Introduction
Cervical spondylotic myelopathy (CSM) is a
degenerative disease of the cervical spine in which the severity of
clinical signs and symptoms depends on the pathophysiology of the
spinal cord. Since osteoarthritic degeneration of the cervical
spine may provoke irreversible damage to the spinal cord and delays
in surgical treatment tend to result in a poor outcome (1–3),
early decompression surgery is usually recommended for patients
with a definite diagnosis of moderate or severe CSM (4–6).
However, in patients with mild, non-progressive or slowly
progressive CSM, a relatively benign natural course has been
observed (7,8) and the superiority of surgical
treatment over conservative treatment has not been established
(9–11). It appears that conservative
treatment is the preferred choice for these patients since it
avoids the complications of surgery and is less expensive (12,13).
However, even with the same treatment protocols, the outcome of
conservative treatment for mild forms of CSM (MCSM) varies between
individuals. Although efforts have been made to determine
prognostic factors for the deterioration of MCSM, results remain
highly controversial (7,8,14–16).
Furthermore, for MCSM patients with adverse prognostic factors,
little is known with regard to the optimal timing of surgery.
Surgeons are faced with a dilemma as to whether surgery should be
performed as early as possible or only after conservative treatment
has failed.
With the aim of providing evidence-based guidelines
for the effective treatment of MCSM, the present prospective study
was conducted to investigate the clinical outcome of conservative
treatment, identify factors associated with the prognosis of
conservative treatment and to verify whether it is too late to
perform surgical procedures after conservative treatment fails.
Materials and methods
Inclusion and exclusion criteria
Following approval from the ethics committee of The
Third Hospital of Hebei Medical University (Shijiazhuang, China),
90 MCSM patients attending The Third Hospital of Hebei Medical
University (Shijiazhuang, China) between February 2007 and January
2009 were prospectively enrolled in this study, and informed
consent was obtained from all patients. Inclusion criteria for
patients were as follows: objective clinical findings of CSM, for
example, increased deep tendon reflexes, positive pathological
reflexes and abnormal sensory disturbances; correlative spinal cord
compression on magnetic resonance imaging (MRI); a Japanese
Orthopedic Association (JOA) score (Table I) of ≥13; a recent non-progressive
process; and consent provided for the recommended treatment plan.
Patients with ossification of the posterior longitudinal ligament,
traumatic cervical myelopathy, motor neurone disease, multiple
sclerosis, progressive polyarthritis, congenital anomalies and
vitamin B12 deficiency were excluded from the study.
 | Table IJapanese Orthopaedic Association (JOA)
scores for assessment of cervical myelopathy. |
Table I
Japanese Orthopaedic Association (JOA)
scores for assessment of cervical myelopathy.
| Category | Score (points) |
|---|
| Motor function of the
upper extremity |
| Unable to eat with
either chopsticks or a spoon | 0 |
| Able to eat with a
spoon, but not with chopsticks | 1 |
| Able to eat with
chopsticks, but inadequately | 2 |
| Able to eat with
chopsticks, but awkwardly | 3 |
| Normal | 4 |
| Motor function of the
lower extremity |
| Unable to walk | 0 |
| Needs a cane or
other walking aid on flat ground | 1 |
| Needs walking aid
only on stairs | 2 |
| Able to walk
unaided, but slowly | 3 |
| Normal | 4 |
| Sensory function |
| Upper extremity |
| Apparent sensory
disturbance | 0 |
| Minimal sensory
disturbance | 1 |
| Normal | 2 |
| Lower extremity |
| Apparent sensory
disturbance | 0 |
| Minimal sensory
disturbance | 1 |
| Normal | 2 |
| Trunk |
| Apparent sensory
disturbance | 0 |
| Minimal sensory
disturbance | 1 |
| Normal | 2 |
| Bladder function |
| Urinary retention or
incontinence | 0 |
| Severe dysuria
(sense of retention) | 1 |
| Slight dysuria
(pollakiuria, retardation) | 2 |
| Normal | 3 |
Treatment protocol
Each patient was hospitalized and received treatment
according to the following protocol. The initial treatment
comprised continuous cervical traction [Good-Samaritan traction
(17)] in which the neck of the
patient was placed in a position of slight flexion for 8 h per day
for ~2 weeks. Regardless of the outcome of cervical traction,
patients were discharged. Hyper-extended or hyper-flexed neck
positions, slips and falls, intense exercise and other potentially
dangerous activities in daily life were avoided at home. Patients
were followed up periodically every three months and advised to
visit the hospital immediately if their symptoms became
exacerbated. Surgery was performed on patients who experienced a
deterioration of myelopathy that resulted in JOA scores of <13
with a reduction of ≥2 points.
