Introduction
Chronic lumbar pain is mainly caused by lumbar
discogenic pain that originates from lumbar spondylosis. Lumbar
spondylosis manifests as mechanical back pain with instability of
the lumbar spine and regression of zygapophysial joints, which may
develop into lumbar pain and neurogenic intermittent claudication
(1,2), caused by lumbar spinal stenosis.
Conservative treatments for severe lumbar spondylosis tend to be
ineffective and surgery is currently the main treatment method. In
addition to bone grafting and internal fixation, the surgery
includes removal of the nucleus gelatinosus and/or a laminectomy
for decompression. However, several studies have indicated that
fusion procedures do not improve the outcome of lumbar spondylosis,
even with a success rate of 98% (3). Furthermore, the analgesic period
following fusion procedures that include internal fixation is
shorter than the surgery itself (excluding the internal fixation)
(3). The discrepancy mainly occurs
due to the surgery destroying the biomechanical environment of the
lumbar motion segment, particularly those that include rigid
internal fixation, which prevents the load transfer from conforming
to physiological conditions. This ultimately accelerates the
degeneration of adjacent segment facets, loosens the internal
fixation and results in fatigue fractures. Consequently, lumbar
non-fusion fixation has gained increasing attention in previous
years. Among numerous non-fusion fixation procedures, artificial
lumbar disc replacement is regarded as a promising area of
development. Its theoretical advantages include removal of the
source of discogenic lumbar pain, allowance for the motion of an
implanted segment, restoration of intervertebral disc height and a
shorter rehabilitation time compared with that of fusion
operations. At present, the predominant design of artificial lumbar
disc involves reconstruction as ball and socket joints, which allow
rotation of the intervertebral disc segments, such as with
Prodisc-L™ (Synthes Spine, Inc., Paoli, PA, USA), which employs a
polyethylene nucleus pulposus and metal soleplate (4). Additionally, Activ-L® (B.
Braun/Aesculap, Tuttlingen, Germany) allows rotation and retains
backward motion (5); and
Mobidisc® (LDR Médical, Troyes, France) is capable of
movement in all directions in the plane parallel to the
physiological soleplate (6).
However, with increasing application, the clinical effects of
artificial lumbar disc replacement fail to meet the theoretical
standards. Related studies have demonstrated that this failure is
due to regression of the zygapophysial joints, an impractical
intervertebral opening height and an undesirable prosthesis
position. Rohlmann et al(7)
identified that the occurrence of lower back pain following
artificial lumbar disc replacement is associated with increased
stress on the zygapophysial joints. Additionally, Kim et
al(8) indicated that following
artificial lumbar disc replacement, segment extension activity
increases significantly during extension, which directly increases
the stress on zygapophysial joints compared with the direct stress
on the zygapophysial joints of adjacent segments. Subsequently, the
increased stress causes regression of the zygapophysial joints and
ultimately results in lumbar regression.
The current design of non-constrained artificial
discs (NADs) may be improved by constructing semi-constrained disc
prostheses, wherein a fiber structure is added to simulate the
fiber-connecting properties of the physiological disc and to
constrain its activity. This modification may decrease the stress
on the zygapophysial joints and improve the clinical therapeutic
effects of lumbar disc replacement (5). The present study investigated a newly
designed semi-constrained integrated artificial disc (SIAD; Weigao
Orthopaedic Device Co., Ltd., Weihai, China) with a titanium plate
in its framework, polyethylene glycol terephthalate elastic
ligaments that simulate the annulus fibrosus of the physiological
discs and a polyetheretherketone (PEEK) core that simulates the
nucleus pulposus. This study compared the effects of physiological
discs, SIADs and NADs on the stresses on zygapophysial joints and
the load translation of the implanted segments, using finite
element (FE) analysis. Furthermore, the rationality of using the
artificial disc prosthesis for the treatment of chronic lumbar
pain, was evaluated.
