfer in their setting had superior
outcomes, compared with the majority of studies in rural Asia and
to the patients in their cohort treated in other facilities
(11). Congdon et al
suggested that VF was superior in their cohort and that the
potential benefits of avoiding refraction and second-eye surgery
were substantial. However, the acceptance of such services was
modest (12). Taylor et al
concluded that cataract surgery in Pakistan had not led to VF and
QOL scores equivalent to those in unoperated individuals with the
same levels of visual acuity. The higher proportion of intraocular
lens (IOL) surgery in previous years was likely to improve QOL
following cataract surgery. Further focus was required on rural and
illiterate populations, to ensure that patients achieve comparable
VF and QOL outcomes following surgery (13). However, it is unclear how much the
cataract patients have benefited from the SICS with IOL
implantation in the rural area of China and whether changes in VF
and QOL outcomes occurred following the blindness prevention
activities of Sight First China Action, funded by the
International Lions Club. Therefore, the present study was
conducted. Similar protocols have been employed previously
(5–7). Chan et al reported that the
QOL and surgical outcomes in cataract patients may be assessed by a
simple questionnaire, but that the local culture and environment
should be taken into consideration in the questionnaire design
(14). Dam et al also
demonstrated that a Chinese-language version of the visual function
assessment (VFA) questionnaire was reliable and valid. In
industrialized countries with large Chinese-speaking populations
and newly developed countries of East and Southeast Asia, the VF
assessment may be helpful in assisting routine clinical patient
evaluation and cross-cultural outcome assessment programs. These
results also suggested that self-administered VF assessments may be
more reliable and valid than interview-generated assessments
(15). Therefore, we consider that
our results may be directly compared with the results from other
population-based studies in China.
Materials and methods
Study design and sampling
The study was conducted in Jiangyan county, a
district approximately 200 km northwest of Shanghai, in the
relatively developed Jiangsu province with a primarily rural
population of middle socioeconomic status. Jiangyan county is
considered a good representation of geographical character,
economic status, developing culture and health care conditions in
the rural areas of Eastern China (16). The ethics committee of the
Affiliated Hospital of Nantong University (Nantong, China) approved
the survey and consent forms were obtained from each patient
participating in this study.
The patients completed the survey prior to and 6
months after surgery. The patients were selected by two procedures.
First, the mobile eye disease screening camps and hospitals
selected the 38 villages as working sites in Jiangyan county,
according to the population size and location, ensuring that there
were no less than two working sites in every town of this county.
The mobile eye disease screening camps were organized by the local
government. The government informed the villagers of the purpose,
methods and arrangement of eye examination by a local broadcasting
network repeatedly, and asked the village head to be responsible
for the patient organization according to the program schedule.
In these camps, local ophthalmologists and specially
trained local health workers were responsible for the eye
examinations, which were conducted by a flashlight and included an
examination of the lids, conjunctiva, cornea, anterior chamber,
iris, pupil, lens and ocular movement, without examination of the
dilated fundus. A total of 2,431 patients received eye examination
and 251 patients with visual acuity of the naked eye less than 6/18
in at least one eye were suspected cataract patients. The
potentially eligible patients were transported to a hospital by a
special bus free of charge, where they were re-examined by the
members of the Sight First China Action cataract surgery
team. A dilated fundus examination was performed on each patient.
Finally, 178 patients whose corrected vision at best was <6/18
in at least one eye were identified as candidates for cataract
surgery and accepted the SICS and questionnaire of VF and QOL. The
patients completed the first survey and arrangements were made for
the patients to be treated at two hospitals within one week,
Jiangyan People’s Hospital and Jiangyan Chinese Medical Hospital
(Taizhou, China). The 178 patients were instructed by the surgery
doctors to travel to the surgical hospital six months later to
receive free eye examinations and fill out the survey again. Of
these, 131 patients accepted and 8 patients were deceased within
six months.
The interviews were administered in separate rooms
by trained interviewers. The patients were told that they could
refuse the interview and were asked to be honest in answering the
questions on the survey. Patients were informed that the personal
answers would be confidential and would not be reported
individually and that the answers would not affect the treatment or
the cost. A few patients with slight hearing impairments finished
the questionnaire with the assistance of a family member.
VF and QOL questionnaires
The VF and QOL questionnaires used in this survey
were adapted from a large-scale clinical trial of cataract surgery
at the Aravind Eye Hospital (Madurai, Tamil Nadu) in India
(8,9). The two questionnaires have been
successfully used in surveys of blindness and cataract outcomes in
Nepal (17) and in the Shunyi
(5), Doumen (6) and Shatin districts (7) of China. A translation of the original
English version into Chinese was modified to include some of the
local dialect.
The VF questionnaire consisted of 13 items in the
following subscales: general (a single question that assessed
overall VF), visual perception (four questions dealing with
activity limitation, near vision, intermediate vision and distance
vision), sensory adaptation (six questions dealing with light/dark
adaptation, visual search, color discrimination and glare
disability), peripheral vision (one question) and depth perception
(one question). The 12 questions in the QOL questionnaire addressed
limitations of daily living due to vision problems, and contained
the following subscales: self-care (including bathing, eating,
dressing and toileting), mobility (including walking to neighboring
houses, walking to shops and doing household chores), social (such
as attending social functions and meeting friends) and mental
(including feelings of being a burden on others, dejection and loss
of confidence).
Using a four-point scale, each question asked about
the extent to which the individual was currently experiencing a
difficulty, from ‘not at all’ to ‘a lot’. The subscale scores were
linearly transformed such that the response range was between 0 and
100. The composite scores for VF (VF total) and QOL (QOL total)
questionnaires were calculated by equal weighting of subscale
scores; weights were 1.0 for exact agreement and 0.66, 0.33 and 0
for disagreement of 1, 2 and 3 points, respectively (7).
