Introduction
For patients with carcinomas of the head, neck,
thorax or other parts of the body who have received radiotherapy,
lower absolute numbers of T and B lymphocytes compared with those
before radiotherapy and an imbalance in the absolute counts of T
lymphocyte subsets may be observed in the peripheral blood, which
may result in a decreased immune function and increased incidence
of radiation-induced esophagitis (1,2). The
duration of the impaired cellular and humoral immunity of patients
who have received radiotherapy may be between several months and
several years, and this phenomenon has also been further verified
in experiments with rats irradiated by 60Co γ-rays
(3). The duration of the impaired
immunity is likely due to the inhibitory effect of radioactive rays
on the immune system and may have a certain association with the
obstinate, intractable characteristics of radiation-induced
esophagitis.
A composition isolated from white peony root oral
liquid (cWPROL), whose major components are white peony (Paeonia
suffruticosa), Sophora tonkinensis and Bletilla
striata, is a prescription formulation independently developed
by our investigators and has a good efficacy for the treatment of
radiation-induced esophageal toxicity in previous experiments and
in clinic (4), however, its
functional mechanism remains unclear. This study analyzed the
variations of leukocytes and indicators of cellular and humoral
immunity in rats with radiation-induced esophagitis and following
various treatments. The results demonstrated that cWPROL may exert
its preventive and therapeutic effects on the disease by restoring
the immunity system that has been damaged by radioactive
radiation.
Materials and methods
Animals
A total of 128 adult Wistar rats weighing 180–220 g,
half male and half female, were provided by the Animal Department
of Hebei Medical University (Shijiazhuang, China). The animal care
and experimental protocols complied with the internationally
recognized guidelines on animal welfare, Regulations for the
administration of affairs concerning experimental animais of the
State Science and Technology Commission of the People’s Republic of
China and the guidelines for the Care and Use of Laboratory Animals
of Hebei Medical University. In addition, this study was approved
by the Medical Ethics Committee of The Fourth Hospital of Hebei
Medical University.
Medication
The cWPROL was processed according to the formula
and provided by the Pharmacy Department of the Fourth Hospital of
Hebei Medical University. The concentration of crude medicinal
components contained in the cWPROL was 2.88 g/ml and its relative
density was 1.18. The major components of cWPROL are white peony
root, Sophora tonkinensis and Bletilla striata. Its
production process was as follows: first, the Sophora tonkinensis
(100 g) and Paeonia suffruticosa root (300 g) are soaked for
2 hours, the solution was boiled for 1 hour and the liquid was
removed. The solids were boiled again with new water for 40 min,
the solutions of both steps were mixed, filtered through a signle
layer of gauze and concentrated to a relative density of 1.07
(between 70–80°C). The solution was refrigerated (2°C) for 48
hours, and filtered again. Second, Bletilla striata (150 g)
was soaked for 1 hour, boiled for 45 min, liquids removed, boiled
with new water for 30 min and the liquids were mixed. The liquids
were filtered with a single layer of gauze and mixed with the
filtered liquids of the first step. The solution was concentrated
to a relative density of 1.18 (between 70–80°C), refrigerated (2°C)
for 12 hours, purified water was added to a final volume of 1,000
ml and the solution was homogenized. The liquids were filtered
through a single layer of gauze, sealed in polypropylene plastic
bottles and sterilized in an autoclave sterilizer (Chenfeng medical
apparatus and instruments manufacturing Corp. Ltd, Jixi,
Heilongjiang, China; 105°C, 0.25 MPa) for 30 min to obtain the
final cWPROL. The western medicines used were lidocaine
hydrochloride injection (2%; Fuda Pharmaceutical Corp. Ltd.,
Shanghai, China), dexamethasone sodium phosphate injection (5 mg;
Taikang Pharmaceutical Corp. Ltd, Hangzhou, Zhejiang, China),
gentamicin sulfate injection (40,000 U/ml; Tiancheng Pharmaceutical
Corp. Ltd, Cangzhou, Hebei, China) and normal saline (250 ml;
Tiancheng Pharmaceutical Corp. Ltd.). All injections were
administered orally.
Immunology
Fluorescein isothiocyanate (FITC)-labeled mouse
anti-rat CD3 monoclonal antibodies (clonal code: 1F4) and mouse
anti-rat FITC-labeled CD4 and RPE-labeled CD8 double-labeled
monoclonal antibodies (CD4 clonal code: W3/25, CD8 clonal code:
OX8) were provided by AbD Serotec (Raleigh, NC, USA). Serum
immunoglobulin IgG and complement C3 kits were purchased from Sun
Biotechnology Company (Shanghai, China).
Animal models of radiation-induced
esophagitis
The rats were placed into a specific fixator made of
organic glass and, while conscious, the chest was exposed to a
single irradiation with a total dose of 43 Gy. In addition, the
irradiation field was 3x30 cm, the center dose point on the back of
rats was 1 cm under the body surface and the irradiation range was
3 cm above the esophagus, while the rest of the rat was covered.
60Co therapy apparatus (SFCC-8000C type, SSD=80 cm, dose
rate: 111 cGy/min, Shandong Xinhua Medical Instrument Co., Ltd.,
Shandong, China) was used for irradiation. On the 7th and 14th day
after irradiation, the pathological changes of radiation-induced
esophagitis were observed in the animal models.
