Introduction
Symptoms and signs of acute respiratory
insufficiency, including cough, expectoration and asthma, may occur
during thrombolytic therapy of left ventricular myocardial
infarction, and may cause respiratory failure. Therefore,
protecting the lungs from injury throughout thrombolytic therapy is
becoming a focus of particular interest in cardiovascular
research.
Erigeron breviscapus is a wild herbal plant
of Yunnan Province, China. The major effective component is a
flavone, breviscapine. Breviscapine activates blood circulation,
removes blood stasis, relieves pain and enforces microcirculation.
The pharmacological effects of breviscapine include the inhibition
of platelet and erythrocyte adhesion, reduction of blood viscosity
and dilation of blood vessels (1,2).
Breviscapine is commonly used in the clinic for treating coronary
heart disease. Previous studies (3,4) have
identified that breviscapine suppresses the production of
procalcitonin (PCT) and neutrophil elastase (NE), reduces the
systemic inflammatory response and protects the lungs of children
undergoing open heart surgery. Another study (5) showed that a breviscapine injection
had anti-injury effects on hypoxic-ischemic brain damage in
neonatal rats, possibly by reducing the expression of Bcl-2 and
Bax.
Since breviscapine may be used to treat coronary
heart disease and reduce the systemic inflammatory response, it is
possible that breviscapine may protect the lungs in left heart
ischemic reperfusion. There are no relevant reports of whether
breviscapine affects the expression of inflammatory factors in
acute lung injury induced by left heart ischemic reperfusion, or
concerning the underlying mechanism.
In the present study, an acute lung injury rat model
induced by left heart ischemic reperfusion was established and
treated with breviscapine. We investigated the effect of
breviscapine on the expression of interleukin 18 (IL-18) and
intercellular adhesion molecule-1 (ICAM-1) and provide a possible
mechanism of the protective role of breviscapine on respiratory
function. The results revealed that breviscapine decreased the
expression of IL-18 and ICAM-1, and reduced inflammatory injury in
the lungs. The present study provides a theoretical basis for the
clinical application of breviscapine to treat left ventricular
dysfunction in acute respiratory failure.
Materials and methods
Laboratory animals
Sixty healthy rats of mixed gender, weighing 250–350
g were obtained from the Experimental Animal Center of Zhengzhou
University (Zhengzhou, China) and were randomly divided into two
groups: the treatment group (TG; n=30) and the control group (CG;
n=30). The rats in the TG received breviscapine and the rats in the
CG received normal saline. The study was approved by Ethics
Committee of Xinxiang Medical University (Xinxiang, China). The
research was compliance with the principles enunciated in Helsinki
ethical principles declaration.
Main reagents and instruments
Breviscapine injections were purchased from
Heilongjiang Feixia Pharmaceutical Industry Co., Ltd. (Harbin,
China). The BL-420 biological signal collecting and processing
system (Chengdu TME Technology Co., Ltd., Chengdu, China) was
supplied by the Functional Laboratory of Xinxiang Medical
University. A blood gas analyzer was purchased from Shanghai Yuyan
Instruments Co., Ltd. (Shanghai, China). IL-18 and ICAM-1
polyclonal antibodies, and an SP kit were purchased from Beijing
Zhong Shan -Golden Bridge Biological Technology Co., Ltd. (Beijing,
China). A myeloperoxidase kit was supplied by Nanjing Jiancheng
Bioengineering Institute (Nanjing, China).
Methods
Surgery
Surgery was performed according to a previously
described method (6). Briefly, a
cannula was inserted into the left external jugular vein after the
rats had received general anesthesia with 4% chloral hydrate (1
ml/100 g body weight). Each rat underwent thoracotomy and left
anterior descending coronary artery ligation. Rats in the TG
received treatment with a breviscapine injection (10 mg/kg body
weight) through the external jugular vein cannula once the left
anterior descending coronary artery had been ligated for 10 min.
The rats in the CG received normal saline. The rats in the two
groups were ligated for 30 min and then reperfused.
In each rat, the diaphragm was exposed prior to
thoracic surgery and connected to the BL-420 biological signal
collecting and processing system through a needle electrode. Then,
respiratory curve data was obtained. Following the collection of 5
ml peripheral blood samples at 30 min after ligaturing (T1), 30 min
after reperfusion (T2) and 60 min after reperfusion (T3), and the
measurement of the arterial partial pressure of oxygen
(PaO2) using a blood gas analyzer, all rats were
sacrificed. The lungs were removed and bronchialalveolar lavage was
performed immediately. Then, 5 ml bronchialalveolar lavage fluid
(BALF) was collected. The lower lobe of the right lung was removed
and fixed with paraformaldehyde solution (1 ml/100 g).
