Introduction
Splenogonadal fusion (SGF) is a rare congenital
anomaly in which close proximity of spleen and gonad during early
embryological development facilitates fusion. SGF may be divided
into continuous or discontinuous types. The continuous type of SGF
describes the gonad attached to the spleen. The discontinuous type
consists of gonadal fusion with an accessory spleen or ectopic
splenic tissue. The diagnosis of this uncommon anomaly is rare and
difficult to diagnose preoperatively. Certain patients with SGF
have undergone unnecessary orchidectomy due to the presence of a
testicular lump (1). Therefore,
re-evaluation of the diagnosis and surgical treatment of SGF is
necessary. In the current study, we report four cases of children
with SGF, three of which were treated by laparoscopy. Combined with
the relevant literature, we discuss the diagnosis and treatment of
SGF, and the value of exploration by laparoscopy. This study was
approved by the ethics committee of The First Affiliated Hospital
of Xinjiang Medical University. The informed consent was obtained
from the family of all patients.
Case reports
Case 1
A male, 6 years old, presented with a painless mass
in the left scrotum. Upon physical examination, a swollen testicle
~2.5×2.5×4.5 cm3 in size, of medium hardness without any
tenderness was palpable in the left scrotum. Surgery was performed
under general anesthesia. During the surgery, a reddish-brown mass
attached to the upper pole of the left testis was identified. The
mass and testis were free from other intra-abdominal structures.
The mass was confined to an intact capsule on the upper pole of the
testis and occupied one-third of the volume of the testis.
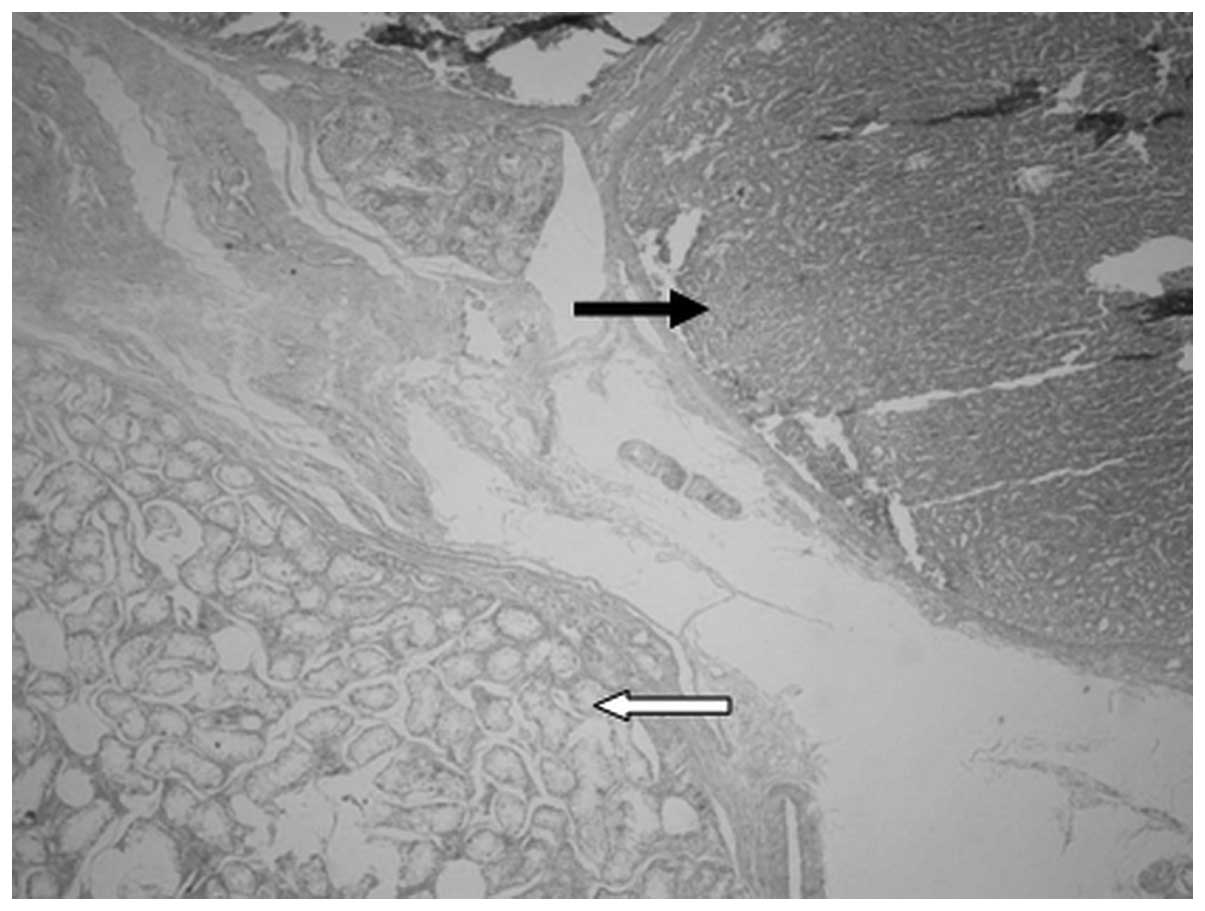
Postoperative examination of the specimen under the microscopic
revealed it was spleen tissue that was separated from the
surrounding compressed testicular tissue (Fig. 1).