Grouping of experimental animals and
administration method
A total of 128 Wistar rats were randomly divided
into eight groups with 16 rats in each group, half male and half
female. Group 1 (the normal group) was the blank control without
any radiation or treatment. Group 2 (single radiation group 1) was
sacrificed for evaluation on the 7th day after being irradiated
with 43 Gy 60Co γ-rays. Group 3 (single irradiated group
2) was sacrificed for evaluation on the 14th day after being
irradiated. Group 4 (prevention group 1) was treated with cWPROL at
a normal dose of 0.475 g/ml, 2 ml 3 times a day and at an interval
of 6 h from the 1st to 14th day after radiation for the prevention
of radiation-induced esophagitis. Group 5 (prevention group 2) was
treated with cWPROL at a high dose of 1.425 g/ml, 2 ml 3 times a
day and at an interval of 6 h from the 1st to 14th day after
radiation. Group 6 (treatment group 1) was treated with cWPROL at a
normal dose of 0.475 g/ml, 2 ml 3 times a day and at an interval of
6 h from the 7th to 14th day after radiation for treatment of
radiation-induced esophagitis. Group 7 (treatment group 2) was
treated with cWPROL at a high dose of 1.425 g/ml, 2 ml 3 times a
day and at an interval of 6 h from the 7th to 14th day after
radiation. Group 8 (treatment group 3) was treated with a
formulation of western medicines at a dose of 2 ml 3 times a day
with an interval of 6 h from the 7th to 14th day after radiation.
The rats in Groups 4, 5, 6, 7 and 8 were sacrificed for evaluation
on the 14th day after being irradiated. The normal dose of cWPROL
for the rats was converted from the human dose regulated according
to the dosage standard of pharmacology (5,6). The
formulation of the western medicine oral liquids was normal saline
250 ml, 2% lidocaine 20 ml, dexamethasone 10 mg and gentamicin
sulfate 320,000 units. The concentration of oral western medicine
for the rats was 0.16 times the human dose.
Collection of blood samples
At each experimental time point, the experimental
rats were anesthetized with 2% pentobarbital sodium via
intraperitoneal injection (45 mg/kg), blood was harvested from the
orbital sinus into EDTA-K2 anticoagulative tubes and
mixed quickly for the analysis of T-lymphocyte subsets. An
additional 3 ml of blood was collected from the femoral vein,
centrifuged at a speed of 2,000 × g for 10min by Labofuge 400R
centrifuge (Saimo Biotechonology development Corp. Ltd., Shanghai,
China) and then the supernatant was collected and maintained at
−80°C for evaluation of IgG and complement C3 in the serum.
Immunofluorescence staining and flow
cytometry
EDTA-K2 anticoagulative rat blood (100
μl) was placed into the bottom of two tubes. FITC-labeled
mouse anti-rat CD3 (10 μl) and 10 μl mouse anti-rat
FITC-labeled CD4 and RPE-labeled CD8 double-labeled monoclonal
antibodies was added to separate tubes. The components in the tubes
were mixed, stained in the warm incubator in the dark for 30 min
and then detected by flow cytometry (Epics XLII; Beckman Coulter,
Miami, FL, USA). The automatic calibration program of the flow
cytometry was run to refine its sensitivity, threshold, compensate
fluorescence and photoelectric multiple voltage. Prior to testing,
fluorescent microspheres of Flow-Check™ Fluorospheres (10
μl) were employed as standard samples to regulate the
coefficient of variability (CV) value of the instrument and control
it within 2%. Following calibration, the percentages and absolute
numbers of T lymphocyte subsets were analyzed by detecting
immunofluorescence data with Expo 32 ADC software, and the
percentages and absolute values of T lymphocytes (CD3+),
Th cells (helper T lymphocytes,
CD3+CD4+CD8−) and Tc cells
(cytotoxic T lymphocytes,
CD3+CD4−CD8+) and the Th/Tc ratio
were determined.
Immune nephelometry
Immune nephelometry was applied as previously
described (7) to evaluate the
levels of IgG and complement C3.
Statistical analysis
The data were analyzed using the SPSS 13.0 software
package (SPSS, Inc., Chicago, IL, USA). The comparisons between the
different groups were made by one-way ANOVA. The
Student-Newman-Keuls test was adopted when the variance was equal
and the Kruskal-Wallis one-way analysis of variance H test was
employed when the variance was unequal. The results were presented
as mean ± standard deviation. P<0.05 was considered to indicate
a statistically significant result.