Immunohistochemistry. Formalin-fixed and
paraffin-embedded lung tissues were deparaffinized and rehydrated,
quenched with 3% H2O2, blocked with 5% normal
goat serum and probed with rabbit anti-rat IL-18/ICAM-1 antibody.
Detection was with biotinylated anti-rabbit IgG, followed by
incubation with avidin-biotin complex and substrate
(diaminobenzidine) followed with hematoxylin counterstaining. These
experiments were performed in triplicate.
Enzyme-linked immunosorbent assay (ELISA).
The IL-18 levels in serum and BALF were measured by ELISA according
to the manufacturer’s instructions (Nanjing Huadong electron group
medical equipment Co., Ltd., Nanjing, China), the sensitivity and
specificity of the method are 99 and 92%, respectively. Each
diluted sample (100 μl) was applied in triplicate on 96-well
plates pre-coated with capture antibody for 2 h, followed by
incubation with detection antibody for 1 h and avidin-HRP for 30
min. The plates were then developed using
3,3′,5,5′-tetramethylbenzidine and terminated by 2 M
H2SO4. The OD value was then recorded at 450
nm. These experiments were performed in triplicate.
Statistical analysis
All data were analyzed using SPSS 11.0 statistical
software (SPSS, Inc., Chicago, IL, USA). Respiration curve data and
the level of IL-18 in peripheral blood and BALF were analyzed by
analysis of variance (ANOVA). The rank sum test and Spearman’s rank
correlation analysis were used to analyze the expression of IL-18
and ICAM-1 in the two groups. P<0.05 was considered to indicate
a statistically significant difference.
Results
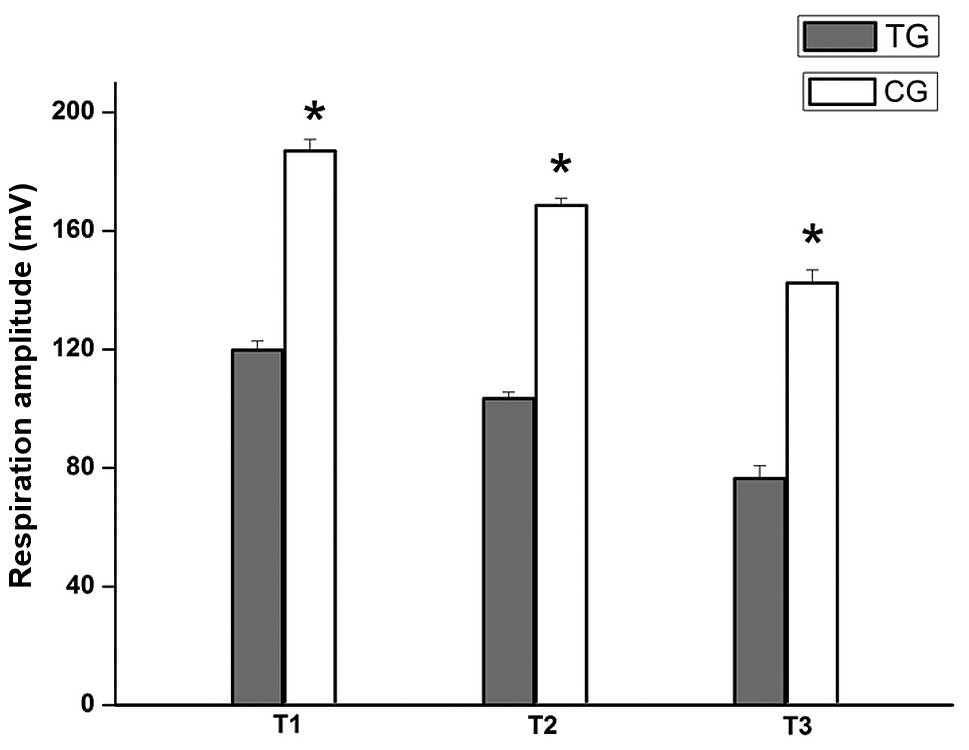
Comparison of the respiration curves
of the two groups
A respiration curve was collected and recorded using
the BL-420 biological signal collecting and processing system.
Respiration amplitude reflects alveolar ventilation; respiration
amplitude is likely to deepen or enlarge when the lung function
reduces. Respiration duration time reflects the breathing rate. As
shown in Figs. 1 and 2, at the same time-point, the respiration
amplitude of TG rats was lower and the duration time was shorter
compared with the respective value in CG rats. The respiration
curve shows that after using breviscapine, the respiration curve of
TG rats tended to be closer to normal compared with that of CG
rats. Therefore, breviscapine may enhance respiratory function.
