Introduction
Lung cancer is one of the leading causes of
morbidity and mortality worldwide (1). Non-small cell lung cancer (NSCLC)
accounts for >80% of total lung cancer cases. NSCLC may be
removed surgically if diagnosed in the early stages (2). However, the majority of patients are
diagnosed at more advanced stages of the disease when surgery is no
longer possible. Such patients are candidates for chemotherapy,
which is associated with high toxicity and high cost, with limited
efficacy.
Patients undergoing chemotherapy require monitoring
to assess tumor progression. Various techniques, including computed
tomography (CT) and positron-emission tomography (PET), alone and
in combination with specific biomarkers are routinely used
(3). Compared with other methods,
tumor markers provide an economical and convenient method for
detecting early tumor recurrence (4,5).
Several markers have been shown to be sensitive and effective in
monitoring NSCLC (5,6). However, due to their lack of
specificity, the identification of new markers for NSCLC
progression in patients undergoing different chemotherapy regimens
is required.
Cytokeratin 19 (CK 19) is a constituent of the
intermediate filament protein responsible for the structural
integrity of epithelial cells. It has been used as a surrogate
biomarker of circulating tumor cells of epithelial origin,
including adenocarcinoma. A fragment of CK 19, CYFRA 21-1, has been
proposed as a tumor marker for several malignancies, including
NSCLC (5,7).
Carcinoembryonic antigen (CEA) is a cell surface
anchoring protein. It is a member of the immunoglobulin cell
adhesion molecule (IgCAM) superfamily and participates in cell
adhesion. High serum concentrations of CEA have been shown to be
associated with advanced disease and tumor relapse in patients with
NSCLC and other cancers (8,9).
The neuroendocrine marker neuron-specific enolase
(NSE) is a glycolytic enzyme associated with high diagnostic
sensitivity and specificity in small cell lung cancer (SCLC);
however, its use in monitoring the effect of chemotherapy in NSCLC
is controversial (10,11).
The aim of the present study was to evaluate the
prognostic significance of serum tumor markers in predicting the
response to different chemotherapy regimens in patients with
NSCLC.
Patients and methods
Patients
Data from 276 patients diagnosed with NSCLC at the
Department of Pulmonary and Critical Care Medicine, Beijing
Shijitan Hospital, Capital Medical University (Beijing, China)
between February 2009 and October 2012 were retrospectively
reviewed. All patients had a recent histological diagnosis of NSCLC
classified according to the World Health Organization criteria
(12). None of the patients had
received previous treatment for NSCLC and none had a history of
other forms of malignancies. Clinical data were recorded, including
age, gender, disease stage and Eastern Cooperative Oncologic Group
(ECOG) performance status.
The majority of the patients (180 patients, 65.22%)
received a four-cycle chemotherapy regimen or 4 months of treatment
with an epidermal growth factor receptor (EGFR) tyrosine kinase
inhibitor (TKI). A number of patients (63 patients, 22.83%)
received no further treatment. However, 33 patients (11.96%), who
were in disease progression, only received two cycles of
chemotherapy or 2 months of treatment with an EGFR kinase
inhibitor.
Chemotherapy included third-generation
platinum-based regimens used in combination with gemcitabine,
paclitaxel, docetaxel or pemetrexed. Response, based on CT scans
performed every 2 months after treatment, was evaluated according
to the Response Evaluation Criteria in Solid Tumors (RECIST)
criteria (13). Outcomes were
classified as complete response (CR), partial response (PR),
progressive disease (PD) or no change (NC). Written informed
content was obtained from the patients. The study was approved by
the Ethics Committee of Beijing Shijitan Hospital, Capital Medical
University.
Blood samples
Blood samples were collected within 14 days before
surgery or chemotherapy and 3 weeks after completion of the second
or fourth chemotherapy cycles. On the two occasions, CYFRA 21-1,
CEA, NSE, CA 125 and CA 19-9 were measured by automated
electrochemiluminescent assays (Roche Diagnostics GmbH, Mannheim,
Germany).
Statistical analysis
Statistical analysis was performed using SPSS
version 16.0 (SPSS, Inc., Chicago, IL, USA). χ2 and
logistic regression analyses were used to evaluate associations
between tumor response and baseline clinical variables. Independent
sample t-tests were used to analyze correlations between outcome
and blood levels of CEA, CYFRA 21-1, CA 125, CA 19-9 and NSE.
