Introduction
Peripherally inserted central catheter (PICC)
technology has been widely used to provide long-term intravascular
access in children and adults. With such frequent application in
clinical practice, an increasing number of catheter complications
have been observed. The incidence of malpositioned catheter is
5–31%, including malpositioned catheter, catheter slide or
extrusion, and catheter drift (1).
Malpositioned catheters result in discomfort and pain to the
patients, and also induce serious consequences, such as loss of
usage (2).
It has been shown that a central tip location for
the PICC is essential to minimize the risk of complications.
However, different catheter tip locations may generate different
symptoms in patients (3,4). If the tip is inserted into the heart,
precordial discomfort, arrhythmia, cardiac tamponade and heart
valve damage may occur in the patient; if the catheter remains in a
peripheral vein, it may induce swelling, pain, fluid in the limb of
the patient and discomfort and pain at the site where the catheter
tip attaches to the vessel wall. In addition, the placement of the
catheter tip in the jugular vein may result in discomfort,
difficulty in turning the head and neck soreness occurring in the
affected side (5). Therefore, the
establishment of a protocol to avoid the misplacement of the PICC
is very important in clinical practice. In the present study, we
monitored a total of 3,012 patients with cancer who underwent
insertion of a PICC and summarized the data from these
patients.
Materials and methods
Patients
From August 2000 to March 2012, a total of 3,012
cases underwent insertion of a PICC (1,590 adult males, 1,121 adult
females and 301 children; age range, 1∼94 years; median age: 52
years). All the patients received chemotherapy or nutritional
support.
PICC placement
Three types of 4F catheters were prepared for PICC
insertion, with the selection dependent on the patient: i)
3-position Groshong valve type catheter, 60 cm in length (C.R.
Bard, Inc., Murray Hill, NJ, USA); ii) catheter with a length of 55
cm (Arrow International, Inc., Reading, PA, USA); iii) catheter
with a length of 45 cm (B. Braun Melsungen AG, Melsungen, Germany).
The catheters were inserted through the basilic vein in 1,805
cases, through the median cubital vein in 791 cases and through the
cephalic vein in 416 cases.
All the catheters were placed by PICC nurses who had
undergone specialized training. Prior to the PICC insertion, the
catheter length was estimated by the professional carrying out the
insertion (6). The insertion of
the PICC was performed using aseptic techniques and procedures by
the bedside. A chest X-ray was obtained following the procedure.
PICC tips were defined as central if they resided anywhere within