Results
Evaluation of the white blood cells in
the peripheral blood of the rats
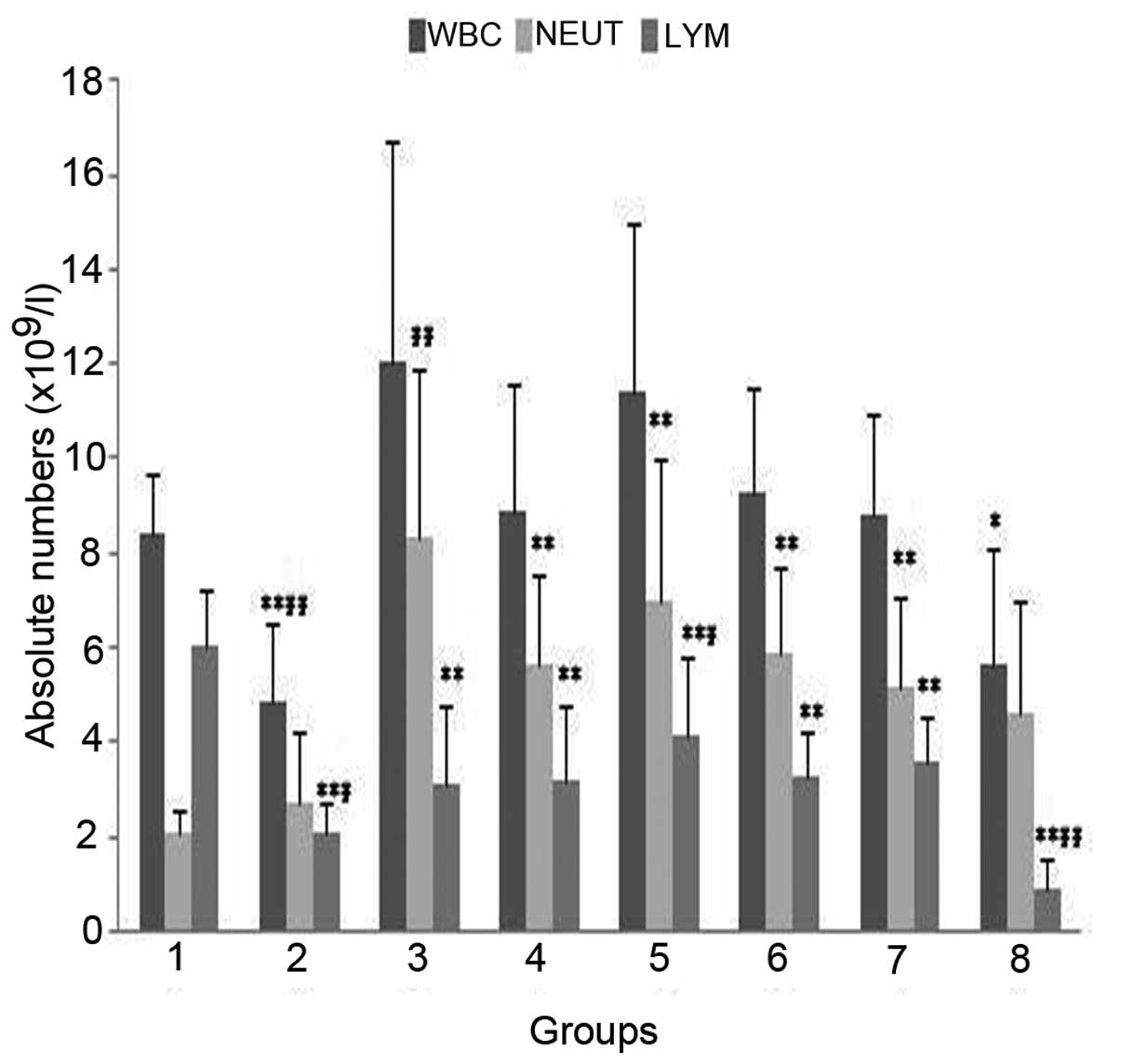
The total number of white blood cells in the
peripheral blood of the irradiated rats was significantly decreased
compared with that of the normal group (Group 1), on the 7th day
after irradiation (Group 2; P<0.001), but was not markedly
different on the 14th day after radiation (Group 3; P>0.05;
Fig. 1). The total numbers of
white blood cells in the peripheral blood were within the normal
range in the prevention and cWPROL treatment groups (Groups 4, 5, 6
and 7; P>0.05), but significantly lower than normal in the
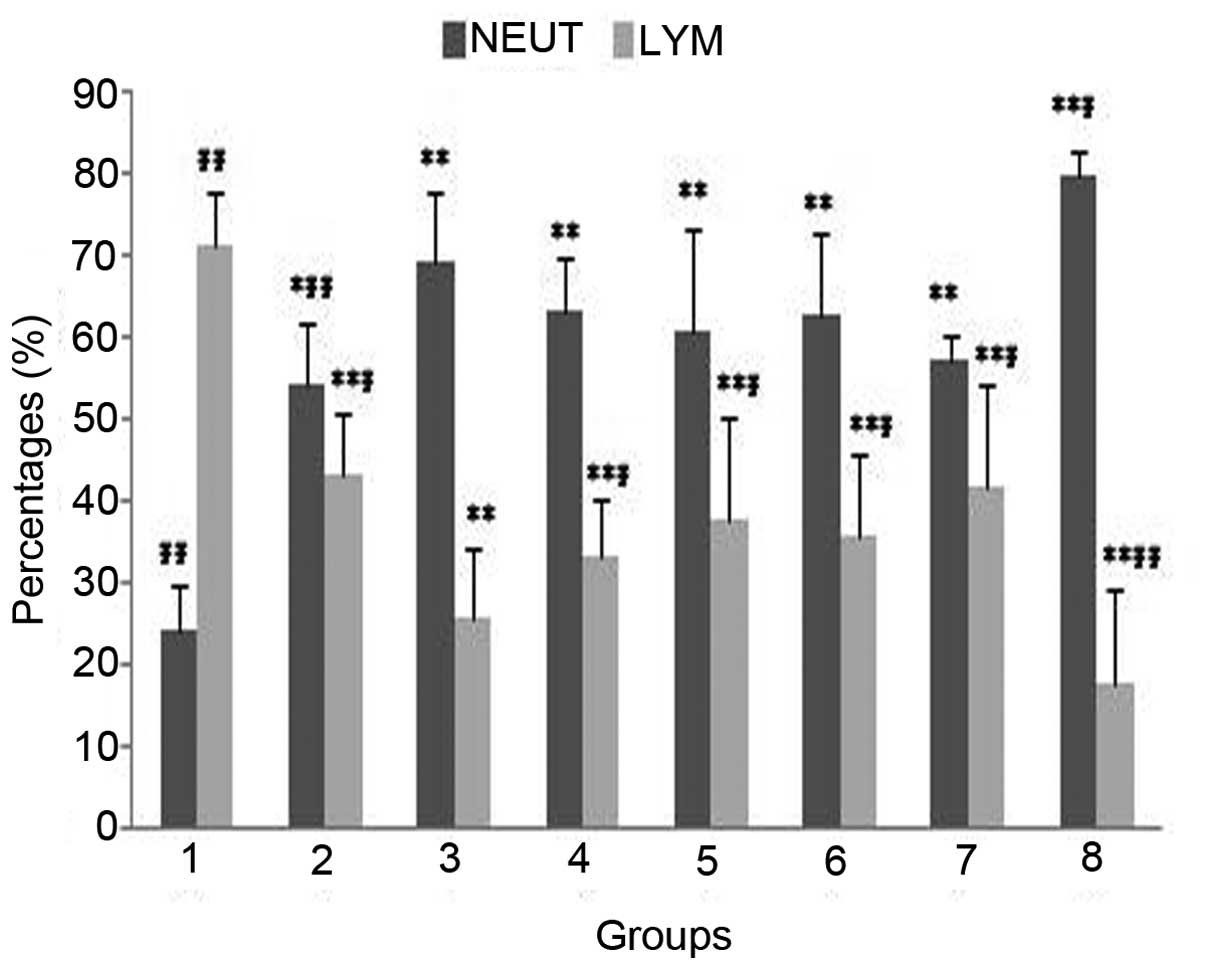
western medicine treatment group (Group 8; P<0.05; Fig. 1). The percentage of neutrophile
granulocytes (NEUT) on the 7th day after irradiation (Group 2) was
significantly elevated compared with that in the normal group
(Group 1; P<0.05), furthermore, it was much higher on the 14th
day after radiation (Group 3) than that in Group 2 (P<0.01;
Fig. 2).