Numerical values for the tumor markers were transformed using
natural logarithms to obtain near normal data distribution.
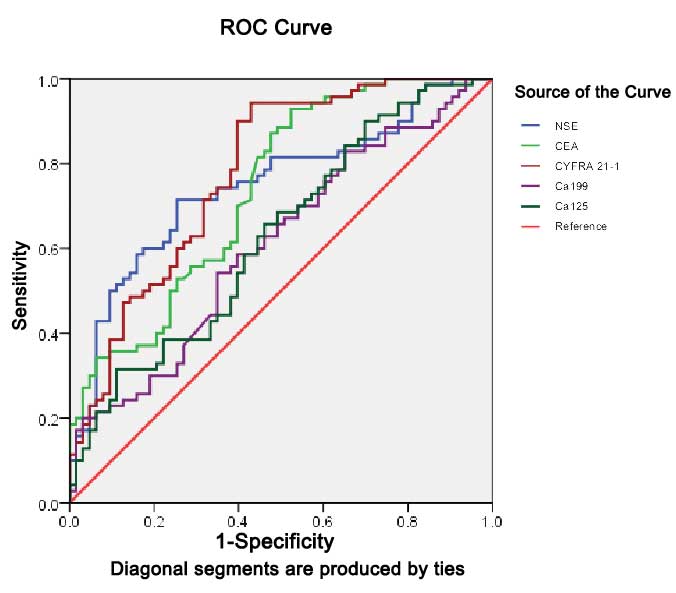
Receiver operating characteristic (ROC) curves were created to
evaluate the role of different tumor markers in predicting the
response to chemotherapy. Cut-off values were determined by the
Youden’s index and the area under the curve was used as a measure
of sensitivity. P<0.05 was considered to indicate a
statistically significant difference.
Results
Decline in CYFRA 21-1 predicts response
for different chemotherapy in NSCLC
The baseline characteristics of the patients
included in the study are shown in Table I. The study included 172 males and
104 females with a median age of 63 years (range, 29–88 years). The
majority of tumors were adenocarcinoma (70.7%); squamous cell
carcinoma (SCC) accounted for 26.1% of tumors and other
histological types for 3.2%. The majority of patients (51.8%)
received surgery, with the exception of those diagnosed as clinical
Stage IV.
 | Table I.Baseline characteristics. |
Table I.
Baseline characteristics.
| Variable | N | (%) |
|---|
| Gender | | |
| Male | 172 | 62.3 |
| Female | 104 | 37.7 |
| ECOG PS score | | |
| ≤1 | 233 | 84.4 |
| >1 | 43 | 15.6 |
| Histological
type | | |
| Squamous cell
carcinoma | 72 | 26.1 |
| Other | 204 | 73.9 |
| Postoperative
stage | | |
| I | 34 | 12.6 |
| II | 44 | 15.9 |
| IIIa | 27 | 9.8 |
| IIIb | 28 | 10.1 |
| IV | 143 | 51.8 |
| Surgery | | |
| Yes | 143 | 51.8 |
| No | 133 | 48.2 |
| First line
treatment | | |
| NO | 63 | 22.8 |
| TP | 73 | 26.4 |
| GP | 54 | 19.6 |
| PP | 47 | 17.0 |
| TKI | 33 | 12.0 |
| Other | 6 | 2.2 |
The treatment response was CR in 64 patients, PR in
47 patients, NC in 69 patients and PD in 96 patients. Based on the
different treatment options, patients were divided into five groups
as follows: a surgery only group (25 SCC and 38 adenocarcinoma
patients); a paclitaxel or docetaxel (TP) group (19 SCC and 54
adenocarcinoma patients); a gemcitabine (GP) group (24 SCC and 30
adenocarcinoma patients); a pemetrexed (PP) group (0 SCC and 47
adenocarcinoma patients) and a TKI group (0 SCC and 33
adenocarcinoma patients). Thirty-two samples (11.6%) were collected
following the second cycle of treatment in cases where the patients
were unable to tolerate further chemotherapy or their response was
evaluated as PD.
Multivariate analysis revealed that performance
status, age, postoperative stage and surgery were significantly
correlated with the response to chemotherapy (Table II). However, there was no
significant association between tumor response and gender, tumor
type, chemotherapy regimen or baseline serum levels of tumor
markers.
 | Table II.Logistic regression analysis of the
correlation between effectiveness of chemotherapy and clinical
factors. |
Table II.