Materials and methods
FE model
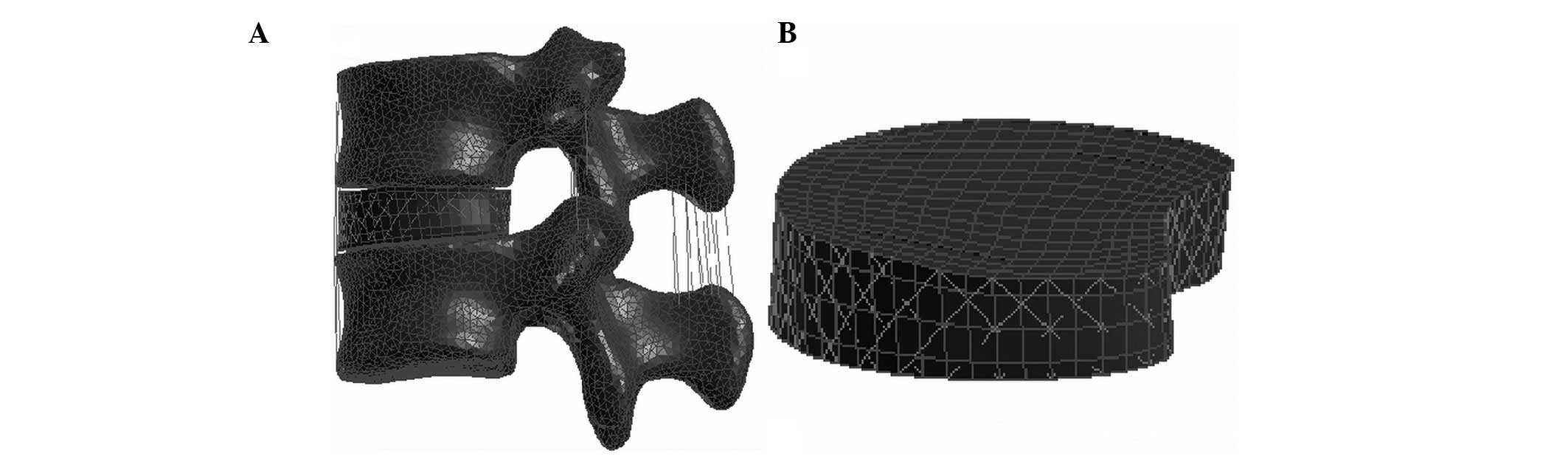
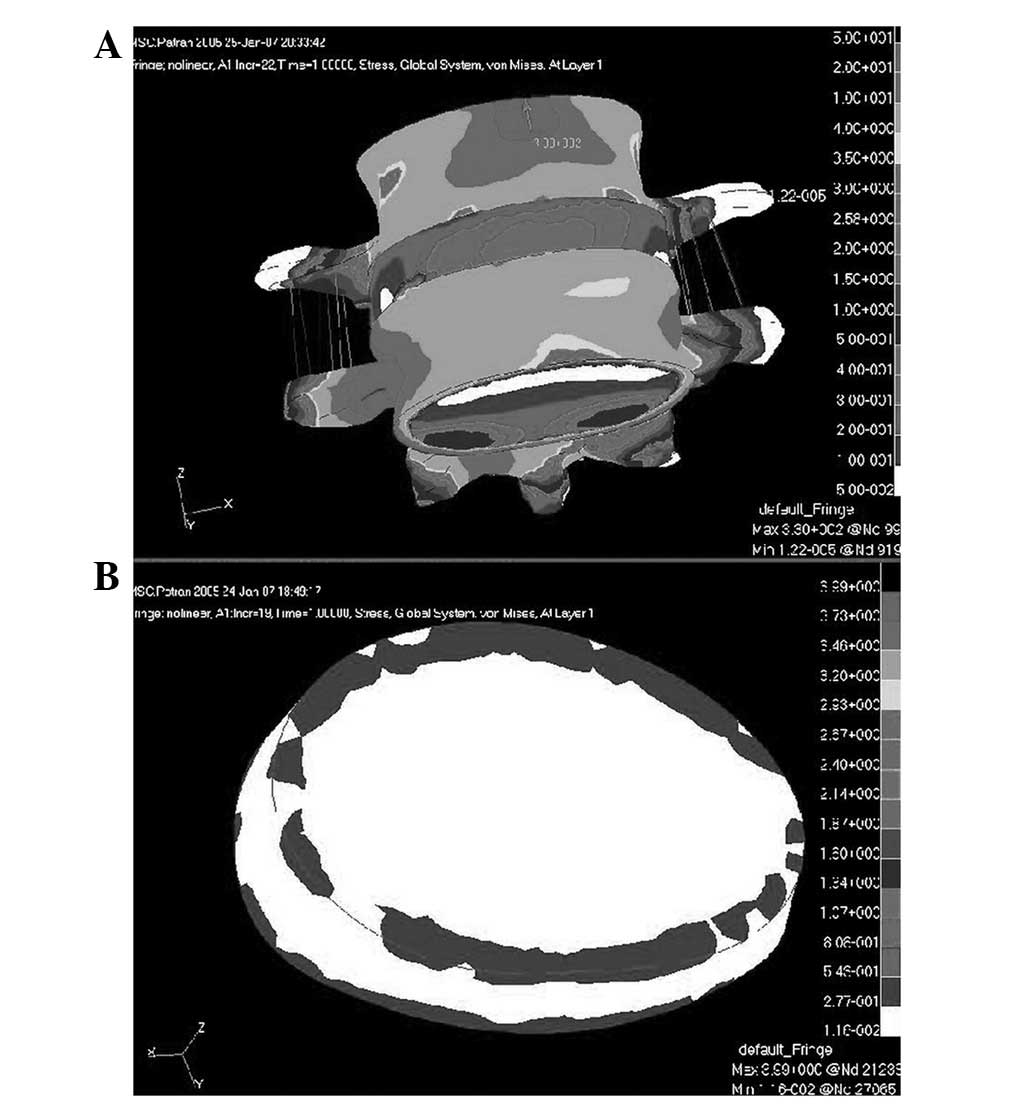
A 21-year-old male volunteer (height, 175 cm) was
selected as the simulation subject. The L4–L5 spinal segment of the
patient was allowed a 0.75 mm stratum depth. The data required for
constructing the FE model of the lumbar L4–L5 segment was obtained
through continuous computed tomography (CT) scanning. The lumbar FE
model was constructed after converting data from the CT scan into
3D data using Mimics software (version 10.0, Materialise Inc.,
Leuven, Belgium) and Patran preprocessing software (MSC.Software
Corp., Surrey, United Kingdom; Fig.