the superior vena cava (SVC). All X-ray images were read by a
radiologist to determine the PICC tip locations.
Results
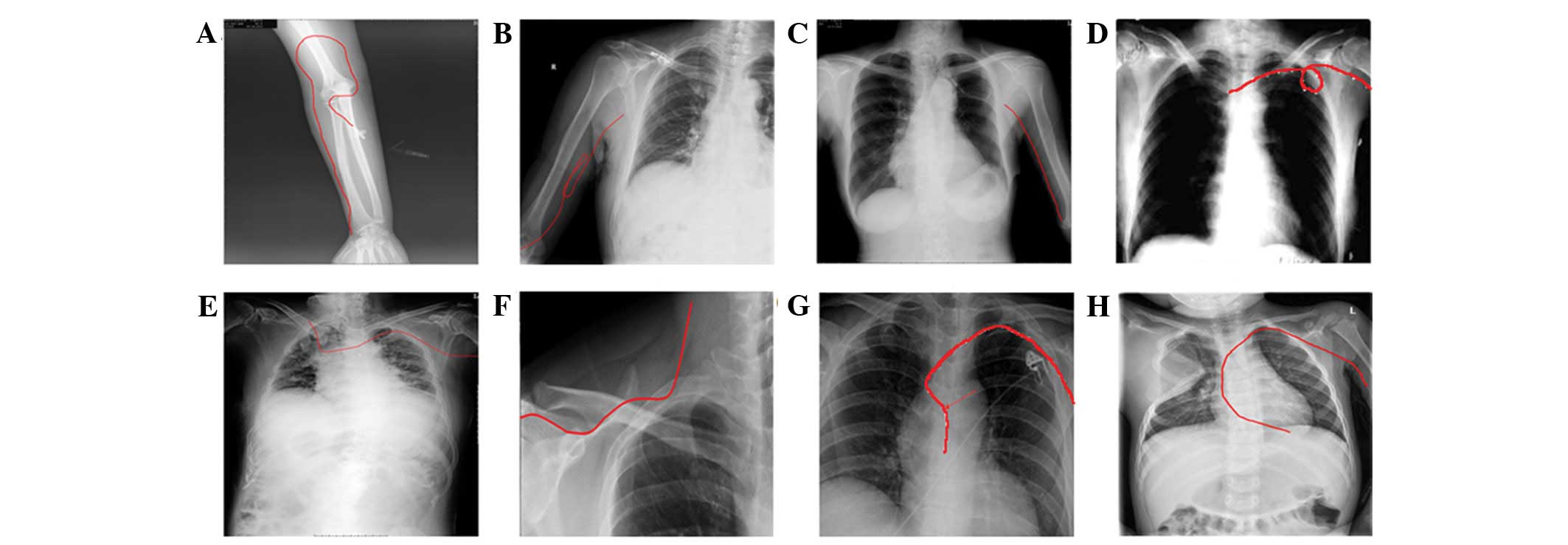
The rate of successful initial placement was 94.6%
(2848/3012). Catheter malposition occurred in 237 out of the 3,012
patients (7.87%). X-ray examination clearly showed the malposition
of PICC in forearm, basilic vein and armpit, which is indicated by
red lines in Fig. 1. The most
frequently occurring site of misplacement was the jugular vein
which occurred in 99 patients (99/327, 30.3%), followed by the
axillary vein (65/327, 19.9%) and brachial vein (25/327, 7.6%).
Catheter prolapse was another noteworthy complication following
PICC insertion (Table I).
 | Table I.Two hundred and thirty-seven cases of
malpositioned PICC. |
Table I.
Two hundred and thirty-seven cases of
malpositioned PICC.
| Location | During PICC
insertion | Following PICC
insertion |
|---|
| Right atrium | 2 | 1 |
| Right ventricle | 1 | 0 |
| Radial vein | 1 | 0 |
| Jugular vein | 77 | 22 |
| Brachial vein | 19 | 6 |
| Fold in basilic
vein | 3 | 0 |
| Fold from basilic
vein back into cephalic vein | 2 | 0 |
| Fold from cephalic
vein back into basilic vein | 1 | 0 |
| Fold in cephalic
vein | 1 | 0 |
| Catheter
prolapse | 0 | 19 |
| Axillary vein | 45 | 20 |
| Contralateral
subclavian vein | 7 | 5 |
| Azygos vein | 5 | 0 |
| Total | 164 | 73 |
Discussion
PICCs have been widely used in clinical practice for
several decades and have been shown to be a safe and convenient
means of administering chemical drugs and parenteral
hyperalimentation (7,8). When the catheter does not reach the
appropriate location within the vena cava, it is considered to be
misplaced. This complication is very common in clinical practice.
If the catheter is difficult to thread or to insert to the
premeasured depth, blood withdrawal is difficult, the catheter
flushes with resistance or removal of the stylet is difficult, this
is an indication that malpositioning may have occurred (9). An X-ray examination following PICC
insertion is necessary to identify whether the catheter is
misplaced.
It has been reported that the internal jugular vein
is the most common malpositioning site following catheter insertion
into the basilic vein, while the axillary and basilic veins are the
most common malpositioning sites following catheter insertion into
the cephalic vein. The insertion of catheters through the saphenous
or other leg veins may lead to entry into the ascending lumbar vein
(10,11), while catheter insertion into the
scalp may result in entry into the intracranial veins or tissue and
thoracic veins (12).
The clinical skill and experience of the healthcare
professional is important to ensure successful catheter placement.