The interviewers were trained in general
interviewing techniques and administration of the questionnaire.
Practice interviews were conducted on outpatients at Jiangyan
People’s Hospital and Jiangyan Chinese Medical Hospital. None of
the outpatients were study subjects. Intra-observer and
inter-observer agreement of VF and QOL questionnaire responses were
evaluated in twenty-six of the pilot studies in Jiangyan. Repeat
interviews were conducted 45 min after the initial interview. A
weighted kappa statistic was used to assess the degree of agreement
across the original four-point rating scale of each VF and QOL
item. The average kappas for intra-observer agreement (n=12) were
0.81 (range, 0.58–1.00) for VF items and 0.83 (range, 0.66–1.00)
for QOL items, respectively. The average kappas for inter-observer
agreement (n=14) were 0.71 (range, 0.53–0.86) for VF items and 0.82
(range, 0.57–1.0) for QOL items, respectively.
Data analysis
Visual acuity was recorded according to normal
living vision, i.e., to record the corrected visual acuity if the
patient usually wears glasses, or to record the uncorrected visual
acuity if the patient did not wear glasses, even if their visual
acuity could be corrected with glasses.
The bilateral vision was defined by the following
criteria: i) visual acuity in the better eye vs. worse eye: normal
or near normal, both eyes ≥6/18 or higher; ii) visual impairment,
≥6/60 vs. <6/18 to ≥6/60; iii) unilateral blindness, ≥6/60 vs.
<6/60; iv) moderate blindness, <6/60 to ≥3/60 vs. <6/60;
and v) severe blindness, both eyes <3/60 (17).
SPSS 12.0 (SPSS, Inc., Chicago, IL, USA) and Epidata
2.0 (The EpiData Association, Odense, Denmark) were used to analyze
the data. The correlation between vision status and VF and QOL
scores was assessed by the Spearman correlation coefficients. The
transformed VF and QOL scores passed a normality test. The paired
Student’s t-test was used to compare the preoperative and
postoperative VF and QOL scores. Multiple linear regression
analysis was used to analyze the VF and QOL scores using vision
status and demographic variables, and the multivariate model
included the age, gender, grade of vision, residence area,
disability, education, systemic disease history and previous
history of ophthalmopathy. P<0.05 was considered to indicate a
statistically significant result.
Results
Preoperative characteristics of
patients
A total of 178 patients completed the survey and
their average age was 69.9±9.9 years (ranging from 37 to 95 years).
The majority (92.03%) of the patients lived in the country, with
the remainder living in small towns. Of the patients, 60.2% were
female and had an average age of 69.54 years. The average age of
male patients was 70.36 years. There was no statistical difference
between the average age of the males and females (P=0.522). None of
the patients refused the questionnaire and none of those questioned
were suffering from Alzheimer’s disease. The VF and QOL scores of
178 preoperative cases are shown in Tables I and II. It was noted by multivariate analysis
of variance that the VF and QOL scores were significantly different
for the various vision grades (fVF=10.145, P=0.000;
fQOL=9.057, P=0.000), however, the score of visual
perception in the unilateral blindness group was higher than that
of the vision impairment group, and the QOL score in the unilateral
blindness group was similar to that of the vision impairment
group.
 | Table IPreoperative visual function (VF)
scores by category of visual acuity (mean ± SD). |
Table I
Preoperative visual function (VF)
scores by category of visual acuity (mean ± SD).
| Variable | Vision category
| Spearman correlation
coefficient |
|---|
| Vision
impairment | Unilateral
blindness | Moderate
blindness | Severe blindness | All |
|---|
| No. of cases | 33 (25.19%) | 9 (6.87%) | 77 (58.78%) | 12 (9.16%) | 131 | |
| General | 44.08±9.46 | 39.92±8.63 | 29.33±5.80 | 17.00±6.75 | 33.80±27.71 | −0.41 |
| Visual
perception | 51.17±25.30 | 61.99±26.42 | 38.69±29.65 | 17.78±18.74 | 48.26±30.95 | −0.57 |
| Peripheral
vision | 71.10±25.29 | 72.33±24.63 | 49.76±25.74 | 25.77±21.43 | 58.94±31.10 | −0.54 |
| Sensory
adaptation | 60.92±42.24 | 61.75±41.80 | 25.78±36.32 | 8.00±18.50 | 45.66±43.59 | −0.60 |
| Depth perception | 44.08±35.55 | 49.08±37.63 | 11.00±16.50 | 10.00±17.47 | 36.16±36.72 | −0.50 |
| Total VF | 60.03±23.87 | 64.05±24.94 | 39.96±23.99 | 20.06±16.86 | 50.95±29.62 | −0.60 |
 | Table IIPreoperative quality of life (QOL)
scores by category of visual acuity (mean ± SD). |
Table II
Preoperative quality of life (QOL)
scores by category of visual acuity (mean ± SD).