Surgical protocol
The procedures included anterior and posterior
approaches, the choice of which depended on the cervical alignment
and the levels and sources of compression. Anterior discectomy
followed by autologous bone grafting and cervical plate fixation
were adopted for patients with 1- or 2-level compression,
particular those with greater compression on the anterior side. In
patients exhibiting preserved cervical lordosis and >3-level
canal stenosis, C3 to C6 (or C7) laminoplasty was performed. In the
case of significant compression on the posterior side, laminoplasty
was also selected, even if the patients exhibited <3-level
compression. All surgeries were performed within one month of
deterioration of myelopathy. At the end of the study, all
surgically treated patients were followed up for ≥1 year
postoperatively.
Outcome assessments
In order to analyze the prognostic factors, relevant
clinical factors, including gender, age and duration of disease,
were collected from the records of the patients. On the first visit
to the hospital, all patients underwent plain antero-posterior,
lateral and extension-flexion radiographs with a tube-to-film
distance of 120 cm. All patients underwent high-resolution MRI with
a 1.5-T imager (Siemens Magnetom Symphony; Siemens, Berlin,
Germany). The conditions for the MRI study were as previously
described (3). Plain radiographs
and MRI yielded imaging parameters as follows: The C2–C7 angle was
measured using the Cobb method, which was determined by the
inferior margin of C2 body and the inferior margin of C7 body on
lateral radiographs; segmental instability was considered to be