Case 2
A male, 7 years old, presented with a left inguinal
mass. It was a soft mass with a clear boundary, which was palpable
from the left groin area to the scrotum, but was not able to be
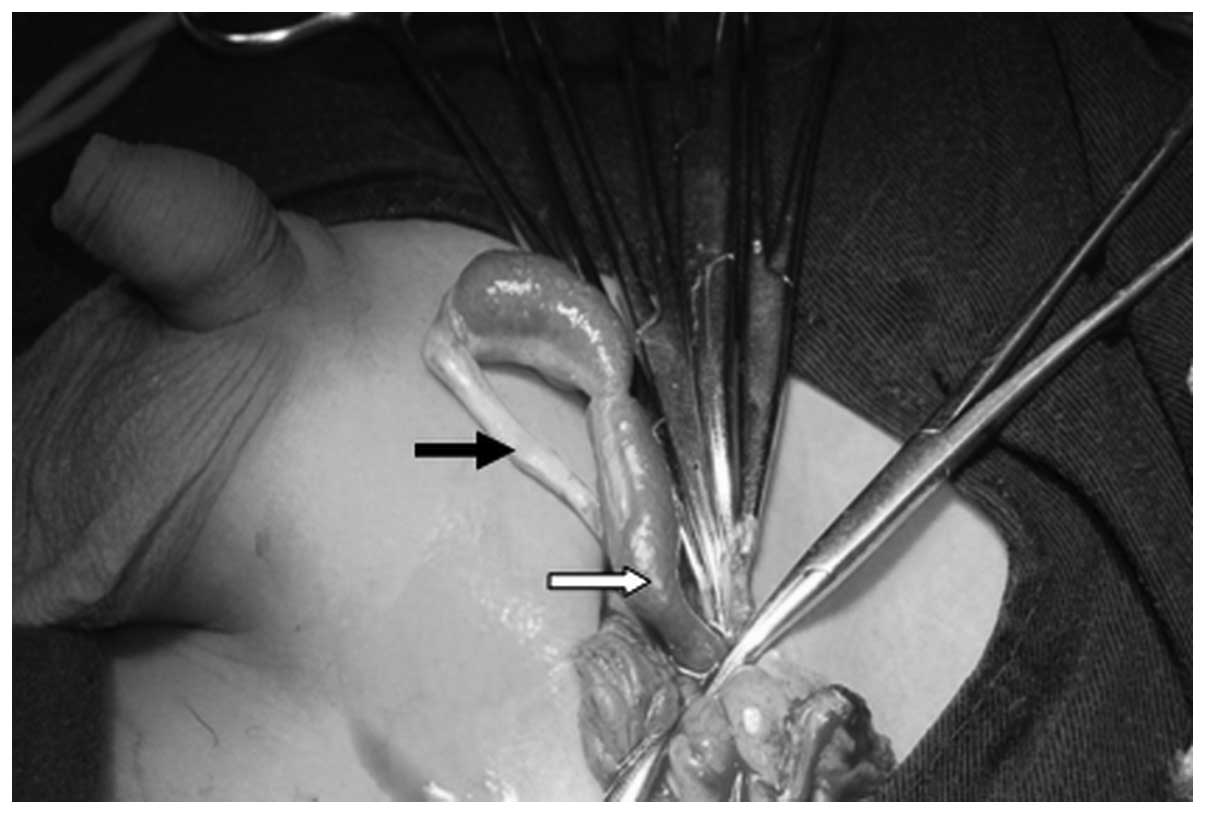
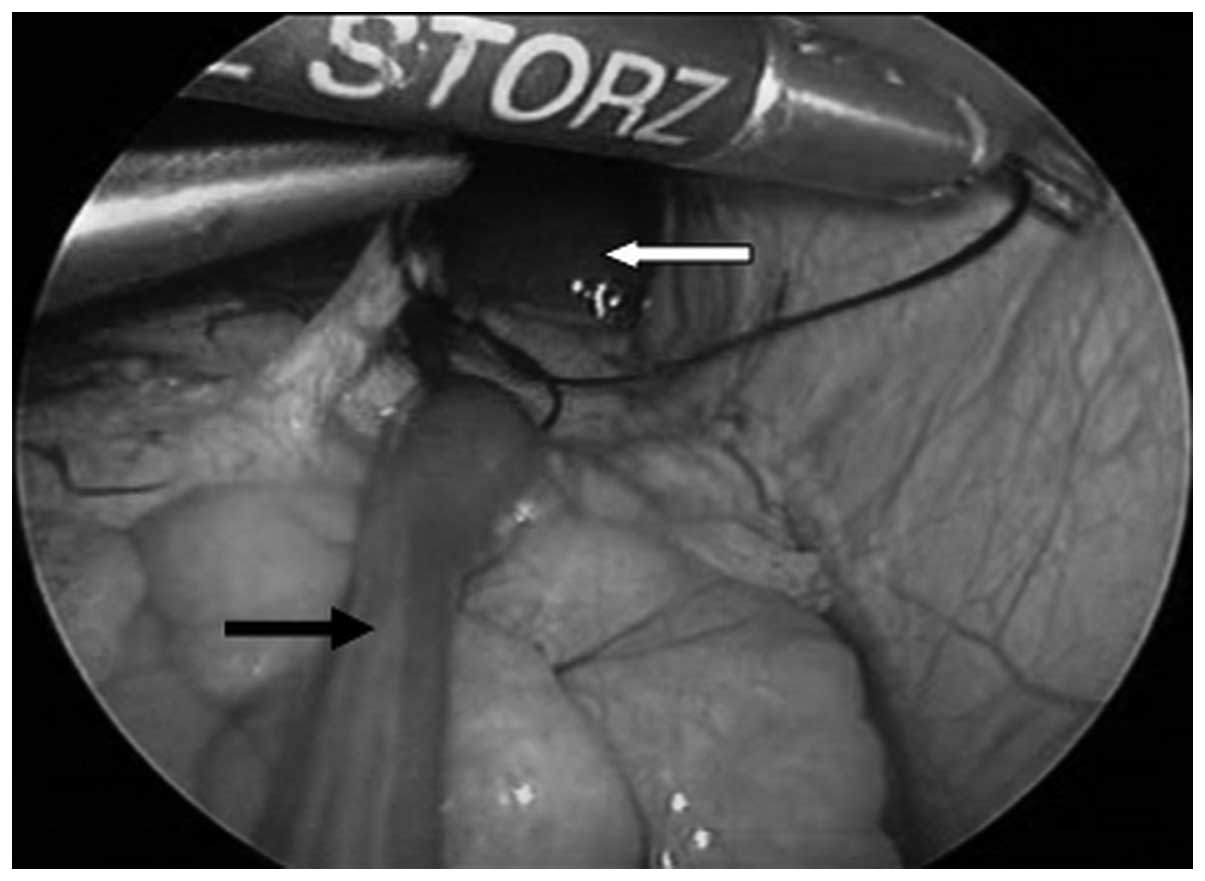
completely pushed back into the abdominal cavity. During
laparoscopy, a congenital hernia was confirmed by the red cord-like
tissue in the left inguinal region that connected to the testicle,
entered into the left internal inguinal ring and were fused to the
hilum of the spleen. The diameter of the cord-like tissue was ~1.0
cm. The proximal cord-like tissue was ligatured prior to being
resectioned (Figs. 2 and 3). Postoperative examination of the
specimen under the microscope revealed it was spleen tissue.