| Variable | Vision category
| Spearman correlation
coefficient |
|---|
| Vision
impairment | Unilateral
blindness | Moderate
blindness | Severe blindness | All |
|---|
| No. of cases | 33 (25.19%) | 9 (6.87%) | 77 (58.78%) | 12 (9.16%) | 131 | |
| Self-care | 92.31±20.04 | 86.09±20.42 | 68.22±29.25 | 44.94±31.34 | 75.07±30.09 | −0.55 |
| Mobility | 82.19±20.00 | 79.88±24.19 | 57.78±30.86 | 36.48±31.51 | 67.64±32.25 | −0.54 |
| Social | 72.13±35.10 | 80.42±27.19 | 72.06±29.00 | 57.42±30.08 | 73.29±30.08 | −0.36 |
| Mental | 74.81±27.78 | 60.03±25.66 | 52.70±28.17 | 39.45±26.64 | 55.70±28.04 | −0.35 |
| Total QOL | 82.04±16.41 | 77.08±19.01 | 62.37±23.93 | 43.54±22.93 | 68.07±24.90 | −0.55 |
It was revealed by multiple linear regression that
the VF and QOL scores were correlated with the vision grade
(rVF=−17.2093, t=−10.87, P=0.000,
rQOL=−13.1399, t=−8.87, P=0.000) and age
(rVF=−0.6505, t=−3.87, P=0.000, rQOL=−0.3309,
t=−2.10, P=0.037) of the patient, and the far visual acuity was
able to explain 37.2% of the VF results and 31.4% of the QOL
results. The gender, disability, education, systemic disease
history, residence area and previous history of ophthalmopathy had
no statistical significance (P>0.05). The correlation
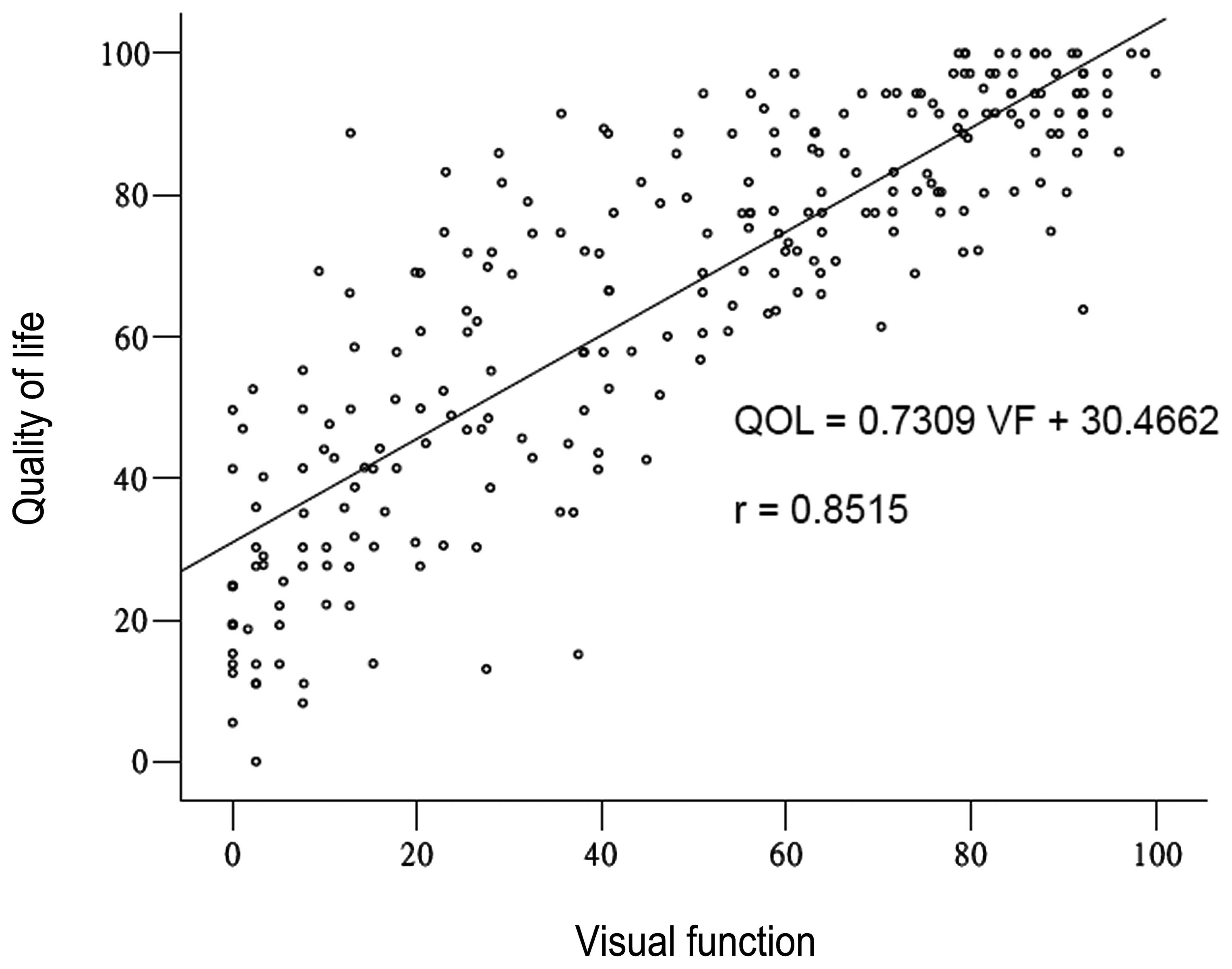
coefficient for patient VF and QOL scores was statistically
significant (t=25.62, P<0.001; Fig.
1).