1). The centrum consisted of external cortical bone and
internal cancellous bone. The cortical bone was set at 1.0 mm and
the different sections were connected and simulated as a solid
unit, which was then simplified into continuous, even and isotropic
bone structures. The thickness of the soleplate was 1.0 mm and the
interval between the zygapophysial joints was 1.0 mm. In addition,
the articular cartilage surface was simulated using an area unit
with a thickness of 1.0 mm. The two contact surfaces had no
friction, moved relatively at a 0.6-mm distance and were simulated
by a nonlinear link unit. The intervertebral disc consisted of an
annulus fibrosus and a nucleus pulposus. The annulus fibrosus was
simulated as a ring of stroma embedded with three layers of
collagen fiber that intersected the horizontal plane of the
intervertebral disc at a ±30° included angle. A linear elastic
material that only accepts tensile stress was used and simulated a
link linear unit. Moreover, the stroma of the annulus fibrosus was
simulated as a solid unit, with an elastic modulus of 4.2. The
ligament structure such as the spinal ligaments (anterior
longitudinal, posterior longitudinal, inter- and supraspinal and
intertransverse ligaments, ligamentum flavum and zygapophysial
joint ligaments), the fibers and capsula articularis were simulated
as link units using a linear elastic material that only accepts
tensile stress. The elastic moduli and the Poisson’s ratio of the
different parts of the FE model were in accordance with the
literature (9–11) (Table
I). This study was conducted in accordance with the Declaration
of Helsinki with approval from the ethics committee of Nanjing
Medical University Hospital (Nanjing, China). Written informed
consent was obtained from the participant.