Furthermore, a knowledge of venous anatomy, which may aid in the
selection of a suitable vein and a suitable catheter for insertion,
is essential. It is also important for the catheter to be inserted
slowly, to allow the blood returning to the heart to carry the
catheter to the vena cava. Rapid threading of the catheter may
increase the risk of malposition. In addition, the position of the
patient may impact the PICC insertion, with misplacement
potentially occurring if it is not possible to position the
patient’s jaw close to the shoulder.
Catheter care and maintenance is an important issue
requiring the efforts of nurses and patients. There is a
requirement for all nurses caring for patients with a PICC to be
knowledgeable about the effective management of the catheter, in
order to prolong the indwelling time of the catheter and to prevent
complications and injury to the patients. Using a team of
caregivers with trouble-shooting expertise and the ability to
change dressings and repair catheters has been observed to enhance
success with PICCs (13). To
ensure that the catheter is kept in good condition, it is of great
importance to educate the patients following the insertion of the
PICC. Even after a successful placement, inappropriate movements of
the patients and high intracranial pressure in patients with severe
nausea, vomiting, hiccups and constipation may result in the
malpositioning of the catheter tip. Certain additional factors may
also result in the malpositioning of the catheter, such as patient
stress and a cooler surrounding environment.
In conclusion, the most frequently occurring site of
catheter misplacement is the jugular vein, followed by the axillary
vein. Many factors may lead to the malposition of PICCs. The
appropriate placement of PICCs requires the combined efforts of
healthcare professionals and patients.
References
|
1.
|
Ryder MA: Peripherally inserted central
venous catheters. Nurs Clin North Am. 28:937–971. 1993.PubMed/NCBI
|
|
2.
|
Walshe LJ, Malak SF, Eagan J and Sepkowitz
KA: Complication rates among cancer patients with peripherally
inserted central catheters. J Clin Oncol. 20:3276–3281. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Yamamoto AJ, Solomon JA, Soulen MC, et al:
Sutureless securement device reduces complications of peripherally
inserted central venous catheters. J Vasc Interv Radiol. 13:77–81.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Kearns PJ, Coleman S and Wehner JH:
Complications of long arm-catheters: a randomized trial of central
vs peripheral tip location. JPEN J Parenter Enteral Nutr. 20:20–24.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
James L, Bledsoe L and Hadaway LC: A
retrospective look at tip location and complications of
peripherally inserted central catheter lines. J Intraven Nurs.
16:104–109. 1993.PubMed/NCBI
|
|
6.
|
Marcy PY: Central venous access:
techniques and indications in oncology. Eur Radiol. 18:2333–2344.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Tian G, Zhu Y, Qi L, Guo F and Xu H:
Efficacy of multifaceted interventions in reducing complications of
peripherally inserted central catheter in adult oncology patients.
Support Care Cancer. 18:1293–1298. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Cunningham RS and Ravikumar TS: A review
of peripherally inserted central venous catheters in oncology
patients. Surg Oncol Clin N Am. 4:429–441. 1995.PubMed/NCBI
|
|
9.
|
Aladangady N, Roy R and Costeloe KL: The
cobweb sign: percutaneous silastic long line tip placement in
tributaries of superficial veins. J Perinatol. 25:671–673. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Clarke P, Wadhawan R, Smyth J and Emmerson
AJ: Parenteral nutrition solution retrieved by lumbar puncture
following left saphenous vein catheterization. J Paediatr Child
Health. 39:386–389. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
De A and Imam A: Long line complication:
accidental cannulation of ascending lumbar vein. Arch Dis Child
Fetal Neonatal Ed. 90:F482005. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Andersen C, Hart J, Vemgal P and Harrison
C: Prospective evaluation of a multi-factorial prevention strategy
on the impact of nosocomial infection in very-low-birthweight
infants. J Hosp Infect. 61:162–167. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Golombek SG, Rohan AJ, Parvez B, Salice AL
and LaGamma EF: “Proactive” management of percutaneously inserted
central catheters results in decreased incidence of infection in
the ELBW population. J Perinatol. 22:209–213. 2002.
|