Case 3
A male, 2-years-old, presented with bilateral
undescendent testes. The penis was bent downwards, while the
urethra was located at the junction of the penis and scrotum. The
testis were not palpable in bilateral scrotums and bilateral
inguinal region. Ultrasound demonstrated there was no
testicular-like mass in the bilateral inguinal and abdominal
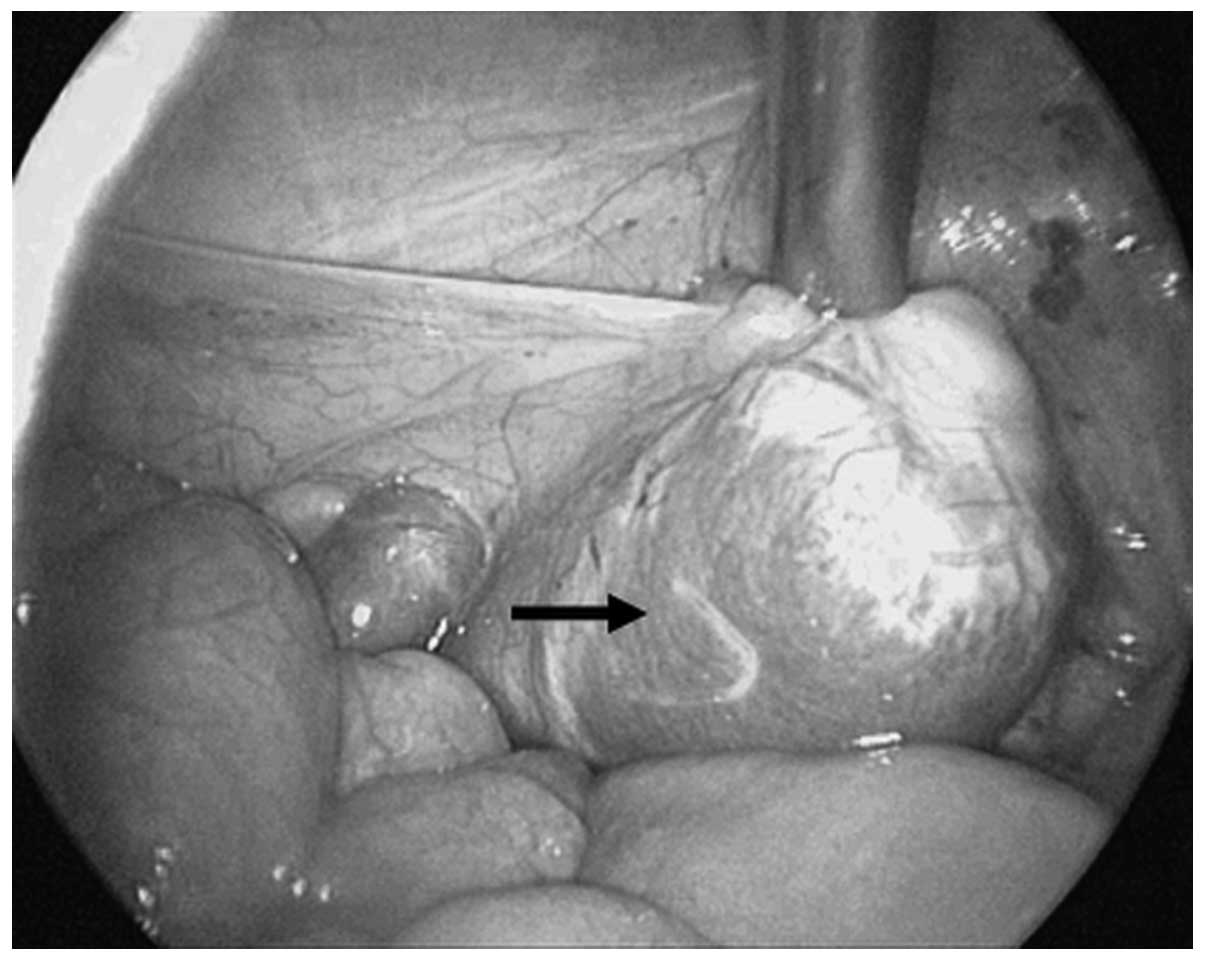
cavities. During laparoscopy, a testicle-like mass was located in
the left iliac fossa. It was dark red, with clear fixed boundaries
and measured 2.0×3.0×4.0 cm3 (Fig. 4). The removal of the left
testis-like mass was followed by the high ligature of the spermatic
vein. The right testicle was pulled down and fixed in a secondary
surgery. Pathological examination of the mass revealed SGF.
Case 4
A male, 12-years-old, presented with bilateral
undescendent testes. The penis had a postoperative appearance, a
bend in it having been corrected. The urethra was located in the
glands. The bilateral scrota were underdeveloped, without the
testis. Surgical scars were visible at the bilateral inguinal
region, but there was no testis-like mass. An oval-shaped mass
shadow on the lower pole of the left kidney was confirmed by MRI.