present if >2 mm of slippage displacement was observed on
extension-flexion radiographs at the compression-affected levels
(18). The sagittal diameters of
the cerebrospinal fluid (CSF) column were measured at the
mid-vertebra level on T2 sagittal MRI from C4 to C7, and the mean
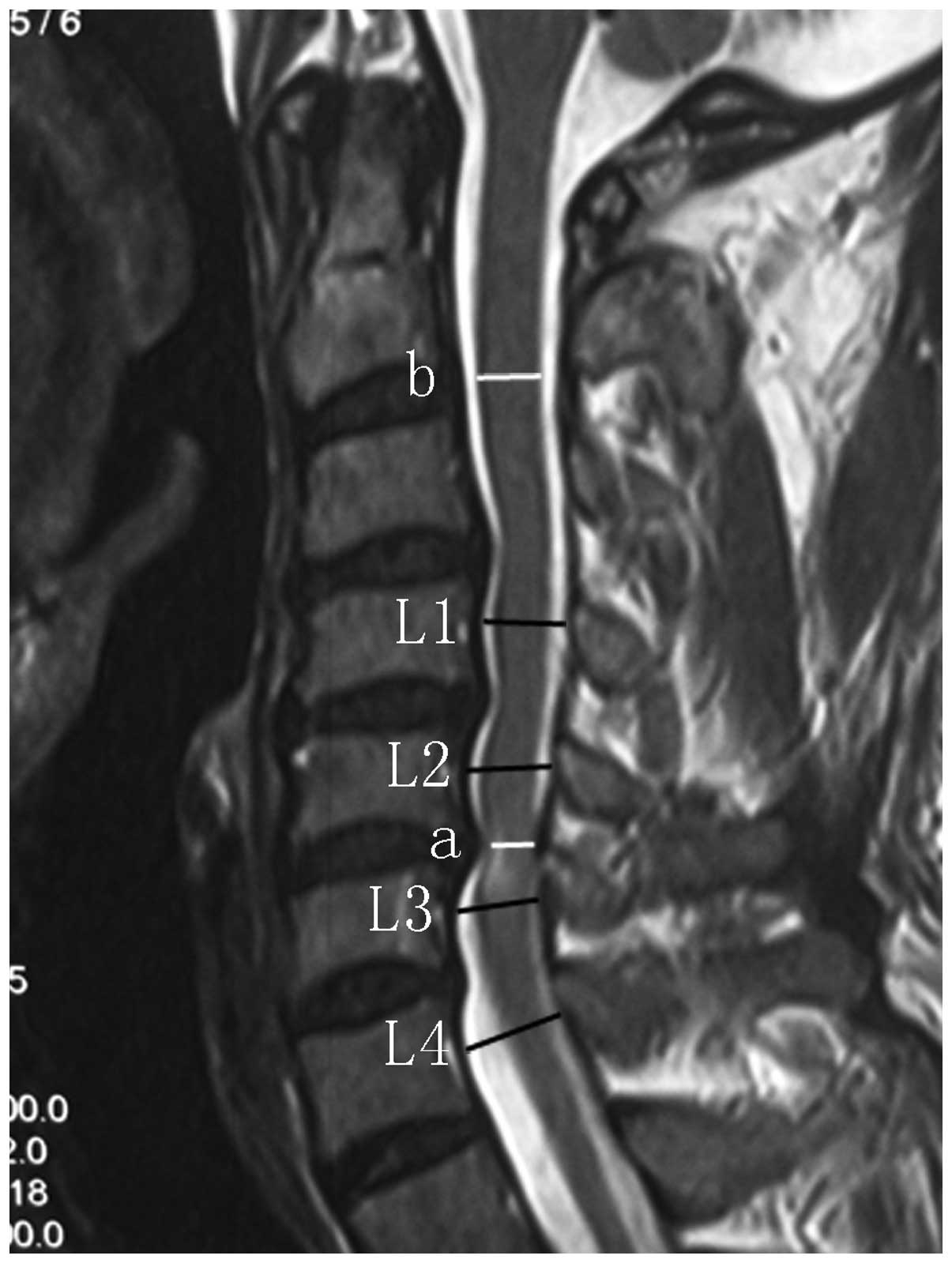
value was calculated (Fig. 1). The
extent of spinal cord compression was defined by the ratio of the
spinal cord diameter of the narrowest part to that of the C2/3
intervertebral level using sagittal images on T2-weighted MRI
(Fig. 1). The number of
compression-affected levels on T2-weighted MRI was also recorded.
Data measurements were performed twice by a single observer and the
mean value was used for analysis.
To investigate treatment outcomes, JOA scores at the
time of the initial visit and final follow-up were analyzed. For
patients who neurologically deteriorated and therefore underwent
surgery, JOA scores at the time of conversion to surgery were also
evaluated.
To determine which prognostic factors correlated
with failed conservative treatment, each of the clinical and
radiological factors was compared between patients who were treated
conservatively throughout and those who had undergone surgery by
the final follow-up.
Statistical analysis
A parametric analysis was performed using the
Mann-Whitney U test. Categorical variables were analyzed using the
Fisher's exact test. The Statistical Package for the Social
Sciences (version 13.0 for Windows; SPSS, Inc., Chicago, IL, USA)
was used for the statistical analysis. P<0.05 was considered to
indicate a statistically significant difference.