The absolute numbers and percentages of lymphocytes
(LYM) in the peripheral blood of the irradiated rats (Groups 2, 3,
4, 5, 6, 7 and 8) were significantly lower than those in Group 1
(P<0.01; Figs. 1 and 2) and the percentage of LYM reached the
minimum on the 14th day after radiation (Fig. 2). Compared with single radiation
group 2 (Group 3), the percentage of NEUT in the western medicine
treatment group (Group 8) was significantly increased (P<0.05)
while the percentage and absolute number of LYM were significantly
decreased in Group 8 (P<0.01; Figs.
1 and 2). In addition, the
percentages of LYM in the groups treated with cWPROL (Groups 4, 5,
6 and 7) and the absolute number of LYM in the prevention group
treated with a high dose of cWPROL (Group 5) were both higher
compared with those of single radiation group 2 (Group 3;
P<0.05; Figs. 1 and 2).
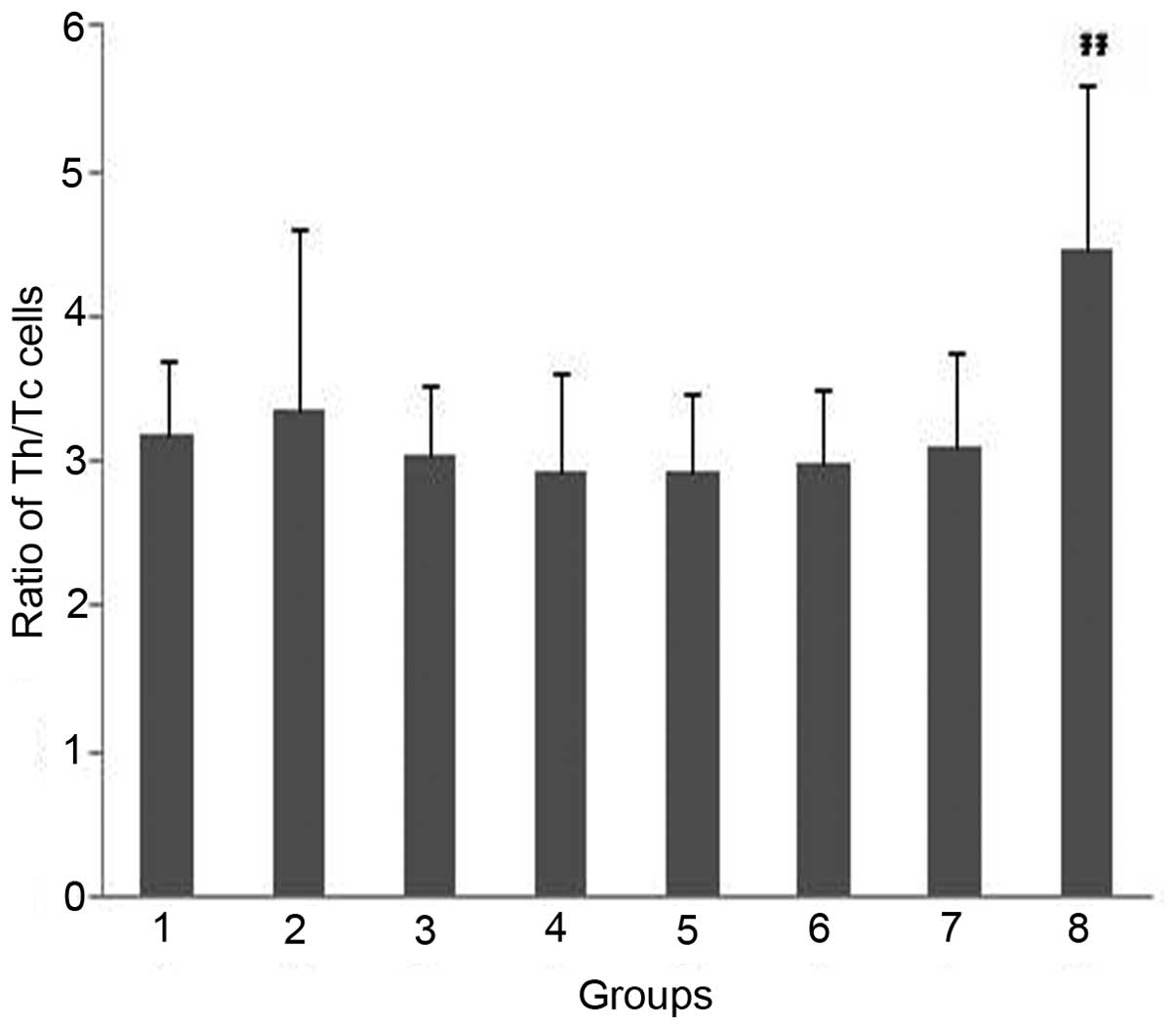
Impacts on the quantity of T-lymphocyte
