Introduction
Bile duct obstruction, usually caused by tumors,
calculus, inflammation, trauma or external compression, is a common
surgically treated disease. The preoperative localization,
qualitative diagnosis and determination of the anatomical
relationship between pathological tissue and ambient tissue are
important when planning surgery. Therefore, an accurate assessment
of the causes and pathological severity of the bile duct
obstruction is useful for preoperative surgical planning, reducing
the surgical exploration time and for assessing the prognosis of
patients. It has been reported that the diagnosis rates of bile
duct obstruction by CT, magnetic resonance imaging (MRI) and
magnetic resonance cholangiopancreatography (MRCP) are 86.7%, 93.3%
and 100%, respectively (1). In the
past, the diagnosis rate of bile duct obstruction by common CT was
low. Recently, with improvements in scanning speed, and spatial and
isotropic resolution, multi-slice spiral CT (MSCT) has been used
more frequently in the bile duct system. Due to continuous
improvements in the post-processing techniques of MSCT, it is
possible to enhance image reconstruction to show the deformation,
pathological location, pathological shape and the surrounding
tissue lesions clearly using various methods, including rapid thin
slice CT scanning, multiple planar reconstruction (MPR) and curved
planar reformation. The structure of the common bile duct and
ambient tissues is shown more clearly, which further improves the
diagnosic accuracy of CT in bile duct obstruction (2–9). In
the present study, 34 patients with clinically confirmed biliary
obstructive diseases were retrospectively analyzed by
reconstructing images of the portal vein from 64-slice spiral CT
data. The application value of bile duct reconstruction technology
with spiral CT in the diagnosis of obstructive disease is also
discussed.
Materials and methods
General information
We retrospectively analyzed the spiral CT images of
34 patients with biliary obstructive diseases between May 2009 and
February 2010. Twenty cases were male, while 14 patients were
female. Aged between 46 and 92 years, the patients had an average
age of 67.4 years. Common clinical manifestations included
jaundice, abdominal pain, nausea, vomiting, fever and pruritus. The
patients in this group were diagnosed by surgical pathology
diagnosis or endoscopic retrograde cholangiopancreatography (ERCP).
This study was approved by the Ethics Committee of the People’s
Liberation Army 101 Hospital (Wuxi, China). Signed informed consent
was obtained from each patient prior to examination.
Equipment and inspection methods
A GE 64-slice spiral CT instrument (GE Medical
Systems, Waukesha, WI, USA) was used to scan from the liver top to
the L3 level for both plain and multi-phase scanning. A trigger
scan was used for the hepatic arterial phase and the trigger point
was set at the abdominal aorta. The trigger threshold was set at
120 Hu. The portal venous phase was ∼70 sec and the lag phase was
180 sec. The scan parameters were set as follows: voltage, 120 kV;
current, 400 mA; screw pitch, 0.984:1; rotation period of bulb
tube, 0.6 sec; and layer thickness, 5 mm. Contrast medium (70–90
ml, Ultravist, 300 mg/ml; Schering Pharmaceutical Co.Ltd.,
Guangzhou, China) was injected at the speed of 3.5 ml/sec and 1000
ml water was consumed 10–15 min prior to inspection. All original
data of the portal venous phase (70 sec) were used for thin-layer
reconstruction in the standard mode. The reconstruction thickness
was 0.625 mm. The images were sent to a workstation (Advantage
workstation, AW4.4; GE Medical Systems) for observation and
post-processing analysis. According to the pathological condition,
we selected from the following reconstruction methods: MPR,
thin-slab minimum intensity projection (TS-MinIP), curved planar
reconstruction (CPR) and maximum intensity projection (MIP).
Results
Comparison of CT diagnosis and clinical
results
A total of 34 patients with biliary obstructive
diseases were confirmed by surgical pathological diagnosis or ERCP.
The CT diagnosis prior to surgery of 30 of the patients was in
accordance with the last clinical result (Table I): 2 cases of hilar
cholangiocarcinoma, 6 cases of gallbladder carcinoma invading the
common hepatic duct, 8 cases of periampullary adenocarcinoma and
carcinoma of the head of the pancreas, 2 cases of common bile duct
cancer, 1 case of duodenal papillary adenoma, 2 cases of duodenal
papilla diverticula with stenosis of the lower common bile duct and
8 cases of intrahepatic and extrahepatic bile duct calculus. In one
case, the pancreaticoduodenal vein surrounded the common bile duct
in the shape of semi-circle and compressed it, leading to a slight
narrowing of the common bile duct. The CT diagnosis prior to
surgery of 4 patients did not agree with the surgical results: CT
reconstruction prior to surgery of one patient suggested that
ampulla space-occupying caused secondary expansion of the
pancreatic and bile ducts, while surgical results showed that it
was pancreatitis (Table II). The
CT reconstructed image prior to surgery of another case suggested a
slight expansion of the pancreatic and bile ducts, but it was later
confirmed to be ampullary carcinoma by surgery. CT inspection prior
to surgery of 2 cases suggested a slight expansion of the
intrahepatic and extrahepatic bile duct, but was verified to be
common bile duct negative calculus.
 | Table I.Diagnostic accordance of the
patients. |
Table I.