 | Table IElastic modulus, Poisson ratio and
sectional area of different structures. |
Table I
Elastic modulus, Poisson ratio and
sectional area of different structures.
| Structure | Elastic modulus
(MPa) | Poisson ratio | Sectional area
(mm2) |
|---|
| Titanium plate | 77000.0 | 0.3000 | - |
| PEEK | 3600.0 | 0.3000 | - |
| Cortical bone | 12000.0 | 0.3000 | - |
| Cancellous bone | 100.0 | 0.2000 | - |
| Articular
cartilage | 10.0 | 0.4000 | - |
| Posterior part of the
vertebral body | 3500.0 | 0.2500 | - |
| Lamina
terminalis | 1000.0 | 0.4000 | - |
| Matrix of fibrous
ring of intervertebral disc | 4.2 | 0.4500 | - |
| Nucleus pulposus
intervertebral disc | 0.2 | 0.4999 | - |
| Fiber of fibrous
ring | 450.0 | 0.3000 | 0.15 |
| Anterior
longitudinal ligament | 20.0 | 0.3000 | 38.00 |
| Posterior
longitudinal ligament | 70.0 | 0.3000 | 20.00 |
| Ligament
flavum | 50.0 | 0.3000 | 60.00 |
| Interspinous
ligament | 28.0 | 0.3000 | 35.50 |
| Supraspinous
ligament | 28.0 | 0.3000 | 35.50 |
| Intertransverse
ligament | 50.0 | 0.3000 | 10.00 |
| Articular
capsule | 100.0 | 0.3000 | 40.00 |
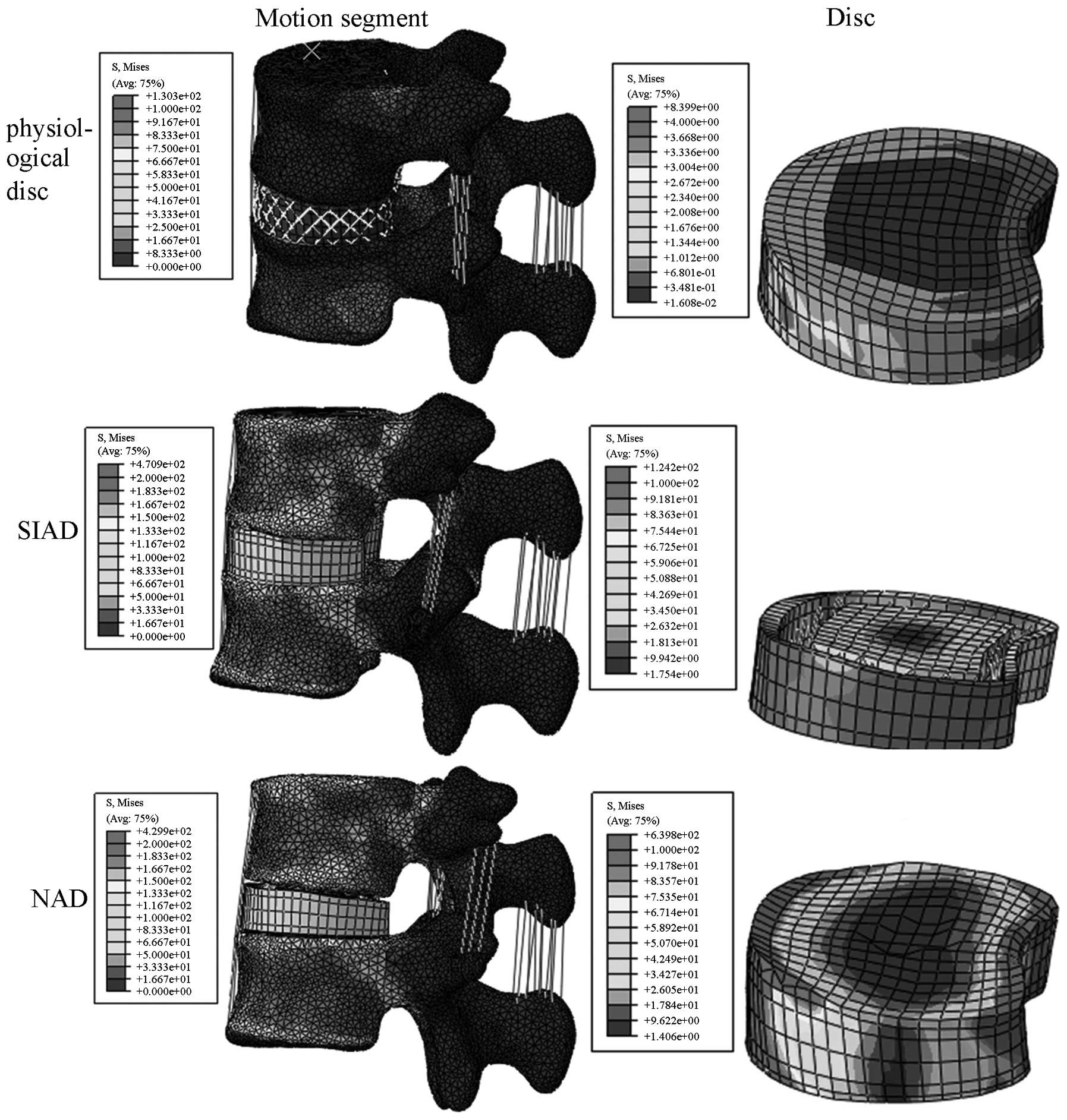
SIAD FE model construction
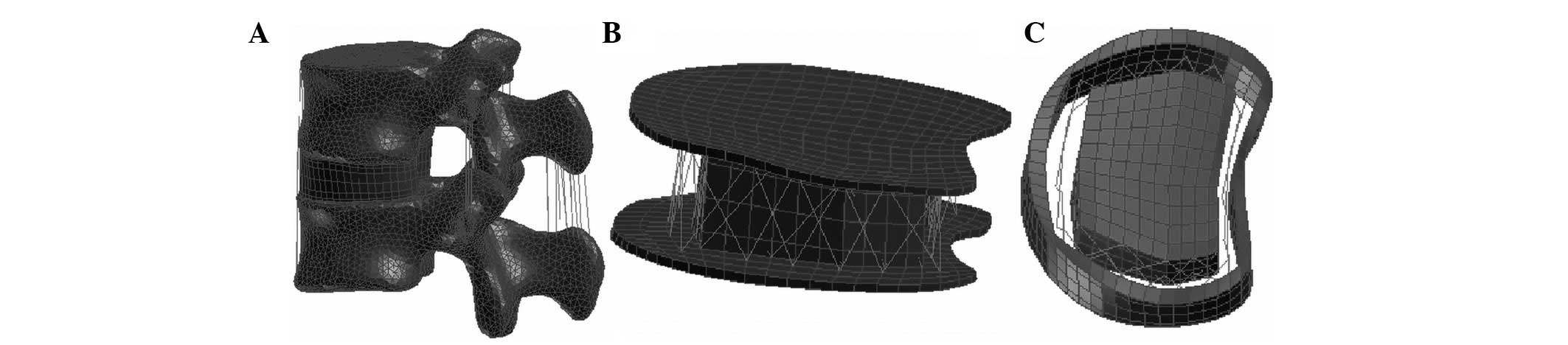
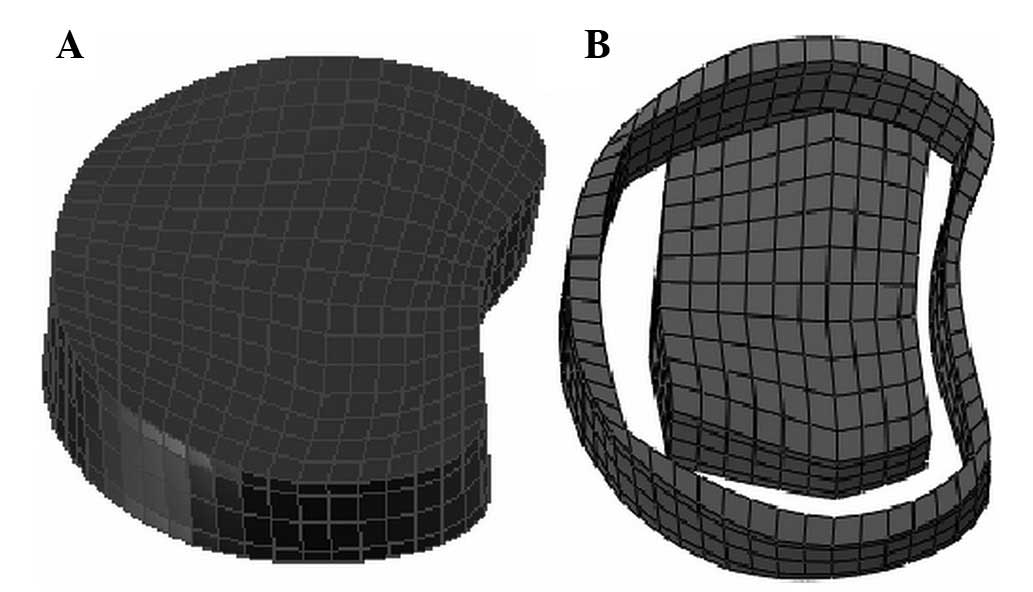
The SIAD artificial disc was integrated as an
artificial disc prosthesis. The elastic modulus of its titanium
soleplate was 77,000 MPa and its nucleus pulposus consisted of PEEK
with an elastic modulus of 3,600 MPa. The polyethylene glycol
terephthalate elastic ligament that enveloped the PEEK nucleus
pulposus, was woven into the soleplate to form a ±30° included
angle with the horizontal plane of the intervertebral disc. The
annulus fibrosus of the physiological disc was simulated using a