Postoperative patient outcomes
Of the 178 eligible subjects, 131 were interviewed
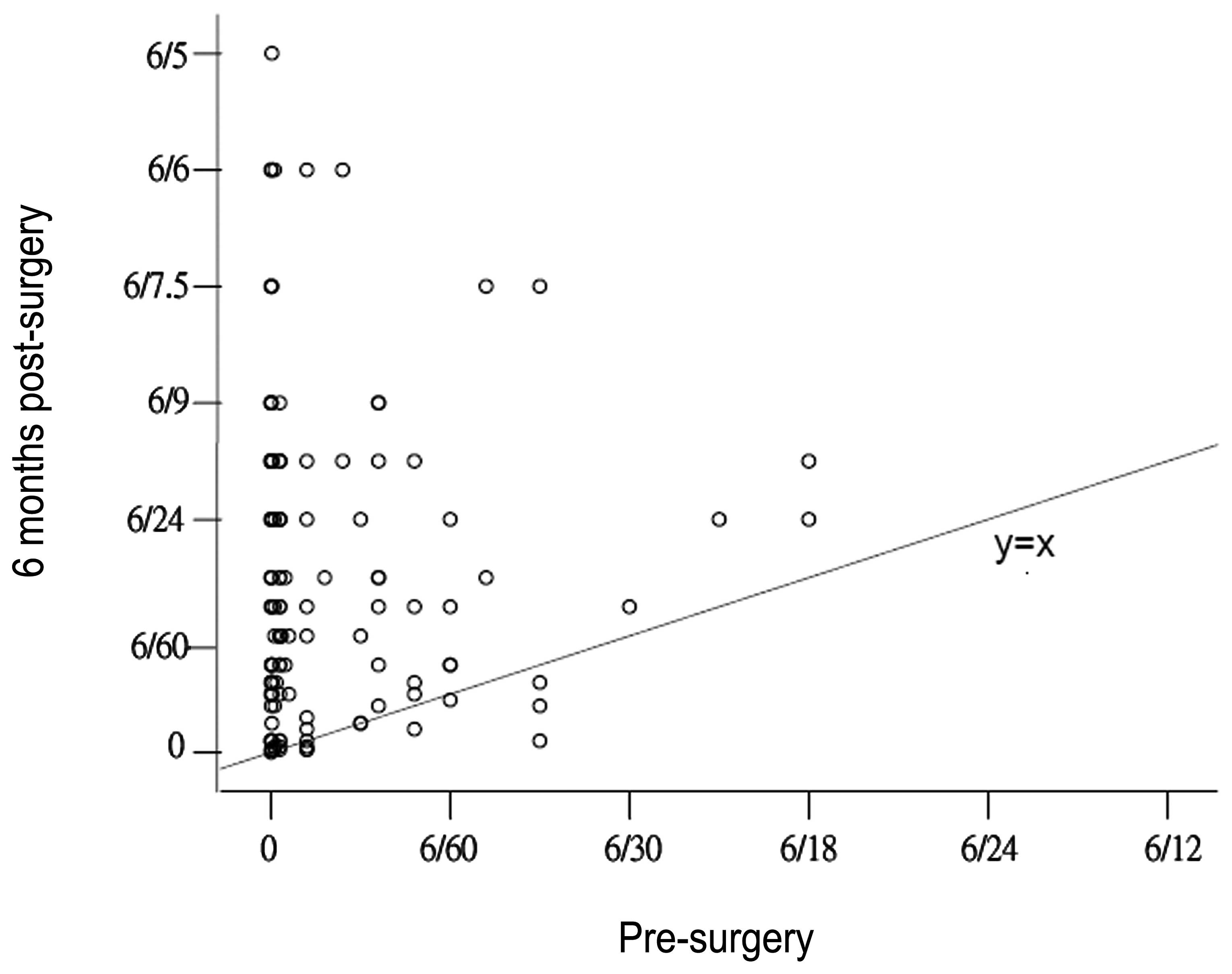
postoperatively, and 8 were deceased. The results of the visual
acuity of the operated eye preoperatively and postoperatively are
presented in Fig. 2. The 131
patients who responded to the postoperative survey had an average
age of 69.4±9.9 years (ranging from 39 to 96 years). A total of 84
patients were female. Excluding the 8 patients who died, 77.1% of
the patients completed the second survey. The preoperative data of
the 131 patients was compared with the total data for 178 patients.
The comparison showed that there were no significant differences in
age, gender, vision grade, systemic diseases history, other
disability, level of education, residence area and previous history
of the eye.
Tables III and
IV show the postoperative VF and
QOL scores of the 131 patients, respectively. It was demonstrated
by multiple linear regression that the VF scores were primarily
correlated with the grade of vision (r=−8.3542, t=−7.51,
P<0.001) and residence area (r=−3.5913, t=−2.01, P=0.047) of the
patient more so than other factors. We noted that the VF of
patients who lived in towns was higher than that of the patients
who lived in villages. The age, gender, disability, education,
systemic disease history and previous history of ophthalmopathy had
no statistical significance (P>0.05). The outcomes also
suggested that the QOL scores were mainly correlated with the grade
of vision (r=−9.9501, t=−10.27, P<0.001) and gender of the
patient (r=−6.7718, t=−2.59, P=0.011), since the QOL of female