Diagnostic accordance of the
patients.
| Category | Diagnostic
accordance |
|---|
| Total number | 30 |
| Hilar
cholangiocarcinoma | 2 |
| Gallbladder carcinoma
invading common hepatic duct | 6 |
| Periampullary
adenocarcinoma and carcinoma of head of pancreas | 8 |
| Common bile duct
cancer | 2 |
| Duodenal nipple
department adenoma | 1 |
| Intrahepatic and
extrahepatic bile duct calculus | 8 |
| Duodenal papillary
diverticula with stenosis of lower common bile duct | 2 |
| Pancreaticoduodenal
varicosity compressing common bile duct | 1 |
 | Table II.Diagnostic discordance of the
patients. |
Table II.
Diagnostic discordance of the
patients.
| Category | Diagnostic
discord |
|---|
| Total number | 4 |
| Pancreatitis | 1 |
| Periampullary
adenocarcinoma | 1 |
| Radioparent calculus
of common bile duct negative stone | 2 |
The 64-slice spiral CT bile duct reconstructed
images of the 34 patients in this group had an coincidence rate of
88.2% (30/34) for judgment of the obstruction cause and a relevance
rate of 100% for judgment of the obstruction location.
Discussion
The 64-slice spiral CT imaging technique, with its
high scanning speed, spatial resolution, isotropic resolution and
image clarity, showed anatomical relationships clearly. The
relationship between the bile duct and the ambient soft tissue
structure was displayed well by bile duct reconstruction in the
portal vein phase. Due to the significant enhancement of the portal
vein near the bile duct and liver parenchyma in the portal vein
phase compared with the arterial phase, the contrast between
relatively low-density bile in the intrahepatic and extrahepatic
bile duct and enhanced ambient soft tissue was clear. The
reconstructed images of the bile duct in the portal vein phase were
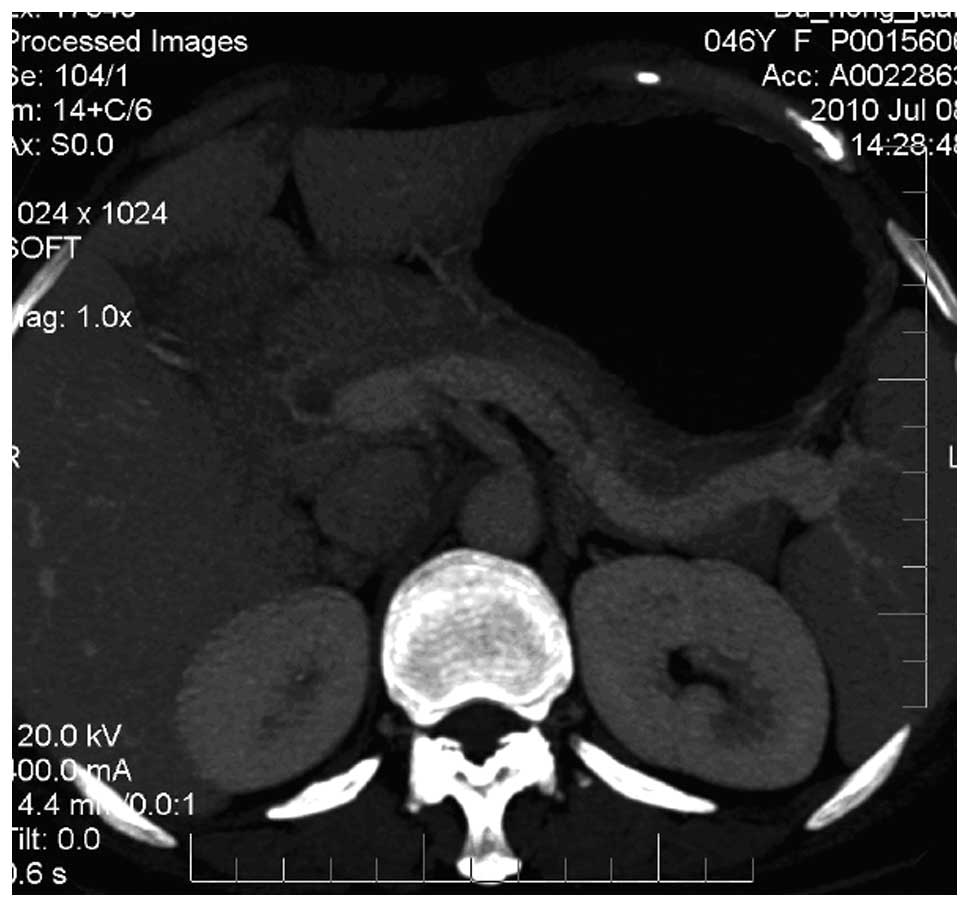
markedly superior to those in the arterial phase (Figs. 1 and 2) (10).
Based on the pathological properties, different imaging methods,
including MPR, CPR, Ts-MinIP and MIP, were used in the
reconstruction. Optimum reconstruction images were chosen and
turned to any angle that showed the anatomical configuration and
heteromorphosis of the bile and pancreatic ducts clearly and
vividly. Contiguous pathological and adjacent tissues were observed
for location diagnosis and qualitative diagnosis. Through
three-phase enhancement scanning, we were able to confirm the
enhanced features of pathological changes, including benignity or
malignancy, violation degree, lymph node metastasis, intrahepatic
metastasis, vascular embedding and ascites, which may indicate the
feasibility of tumor staging and surgical resection (11–22).