Results
A total of 90 patients with MCSM were enrolled in
this study. By the end of January 2012, nine patients had withdrawn
from the study, one patient was affected by an acute spinal cord
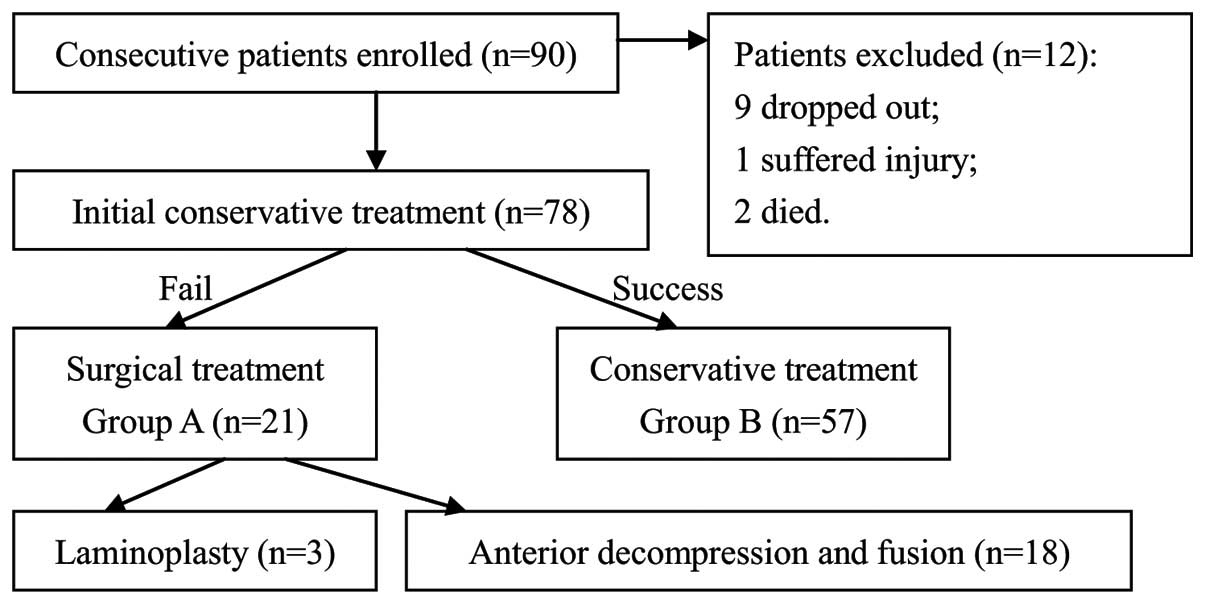
injury and two patients had succumbed to unrelated causes (Fig. 2). At the final follow-up, 78 (45
male and 33 female) of 90 patients (follow-up rate, 86.7%) were
investigated. The average age at first visit was 57.8 years (range,
37–71 years). The average follow-up period was 40 months (range,
36–56 months). The mean JOA scores at the time of the first and the
last follow-up were 14.1 points (range, 13–16 points) and 14.0
points (range, 10–16 points), respectively (Table II).
 | Table IIBaseline demographic
characteristics. |
Table II
Baseline demographic
characteristics.
| Variable | Value |
|---|
| No. of patients | 78 |
| No. of deteriorated
patients | 21 |
| Gender
(male:female) | 45:33 |
| Age (years) | 37–71 (57.8) |
| Follow-up period
(months) | 36–56 (40.0) |
| JOA scores of initial
follow-up | 13–16 (14.1) |
| JOA scores of final
follow-up | 10–16 (14.0) |
The 78 patients were divided into two groups
according to the results of conservative treatment. The 21 patients
who had gradual reductions in JOA scores to a mean of 2.9 points
(range, 2–5 points) and underwent surgery were group A, while the
remaining 57 patients who were treated conservatively throughout
were group B. Among the 21 patients in group A, 18 patients
underwent anterior decompression and fusion and three underwent
laminoplasty. There were no incidences of infections, cervical
fluid leakage, esophageal or tracheal ruptures and neurological
deterioration. Transient recurrent laryngeal nerve palsy was
observed in one patient without further management. Three patients
reported axial pain, which subsided gradually in 1–2 months without
any treatment.
The prognostic factors correlating with the outcome
of conservative treatment are displayed in Table III. The mean diameter of the CSF
column in group A was significantly smaller than that in group B
(10.7±1.8 vs. 12.1±1.2 mm, P=0.02). Additionally, nine of 21
(42.9%) patients exhibited segmental instability in group A
compared with only eight of 57 (14.0%) patients in group B. This
difference was statistically significant (P=0.01). No significant
differences were identified between the two groups with regard to
age, gender, duration of disease, C2–C7 angle, signal intensity
changes on MRI, the number of compression-affected levels and the
degree of spinal cord compression.