It was ~2.3×4.0 cm2 in size with a uniform signal and
clear boundary. The location and shape of the spleen was noted to
be normal during the laparoscopy. A testis-like reddish brown mass
was observed that was attached to the lower pole of the left
kidney, with clear, fixed boundaries and measuring 2.0×2.5×4.0
cm3. The right testicle was pulled down and fixed, while
the left, testis-like mass was removed. Pathological examination of
the specimen obtained from the left side revealed SGF.
Discussion
SGF is a rare congenital anomaly, between the spleen
and a gonad or mesonephric derivatives, almost always presenting on
the left side in males. The male preponderance may be due to the
fact that the male sex gland is located superficially and is easily
located. Female gonads are inside the body and have fewer
complications than their male counterparts. SGF is often discovered
accidentally during gynecological surgery, with a higher prevalence
in Caucasian individuals, followed by that in African descent and
other ethnicity (2,3). SGF is common in children and
adolescents. The number of cases reported in patients <10 years
of age account for 50% of the total cases reported, while patients
<20 years old account for 70% (1). The four patients in the current study
are all male, three of the four patients are <10 years old, and
all anomalies occurred on the left side.
SGF may be classified into two types, continuous and
discontinuous, but clinically there are no significant differences
between the two types (4). Le Roux
and Heddle (5) speculated that
discontinuous SGF is a rare type of lienculus. Case 2 is an example
of continuous SGF, and postoperative examination of the specimen
under a microscope revealed that it was spleen tissue. The other
three cases are examples of discontinuous SGF in which no cord-like
tissue was connected with the spleen.
Cryptorchidism and inguinal hernias are the most
common malformations associated with SGF. In total, 31% of SGF
patients are diagnosed with cryptorchidism or inguinal hernias, and
in 59% of cases the cryptorchidism is diagnosed as bilateral
(6). In cases of continuous SGF,
~50% are accompanied by other congenital malformations (7). The incidence rate for continuous SGF
is five-fold higher than that of discontinuous SGF and most cases
are accompanied by limb defect syndrome (8,9).
Bonneau et al(10) reviewed
29 cases of splenogonadal fusion limb defect syndrome (SGFLD), of
which 24 cases (82.7%) were continuous SGF, while 70% were
associated with micrognathia. Approximately one-fifth of continuous
SGF cases also have other major congenital defects, such as limb
hypoplasia, micrognathia, cardiac defects, palatal defects and anal
defects. Karaman and Gonzales (4)
reported a case of both transverse testicular ectopia and SGF. In
the current study, case 1 has no associated malformation, case 2
has a left inguinal hernia and cases 3 and 4 have bilateral
cryptorchidism and hypospadias.
The diagnosis of SGF prior to surgery is
challenging. SGF typically presents as an asymptomatic testicular
mass and other manifestations may include acute testicular pain and
swelling caused by ectopic splenic tissue infections (11), but the actual disease itself lacks
characteristic features. In the current study, case 1 was
undergoing treatment due to a left scrotal mass, case 2 was
undergoing treatment for a left inguinal hernia and cases 3 and 4
were being treated for bilateral cryptorchidism. All four cases
were inaccurately diagnosed prior to surgery. The lack of awareness
of SGF is a major factor in its misdiagnosis. Imaging methods,
including B-type ultrasonography, computed tomography (CT),
magnetic resonance imaging(MRI) and 99TCm
spleen scanning, aid with the diagnosis of SGF (12–15).
However, laparoscopies have achieved improved diagnoses and
management of SGF (16). In the
current study, three of the four cases were treated by laparoscopy,
which aided with diagnosis and surgery.
The decision to resection the entire splenogonadal
tissue was based upon the anomalous appearance of the testicle and
its fusion to ectopic splenic tissue. Once an accurate diagnosis
has been achieved without significant complications, particularly
in the scrotum, no surgery is required. Even if surgery is
performed, in most cases the testis may be preserved. Performing
laparoscopy and testicle-sparing surgery is advised. Spleen tissue
is easily separated from the gonad and as a result the testis may
be retained, unless there is a high degree of cryptorchidism. If a
tumor is suspected, frozen sectioning may aid with the diagnosis.
Currently, to the best of our knowledge, there have been no reports
of malignant SGF.