Logistic regression analysis of the
correlation between effectiveness of chemotherapy and clinical
factors.
| Variable | Odds ratio | 95% CI | P-value |
|---|
|
|---|
| Lower | Upper |
|---|
| ECOG PS score | 2.225 | 1.073 | 4.616 | 0.032a |
| Age | 1.053 | 1.009 | 1.099 | 0.018a |
| Gender | 0.759 | 0.353 | 1.631 | 0.480 |
| Histological
type | 0.977 | 0.422 | 2.263 | 0.957 |
| Stage | 2.366 | 1.038 | 5.395 | 0.041a |
| Surgery | 3.441 | 1.431 | 8.273 | 0.006a |
| Chemotherapy
regimen | 1.033 | 0.759 | 1.407 | 0.837 |
| CEA | 1.000 | 0.997 | 1.002 | 0.679 |
| CYFRA 21-1 | 1.010 | 0.983 | 1.038 | 0.465 |
| CA 125 | 0.999 | 0.997 | 1.002 | 0.327 |
Patients were further divided into high and low
tumor marker groups based on the pretreatment marker levels. The
cut-off values that defined these groups are shown in Table III. Correlation analysis revealed
that baseline CYFRA 21-1 (P= 0.047) and CA 19-9 (P<0.001) were
significantly correlated with effectiveness of chemotherapy
(Table III). No similar
associations were identified for CEA, CA 19-9 and NSE (Table III).
 | Table III.Correlation between effectiveness of
chemotherapy and baseline serum levels of tumor markers. |
Table III.
Correlation between effectiveness of
chemotherapy and baseline serum levels of tumor markers.
| Variables | N | CR + PR | NC + PD | χ2 | P-value |
|---|
| CYFRA 21-1
(ng/ml) | | | | | |
| <3.3 | 98 | 53 | 45 | | |
| ≥3.3 | 130 | 50 | 80 | 3.935 | 0.047a |
| CEA (ng/ml) | | | | | |
| <5.0 | 143 | 63 | 80 | | |
| ≥5.0 | 129 | 47 | 82 | 1.636 | 0.201 |
| CA 125 (U/ml) | | | | | |
| <35 | 135 | 69 | 66 | | |
| ≥35 | 107 | 34 | 73 | 0.710 | 0.791 |
| CA 19-9 (U/ml) | | | | | |
| <37 | 210 | 81 | 119 | | |
| ≥37 | 42 | 12 | 30 | 21.885 | <0.001a |
| NSE (ng/ml) | | | | | |
| <17 | 145 | 70 | 75 | | |
| ≥17 | 68 | 25 | 43 | 2.482 | 0.115 |
Table IV shows the
correlations between changes in tumor markers following
chemotherapy and the effectiveness of different chemotherapy
regimens. Reductions in the serum levels of CYFRA 21-1, CEA, CA
19-9 and CA 125 were significantly associated with outcome in the
surgery only group. Reduced serum levels of CEA, CYFRA 21-1 and CA
19-9 were significantly correlated with effectiveness of TP and PP
chemotherapy. CYFRA 21-1 and NSE were significantly associated with
responses to gemcitabine. Responses in the TKI group were
associated with reductions in the serum levels of CEA, CYFRA 21-1
and CA 125.
 | Table IV.Correlation between responses of
tumor markers and effectiveness of different chemotherapy
regimens. |
Table IV.
Correlation between responses of
tumor markers and effectiveness of different chemotherapy
regimens.