 | Table IIIRisk factors of neurological
deterioration. |
Table III
Risk factors of neurological
deterioration.
| Factor | Group A (n=21) | Group B (n=57) | P-value |
|---|
| Age (years) | 58.8±11.3 | 57.5±10.5 | 0.62 |
| Gender
(male:female) | 13:8 | 32:25 | 0.80 |
| Duration of disease
(months) | 23.3±19.2 | 19.3±15.0 | 0.70 |
| C2–C7 angle
(degrees) | 9.9±10.7 | 11.6±10.7 | 0.61 |
| Segmental instability
(yes:no) | 9:12 | 8:49 | 0.01 |
| Spinal cord intensity
changes (yes:no) | 14:7 | 26:31 | 0.13 |
| Compression-affected
levels (no.) | 1.4 | 1.3 | 0.53 |
| Diameter of the CSF
column (mm) | 10.7±1.8 | 12.1±1.2 | 0.02 |
| Spinal cord
compression (%) | 78.2±6.3 | 75.3±8.1 | 0.19 |
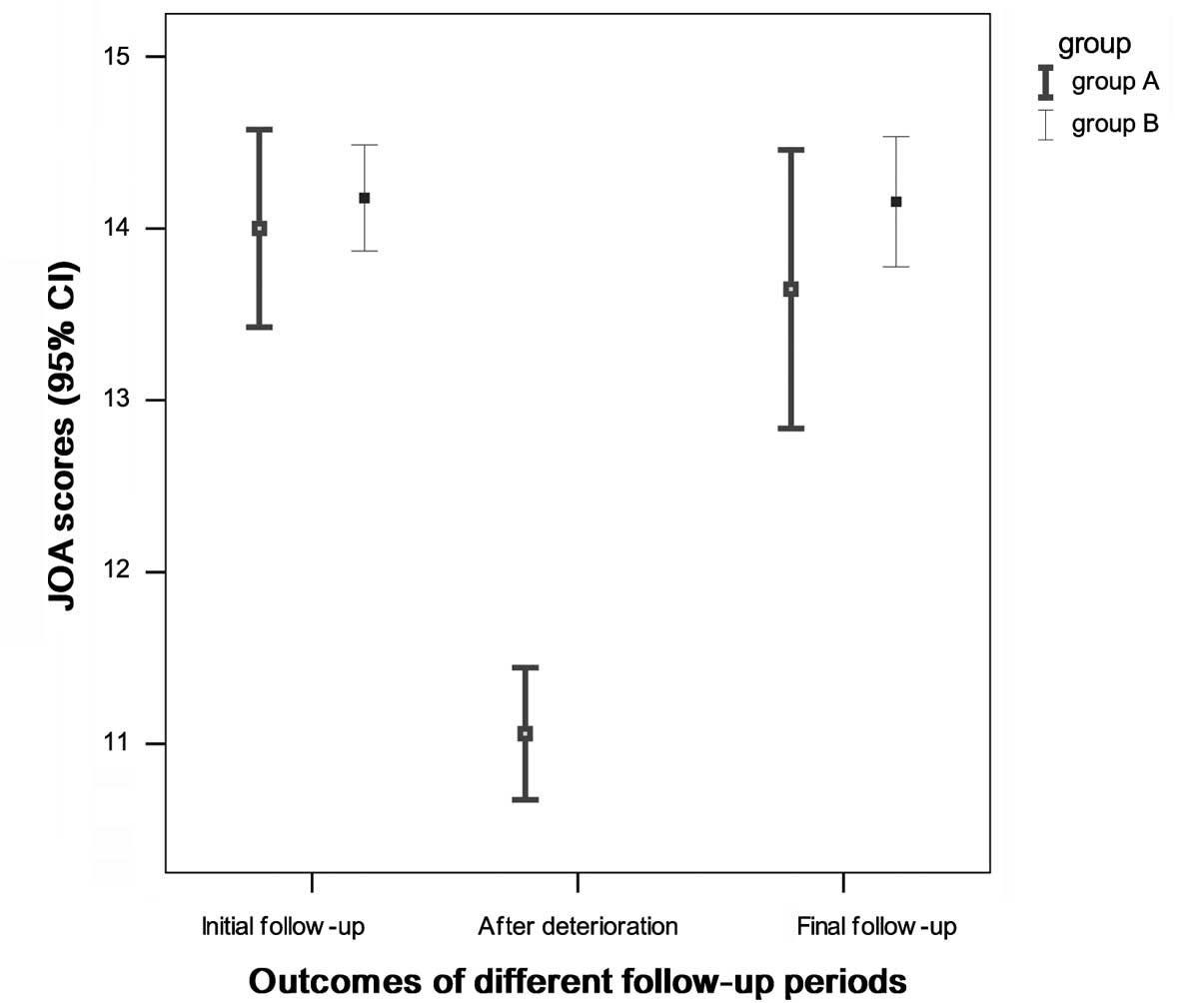
Fig. 3 shows the
mean JOA scores at different follow-up periods. On the first visit
to the hospital, the mean JOA scores were 14.0±1.1 in group A and
14.2±1.0 in group B, and no significant difference was identified
between the two groups (P=0.62). Although the mean JOA score of
group A decreased to 11.1±0.8 as the condition deteriorated,
following timely surgical intervention, the final mean JOA scores
of the two groups (13.4±2.5 in group A and 14.2±1.3 in group B,
P=0.46) were not observed to be significantly different.
Discussion
The present study revealed a satisfactory outcome of
conservative treatment in MCSM patients; only 21 of 78 (26.9%)
patients experienced a deterioration of myelopathy during a
>3-year follow-up. This demonstrated that in the majority of the
MCSM patients, neurological function either improved or was
non-progressive. This finding is consistent with a number of
previous reports. Oshima et al(7) conducted a retrospective study with a
mean follow-up period of 78 months to investigate the natural
course of MCSM; 16 of 43 (37.2%) patients exhibited a deterioration
in motor function and underwent decompression surgery. Following
Kaplan-Meier survival analysis, it was revealed that 82 or 56% of
patients in the study did not require surgery five or 10 years
after initial treatment, respectively. Sumi et al(8) performed a prospective cohort study
that only focused on MCSM and had a 5–12-year follow-up period, in
which deterioration in myelopathy was observed in 14 of 55 (25.5%)