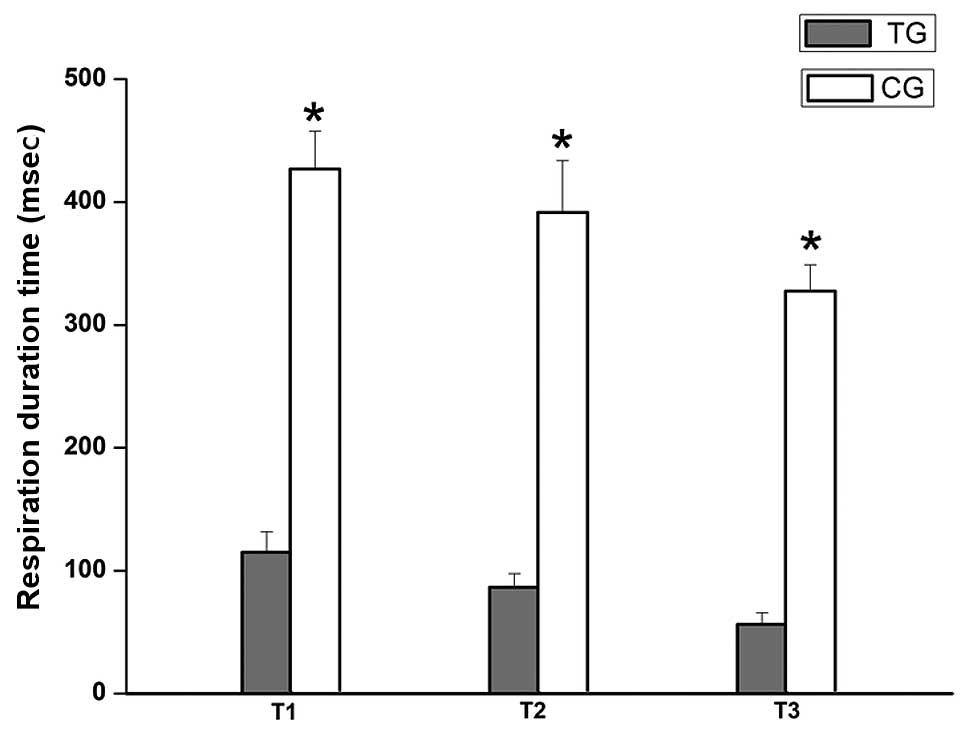
Comparison of PaO2 between
the two groups
PaO2 was measured with a blood gas
analyzer. PaO2 is used to judge respiratory function.
PaO2 reduces during respiratory dysfunction. As shown in
Fig. 3, PaO2 in the TG
was higher compared with that in the CG, which suggests that
respiratory function was improved following the administration of
breviscapine.
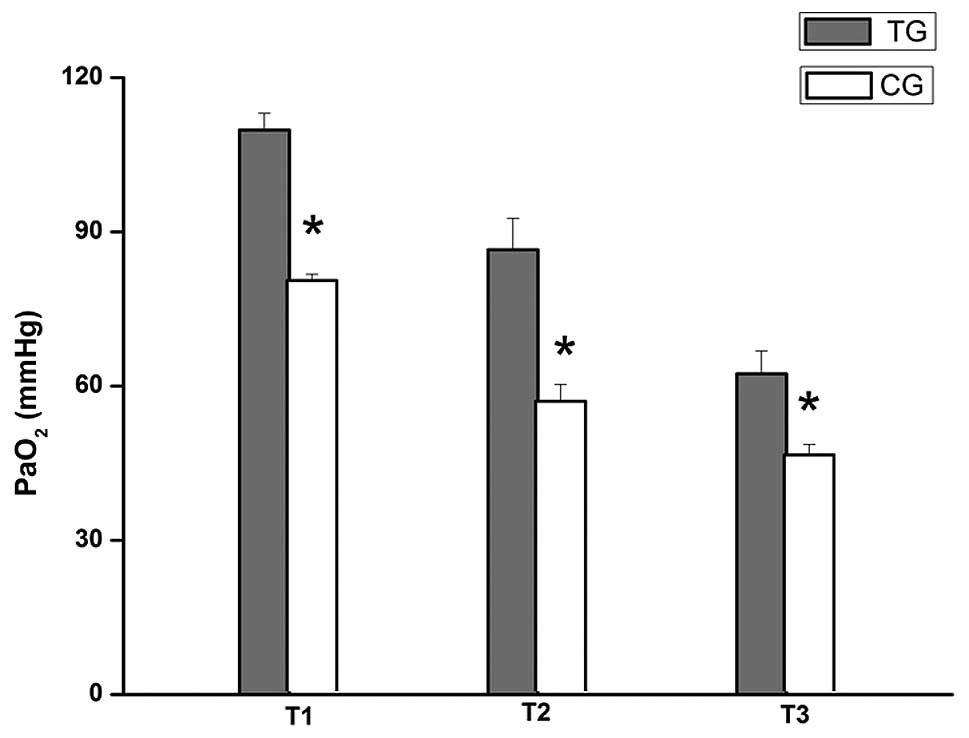
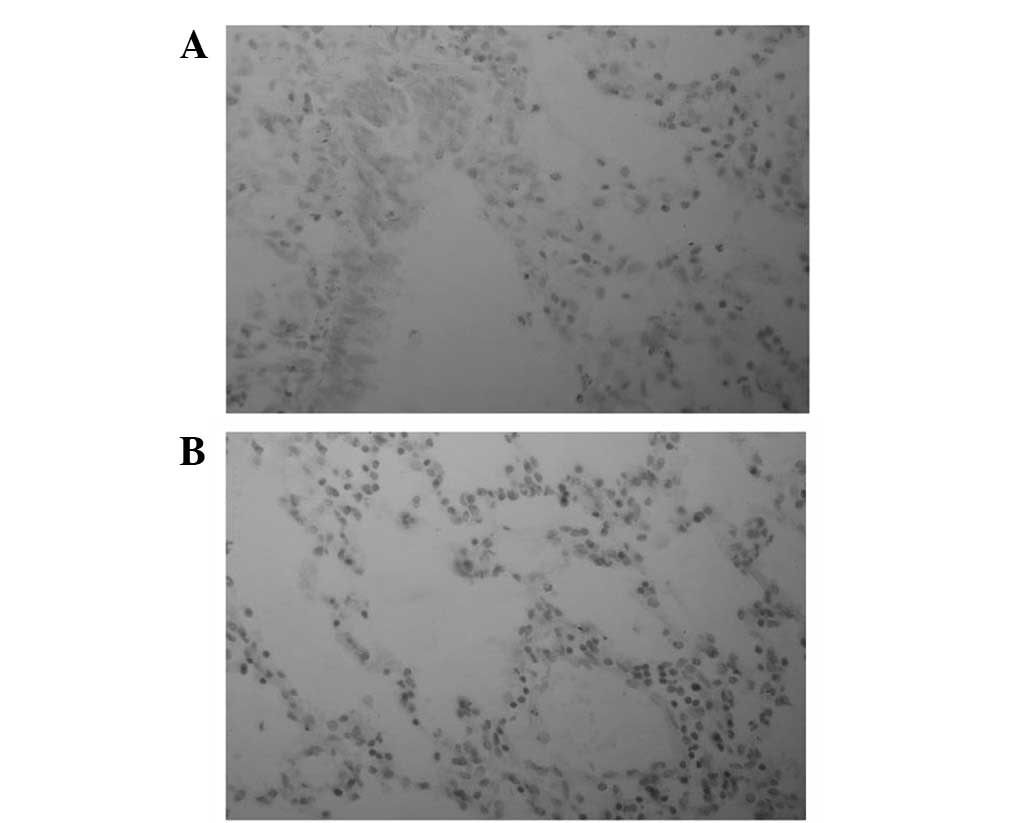
Comparison of the expression of IL-18
in lung tissue between the two groups
IL-18 is pro-inflammatory factor, which is released
as a result of inflammation. As IL-18 levels increase, more
pro-inflammatory cytokines are released; therefore, inflammation is
amplified. Immunohistochemistry was used to examine the expression
of IL-18. The immune response products of IL-18 are mainly located
in the cytoplasm. As shown Table I
and Fig. 4, the positive
expression of IL-18 in TG lung tissue was lower compared with that
in CG lung tissue, which indicates that acute inflammation in TG
lung tissue was milder.
 | Table I.Comparison of the expression level of
IL-18 in lung tissue between the two groups. |
Table I.
Comparison of the expression level of
IL-18 in lung tissue between the two groups.