In conclusion, the diagnostic evaluation of patients
with an abnormal gonad is complex due to multifactorial
etiopathogenesis and the rarity the condition. The primary aim of
diagnosis is to rule out malignancy. We suggest three steps that
should be considered when diagnosing and treating SGF. Firstly, a
mass found at birth growing slowly for several years in a benign
condition should be considered. Secondly, various imaging
techniques should be used to investigate the nature of the mass.
Thirdly, in doubtful cases, a biopsy should performed during
surgery or, preferably prior to making an incision, for example, by
needle biopsy, punch biopsy or a classical bivalve biopsy and
regional node evaluation. If the mass proves to be malignant, a
radical resection should be performed immediately. If the
malignancy is unconfirmed, an orchiectomy is sufficient for further
pathological study. In cases where the mass has been identified to
be benign, but the organ has been opened, removal of splenic tissue
may be performed. With SGF, there may be no need for surgery.
However, diagnosis and surgical treatment by a diagnostic
laparoscopy are suggested. Laparoscopy is a safe and reliable
approach that is highly accurate in the diagnosis and treatment of
nonpalpable testis.
References
|
1
|
Shen XC, Du CJ, Chen JM, Zhang ZW and Qiu
YQ: Splenogonadal fusion. Chin Med J (Engl). 121:383–384.
2008.PubMed/NCBI
|
|
2
|
Molaeian M and Shojaei H: Splenogonadal
fusion presented with cryptorchidism. Urol J. 6:130–131.
2009.PubMed/NCBI
|
|
3
|
McPherson F, Frias JL, Spicer D, Opitz JM
and Gilbert-Barness EF: Splenogonadal fusion-limb defect ‘syndrome’
and associated malformations. Am J Med Genet A. 120A:518–522.
2003.
|
|
4
|
Karaman MI and Gonzales ET Jr:
Splenogonadal fusion: report of 2 cases and review of the
literature. J Urol. 155:309–311. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Le Roux PJ and Heddle RM: Splenogonadal
fusion: is the accepted classification system accurate? BJU Int.
85:114–115. 2000.PubMed/NCBI
|
|
6
|
Cortes D, Thorup JM and Visfeldt J: The
pathogenesis of cryptorchidism and splenogonadal fusion: a new
hypothesis. Br J Urol. 77:285–290. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lin CS, Lazarowicz JL, Allan RW and
Maclennan GT: Splenogonadal fusion. J Urol. 184:332–333. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Basbug M, Akgun H, Ozgun MT, Turkyilmaz C,
Batukan C and Ozcelik B: Prenatal sonographic findings in a fetus
with splenogonadal fusion limb defect syndrome. J Clin Ultrasound.
37:298–301. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gouw AS, Elema JD, Bink-Boelkens MT, de
Jongh HJ and ten Kate LP: The spectrum of splenogonadal fusion.
Case report and review of 84 reported cases. Eur J Pediatr.
144:316–323. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bonneau D, Roume J, Gonzalez M, et al:
Splenogonadal fusion limb defect syndrome: report of five new cases
and review. Am J Med Genet. 86:347–358. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Stewart VR, Sellars ME, Somers S, Muir GH
and Sidhu PS: Splenogonadal fusion: B-mode and color Doppler
sonographic appearances. J Ultrasound Med. 23:1087–1090.
2004.PubMed/NCBI
|
|
12
|
Netto JM, Pérez LM, Kelly DR, Joseph DB
and Royal SA: Splenogonadal fusion diagnosed by Doppler
ultrasonography. Scientific World Journal. 4:253–257. 2004.
View Article : Google Scholar
|
|
13
|
Li YH: Preoperative detection of
splenogonadal fusion by CT. Surg Radiol Anat. 31:733–735. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Varma DR, Sirineni GR, Rao MV, Pottala KM
and Mallipudi BV: Sonographic and CT features of splenogonadal
fusion. Pediatr Radiol. 37:916–919. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Alalayet YF, Mansoor K, Shiba NA, Khan AM
and Al Kasim F: Splenogonadal fusion. Eur J Pediatr Surg.
18:342–344. 2008. View Article : Google Scholar
|
|
16
|
Papparella A, Nino F, Coppola S,
Donniacono D and Parmeggiani P: Laparoscopy in the diagnosis and
management of splenogonadal fusion: case report. Eur J Pediatr
Surg. 21:203–204. 2011. View Article : Google Scholar
|