patients, whereas 41 of 55 (74.5%) patients maintained mild
myelopathy without deterioration through the follow-up period.
The selection of patients who will truly benefit
from conservative treatment is challenging to surgeons. It is
therefore critical to investigate which prognostic factors
aggravate MCSM. A number of predicting factors that may affect the
surgical outcomes of CSM have been reported, including age
(1,19), duration of disease (1), cervical curvature (20), signal intensity changes in MRI
(3,21) and extent of spinal cord compression
(22). Despite this, studies
reporting the prognostic factors of conservative treatment for MCSM
are limited, and the conclusions controversial. Shimomura et
al(14) reported that
circumferential spinal cord compression in the maximum compression
segment in axial MRI was the only prognostic factor for MCSM.
Subsequently, Sumi et al(8)
further followed the same patients for >5 years and reported
that the presence of angular-edged deformities of the spinal cord
in T1-weighted axial MRI is another risk factor that aggravates
myelopathy. Yoshimatsu et al(15) analyzed the results of conservative
treatment for CSM in 69 cases and concluded that the disease
duration correlated significantly with the clinical outcome.
However, Oshima et al(7)
indicated that a large range of motion (ROM) and segmental
instability at the narrowest canal are considered to be adverse
prognostic factors.
Among several parameters considered in the present
study, the diameter of the CSF column and the existence of
segmental instability were identified to be statistically
significant. Narrowing of the spinal canal has been demonstrated to
be a major risk factor for CSM (23,24).
We hypothesized that the presence of cervical spinal stenosis may
expose individuals to a greater risk of deterioration of MCSM.
Historically, the evaluation of cervical spinal stenosis has been
based on the Pavlov ratio in plain lateral radiographs (25). However, the Pavlov ratio may not
reflect the impact of soft tissue on MCSM, including hypertrophy of
the ligamentum flavum. We consider the diameter of the CSF column
on MRI to more accurately reflect the space in the cervical canal.