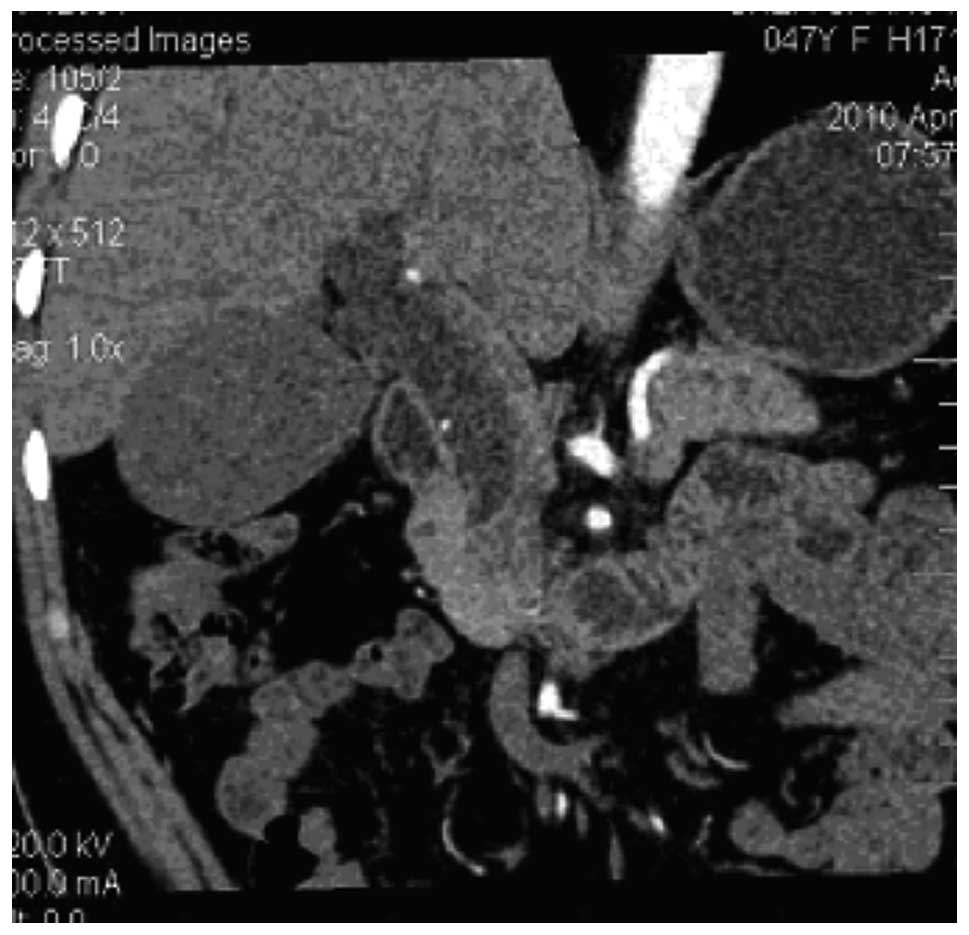
Through portal vein phase MPR of porta hepatis cholangiocellular
carcinoma, we were able to observe that the enhanced portal vein
served as a foil to the irregular shape of the porta hepatis soft
tissue which blocked the common hepatic duct, invaded left and
right hepatic bile ducts and caused the intrahepatic bile ducts of
the right and left lobes of the liver to expand (Fig. 3). MPR revealed the bile system with
high spatial and isotropic resolution, high imaging speed and no