linear elastic material that only accepts tensile stress and a
nonlinear link unit was used for simulation. Furthermore, the upper
and lower soleplates were fixed with a vertebral soleplate. The
nucleus pulposus and the upper and lower soleplates were set as
non-friction contact surfaces that moved relatively 0.6 mm apart
(Fig. 2).
NAD FE model construction
The NAD was integrated as the prosthesis with the
elastic fibers removed. The elastic modulus of its titanium
soleplate was 77,000 MPa and its nucleus pulposus consisted of
PEEK, which was divided into upper and lower sections by a
horizontal plane. The elastic modulus of the PEEK was 3,600 MPa.
The different sections of the model were fixed with an adjacent
titanium soleplate and the two sections were set as non-friction
contact surfaces that moved relatively 0.6 mm apart (Fig. 3).
Model verification
Normal neutral stress on the lower lumbar segment
was simulated to calibrate the FE model to enable it to be compared
with other lumbar FE models. Up to two-thirds of a typical human
weight (~40 kg or 400 N of a 60-kg subject) was divided into four
Von Mises stresses, each at 100 N. Each stress was used as a node
load applied to the anterior and posterior of the vertebral joints
equidistant from the L4 vertebral rotation axis by 19 steps. Von
Mises stress is an equivalent stress based on shear strain energy,
which is calculated using the following formula:
{[(a1−a2)2 + (a2−a3)2 +
(a3−a1)2]/2}1/2, where a1, a2 and a3
represent the first, second and third major stresses, respectively
(9). The degrees of freedom of the
structures on the lower surface of the L5 vertebra, which were
considered static, were set to zero. The results of the model were
compared with those of the lumbar FE models reported by Goto et
al(10) and Grant et
al(11).