| Time | n | IL-18
| Z | P-value |
|---|
| − | + | ++ | +++ |
|---|
| T1 | | | | | | | |
| TG | 10 | 4 | 3 | 3 | 0 | | |
| CG | 10 | 1 | 4 | 3 | 2 | 1.972 | 0.037 |
| T2 | | | | | | | |
| TG | 10 | 2 | 3 | 3 | 1 | | |
| CG | 10 | 1 | 1 | 5 | 3 | 1.963 | 0.042 |
| T3 | | | | | | | |
| TG | 10 | 2 | 2 | 4 | 2 | | |
| CG | 10 | 0 | 1 | 4 | 5 | 2.489 | 0.023 |
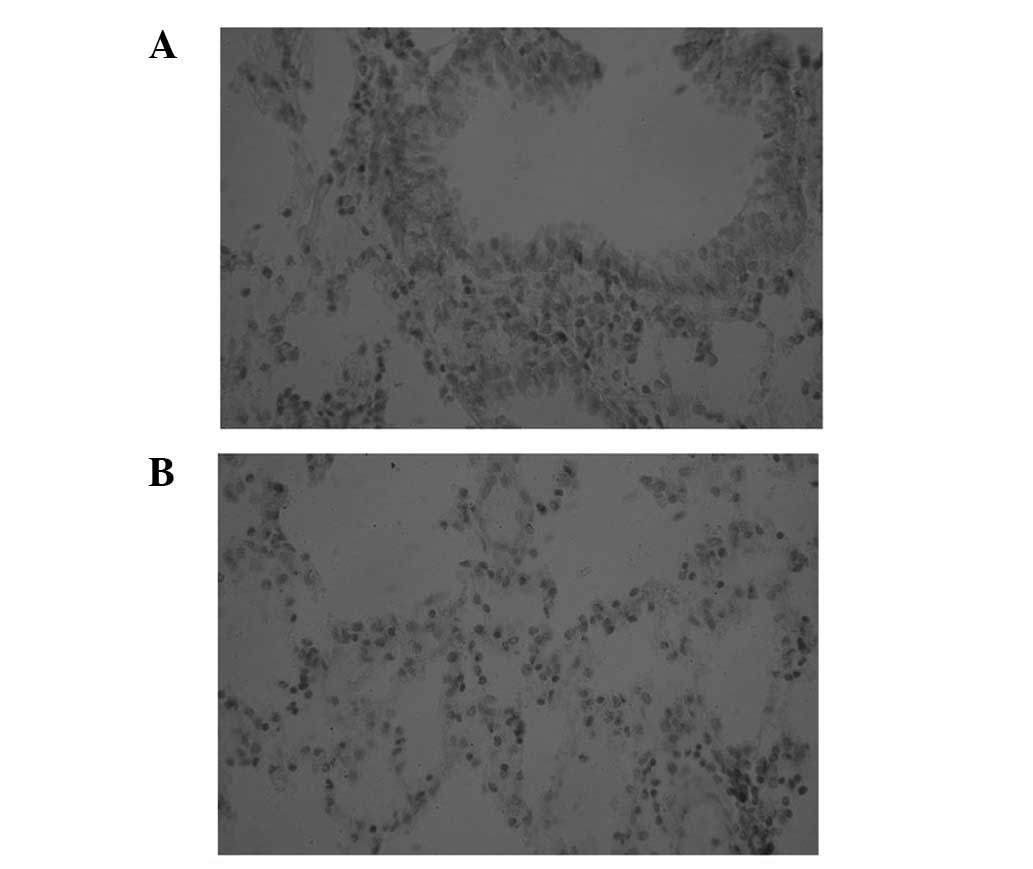
Comparison of the expression of ICAM-1
in lung tissue between the two groups
The immune response products of ICAM-1 were mainly
located in the cytoplasm or membrane. The positive expression of
ICAM-1 was lower in the TG compared with that in the CG (Table II and Fig. 5), which demonstrates that
breviscapine attenuates the damage of lung tissue.
 | Table II.Comparison of the expression of ICAM-1
in lung tissue between the two groups. |
Table II.
Comparison of the expression of ICAM-1
in lung tissue between the two groups.
| Time | n | ICAM-1
| Z | P-value |
|---|
| − | + | ++ | +++ |
|---|
| T1 | | | | | | | |
| TG | 10 | 3 | 3 | 3 | 1 | | |
| CG | 10 | 3 | 4 | 2 | 1 | 2.158 | 0.014 |
| T2 | | | | | | | |
| TG | 10 | 2 | 3 | 2 | 2 | | |
| CG | 10 | 1 | 4 | 3 | 2 | 1.968 | 0.043 |
| T3 | | | | | | | |
| TG | 10 | 2 | 3 | 3 | 2 | | |
| CG | 10 | 1 | 1 | 4 | 4 | 2.263 | 0.012 |
Correlation between IL-18 and ICAM-1
expression in lung tissue of the TG
In order to further evaluate whether the expression
of IL-18 is correlated with the expression of ICAM-1, we used the
rank sum test and Spearman’s rank correlation analysis. The results
demonstrated that the expression of IL-18 and ICAM-1 were directly
correlated (Table III).
 | Table III.Correlation between IL-18 and ICAM-1
expression in the lung tissue of the TG. |
Table III.
Correlation between IL-18 and ICAM-1
expression in the lung tissue of the TG.