| Regimen | CR + PR | NC + PD | t-value | P-value |
|---|
| NO | | | | |
| CEA | 25 | 36 | 3.953 | <0.001a |
| CYFRA 21-1 | 17 | 29 | 2.838 | 0.007a |
| CA 19-9 | 21 | 25 | 2.178 | 0.039a |
| CA 125 | 21 | 30 | 2.361 | 0.025a |
| NSE | 19 | 22 | 1.303 | 0.200 |
| TP | | | | |
| CEA | 34 | 39 | 4.889 | <0.001a |
| CYFRA 21-1 | 32 | 30 | 3.975 | <0.001a |
| CA 19-9 | 24 | 26 | 2.290 | 0.026a |
| CA 125 | 32 | 32 | 1.952 | 0.059 |
| NSE | 23 | 21 | 1.571 | 0.124 |
| GP | | | | |
| CEA | 25 | 27 | 1.912 | 0.062 |
| CYFRA 21-1 | 22 | 20 | 2.419 | 0.020a |
| CA 19-9 | 21 | 22 | 1.004 | 0.327 |
| CA 125 | 22 | 25 | 0.968 | 0.338 |
| NSE | 20 | 18 | 3.003 | 0.004a |
| PP | | | | |
| CEA | 21 | 26 | 3.813 | <0.001a |
| CYFR 21-1 | 20 | 17 | 2.715 | 0.010a |
| CA 19-9 | 18 | 20 | 2.563 | 0.015a |
| CA 125 | 10 | 19 | 1.201 | 0.238 |
| NSE | 16 | 12 | 1.286 | 0.224 |
| TKI | | | | |
| CEA | 5 | 22 | 4.696 | <0.001a |
| CYFRA 21-1 | 6 | 21 | 4.219 | <0.001a |
| CA 19-9 | 5 | 20 | 0.656 | 0.519 |
| CA 125 | 5 | 19 | 2.424 | 0.024a |
| NSE | 6 | 16 | 1.492 | 0.151 |
The reductions of tumor markers in relation to the
effectiveness of chemotherapy are shown in Fig. 1 and Table V. Among all relevant markers, CYFRA
21-1 yielded the most promising sensitivity at 90%. The
corresponding area under the ROC curve was 0.779 (95% CI,
0.700–0.858; P<0001).
 | Table V.Prognostic profile of biomarkers for
responses to chemotherapy. |
Table V.
Prognostic profile of biomarkers for
responses to chemotherapy.
| Marker | AUC | Sensitivity
(%) | Specificity
(%) | 95% CI |
|---|
|
|---|
| Lower | Upper |
|---|
| CEA | 0.738 | 81.4 | 55.6 | 0.654 | 0.822 |
| CYFRA 21-1 | 0.779 | 90.0 | 60.3 | 0.700 | 0.858 |
| CA 19-9 | 0.610 | 62.9 | 54.0 | 0.514 | 0.705 |
| CA 125 | 0.628 | 90.0 | 30.2 | 0.533 | 0.722 |
| NSE | 0.747 | 70.0 | 74.6 | 0.663 | 0.831 |
Discussion
Chemotherapy is one of the main methods of treatment
for NSCLC. Efficacy is routinely evaluated on the basis of
radiological findings; however, this is not conducive to the early
detection of recurrence and metastasis. Consequently, there is
growing demand for convenient tools for estimating prognosis and
for detecting responsiveness to therapy in order to optimize
disease management on an individual basis. Several tumor markers,
including CEA and CYFRA 21-1 in NSCLC, have been previously shown
to provide useful estimates of prognosis (14–16).
However, their role in the evaluation of treatment effectiveness is
controversial, partly due to the lack of comparative studies
evaluating different chemotherapy regimens.
It is well recognized that baseline parameters,
including histology, gender, World Health Organization performance
status, number of positive lymph nodes, gross tumor volume and high
levels of tumor markers are associated with poor chemotherapy
efficacy and poor survival (5,6,17).
In the present study we identified significant associations between
performance status, age, postoperative stage and chemotherapy
response; however, we did not identify similar associations for
gender, tumor type, chemotherapy regimen or baseline tumor
markers.
CYFRA 21-1 is a fragment of CK 19, mainly present in
the cytoplasm of tumor cells of epithelial origin, including lung
and esophageal cancer. Expression of CYFRA 21-1 has been detected
in lung adenocarcinoma and SCC (15). CYFRA 21-1 has also been identified
as a potential tumor marker for the diagnosis and prognosis of
NSCLC. CYFRA 21-1 has previously been identified as a valuable
marker for the individual management of patients with recurrent
NSCLC receiving second-line chemotherapy (18). In the present study we demonstrated
that high serum CYFRA 21-1 levels are indicative of
chemotherapeutic effectiveness in NSCLC. This observation is
consistent with a previous study reporting that baseline serum
levels and changes in CYFRA 21-1 are reliable markers for
chemotherapy response in NSCLC (15).