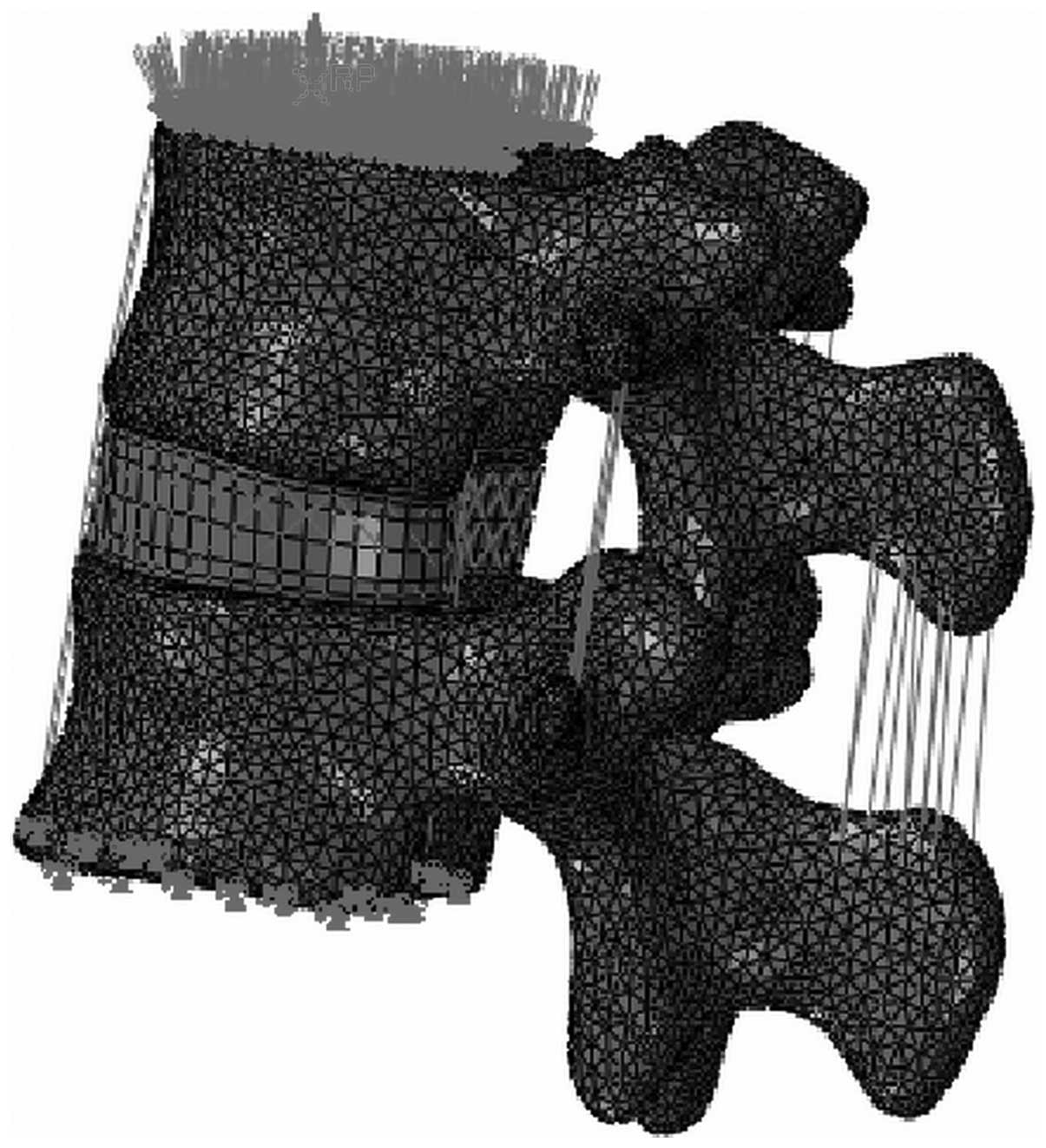
Stress loading
Stress loading was subdivided into two programs. The
Patran preprocessing software (Dassault Systemes Simulia Corp.,
Providence, RI, USA) was used to construct the lumbar FE model and
the Abaqus FE analysis software was used to simulate the
constraints and loadings.
Working condition stress analysis
A 400-N downward force was applied axially on the
upper surface of the thoracic vertebra to simulate gravity on the
upper body at a neutral position. From the neutral position, 5°
anteflexion, 5° extension and 5° rotation were then simulated by
applying a 10-Nm moment. Subsequently, stress on the zygapophysial
joints was observed during 5° anteflexion, 5° extension and 5°
rotation. According to the calculations, the degrees of freedom of
all node translations of the L5 lumbar bottom were set to zero. A
tie constraint was used between the soleplate and the disc to
ensure that they did not separate (Fig. 4).
Statistical analysis
Statistical analysis was performed using SPSS 13.0
statistical software (SPSS, Chicago, IL, USA). P<0.05 was
considered to indicate a statistically significant result.