manual cutting. When the bile system is observed, the ambient
structure is also observed and any angle is available for
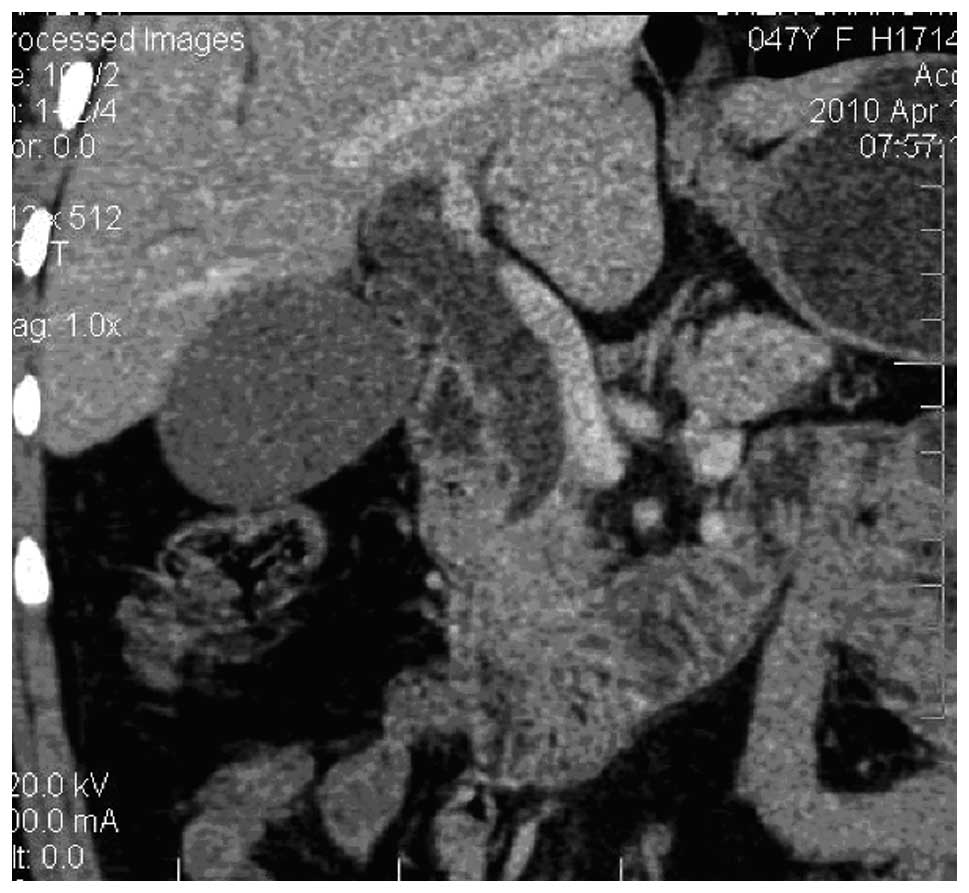
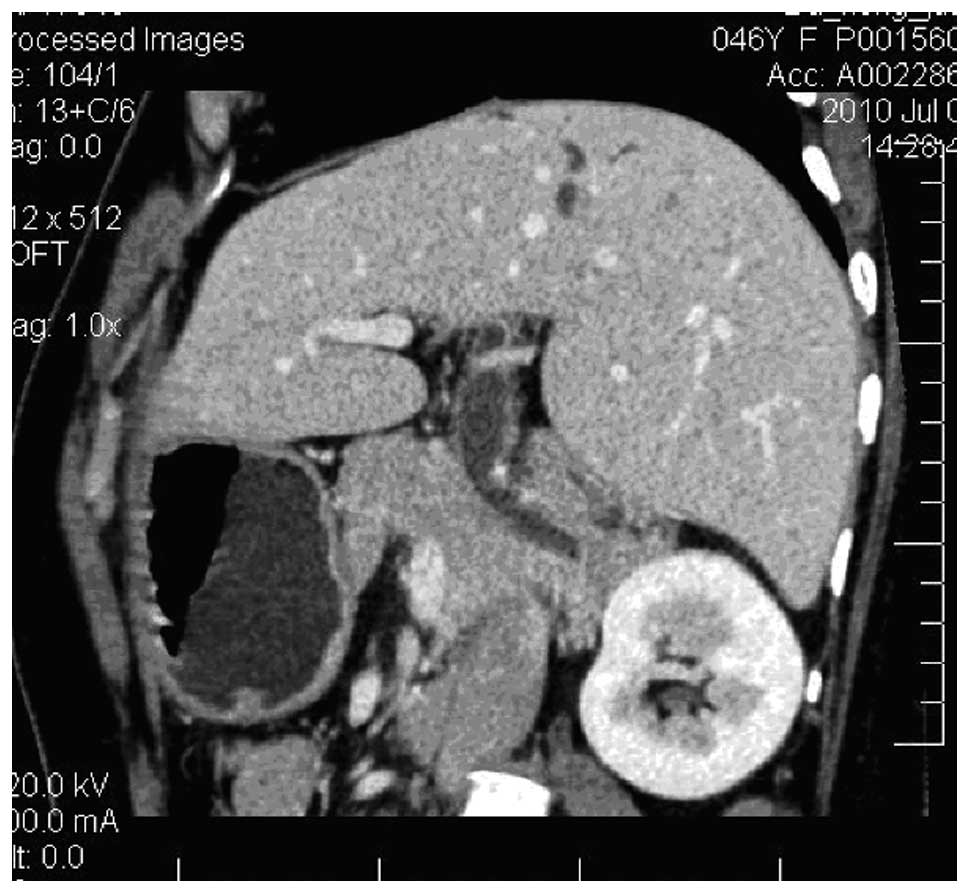
assessment. Portal vein phase MPR of gallbladder carcinoma with
secondary common hepatic duct metastasis showed significant
thickening of the common bile duct wall with homogeneous moderate
enhancement, which caused the bile duct lumen to become narrow
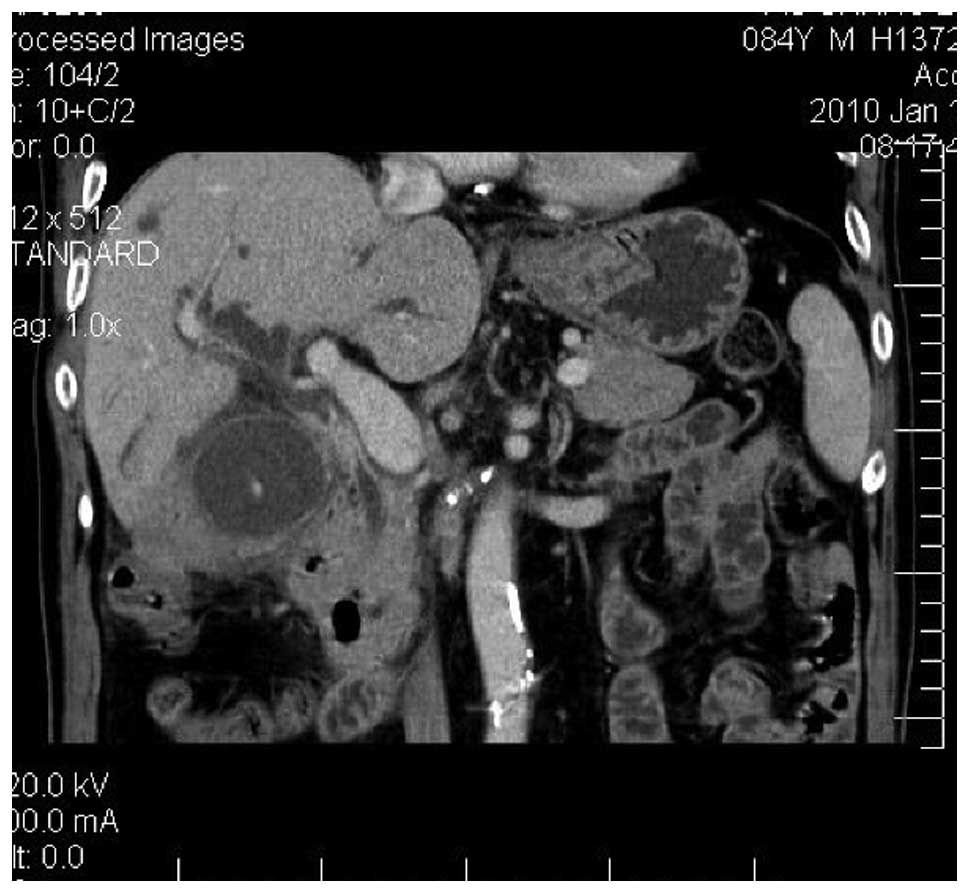
(Fig. 4). TS-MinIP was superior to
traditional cross section images in displaying bile duct expansion