In the present study patients were analyzed in five
groups according to the type of chemotherapy received. The majority
of patients in the TP and GP groups had NSCLC, while all patients
in the PP and TKI groups had adenocarcinoma. Comparison of the
changes in serum tumor markers in the different groups revealed
that reductions in CYFRA 21-1 were significantly associated with a
positive response to chemotherapy in all groups. This finding may
be related to the fact that CYFRA 21-1 expression is dependent on
tumor stage as opposed to histological type (7,18–20).
Two previous studies (21,22) demonstrated that CYFRA 21-1 is an
independent prognostic factor in the earlier stages of SCC.
However, data from another study (5) suggest that CYFRA 21-1 may be a
reliable surrogate marker of chemotherapy efficacy in patients with
advanced NSCLC.
CYFRA 21-1 is ubiquitously found in a number of body
tissues and has been described as a marker of apoptotic cell death
(23). This suggests that CYFRA
21-1 may be a tumor marker in SCLC as well as in NSCLC. One study
demonstrated that high levels and insufficient reductions of CYFRA
21-1 during the first and second cycles of chemotherapy were
correlated with poor outcome in 128 patients with newly diagnosed
SCLC receiving first-line chemotherapy (19).
CEA is widely used as a tumor marker in lung,
gastrointestinal and gynecological cancers, as well as other
tumors. The majority of patients with NSCLC who have elevated CEA
levels have adenocarcinoma (23–26).
CEA is a member of the IgCAM superfamily and is involved in cell
adhesion and transfer (27,28).
High serum levels of CEA have been shown to be a risk factor for
the development of brain metastasis and are associated with poor
prognosis (9). We identified no
significant association between high baseline serum CEA levels and
a poor response to chemotherapy. However, there was a significant
association between decreased serum CEA levels and the
effectiveness of chemotherapy in the groups where the majority of
patients had adenocarcinoma. CEA may, therefore, represent a
molecular target for lung adenocarcinoma. Similar results were
observed for reductions in serum CA 125 and CA 19-9. All three
markers are derived from glandular cells, which may make them
suitable for monitoring the effectiveness of treatment in lung
adenocarcinoma (29–31). However, these three markers are
non-specific and it may be necessary to combine results for other
biomarkers in order to increase sensitivity and specificity
(6,32,33).
Changes in serum NSE predicted responses only in the
GP group. This may be explained by the fact that the majority of
patients receiving this form of chemotherapy had SCC. Previous
studies have identified NSE as a sensitive tumor marker for SCLC
(10), but not for NSCLC (20,34).
More recent results are contradictory. One study concluded that
patients without elevated NSE mRNA had a better prognosis compared
with patients who experienced an increase in NSE, while another
study concluded that pretreatment NSE mRNA had potential as a
prognostic biomarker for advanced NSCLC (20,35).
Published evidence indicates that the most
convincing data available among potential tumor markers for NSCLC,
is that obtained with CYFRA 21-1 (15,18,36,37).
In the present study, CYFRA 21-1 yielded the most promising
sensitivity (90%) and the largest area under the ROC curve,
compared with the other tumor markers.
This retrospective investigation of prognostic tumor
markers suggests that changes in serum levels of CYFRA 21-1 may be
helpful in predicting the effectiveness of different chemotherapy
regimens used to treat NSCLC. We also identified serum CEA, CA 125
and CA 19-9 as possible prognostic factors in lung
adenocarcinoma.
References
|
1.
|
Oken MM, Hocking WG, Kvale PA, et al:
Screening by chest radiograph and lung cancer mortality: the
Prostate, Lung, Colorectal, and Ovarian (PLCO) randomized trial.
JAMA. 306:1865–1873. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Ferlay J, Parkin DM and Steliarova-Foucher
E: Estimates of cancer incidence and mortality in Europe in 2008.
Eur J Cancer. 46:765–781. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Huang TW, Hsieh CM, Chang H, et al:
Standard uptake value of positron emission tomography in clinical
stage I lung cancer: clinical application and pathological
correlation. Eur J Cardiothorac Surg. 41:869–873. 2012. View Article : Google Scholar
|
|
4.
|
Sawabata N, Maeda H, Yokota S, et al:
Postoperative serum carcinoembryonic antigen levels in patients
with pathologic stage IA nonsmall cell lung carcinoma: subnormal
levels as an indicator of favorable prognosis. Cancer. 101:803–809.
2004. View Article : Google Scholar
|
|
5.
|
Ardizzoni A, Cafferata MA, Tiseo M, et al:
Decline in serum carcinoembryonic antigen and cytokeratin 19
fragment during chemotherapy predicts objective response and
survival in patients with advanced nonsmall cell lung cancer.