| ICAM-1 | IL-18
|
|---|
| − | + | ++ | +++ |
|---|
| T1 | | | | |
| − | 0 | 0 | 0 | 0 |
| + | 0 | 1 | 2 | 0 |
| ++ | 0 | 1 | 2 | 1 |
| +++ | 0 | 0 | 2 | 1 |
| T2 | | | | |
| − | 0 | 1 | 0 | 0 |
| + | 0 | 1 | 2 | 0 |
| ++ | 0 | 0 | 2 | 1 |
| +++ | 0 | 1 | 1 | 1 |
| T3 | | | | |
| − | 0 | 0 | 0 | 0 |
| + | 0 | 1 | 1 | 0 |
| ++ | 0 | 1 | 2 | 1 |
| +++ | 0 | 0 | 2 | 2 |
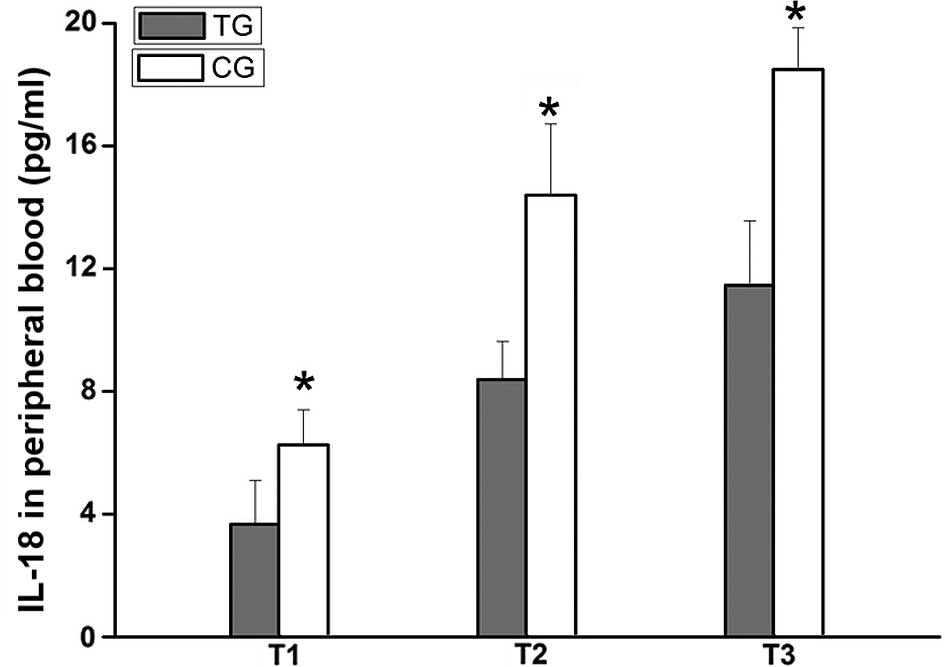
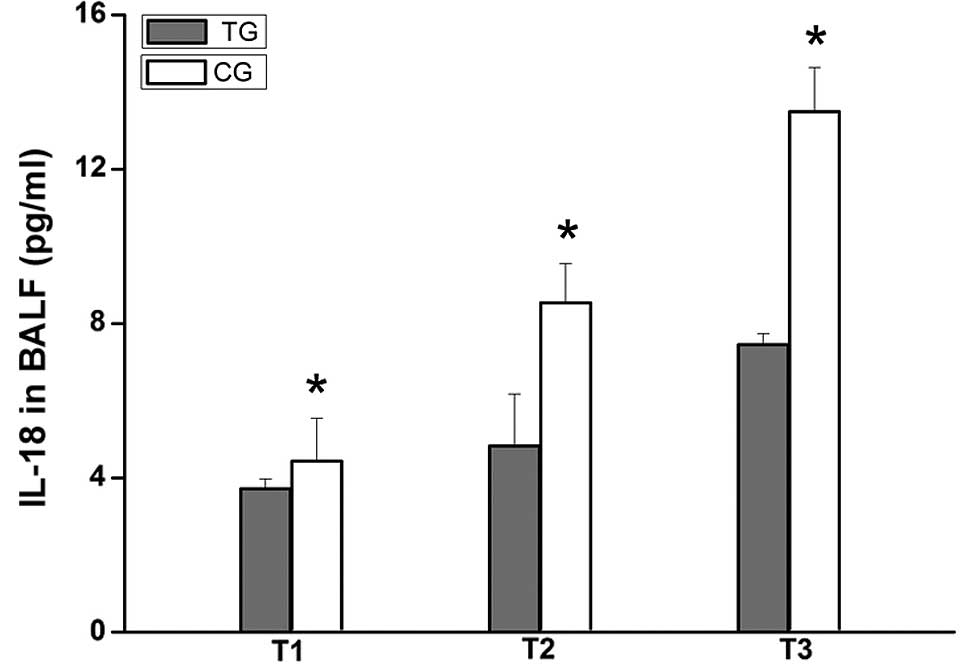
Comparison of the level of IL-18 in
peripheral blood and BALF between the two groups
ELISA was used to measure the level of IL-18 in
peripheral blood and BALF. The results demonstrated that the level
of IL-18 in TG rats was lower in peripheral blood and BALF
(Figs. 6 and 7). The results indicate that breviscapine
reduces the inflammatory reaction.