subsets in each group
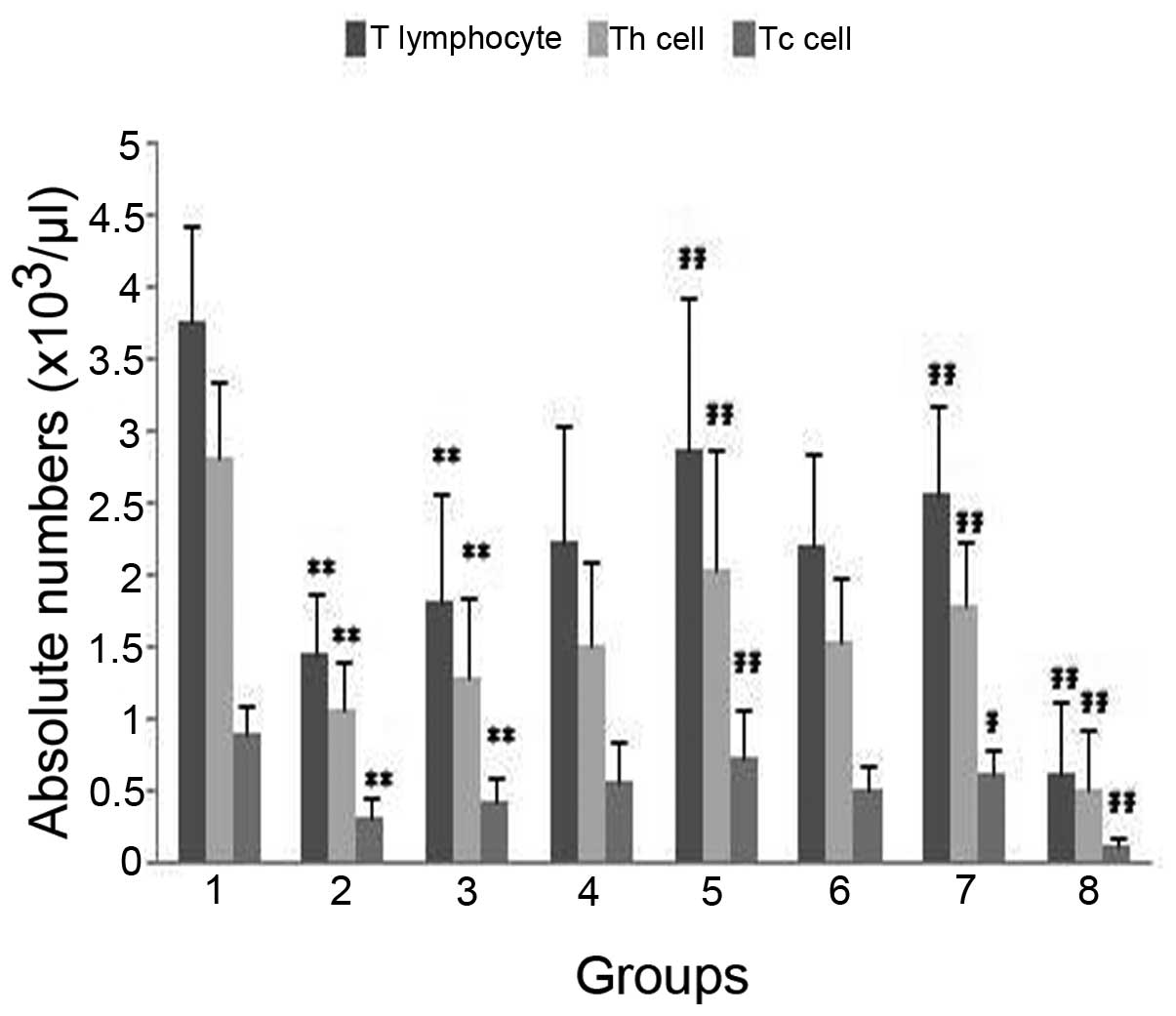
In the single radiation groups (Groups 2 and 3), the
absolute numbers of T lymphocytes, Th cells and Tc cells were
markedly decreased on the 7th and 14th day after irradiation,
(P<0.01; Fig. 3). The
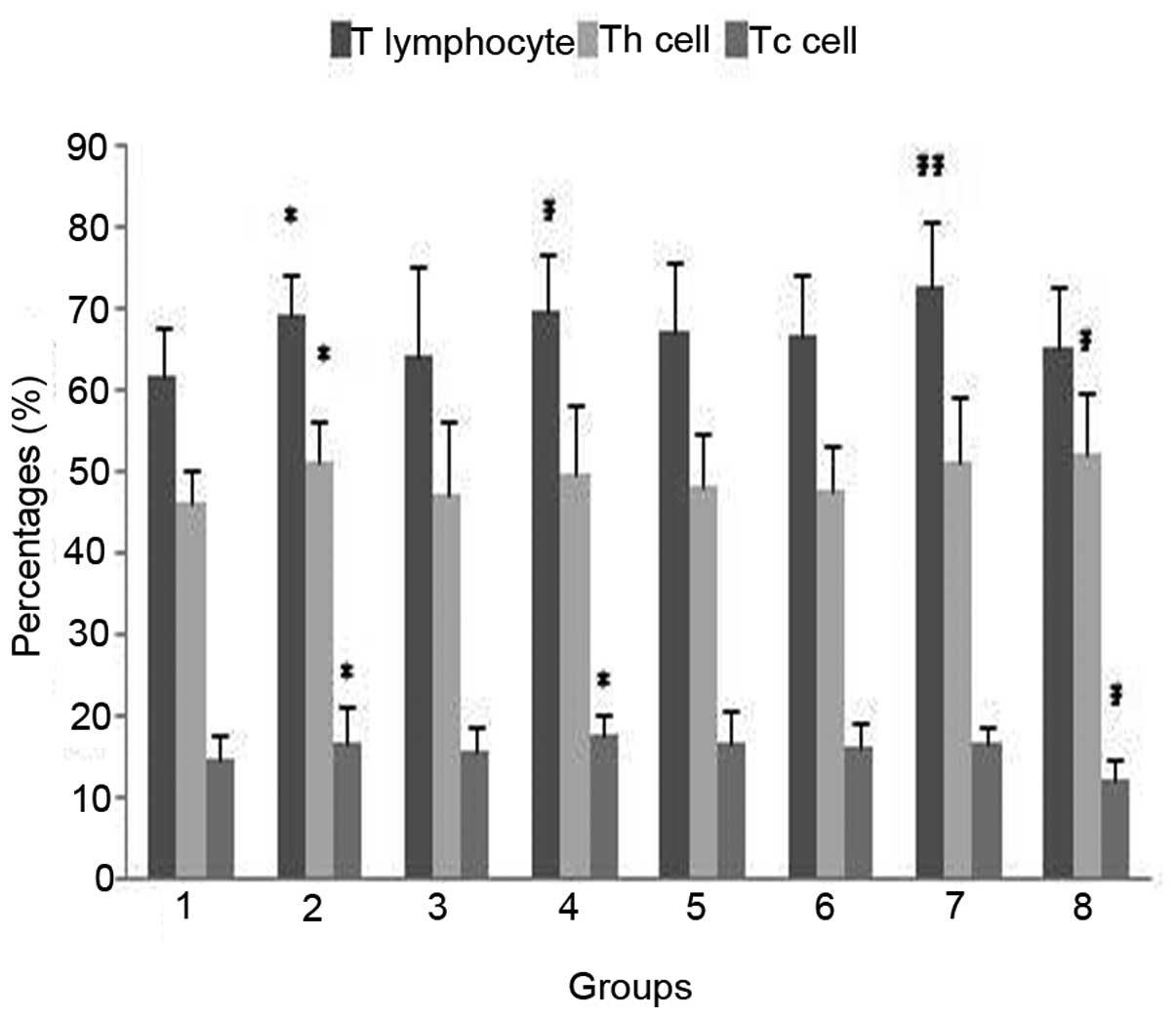
percentages of T lymphocytes, Th cells and Tc cells demonstrated a
transitory rise on the 7th day (Group 2; P<0.05) and then
returned to normal on the 14th day (Group 3; P>0.05) in
comparison with Group 1 Fig. 4).
There was no evident difference in the Th/Tc ratio between Groups
2, 3 and 1 (P>0.05; Fig.
5).
In the prevention group treated with a normal dose
of cWPROL (Group 4), the absolute numbers of T lymphocytes, Th
cells and Tc cells were not significantly different from those in
Group 3 (P>0.05; Fig. 3).
However, the percentage of T lymphocytes was higher than that in
Group 3 (P<0.05; Fig. 4). A
distinct elevation of the percentage of Tc cells was observed
compared with that in Group 1 (P<0.05; Fig. 4). In the prevention group treated
with a high dose of cWPROL (Group 5), the absolute numbers of T
lymphocytes, Th cells and Tc cells were all distinctly greater than
those of Group 3 (P<0.001; Fig.
3).
In the treatment group treated with a high dose of
cWPROL (Group 7), the quantity of T lymphocytes rose significantly
(P<0.01) after 8 days of treatment (14th day after radiation)
and the absolute numbers of Th cells and Tc cells were markedly
higher (P<0.05) compared with those in Group 3 (Fig. 3).
However, the absolute numbers of T lymphocytes, Th
cells and Tc cells in the western medicine treatment group (Group
8) were significantly lower than those in Group 3 (P<0.001;
Fig. 3), and the percentage of Th
cells was markedly higher (P<0.05; Fig. 4); thus the ratio of Th/Tc increased
significantly (P<0.01; Fig.
5).