patients appeared to be lower than that of the males. The age,
disability, education, systemic disease history, residence area and
previous history of ophthalmopathy had no statistical significance
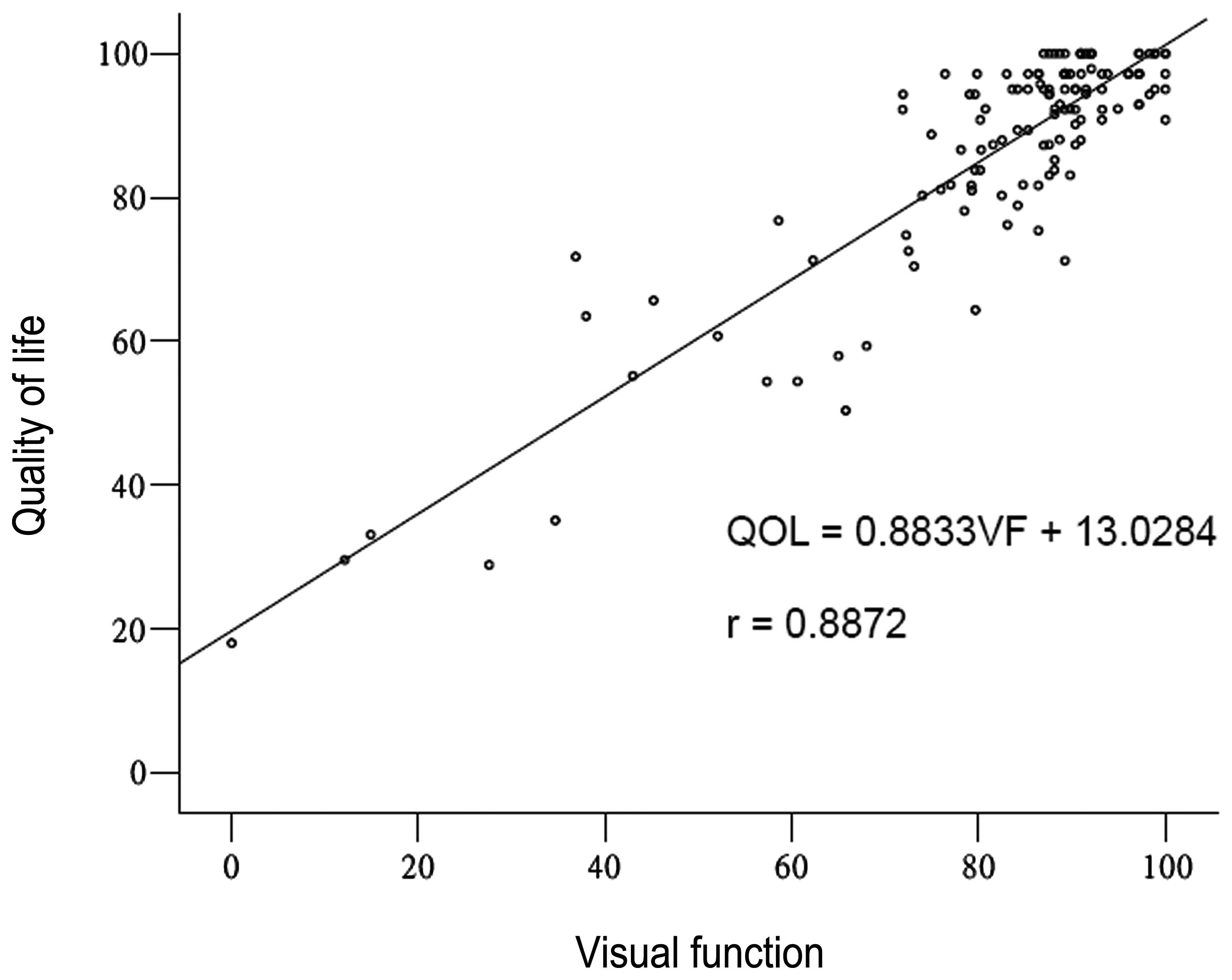
(P>0.05). The correlation coefficient of VF and QOL of the
patients was statistically significant (t=21.84, P<0.001;
Fig. 3).
 | Table IIIPostoperative visual function (VF)
scores by category of visual acuity (mean ± SD). |
Table III
Postoperative visual function (VF)
scores by category of visual acuity (mean ± SD).
| Variable | Vision Category
| Spearman
correlation coefficient |
|---|
| Normal | Vision
impairment | Unilateral
blindness | Moderate
blindness | Severe
blindness | All |
|---|
| No. of cases | 26 (19.8%) | 40 (30.5%) | 46 (35.1%) | 8 (6.1%) | 11 (8.4%) | 131 | |
| General | 79.12±19.32 | 64.50±21.33 | 63.26±20.90 | 45.63±39.59 | 39.00±28.84 | 63.67±25.05 | −0.37 |
| Visual
perception | 91.83±7.00 | 87.50±11.92 | 85.08±11.42 | 62.09±14.06 | 43.75±34.49 | 82.28±19.48 | −0.47 |
| Peripheral
vision | 98.69±6.67 | 94.08±15.08 | 65.57±11.58 | 62.13±27.93 | 45.18±37.26 | 89.46±22.82 | −0.44 |
| Sensory
adaptation | 91.29±7.37 | 85.90±10.62 | 88.59±9.07 | 70.50±9.80 | 60.36±30.04 | 84.83±14.98 | −0.32 |
| Depth
perception | 100.00±0.00 | 95.78±13.63 | 93.37±15.32 | 74.75±29.74 | 48.18±34.48 | 90.49±21.73 | −0.47 |
| Total VF | 91.76±5.75 | 86.13±10.18 | 86.47±8.82 | 65.68±12.12 | 51.50±30.55 | 83.21±16.40 | −0.48 |
 | Table IVPostoperative quality of life (QOL)
scores by category of visual acuity (mean ± SD). |
Table IV
Postoperative quality of life (QOL)
scores by category of visual acuity (mean ± SD).