and measuring the diameter. As an auxiliary diagnosis, TS-MinIP
further confirmed sign of conventional axial images, provided more
diagnosic information and improved the confidence of radiologists.
Although TS-MinIP does not provide more information than
cross-sectional images, it may provide the clinician with a
valuable three-dimensional anatomical image of the bile duct.
Similar to MRCP, TS-MinIP may determine the location of the
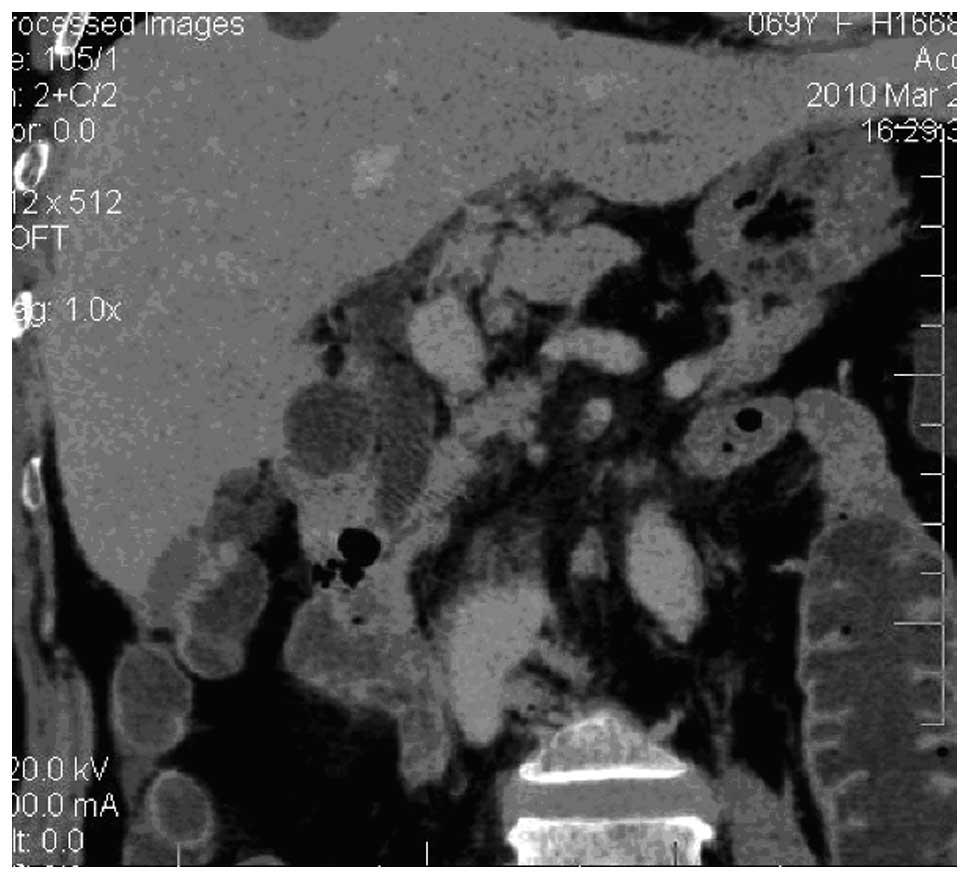
obstruction accurately (Fig. 5).