Cancer. 107:2842–2849. 2006. View Article : Google Scholar
|
|
6.
|
Dehing-Oberije C, Aerts H, Yu S, et al:
Development and validation of a prognostic model using blood
biomarker information for prediction of survival of non-small-cell
lung cancer patients treated with combined chemotherapy and
radiation or radiotherapy alone (NCT00181519, NCT00573040, and
NCT00572325). Int J Radiat Oncol Biol Phys. 81:360–368. 2011.
|
|
7.
|
Pujol JL, Molinier O, Ebert W, et al:
CYFRA 21-1 is a prognostic determinant in non-small-cell lung
cancer: results of a meta-analysis in 2063 patients. Br J Cancer.
90:2097–2105. 2004.PubMed/NCBI
|
|
8.
|
Grunnet M and Sorensen JB:
Carcinoembryonic antigen (CEA) as tumor marker in lung cancer. Lung
Cancer. 76:138–143. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Arrieta O, Saavedra-Perez D, Kuri R, et
al: Brain metastasis development and poor survival associated with
carcinoembryonic antigen (CEA) level in advanced non-small cell
lung cancer: a prospective analysis. BMC Cancer. 9:1192009.
View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Emin Erbaycu A, Gunduz A, Batum O, Zeren
Ucar Z, Tuksavul F and Zeki Guglu S: Pre-treatment and
treatment-induced neuron-specific enolase in patients with
small-cell lung cancer: an open prospective study. Arch
Broncopneumol. 46:364–369. 2010.(In Spanish).
|
|
11.
|
Jin B, Huang AM, Zhong RB and Han BH: The
value of tumor markers in evaluating chemotherapy response and
prognosis in Chinese patients with advanced non-small cell lung
cancer. Chemotherapy. 56:417–423. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Travis WD: Pathology and genetics: tumours
of the lung, pleura, thymus and heart. 7. Iarc; 2004
|
|
13.
|
Eisenhauer EA, Therasse P, Bogaerts J, et
al: New response evaluation criteria in solid tumours: revised
RECIST guideline (version 1.1). Eur J Cancer. 45:228–247. 2009.
View Article : Google Scholar
|
|
14.
|
Seemann MD, Beinert T, Fürst H and Fink U:
An evaluation of the tumour markers, carcinoembryonic antigen
(CEA), cytokeratin marker (CYFRA 21-1) and neuron-specific enolase
(NSE) in the differentiation of malignant from benign solitary
pulmonary lesions. Lung Cancer. 26:149–155. 1999. View Article : Google Scholar
|
|
15.
|
Edelman MJ, Hodgson L, Rosenblatt PY, et
al: CYFRA 21-1 as a prognostic and predictive marker in advanced
non-small-cell lung cancer in a prospective trial: CALGB 150304. J
Thorac Oncol. 7:649–654. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Alataş F, Alataş O, Metintaş M, Colak O,
Harmanci E and Demir S: Diagnostic value of CEA, CA 15-3, CA 19-9,
CYFRA 21-1, NSE and TSA assay in pleural effusions. Lung Cancer.
31:9–16. 2001.PubMed/NCBI
|
|
17.
|
Li CG, Huang XE, Xu L, Li Y and Lu YY:
Clinical application of serum tumor associated material (TAM) from
non-small cell lung cancer patients. Asian Pac J Cancer Prev.
13:301–304. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Holdenrieder S, von Pawel J, Dankelmann E,
et al: Nucleosomes and CYFRA 21-1 indicate tumor response after one
cycle of chemotherapy in recurrent non-small cell lung cancer. Lung
Cancer. 63:128–135. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Holdenrieder S, von Pawel J, Dankelmann E,
et al: Nucleosomes, ProGRP, NSE, CYFRA 21-1, and CEA in monitoring
first-line chemotherapy of small cell lung cancer. Clin Cancer Res.
14:7813–7821. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Alm El-Din MA, Farouk G, Nagy H, Abd
Elzaher A and Abo El-Magd GH: Cytokeratin-19 fragments, nucleosomes
and neuron-specific enolase as early measures of chemotherapy
response in non-small cell lung cancer. Int J Biol Marker.