| Variable | Vision category
| Spearman
correlation coefficient |
|---|
| Normal | Vision
impairment | Unilateral
blindness | Moderate
blindness | Severe
blindness | All |
|---|
| No. of cases | 26 (19.8%) | 40 (30.5%) | 46 (35.1%) | 8 (6.1%) | 11 (8.4%) | 131 | |
| Self-care | 98.37±4.18 | 94.26±9.11 | 88.19±11.50 | 73.50±13.07 | 52.70±29.80 | 88.18±17.41 | −0.65 |
| Mobility | 92.62±7.76 | 87.60±7.94 | 80.93±12.87 | 67.79±11.03 | 44.15±22.72 | 81.40±17.31 | −0.61 |
| Social | 99.35±3.33 | 96.61±8.73 | 90.08±14.87 | 66.44±21.88 | 55.82±29.14 | 89.59±18.88 | −0.58 |
| Mental | 98.26±4.17 | 91.86±15.21 | 87.53±16.43 | 71.88±18.01 | 56.27±31.21 | 87.40±19.63 | −0.48 |
| Total QOL | 97.06±3.87 | 92.39±8.33 | 86.53±11.06 | 70.49±11.49 | 51.98±23.91 | 86.53±16.33 | −0.68 |
The preoperative VF and QOL scores of 131 patients
were compared with those postoperatively (Table III and IV). There were statistically significant
differences between the pre- and postoperative VF and QOL scores of
the 131 patients (Table V).
Table VI illustrates the
comparison of VF and QOL scores preoperatively and postoperatively
in 131 patients divided by age. The Spearman’s correlation
coefficient between the VF change and age was 0.176 (P=0.044), and
the Spearman’s correlation coefficient between the QOL change and
age was 0.123 (P=0.162). The mean VF change significantly
correlated with the mean QOL change in the 131 patients (r=0.767,
P<0.001).
 | Table VPre- and postoperative comparison of
VF and QOL in 131 patients (Student’s t-test). |
Table V
Pre- and postoperative comparison of
VF and QOL in 131 patients (Student’s t-test).
| Variable | t | P-value |
|---|
| Total VF | −11.05 | <0.0001 |
| General | −9.15 | <0.0001 |
| Visual
perception | −10.65 | <0.0001 |
| Peripheral
vision | −9.33 | <0.0001 |
| Sensory
adaptation | −9.98 | <0.0001 |
| Depth
perception | −8.08 | <0.0001 |
| Total QOL | −7.30 | <0.0001 |
| Self-care | −4.32 | 0.0159 |
| Mobility | −4.30 | 0.0090 |
| Social | −5.25 | <0.0001 |
| Mental | −10.60 | <0.0001 |
 | Table VIPre- and postoperative comparison of
QOL and VF between 131 patients divided by patient age (Student’s
t-test). |
Table VI
Pre- and postoperative comparison of
QOL and VF between 131 patients divided by patient age (Student’s
t-test).
| Age (years) | Case (%) | VF | QOL |
|---|
|
|
|---|
| Pr | Po | t | P-value | Pr | Po | t | P-value |
|---|
| <50 | 6 (4.58) | 50.67±35.02 | 75.66±24.55 | 2.433 | 0.059 | 65.85±30.64 | 82.17±27.67 | 2.208 | 0.078 |
| 50–59 | 22 (16.79) | 53.59±30.58 | 81.71±12.66 | 5.062 | <0.0001 | 71.01±22.42 | 84.06±15.60 | 3.749 | <0.0001 |
| 60–69 | 43 (32.82) | 59.23±25.89 | 88.01±7.89 | 7.246 | <0.0001 | 74.86±21.23 | 91.46±8.58 | 5.691 | <0.00001 |
| 70–79 | 52 (39.69) | 40.15±27.37 | 77.41±23.65 | 9.179 | <0.0001 | 61.37±25.63 | 83.58±19.99 | 6.033 | <0.0001 |
| ≥80 | 8 (6.11) | 44.18±31.35 | 87.53±10.20 | 4.589 | 0.003 | 66.36±26.79 | 91.11±8.81 | 3.256 | 0.014 |
| Total | 131 (100) | 49.40±28.86 | 82.15±17.84 | 13.658 | <0.0001 | 67.92±24.38 | 86.64±16.38 | 9.681 | <0.0001 |
Discussion
In the current study the preoperative results
indicated that the mean scores of VF and QOL and their subscales
were directly correlated with vision status (8). It was noteworthy that the scores of
visual perception of the unilateral blindness group were higher
than those of the vision impairment group (t=2.018, P=0.045), which
may be explained by the better eye phenomena. This was different
from the findings of previous studies (5–7).
However, the mean QOL scores of the unilateral blindness group were
similar to those of the vision impairment group (t=0.243, P=0.809)
and there was a large difference between the moderate blindness
group and the severe blindness group (t=3.102, P=0.003). As
identified in the survey, the VF and QOL mean scores were
significantly influenced by factors other than visual status, such
as character traits and cultural background. This may partly
explain why the social and mental Spearman’s correlation
coefficients were low for the visual status. In the unilateral
blindness group, the self-care (t=0.302, P=0.763) and social
capabilities (t=0.005, P=0.996) were similar to those of the vision
impairment group. As observed in other studies (5–7), the
mean VF and QOL scores were not significantly correlated with age,
gender or education levels. In the current study, the mean VF and
QOL scores were also not correlated significantly with the previous
history of ophthalmopathy. A likely explanation is that the
selected patients all had surgical indications, regardless of
disease severity and age, and that certain patients with severe eye
diseases, such as corneal leucoma, were excluded in the
preoperative screening.
The scores of preoperative VF and QOL indicated that
the patients in the severe blindness group were in most need of
improvement. If the visual acuity of one eye improved to 6/60, the
VF and QOL scores would improve significantly (18). In our opinion, in a situation of
limited resources, patients with severe blindness should be
prioritized in order to make the procedure more cost-effective and
efficient. In order to prevent the marked decrease of the VF and
QOL of cataract patients, medical intervention should occur prior
to the onset of severe blindness. We also observed that cataract
patients suffered from psychological problems, as numerous patients
had inferiority complexes. Limited activity and psychological
inferiority resulted in a decrease in the QOL, which led to the
conclusion that attention should be provided for the mental health
problems of cataract patients.