TS-MinIP not only showed a high-density calculus and expansive
intrahepatic and extrahepatic bile duct, but also displayed a soft
tissue density negative calculus in the common bile duct (5). Various routes and rotation angles of
CPR may be chosen to display all or the majority of the right and
left bile ducts, ductus cysticus, common hepatic duct and
common bile duct in the same plane. Multiple reconstruction may be
performed to comprehensively show the whole morphological structure
of the bile duct and clearly show the obstruction location,
expansion around the obstruction, the extent of the obstruction and
the relationship with ambient tissues. An advantage of the
application of CPR is that while traditional CT axial images are
not able to show the bile duct continuously, CPR is able to show
stenosis of the bile duct more directly and measure the extent of
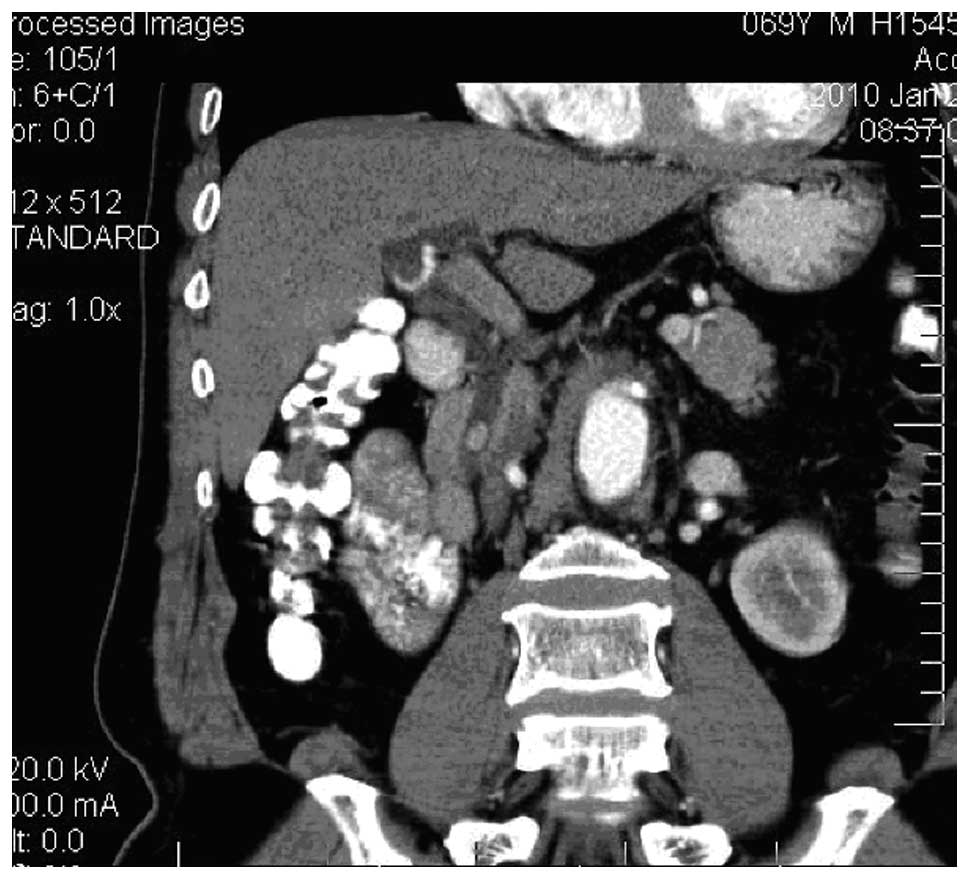
the stenosis (7). As its major
advantage, MIP may be used to assess whether the portal vein is
invaded by a tumor and the relationship between blood vessels and
bile ducts (Fig. 6). In one case,
portal vein phase MIP showed that the portal vein was normal and
was slightly pressed by a common bile duct carcinoma without
invasion. MIP and MPR, performed respectively in the portal vein
phase, directly showed that the pancreaticoduodenal vein partially
surrounded and adjoined the common bile duct, which led to a slight
narrowing of the common bile duct and a secondary expansion of the
common bile duct and part of the intrahepatic bile duct (Figs. 7 and 8).
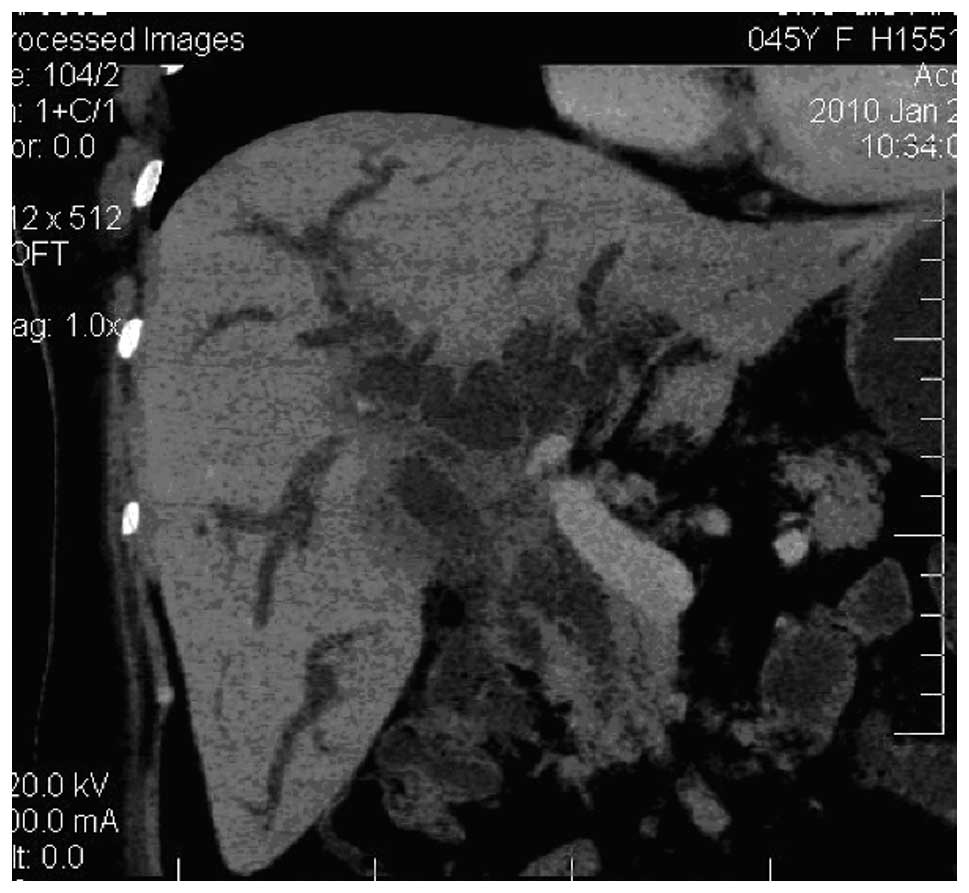
64-slice spiral CT, with a higher-density
resolution, is able to show any density, including that of gas,
fat, liquid and calculus, which contributes to a qualitative
diagnosis of the obstruction position (Fig. 9). MPR almost completely displays
the anatomical relationship between the common bile duct and its
ambient tissues and clearly shows the anatomical position of
positive calculi in the common bile duct. Bile duct calculi are
often accompanied by bile duct inflammation. By enhancing the
scanning of the portal vein phase, the enhancement effect of the
bile duct wall was shown to be significant. Therefore the calculus
with isodensity in the intrahepatic bile duct is able to be
identified. For the calculus with isodensity in the intrahepatic
bile duct, the CT diagnosis rate was improved due to the sharp
contrast to liver parenchyma enhancement after strengthened
scanning and the characteristic presence of limited expansion of
the intrahepatic bile duct. Bile duct inflammatory stenosis often
migrates gradually. The tube wall thickens equally and its edge is
relatively smooth, without soft tissue lumps. The portal vein phase
is superior to other phases in distinguishing soft tissue lump
shadows (Fig. 10). For
extrahepatic bile duct cancer or gallbladder carcinoma invading the
extrahepatic bile duct, 64-slice spiral CT manifested irregular
thickening of the bile duct wall, lumen stenosis obstruction and a
soft tissue lump. The thickened tube wall and soft tissue lump
presented regular or irregular enhancement. The enhancement extent