Results
General data
An FE model of the L4–L5 motion segment was
constructed. The model included 34,123 nodes and 162,858 units,
which contained 161,679 tetrahedral centrum elements, 1,053
hexahedral disc and soleplate elements, and 126 ligament link
units, capsula articularis and fibers. In the neutral position, a
400-N axial stress and a 10-Nm moment were applied to simulate
loading. Under the simulated anteflexion, extension and rotation,
the stresses and distribution of all units in the motion segment
were consistent with the results of the lumbar FE models reported
by Goto et al(10) and
Yamamoto et al(11)
(Fig. 5).
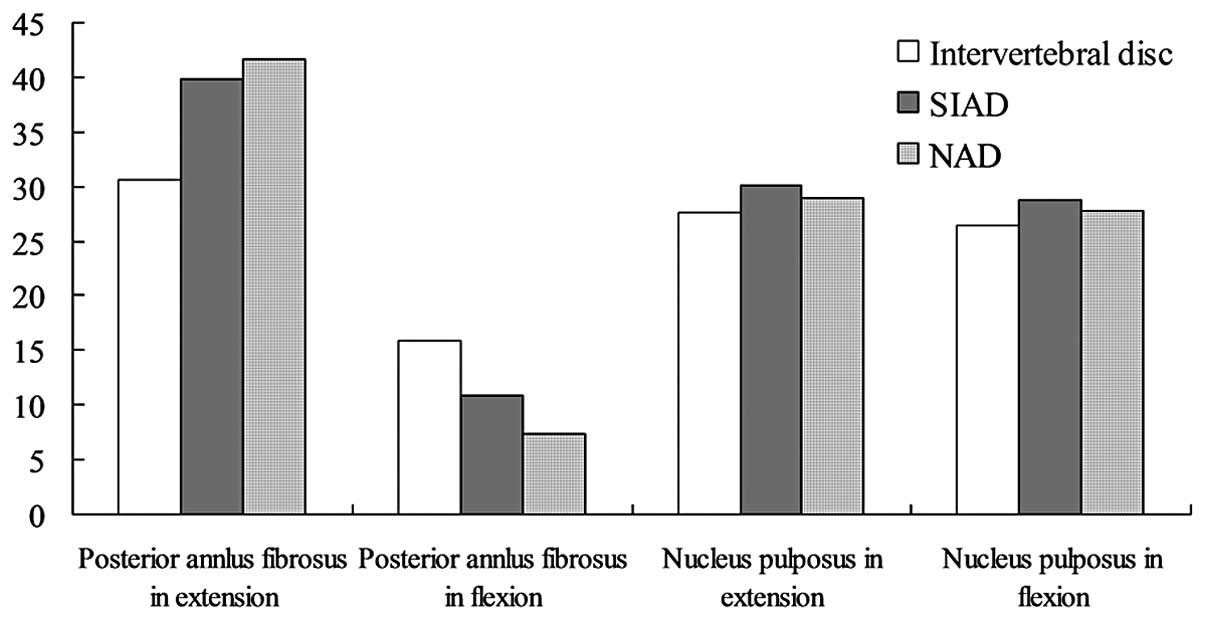
Working condition stress analysis
In anteflexion, the stresses on the zygapophysial
joints with physiological discs and those following implantation of
the SIAD demonstrated no significant differences, and were slightly
greater than those of NAD joints. During extension, the stresses on
the SIAD zygapophysial joints with SIAD and NAD transplants were
greater than those with physiological discs. However, the increase
in SIAD zygapophysial joint stresses was lower compared with that
of the NAD. During rotation, the stresses on the zygapophysial
joints and on the physiological discs were not significantly
different. The stresses on the NAD zygapophysial joints were
significantly greater compared with those on the joints of the
other two types during rotation (Tables II–V and Figs.
6–8).
 | Table IIStress analysis under 400-N applied
axial stress at 5° flexion, 5° extension and neutral positions. |
Table II
Stress analysis under 400-N applied
axial stress at 5° flexion, 5° extension and neutral positions.
| Posterior ring of
intervertebral disc stress (MPa) | Nucleus pulposus
stress (MPa) | Zygapophysial joint
stress (MPa) |
|---|
|
|
|
|
|---|
| Disc type | Extension | Neutral | Flexion | Extension | Neutral | Flexion | Extension | Neutral | Flexion |
|---|
| Physiological
disc | 410.9 | 42.7 | 21.4 | 159.8 | 151.2 | 155.2 | 193.1 | 114.5 | 63.6 |
| SIAD | 592.4 | 44.8 | 19.8 | 169.3 | 170.7 | 151.6 | 253.8 | 118.3 | 62.9 |
| NAD | 639.8 | 59.9 | 17.5 | 181.1 | 178.8 | 149.6 | 357.8 | 113.4 | 43.9 |
 | Table VDisplacement analysis of 400-N
applied axial stress and 10 Nm moment at flexion and extension
positions. |
Table V
Displacement analysis of 400-N
applied axial stress and 10 Nm moment at flexion and extension
positions.