We also observed that there were significant
differences in the VF and QOL scores prior to and following surgery
in the 131 patients. The VF and QOL outcomes improved significantly
following surgery (19),
particularly in the general subscale of VF and the mental subscale
of QOL. The VF scores of the vision impairment group were similar
to those of the unilateral blindness group and depth perception was
the highest subscale of VF. The QOL scores of the normal group were
almost equal to those of the vision impairment group. The greatest
difference in QOL mean scores was between the moderate blindness
group and the severe blindness group. The four subscales of the QOL
were close. The VF mean scores of the patients who lived in towns
were higher than those from patients who lived in villages, partly
due to the difference in living facilities. The QOL scores of
female patients were lower than those of male patients, perhaps
partly due to housework. In general, the responsibilities of women
in the household require better vision. Our results were similar to
those obtained for Hong Kong and the VF and QOL scores were better
than those observed in Shunyi and Doumen (5–7), in
which the outcomes were based on the whole population. Thus, our
results suggest that, performing SICS and IOL implantation
collectively in a short period was effective in a rural area of
China.
In our survey, 6.1% of the patients had moderate
blindness and 8.4% of the patients had severe blindness. Such
patients were not able to recover, mainly due to complications such
as pathological myopia, glaucoma, retinal degeneration, optic nerve
atrophy, vitreous opacity and posterior capsular opacities. In
addition, we also identified a patient with high myopia who was
inappropriately implanted with a normal IOL due to a lack of
examination equipment and unknown myopic history. A routine
follow-up affected the quality of the surgery. We observed that
certain patients with refractive error, trichiasis, chronic
conjunctivitis, uveitis, posterior capsular opacities and
age-related macular degeneration required additional postoperative
treatment. These factors impacted the VF and QOL outcomes of the
surgery (20).
The majority of the patients surveyed in this
project were those with a lower educational background, who were
not able to obtain cataract surgery independently and required
subsidies. Evaluating the outcomes of this surgery will
comprehensively appraise the outcomes of blindness prevention
projects. The survey of the 178 patients was considered as a
baseline. Due to the difficulties of follow-up, the subjects were
not selected randomly. Oliver et al observed that only 41.4%
cataract patients returned for a 12-month follow-up visit and
completed the VF and QOL questionnaires in South India, despite
transport and a meal on the day of the follow-up visit being
offered free of charge to all eligible patients (21). Minassian et al invited
patients to a study comparing the effect of different cataract
surgeries (SICS and phacoemulsification) in England. The patients
who completed the trial in 1 year accounted for the 67.4% of the
total patients invited to participate (22). In the present study, patients were
informed that we required the true results, good or bad, and
attempted to avoid the dissatisfied subjects failing to respond to
the study. However, only 131 patients that were contacted responded
to the second survey, potentially resulting in certain bias
(23). Additionally, establishing
mobile eye camps in the villages may persuade patients to accept
the postoperative survey.
Measuring QOL has advantages in assessing the costs
and benefits. However, the floor-and-ceiling effect should not be
ignored. It is possible that negative effects of cataract are
overestimated and the benefits of treatment are underestimated
(9). It is important to
comprehensively understand the correlation between vision status
and the VF and QOL questionnaires. The VF and QOL assessments
capture vision deficit and individual adaptation to vision deficit.
Vision deficits affect different people differently (5). The self report reflects the personal
level and the vision status reflects the eye level. We observed
there were high correlations between the two questionnaires, preand
postoperatively (Figs. 1 and
3, respectively). Gothwal et
al suggested that the QOL questionnaire was not a valid measure
of QOL. However, the VF questionnaire was a reliable and valid
measure of visual disability in patients with cataract, and
although targeting was suboptimal in a developed country, it may be
optimal in a developing country as was originally intended
(24). We suggest that the two
questionnaires are required due to their differences in numerous
aspects. The VF subscale emphasized the problems of vision function
directly. The QOL subscale was designed to focus specifically on
those activities that are important in daily living for which
vision impairment may have an adverse impact (8). Therefore, it is as predicted that the
VF score changed more dramatically than the QOL score.
In conclusion, the VF and QOL scores of cataract
patients increased significantly following surgery, suggesting that
performing SICS with posterior chamber IOL implantation
collectively in a short period is an effective method for improving
the QOL of cataract patients in rural areas, as observed in this
Blindness Prevention Surgery Program in Eastern China. However, the
patient follow-up is important and should be conducted carefully,
as the untreated complications of the surgery may affect the
stability of patient postoperative VF and QOL.
Acknowledgements
The authors wish to thank Yu Jianping,
Hong Liu, Xu Changshan and Mei Xiaofei of the Department of
Ophthalmology, The People’s Hospital of Jiangyan, and Liu Jinghua
and Zhou Shuping of the Department of Ophthalmology, The Chinese
Medicine Hospital of Jiangyan, Jiangsu, China, who were
instrumental in performing this study. This study was supported by
the Shanghai JiaoTong University School of Medicine Innovation Fund
(YZ1022).
References
|
1.
|
Zhao JL: The progress in the prevention of
blindness in China. Zhonghua Yan Ke Za Zhi. 41:697–701. 2005.(In
Chinese).
|
|
2.
|
Michon JJ, Lau J, Chan WS and Ellwein LB:
Prevalence of visual impairment, blindness, and cataract surgery in
the Hong Kong elderly. Br J Ophthalmol. 86:133–139. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Zhao J, Jia L, Sui R and Ellwein LB:
Prevalence of blindness and cataract surgery in Shunyi County,
China. Am J Ophthalmol. 126:506–514. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Li S, Xu J, He M, Wu K, Munoz SR and
Ellwein LB: A survey of blindness and cataract surgery in Doumen
County, China. Ophthalmology. 106:1602–1608. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Zhao J, Sui R, Jia L, Fletcher AE and
Ellwein LB: Visual acuity and quality of life outcomes in patients
with cataract in Shunyi County, China. Am J Ophthalmol.