Furthermore, the presence of segmental instability is another risk
factor, which indicates that the exacerbation of MCSM is affected
not only by static compression, but also by dynamic factors that
inflict repeated minor traumas on the spinal cord.
Although efforts have been made to identify
prognostic factors, it is difficult to predict whether a given
factor will be responsible for deterioration in a particular
instance. Consequently, it remains to be determined whether
patients with MCSM and adverse prognostic factors should be
surgically treated as soon as possible to avoid potential
deterioration, even if their symptoms and signs are moderate.
Furthermore, if non-surgical therapy is adopted, there may be a
risk of prolonged conservative treatment resulting in a lost
opportunity to obtain satisfactory outcomes after surgery. In an
attempt to clarify these points, patients in group A were further
followed up postoperatively for ≥1 year. A poor outcome would
indicate that patients with adverse prognostic factors require
referral to surgery prior to deterioration. By contrast, the
absence of a poor outcome would indicate that surgery may be
postponed. The results demonstrated that surgical outcomes were
relatively good, suggesting it was not too late to perform surgery
following the failure of conservative treatments. Thus, although
they have a tendency to undergo deterioration, MCSM patients
presenting with segmental instability or cervical spinal stenosis
may initially be treated conservatively with a close follow-up.
Surgical procedures may subsequently be selected when deterioration
of myelopathy is clearly identified. However, surgery should be
performed in a timely manner since CSM may progress rapidly and a
long period of moderate or severe CSM may result in poor prognosis
(1–3).
In summary, in this study, it was observed that MCSM
patients treated conservatively showed a relatively benign clinical
course. Segmental instability and cervical spinal stenosis were
factors correlating with a poor prognosis. For patients with
adverse prognostic factors, conservative treatment remains the
recommendation for the first choice action. If conservative
treatment fails, timely surgical intervention is likely to be
successful.
However, this study had several limitations.
Firstly, the JOA score system was the only criteria used to select
MCSM patients and assess clinical outcomes. The scores were
acquired based on the perspective of an investigator and thus were
vulnerable to subjectivity. Secondly, patients were followed up for
only three years; this relatively short follow-up time weakens the
ability of the study to assess the clinical course of MCSM.
Consequently, future studies involving reliable, validated
assessment tools and long-term follow-up periods are required to
further confirm the present findings.
Acknowledgements
The authors would like to thank Shuaishuai Wu for
collecting the radiographs.
References
|
1
|
Holly LT, Matz PG, Anderson PA, et al:
Clinical prognostic indicators of surgical outcome in cervical
spondylotic myelopathy. J Neurosurg Spine. 11:112–118. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Koyanagi T, Hirabayashi K, Satomi K,
Toyama Y and Fujimura Y: Predictability of operative results of
cervical compression myelopathy based on preoperative computed
tomographic myelography. Spine (Phila Pa 1976). 18:1958–1963. 1993.
View Article : Google Scholar
|
|
3
|
Zhang P, Shen Y, Zhang YZ, Ding WY and
Wang LF: Significance of increased signal intensity on MRI in
prognosis after surgical intervention for cervical spondylotic
myelopathy. J Clin Neurosci. 18:1080–1083. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Acharya S, Srivastava A, Virmani S and
Tandon R: Resolution of physical signs and recovery in severe
cervical spondylotic myelopathy after cervical laminoplasty. Spine
(Phila Pa 1976). 35:E1083–E1087. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cheung WY, Arvinte D, Wong YW, Luk KD and
Cheung KM: Neurological recovery after surgical decompression in
patients with cervical spondylotic myelopathy - a prospective
study. Int Orthop. 32:273–278. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gok B, Sciubba DM, McLoughlin GS, et al:
Surgical treatment of cervical spondylotic myelopathy with anterior
compression: a review of 67 cases. J Neurosurg Spine. 9:152–157.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Oshima Y, Seichi A, Takeshita K, et al:
Natural course and prognostic factors in patients with mild
cervical spondylotic myelopathy with increased signal intensity on
T2-weighted magnetic resonance imaging. Spine (Phila Pa 1976).