was more marked in the vein phase than in the arterial phase. The
bile duct above the obstruction expanded remarkably. For ampullary
cancer, CT showed a lump shadow in the ampullary area and
pancreatic head soft tissue. The bile duct was shown to be ‘cut
off’ and the bile duct above the obstruction and the pancreatic
duct expanded. Based on the tissue source, the enhancement methods
of the ampullary cancer focus were varied. For one patient with
duodenal papillary adenoma (Fig.
11) in this group, focus enhancement in the arterial phase was
clearer than that in the portal vein phase. The efficiency of
64-slice spiral CT reconstruction was not evident for bile duct
expansion. When the contrast medium was intravenously injected,
reconstruction of MPR, Ts-MinIP, CPR and MIP in the portal vein
phase was relatively improved for bile duct three-dimensional
images compared with that in other phases, due to the significant
enhancement of the portal vein near the bile duct and liver
parenchyma and the density contrast between low-density bile in the
bile duct and the enhanced bile wall.
Notably the efficiency of 64-slice spiral CT
reconstruction was not evident for bile duct expansion. The
thickness of the fixed bed will result in much interference. If the
fixed bed is thick, it will shade the focus of infection on the
side of obstruction and extrahepatic bile duct. If it is thin, the
location of pathological changes is not shown fully, particularly
in Ts-MinP and MIP images. Image noise levels were high due to the
thinness of the layer. The qualitative challenge of missed
diagnosis and misdiagnosis of small ampullary foci in this group
remains to be solved, which limited the correct diagnosis. The
objective reason for this is that the anatomical structure of the
ampulla is so complex that relatively small foci are difficult to
recognize. The subjective reason is our insufficient experience.
The normal slightly inward-protruding anatomical structure of the
duodenal papilla of 1 patient in this group was mistaken as a small
tumor when we observed images of the coronal view and inclined
coronal view. Therefore, ampullary disease imaging should be
further explored to improve comprehensive analysis, reduce
misdiagnosis rate and improve the precision of early stage
diagnosis. The density of negative calculi is similar to that of
bile, so CT imaging rarely shows a density contrast between them,
which leads to misdiagnosis. Therefore, the negative calculus
diagnosis rate of CT is lower than that of MRCP and ERCP.
In conclusion, 64-slice spiral CT reconstruction
images in the bile duct portal vein phase are able to clearly show
the bile duct structure with obstruction expansion, situation of
bile duct wall, ambient anatomical structure and the location of
the obstruction. 64-slice spiral CT is capable of affirming the
causes of the majority of bile duct obstructions. Therefore,
64-slice spiral CT is worthy of application and promotion in the
diagnosis of bile duct obstructive diseases.
References
|
1.
|
Chen Y: The Value of CT, MRI, MRCP in
diagnosing biliary obstruction. Journal of Practical Radiology.