126:515–523. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
He M, Xu J, Li S, Wu K, Munoz SR and
Ellwein LB: Visual acuity and quality of life in patients with
cataract in Doumen County, China. Ophthalmology. 106:1609–1615.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Lau J, Michon J J, Chan WS and Ellwein LB:
Visual acuity and quality of life outcomes in cataract surgery
patients in Hong Kong. Br J Ophthalmol. 86:12–17. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Fletcher AE, Ellwein LB, Selvaraj S,
Vijaykumar V, Rahmathullah R and Thulasiraj RD: Measurements of
vision function and quality of life in patients with cataracts in
southern India. Report of instrument development. Arch Ophthalmol.
115:767–774. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Fletcher AE, Vijaykumar V, Selvaraj S,
Thulasiraj RD and Ellwein LB: The Madurai intraocular lens study.
III: Visual functioning and quality of life outcomes. Am J
Ophthalmol. 125:26–35. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Yao K, Tang X and Ye P: Corneal
astigmatism, high order aberrations, and optical quality after
cataract surgery: microincision versus small incision. J Refract
Surg. 22(Suppl): S1079–S1082. 2006.
|
|
11.
|
Lam DS, Congdon NG, Rao SK, Fan H, Liu Y,
Zhang L, Lin X, Choi K, Zheng Z, Huang W, Zhou Z and Pang CP:
Visual outcomes and astigmatism after sutureless, manual cataract
extraction in rural China: study of cataract outcomes and up-take
of services (SCOUTS) in the caring is hip project, report 1. Arch
Ophthalmol. 125:1539–1544. 2007. View Article : Google Scholar
|
|
12.
|
Congdon NG, Rao SK, Zhao X, Wang W, Choi K
and Lam DS: Visual function and postoperative care after cataract
surgery in rural China: study of cataract outcomes and up-take of
services (SCOUTS) in the caring is hip project, report 2. Arch
Ophthalmol. 125:1546–1552. 2007. View Article : Google Scholar
|
|
13.
|
Taylor AE, Shah SP, Gilbert CE, Jadoon MZ,
Bourne RR, Dineen B, Johnson GJ and Khan MD; Pakistan National Eye
Survey Study Group: Visual function and quality of life among
visually impaired and cataract operated adults. The Pakistan
National Blindness and Visual Impairment Survey. Ophthalmic
Epidemiol. 15:242–249. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Chan CW, Wong JC, Chan KS, Wong WK, Tam KC
and Chau PS: Evaluation of quality of life in patients with
cataract in Hong Kong. J Cataract Refract Surg. 29:1753–1760. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Dam OM, Sibley LM, Law FC, Lui L, Le G and
Courtright P: Reliability and reproducibility of a Chinese-language
visual function assessment. Ophthalmic Epidemiol. 8:327–337.
2001.PubMed/NCBI
|
|
16.
|
Zhou JB, Guan HJ, Qu J, Yang XJ, Peng D
and Gu HY: A study on the awareness of cataract disease and
treatment options in patients who need surgery in a rural area of
Eastern China. Eur J Ophthalmol. 18:544–550. 2008.PubMed/NCBI
|
|
17.
|
Pokharel GP, Selvaraj S and Ellwein LB:
Visual function and quality of life outcomes among cataract
operated and unoperated blind populations in Nepal. Br J
Ophthalmol. 82:606–610. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Nirmalan PK, Tielsch JM, Katz J,
Thulasiraj RD, Krishnadas R, Ramakrishnan R and Robin AL:
Relationship between vision impairment and eye disease to
vision-specific quality of life and function in rural India: the
Aravind Comprehensive Eye Survey. Invest Ophthalmol Vis Sci.
46:2308–2312. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Oshika T, Sugita G, Hayashi K, Eguchi S,
Miyata K, Kozawa T and Oki K: Influence of cataract and intraocular
lens surgery on health-related quality of life. Nihon Ganka Gakkai
Zasshi. 109:753–760. 2005.(In Japanese).
|
|
20.
|
Lundqvist B and Mönestam E: Longitudinal
changes in subjective and objective visual function 5 years after
cataract surgery Prospective population-based study. J Cataract
Refract Surg. 32:1944–1950. 2006.
|
|
21.
|
Oliver JE, Thulasiraj RD, Rahmathullah R,
Baburajan, Katz J, Tielsch JM and Schein OD: Vision-specific
function and quality of life after cataract extraction in south
India. J Cataract Refract Surg. 24:222–229. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Minassian DC, Rosen P, Dart JK, Reidy A,
Desai P, Sidhu M, Kaushal S and Wingate N: Extracapsular cataract
extraction compared with small incision surgery by
phacoemulsification: a randomized trial. Br J Ophthalmol.
85:822–829. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Yan L and Feng XS: Mensuration of life
quality in the evaluation of the effectiveness of the cataract
surgery. Zhonghua Yan Ke Za Zhi. 41:858–860. 2005.(In Chinese).
|
|
24.
|
Gothwal VK, Wright TA, Lamoureux EL and
Pesudovs K: Rasch analysis of visual function and quality of life
questionnaires. Optom Vis Sci. 86:1160–1168. 2009. View Article : Google Scholar : PubMed/NCBI
|