37:1909–1913. 2012. View Article : Google Scholar
|
|
8
|
Sumi M, Miyamoto H, Suzuki T, Kaneyama S,
Kanatani T and Uno K: Prospective cohort study of mild cervical
spondylotic myelopathy without surgical treatment. J Neurosurg
Spine. 16:8–14. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fouyas IP, Statham PF and Sandercock PA:
Cochrane review on the role of surgery in cervical spondylotic
radiculomyelopathy. Spine (Phila Pa 1976). 27:736–747. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kadaňka Z, Bednařík J, Novotný O, Urbánek
I and Dušek L: Cervical spondylotic myelopathy: conservative versus
surgical treatment after 10 years. Eur Spine J. 20:1533–1538.
2011.PubMed/NCBI
|
|
11
|
Kadanka Z, Mares M, Bednaník J, et al:
Approaches to spondylotic cervical myelopathy: conservative versus
surgical results in a 3-year follow-up study. Spine (Phila Pa
1976). 27:2205–2211. 2002.PubMed/NCBI
|
|
12
|
Angevine PD, Zivin JG and McCormick PC:
Cost-effectiveness of single-level anterior cervical discectomy and
fusion for cervical spondylosis. Spine (Phila Pa 1976).
30:1989–1997. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fountas KN, Kapsalaki EZ, Nikolakakos LG,
et al: Anterior cervical discectomy and fusion associated
complications. Spine (Phila Pa 1976). 32:2310–2317. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Shimomura T, Sumi M, Nishida K, et al:
Prognostic factors for deterioration of patients with cervical
spondylotic myelopathy after nonsurgical treatment. Spine (Phila Pa
1976). 32:2474–2479. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yoshimatsu H, Nagata K, Goto H, et al:
Conservative treatment for cervical spondylotic myelopathy.
prediction of treatment effects by multivariate analysis. Spine J.
1:269–273. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kadanka Z, Mares M, Bednarík J, et al:
Predictive factors for mild forms of spondylotic cervical
myelopathy treated conservatively or surgically. Eur J Neurol.
12:16–24. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Borden JN: Good Samaritan cervical
traction. Clin Orthop Relat Res. 113:162–163. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kawasaki M, Tani T, Ushida T and Ishida K:
Anterolisthesis and retrolisthesis of the cervical spine in
cervical spondylotic myelopathy in the elderly. J Orthop Sci.
12:207–213. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yamazaki T, Yanaka K, Sato H, Uemura K,
Tsukada A and Nose T: Cervical spondylotic myelopathy: surgical
results and factors affecting outcome with special reference to age
differences. Neurosurgery. 52:122–126. 2003.PubMed/NCBI
|
|
20
|
Naderi S, Ozgen S, Pamir MN, Ozek MM and
Erzen C: Cervical spondylotic myelopathy: surgical results and
factors affecting prognosis. Neurosurgery. 43:43–50. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Suri A, Chabbra RP, Mehta VS, Gaikwad S
and Pandey RM: Effect of intramedullary signal changes on the
surgical outcome of patients with cervical spondylotic myelopathy.
Spine J. 3:33–45. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Fujiwara K, Yonenobu K, Ebara S, Yamashita
K and Ono K: The prognosis of surgery for cervical compression
myelopathy. An analysis of the factors involved. J Bone Joint Surg
Br. 71:393–398. 1989.PubMed/NCBI
|
|
23
|
Murone I: The importance of the sagittal
diameters of the cervical spinal canal in relation to spondylosis
and myelopathy. J Bone Joint Surg Br. 56:30–36. 1974.PubMed/NCBI
|
|
24
|
Edwards WC and LaRocca H: The
developmental segmental sagittal diameter of the cervical spinal
canal in patients with cervical spondylosis. Spine (Phila Pa 1976).
8:20–27. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Pavlov H, Torg JS, Robie B and Jahre C:
Cervical spinal stenosis: determination with vertebral body ratio
method. Radiology. 164:771–775. 1987. View Article : Google Scholar : PubMed/NCBI
|