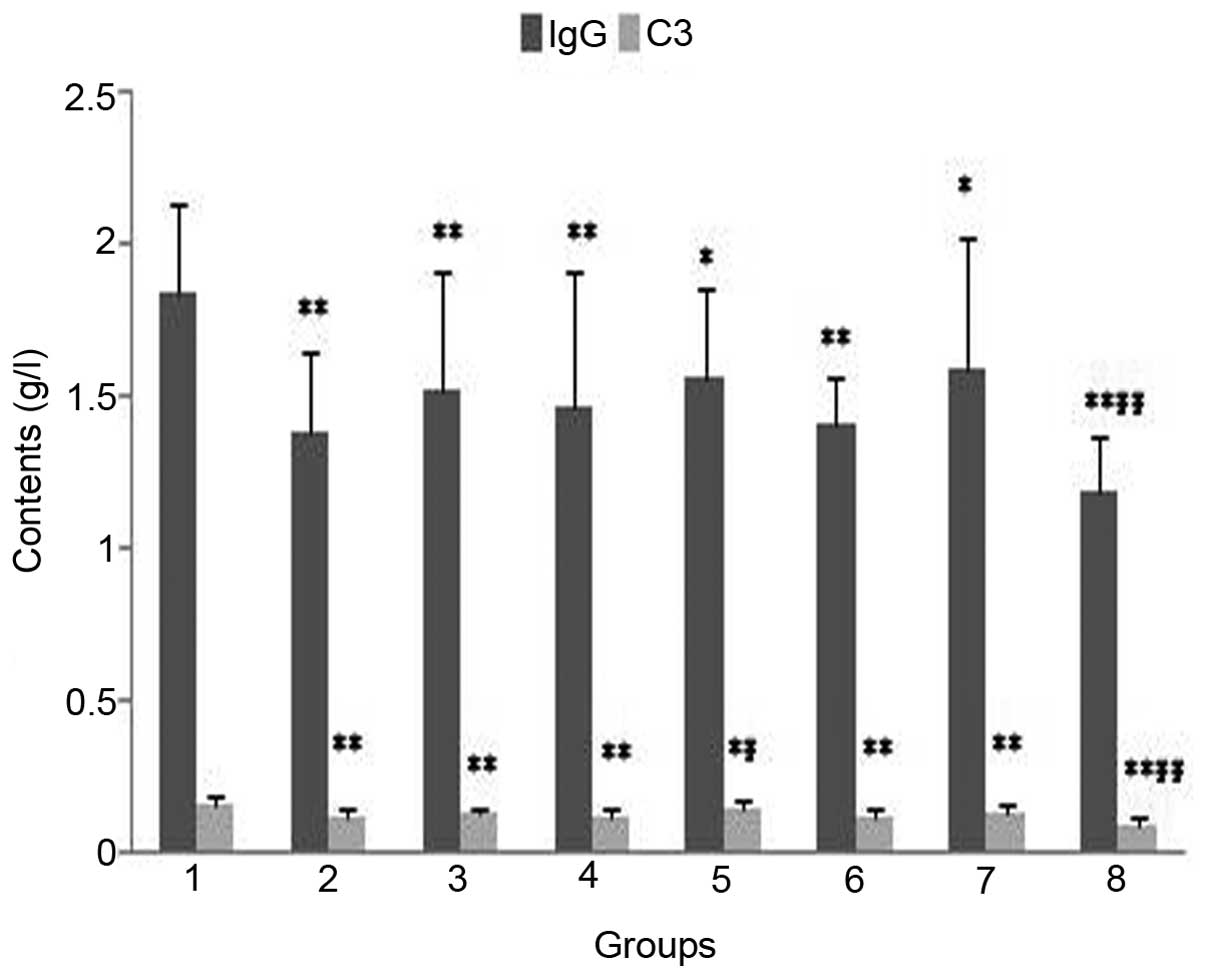
Analysis of the levels of IgG and
complement C3 in the serum of rats in each group
Compared with the levels in Group 1, the levels of
IgG and complement C3 in the serum were significantly decreased on
the 7th and 14th day after radiation (Groups 2 and 3; P<0.01;
Fig. 6). The level of IgG did not
recover in the prevention and treatment groups treated with cWPROL
(Groups 4, 5, 6 and 7; Fig. 6).
The level of complement C3 in the prevention group treated with a
high dose of cWPROL (Group 5) increased significantly (P<0.05)
compared with that in Group 3, however it did not return to the
normal level (Fig. 6).
Discussion
Deficiency of cellular immunity and disordered
humoral immunity have often been observed in patients with
malignant tumors (8). Although
radiotherapy is an effective method for preventing the growth of
tumors, it further inhibits immunological function (1). In the current study, the percentage
of lymphocytes in the peripheral blood of the Wistar rats was
reduced significantly on the 14th day following irradiation with 43
Gy 60Co γ-rays. Consistent with the study by Kajioka
et al (9), the absolute
numbers of T lymphocytes, Th cells and Tc cells of the
radiation-induced rats in the present study were significantly
lower than those in the normal rats (P<0.001). The main cause of
the phenomenon may be the downregulation of CD28 in T lymphocytes,
which may lead to a high level of Fas-mediated apoptosis and
therefore impair the immune system (10). T lymphocytes, particularly
CD4+ and CD8+ T lymphocytes, play a leading
role in the anti-tumor function in vivo; therefore, the
quantities of CD4+ and CD8+ T lymphocytes are
crucial for killing the cancer cell. T lymphocytes are easily
injured by radiation due to their sensitivity to irradiation. The
present study revealed that the immunological function of the rats
with radiation-induced esophagitis was significantly impaired.
Furthermore, the absolute numbers of T lymphocytes, Th cells and Tc
cells of the rats in the prevention group treated with the high
dose of cWPROL and in the cWPROL treatment groups were markedly
elevated compared with those in the single radiation group 2 (Group
3), and the percentage of T lymphocytes was clearly increased in
the prevention group treated with a normal dose of cWPROL. These
results indicate a dose-effect relationship of cWPROL in the
prevention and treatment of radiation-induced esophagitis.
Furthermore, the immune repairing effect of cWPROL may aid the
quick recovery of radiation-induced esophagitis and enhance the
resistance of the body to tumors.
Immune globulins are the key molecules in humoral
immunity, among which the majority are IgG, an important indicator
that reflects the level of immunity of the body (11). Complement C3 is one type of
globulin that has enzymatic activity and is able to kill tumor
cells independently in nonspecific immunity and assist antibodies
and immune cells to kill the cancer cells (12). Pathological changes such as
exuviation, inflammatory cell infiltration and reduced levels of
IgG and complement C3 occur in the radiation-induced rats, which
results in bacterial infection (13). The current study showed that the
levels of IgG and complement C3 significantly declined in
irradiated rats. The levels of IgG in the prevention and treatment
groups treated with cWPROL were not markedly different from that in
the single radiation group 2 (Group 3). The level of complement C3
in the prevention group with a high dose of cWPROL was clearly
recovered. These results suggest that cWPROL may weaken the
pathogenicity of conditioned pathogens on the esophagus by
strengthening the humoral immunity of the body.