20:802–804. 2004.
|
|
2.
|
Tamm E, Charnsangavej C and Szklaruk J:
Advanced 3-D imaging for the evaluation of pancreatic cancer with
multidetector CT. Int J Gastrointest Cancer. 30:65–71. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Nino-Murcia M, Jeffrey RB Jr, Beaulieu CF,
Li KC and Rubin GD: Multidetector CT of the pancreas and bile duct
system: value of curved planar reformations. AJR Am J Roentgenol.
176:689–693. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Becker CD: Multidetector CT and MRI of
biliary diseases. J Radiol. 84:473–479. 2003.(In French).
|
|
5.
|
Reimann AJ, Yeh BM, Breiman RS, Joe BN,
Qayyum A and Coakley FV: Atypical cases of gallstone ileus
evaluated with multidetector computed tomography. J Comput Assist
Tomogr. 28:523–527. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Schima W, Kulinna C, Ba-Ssalamah A and
Grünberger T: Multidetector computed tomography of the liver.
Radiologe. 45:15–23. 2005.(In German).
|
|
7.
|
Lee JY: Multidetector-row CT of malignant
biliary obstruction. Korean J Gastroenterol. 48:247–255. 2006.(In
Korean).
|
|
8.
|
Fulcher AS: MRCP and ERCP in the diagnosis
of common bile duct stones. Gastrointest Endosc. 56:S178–S182.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Sata N, Endo K, Shimura K, Koizumi M and
Nagai H: A new 3-D diagnosis strategy for duodenal malignant
lesions using multidetector row CT, CT virtual duodenoscopy,
duodenography, and 3-D multicholangiography. Abdom Imaging.
32:66–72. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Anderson SW, Rho E and Soto JA: Detection
of biliary duct narrowing and choledocholithiasis: accuracy of
portal venous phase multidetector CT. Radiology. 247:418–427. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Karcaaltincaba M, Haliloglu M, Akpinar E,
Akata D, Ozmen M, Ariyurek M and Akhan O: Multidetector CT and MRI
findings in periportal space pathologies. Eur J Radiol. 61:3–10.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Breiman RS, Coakley FV, Webb EM, Ellingson
JJ, Roberts JP, Kohr J, Lutz J, Knoess N and Yeh BM: CT
cholangiography in potential liver donors: effect of premedication
with intravenous morphine on biliary caliber and visualization.
Radiology. 247:733–737. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Anderson SW, Rho E and Soto JA: Detection
of biliary duct narrowing and choledocholithiasis: accuracy of
portal venous phase multidetector CT. Radiology. 247:418–427. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Tsukada K, Takada T, Miyazaki M, Miyakawa
S, Nagino M, Kondo S, Furuse J, Saito H, Tsuyuguchi T, Kimura F,
Yoshitomi H, Nozawa S, Yoshida M, Wada K, Amano H and Miura F;
Japanese Association of Biliary Surgery; Japanese Society of
Hepato-Biliary-Pancreatic Surgery: Japan Society of Clinical
Oncology: Diagnosis of biliary tract and ampullary carcinomas. J
Hepatobiliary Pancreat Surg. 15:31–40. 2008. View Article : Google Scholar
|
|
15.
|
Unno M, Okumoto T, Katayose Y, Rikiyama T,
Sato A, Motoi F, Oikawa M, Egawa S and Ishibashi T: Preoperative
assessment of hilar cholangiocarcinoma by multidetector row
computed tomography. J Hepatobiliary Pancreat Surg. 14:434–440.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Watadani T, Akahane M, Yoshikawa T and
Ohtomo K: Preoperative assessment of hilar cholangiocarcinoma using
multidetector-row CT: correlation with histopathological findings.
Radiat Med. 26:402–407. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Kawamoto S, Siegelman SS, Hruban RH and
Fishman EK: Lymphoplasmacytic sclerosing pancreatitis (autoimmune
pancreatitis): evaluation with multidetector CT. Radiographics.
28:157–170. 2008.PubMed/NCBI
|
|
18.
|
Senda Y, Nishio H, Oda K, Yokoyama Y,
Ebata T, Igami T, Sugiura T, Shimoyama Y, Nimura Y and Nagino M:
Value of multidetector row CT in the assessment of longitudinal
extension of cholangiocarcinoma: correlation between MDCT and
microscopic findings. World J Surg. 33:1459–1467. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Wani NA, Kosar T, Gojwari T, Robbani I,
Choh NA, Shah AI and Khan AQ: Intrabiliary rupture of hepatic
hydatid cyst: multi-detector-row CT demonstration. Abdom Imaging.
36:433–437. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Sasaki R, Kondo T, Oda T, Murata S,
Wakabayashi G and Ohkohchi N: Impact of three-dimensional analysis
of multi-detector row computed tomography cholangioportography in
operative planning for hilar cholangiocarcinoma. Am J Surg.
202:441–448. 2011. View Article : Google Scholar
|
|
21.
|
Ogawa H, Itoh S, Nagasaka T, Suzuki K, Ota
T and Naganawa S: CT findings of intraductal papillary neoplasm of
the bile duct: assessment with multiphase contrast-enhanced
examination using multi-detector CT. Clin Radiol. 67:224–231. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Donato P, Coelho P, Rodrigues H, Vigia E,
Fernandes J, Caseiro-Alves F and Bernardes A: Normal vascular and
biliary hepatic anatomy: 3D demonstration by multidetector CT. Surg
Radiol Anat. 29:575–582. 2007. View Article : Google Scholar : PubMed/NCBI
|