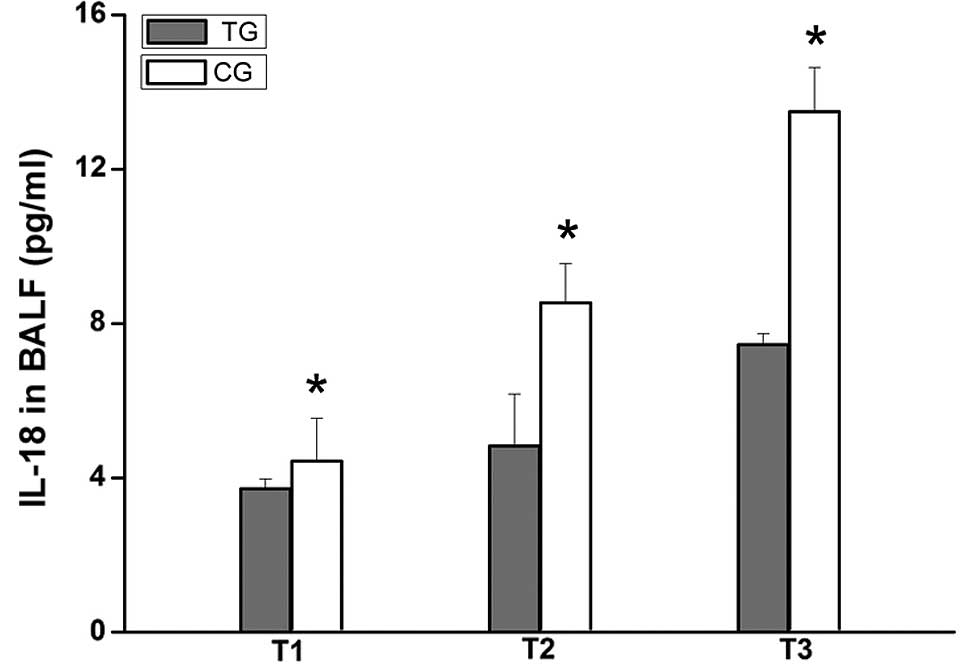 | Figure 7.Comparison of the level of IL-18 in
BALF between the two groups (n=10). The level of IL-18 in BALF was
assessed using ELISA. The level of IL-18 in the BALF of TG rats was
lower compared with that of CG rats at T1, T2 and T3.
*P<0.001, vs. TG rats. BALF, bronchialalveolar lavage
fluid; ELISA, enzyme-linked immunosorbent assay; IL-18, interleukin
18; T1, 30 min after ligating; T2, 30 min after reperfusion; T3, 60
min after reperfusion; TG, treatment group; CG, control group. |
Discussion
IL-18 is mainly released from activated pulmonary
macrophages. As a pro-inflammatory cytokine, IL-18 promotes T-cell
maturation, enhances neutrophil activity and induces the production
of inflammatory mediators, including TNF-α, IL-1β and IL-8. In
addition to this, IL-18 promotes the expression of ICAM-1 (7–9).
The ICAM-1 protein is mainly located on the surface
of endothelial cells and is barely expressed on the majority of
human tissues under physiological conditions (10,11).
The level of expression of ICAM-1 on endothelial cells is increased
under pathological conditions. ICAM-1 interacts closely with
integrin located on the surface of granulocyte cells, which causes
aggregation, adhesion and the release of leucocytes, as well as
immediate cytokine release (12,13).
This process is the molecular biological basis of the inflammatory
reaction.
Based on this, we established a rat model of acute
lung injury induced by left heart ischemic reperfusion and treated
the model rats with breviscapine. Then, we used various methods to
determine the effect of breviscapine on lung function. We observed
the respiration curve, measured PaO2 levels, determined
the expression of IL-18 and ICAM-1 and detected the levels of IL-18
in the peripheral blood and BALF.
The results demonstrated that respiration was better
in amplitude and duration time in the TG rats compared with that of
the TG rats at the same time-point (Figs. 1 and 2). The PaO2 in the TG was
higher compared with that in the CG (Fig. 3). These results indicate that
breviscapine may protect respiratory function.
To further explore the possible mechanism by which
breviscapine protects respiratory function, we measured the
expression levels of IL-18 and ICAM-1 in lung tissue by
immunohistochemistry and analyzed the levels of IL-18 in the
peripheral blood and BALF by ELISA. The results revealed that the
levels of IL-18 in the peripheral blood and BALF of the TG rats
were clearly lower compared with those of the CG rats (Figs. 6 and 7), and the expression levels of IL-18 and
ICAM-1 in the TG rats were markedly reduced (Tables I and II, Figs.
4 and 5). These results
indicate that breviscapine inhibits the expression of IL-18 and
ICAM-1 in lung tissue. To determine whether the expression of IL-18
also affects the expression of ICAM-1, we analyzed the correlation
between IL-18 and ICAM-1 expression. Analysis of the data revealed
that the expression of IL-18 had a positive correlation with the
expression of ICAM-1 in the same lung tissue of TG rats, and that
low IL-18 expression levels always coincided with low ICAM-1
expression levels (Table III).