Glucocorticoids, antibiotics and mucosal anesthetics
are common medicines used in clinic to treat radiation-induced
esophagitis and relieve pain by antibiosis, controlling secondary
infection of local mucosa, alleviating exudation and edema, or
paralyzing the sensory nerve endings in the esophageal mucosa. In
addition, the improvement rate of combined therapy with these
medicines is 72% (14). However,
the present study demonstrated that the total numbers of white
blood cells and lymphocytes, and the percentage of lymphocytes in
the peripheral blood of irradiated rats decreased in the group
treated with western medicine. Despite inhibiting the number and
function of immune cells and chemotaxis of inflammatory cells,
western medicine is able to control the inflammatory response and
thus promote tissue repair, but its long-term use may harm the
ability of the immune system to act against tumors. The rationality
of preventive application of antibiotics on patients who receive
radiotherapy remains to be discussed.
To summarize, cWPROL is extracted from a traditional
Chinese herbal formulation that contains various Chinese herbal
medicines and is highly effective in preventing and treating
radiation-induced esophagitis in clinic. In this study, we
discussed the likely functional mechanisms of cWPROL and revealed
that by elevating the total number and percentage of lymphocytes,
the absolute levels of T lymphocytes, Th cells and Tc cells, and
the level of complement C3, cWPROL may repair the impaired immune
system of rats with radiation-induced esophagitis, and thus
postpone or treat the disease. Therefore, cWPROL not only prevents
and treats complications of radiotherapy, but also enhances the
cellular and humoral immunity of the body, thus improving the
efficacy of anti-tumor activity.
Abbreviations:
|
cWPROL
|
composition isolated from white peony
root oral liquid
|
Acknowledgements
This study was supported by the
Foundation Science Research Program of the Hebei Province Science
and Technology Office (grant no. 04236101D-252004-2005). The
authors would like to thank The Pharmacy Department of The Fourth
Hospital of Hebei Medical University for processing cWPROL.
References
|
1.
|
Kuss I, Hathaway B, Ferris RL, Gooding W
and Whiteside TL: Imbalance in absolute counts of T lymphocyte
subsets in patients with head and neck cancer and its relation to
disease. Adv Otorhinolaryngol. 62:161–172. 2005.PubMed/NCBI
|
|
2.
|
Santin AD, Bellone S, Palmieri M, et al:
Effect of blood transfusion during radiotherapy on the immune
function of patients with cancer of the uterine cervix: role of
interleukin-10. Int J Radiat Oncol Biol Phys. 54:1345–1355. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Gridley DS, Pecaut MJ, Miller GM, Moyers
MF and Nelson GA: Dose and dose rate effects of whole-body
gamma-irradiation: II. Hematological variables and cytokines. In
Vivo. 15:209–216. 2001.PubMed/NCBI
|
|
4.
|
Shen L, Li X, Shan B, et al: Therapeutic
effect of compound of White Peony Root Oral Liquids on
radiation-induced esophageal toxicity via the expression of EGF and
TGF-β1. Biomedical Reports. 1:308–314. 2013.PubMed/NCBI
|
|
5.
|
Yao WH: Observation of the preventive and
therapeutic effect of modified Shashen Maidong Decoction on
radiation-induced esophagitis. Chinese Journal of Radiological
Medicine and Protection. 24:3762004.(In Chinese).
|
|
6.
|
Zhu AF, Yan XY, Ren JH, et al: Experience
in treatment of radiation-induced esophagitis with the integrated
Chinese Western therapy. Chinese Journal of Radiation Oncology.
12:582003.
|
|
7.
|
Levinson SS and Goldman J: Absorbance
nephelometry of immune complexes by reaction with anti-IgG after
treatment with polyethylene glycol. Clin Chem. 29:2035–2039.
1983.PubMed/NCBI
|
|
8.
|
Lissoni P, Brivio F, Ferrante R, et al:
Circulating immature and mature dendritic cells in relation to
lymphocyte subsets in patients with gastrointestinal tract cancer.
Int J Biol Markers. 15:22–25. 2000.PubMed/NCBI
|
|
9.
|
Kajioka EH, Gheorghe C, Andres ML, et al:
Effects of proton and gamma radiation on lymphocyte populations and
acute response to antigen. In Vivo. 13:525–533. 1999.PubMed/NCBI
|
|
10.
|
Ballow M: The IgG molecule as a biological
immune response modifier: mechanisms of action of intravenous
immune serum globulin in autoimmune and inflammatory disorders. J
Allergy Clin Immunol. 127:315–323. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Gelfand EW: Intravenous immune globulin in
autoimmune and inflammatory diseases. N Engl J Med.
368:7772013.PubMed/NCBI
|
|
12.
|
Saito T, Shimoda K, Kinoshita T, et al:
Prediction of operative mortality based on impairment of host
defense systems in patients with esophageal cancer. J Surg Oncol.
52:1–8. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Bar-Ad V, Ohri N and Werner-Wasik M:
Esophagitis, treatment-related toxicity in non-small cell lung
cancer. Rev Recent Clin Trials. 7:31–35. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Yang HH, Wang JH and Ding WJ: Analysis of
the function of antibiotics in the treatment of Grade 2
radiation-induced esophagitis. Zhejiang Journal of Clinical
Medicine. 8:2052006.(In Chinese).
|