27:e139–e146. 2012.PubMed/NCBI
|
|
21.
|
Kulpa J, Wójcik E, Reinfuss M and
Kolodziejski L: Carcinoembryonic antigen, squamous cell carcinoma
antigen, CYFRA 21-1, and neuron-specific enolase in squamous cell
lung cancer patients. Clin Chem. 48:1931–1937. 2002.PubMed/NCBI
|
|
22.
|
Song WA, Liu X, Tian XD, et al: Utility of
squamous cell carcinoma antigen, carcinoembryonic antigen, Cyfra
21-1 and neuron specific enolase in lung cancer diagnosis: a
prospective study from China. Chin Med J (Engl). 124:3244–3248.
2011.PubMed/NCBI
|
|
23.
|
Sheard MA, Vojtesek B, Simickova M and
Valik D: Release of cytokeratin-18 and -19 fragments (TPS and CYFRA
21-1) into the extracellular space during apoptosis. J Cell
Biochem. 85:670–677. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Matsuoka K, Sumitomo S, Nakashima N,
Nakajima D and Misaki N: Prognostic value of carcinoembryonic
antigen and CYFRA21-1 in patients with pathological stage I
non-small cell lung cancer. Eur J Cardiothorac Surg. 32:435–439.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Tomita M, Shimizu T, Ayabe T, Yonei A and
Onitsuka T: Prognostic significance of tumour marker index based on
preoperative CEA and CYFRA 21-1 in non-small cell lung cancer.
Anticancer Res. 30:3099–3102. 2010.PubMed/NCBI
|
|
26.
|
Tomida M, Mikami I, Takeuchi S, Nishimura
H and Akiyama H: Serum levels of nicotinamide N-methyltransferase
in patients with lung cancer. J Cancer Res Clin Oncol.
135:1223–1229. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
Iwanicki-Caron I, Di Fiore F, Roque I, et
al: Usefulness of the serum carcinoembryonic antigen kinetic for
chemotherapy monitoring in patients with unresectable metastasis of
colorectal cancer. J Clin Oncol. 26:3681–3686. 2008. View Article : Google Scholar
|
|
28.
|
Konstantopoulos K and Thomas SN: Cancer
cells in transit: the vascular interactions of tumor cells. Annu
Rev Biomed Eng. 11:177–202. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29.
|
Thomas SN, Zhu F, Schnaar RL, Alves CS and
Konstantopoulos K: Carcinoembryonic antigen and CD44 variant
isoforms cooperate to mediate colon carcinoma cell adhesion to E-
and L-selectin in shear flow. J Biol Chem. 283:15647–15655. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
30.
|
Thomas SN, Tong Z, Stebe KJ and
Konstantopoulos K: Identification, characterization and utilization
of tumor cell selectin ligands in the design of colon cancer
diagnostics. Biorheology. 46:207–225. 2009.PubMed/NCBI
|
|
31.
|
Nuñez GR, Ito C and Del Giglio A:
Increased serum CA-125 levels in patients with lung cancer post
thoracotomy. South Med J. 102:427–428. 2009.PubMed/NCBI
|
|
32.
|
Li X, Asmitananda T, Gao L, et al:
Biomarkers in the lung cancer diagnosis: a clinical perspective.
Neoplasma. 59:500–507. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
33.
|
Muley T, Fetz TH, Dienemann H, et al:
Tumor volume and tumor marker index based on CYFRA 21-1 and CEA are
strong prognostic factors in operated early stage NSCLC. Lung
Cancer. 60:408–415. 2008.PubMed/NCBI
|
|
34.
|
Ma S, Shen L, Qian N and Chen K: The
prognostic values of CA125, CA19.9, NSE, AND SCC for stage I NSCLC
are limited. Cancer Biomark. 10:155–162. 2011.PubMed/NCBI
|
|
35.
|
Wang Y, Tang D, Sui A, et al: Prognostic
significance of NSE mRNA in advanced NSCLC treated with gefitinib.
Clin Transl Oncol. 15:384–390. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
36.
|
Gridelli C, Rossi A and Maione P:
Treatment of non-small-cell lung cancer: state of the art and
development of new biologic agents. Oncogene. 22:6629–6638. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
37.
|
Wang J, Zhang N, Li B, et al: Decline of
serum CYFRA21-1 during chemoradiotherapy of NSCLC: a probable
predictive factor for tumor response. Tumour Biol. 32:689–695.
2011. View Article : Google Scholar : PubMed/NCBI
|