These results indicate that breviscapine reduces the release of
IL-18 by lowering the aggregation and adhesion of neutrophils. As a
result, the release of ICAM-1 is reduced and the inflammatory
reaction is weakened. Therefore, breviscapine may decrease the
acute lung injury induced by left heart ischemic reperfusion by
inhibiting the inflammatory reaction.
In conclusion, in the acute lung injury model
induced by left heart ischemic reperfusion, breviscapine was able
to decrease the expression of IL-18 and ICAM-1, and relieve
inflammatory injury in the lungs, therefore, lung function was
protected.
Abbreviations:
|
IL-18
|
interleukin 18;
|
|
ICAM-1
|
inflammatory cell adhesion
molecule-1;
|
|
TG
|
treatment group;
|
|
CG
|
control group;
|
|
T1
|
30 min after ligaturing;
|
|
T2
|
30 min after reperfusion;
|
|
T3
|
60 min after reperfusion;
|
|
PaO2
|
arterial partial pressure of
oxygen;
|
|
BALF
|
bronchialalveolar lavage fluid;
|
|
PCT
|
procalcitonin;
|
|
NE
|
neutrophil elastase;
|
|
ELISA
|
enzyme-linked immunosorbent assay;
|
|
ANOVA
|
analysis of variance.
|
Acknowledgements
This study was supported by grants
from the Foundation of Henan Educational Commission (grant no.
2011GGJS-127), Henan Science and Technology Bureau to Mingli Ji
(grant no. 132300410160) and Henan Natural Science (grant no.
12B310017) to Yuxia Wang.
References
|
1.
|
Ji M, Qian Z, Song X and Wang Y: An animal
model of acute lung injury induced by left heart
ischemia-reperfusion. Chin J Pathophysiol. 27:1453–1456. 2011.(In
Chinese).
|
|
2.
|
van de Veerdonk FL, Netea MG, Dinarello CA
and Joosten LA: Inflammasome activation and IL-1β and IL-18
processing during infection. Trends Immunol. 32:110–116. 2011.
|
|
3.
|
Chen J, Zhao YH, Liu XL, Chen XL, Li J,
Lian QQ, et al: Effects of breviscapine on pulmonary inflammatory
response and lung injury in children undergoing open heart surgery.
J Asian Nat Prod Res. 14:270–275. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Xie WX, Yue LM and Song HL: Protective
effect of breviscapine on cardiac function in children after
cardiopulmonary bypass undergoing open heart surgery. Zhongguo
Zhong Xi Yi Jie He Za Zhi. 30:264–267. 2010.(In Chinese).
|
|
5.
|
Zhang MY, Fan SJ, Li LP, Wu BY and Wang Y:
The anti-injury effect of breviscapine injection on the hypoxic
ischemic brain damage of neonatal rats and the expression of Bcl-2
and Bax. Zhongguo Ying Yong Sheng Li Xue Za Zhi. 27:196–200.
2011.(In Chinese).
|
|
6.
|
Barker BR, Taxman DJ and Ting JP:
Cross-regulation between the IL-1β/IL-18 processing inflammasome
and other inflammatory cytokines. Curr Opin Immunol. 23:591–597.
2011.
|
|
7.
|
Volin MV and Koch AE: Interleukin-18: a
mediator of inflammation and angiogenesis in rheumatoid arthritis.
J Interferon Cytokine Res. 31:745–741. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Nishimoto N: Interleukin-6 as a
therapeutic target in candidate inflammatory diseases. Clin
Pharmacol Ther. 87:483–487. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Pedroza M, Schneider DJ and
Karmouty-Quintana H: Interleukin-6 contributes to inflammation and
remodeling in a model of adenosine mediated lung injury. PLoS One.
6:e226672011. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Yokomura I, Iwasaki Y, Nagata K, et al:
Role of intercellular adhesion molecule-1 in acute lung injury
induced by candidemia. Exp Lung Res. 27:417–411. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Porter JC and Hall A: Epithelial ICAM-1
and ICAM-2 regulate the egression of human T cells across the
bronchial epithelium. FASEB J. 23:492. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Gustapane M, Cardillo MT, Biasillo G and
Biasucci LM: Myeloperoxidase as possible diagnostic and prognostic
marker of acute coronary syndrome. Recenti Prog Med. 102:447–450.
2011.(In Italian).
|
|
13.
|
Ramirez P, Ferrer M, Gimeno R, et al:
Systemic inflammatory response and increased risk for
ventilator-associated pneumonia: a preliminary study. Crit Care
Med. 37:1691–1615. 2009. View Article : Google Scholar : PubMed/NCBI
|