| Displacement of
anterior ring of intervertebral disc (mm) | Displacement of
posterior ring of intervertebral disc (mm) | Average
displacement of zygapophysial joint (mm) |
|---|
|
|
|
|
|---|
| Disc type | Extension | Flexion | Rotation | Extension | Flexion | Rotation | Extension | Flexion | Rotation |
|---|
| Physiological
disc | 1.0 | - | 0.5 | - | 1.0 | 0.2 | 0.4 | 1.2 | 0.2 |
| SIAD | 1.4 | - | 0.7 | - | 1.3 | 0.3 | 0.7 | 1.5 | 0.3 |
| NAD | 2.0 | - | 1.3 | - | 2.0 | 0.6 | 1.2 | 2.2 | 0.5 |
The stresses on the SIAD zygapophysial joints during
anteflexion were not significantly different compared with those on
the zygapophysial joints of physiological discs. The zygapophysial
joint stresses and displacements of the SIAD and NAD following
implantation were greater than those of physiological discs during
extension (Fig. 8); however, the
increase in the stresses and segment activity of the SIAD
zygapophysial joints was lower than that of the NAD joints. The
stresses on the SIAD zygapophysial joint and those on the
physiological discs during rotation were not significantly
different; however, the stresses on the NAD zygapophysial joints
were significantly greater than those in the joints of the other
two types.
Discussion
Lumbar degenerative disease (LDD) is one of the most
common spinal diseases treated by surgery, affecting 80% of the
world’s population according to Hult statistics (12). The National Center for Health
Statistics of the USA reported that the most common factor for the
limitation of movement among people <45 years old is lumbar pain
syndrome caused by LDD. The annual treatment cost for LDD has
increased to millions of dollars, excluding losses from absenteeism
(13).
Treatment for chronic discogenic lumbar pain
includes artificial disc replacement, which maintains the activity
of the lumbar motion segment unlike traditional fusion operations
(14). Therefore, artificial disc
replacement is of increasing interest and FE analyses and clinical
application studies of artificial discs are increasing. Artificial
disc replacement is an important area for the development of
treatments for lumbar spondylosis due to the following (15–17):
i) it completely restores diseased intervertebral disc tissue and
eliminates mechanical back pain caused by intervertebral disc
disease; ii) it relieves the compression stimuli of degenerative
intervertebral discs on the spinal nerve and the nerve root, and
effectively releases the symptoms of nerve compression; iii) it
allows the activity of the operated segment to be maintained and
reduces the loss of lumbar activity following the surgical
procedure; and iv) it minimally affects the lumbar biomechanical
environment following implantation, with a lower incidence rate of
degeneration of the adjacent segments compared with that of
traditional fusion operations. Therefore, artificial disc
replacement may be applied in multisegment replacements (18,19).
Various artificial disc prostheses have been
designed (4,20–24).
Four major artificial disc prostheses are used in the USA: Charité
(DePuy Spine Inc., Raynham, MA, USA) (20) and Prodisc (Synthes Spine, Paoli,
PA, USA) (4), which are
metal-polythene prostheses that underwent clinical trials and
registration in the USA; and Maverick (Medtronic Sofamor Danek
Inc., Memphis, TN, USA) (25) and
FlexiCore (Stryker Spine, Allendale, NJ, USA) (26,27),
which are metal-metal (Co-Cr) interface prostheses. Artificial
discs are currently classified as three-component prostheses,
two-component prostheses and integrated prostheses. Regardless of
the various architectural designs, the clinical effects of
artificial disc replacement are considered unsatisfactory (28). For example, the two-component
prostheses (Prodisc) perform the loading function of the upper and
lower soleplates, respectively. They form a self-constrained
articular facet, but lose the stretching-constraining function of
physiological discs during lumbar twisting and have no load
buffering function. The three-component prostheses (Charité)
consist of upper and lower soleplates and an elastic core that
forms the articular facet of the prosthesis following composition
(29). However, three-component
prostheses have comparatively greater activity and do not feature
disc-constrained motion, which subsequently causes strain on the
rear zygapophysial joints that results in unsatisfactory long-term
clinical effects. The therapeutic effects of this type of
prosthesis do not meet theoretical expectations; therefore, disc
fiber-connecting mechanisms have gained increasing attention. With
this mechanism, a disc has a deformable fiber cartilage joint in
place of a movable vertebral synovial joint. A multi-cartilage
joint inhibits the range of activity and does not achieve the
buckling stress-strain curve of the physiological discs (Fig. 1). Therefore, all the described
prostheses result in biomechanical changes in the implanted
segments. A key reason for the unsatisfactory clinical effects is
the secondary degeneration of the implanted segments due to
accelerated degeneration of zygapophysial joints following the
surgery and secondary spinal stenosis. Therefore, development of an
integrated prosthesis that matches the disc fiber-connecting
function has become a topic of great interest in artificial disc
development (21–24).
McNally et al(30) anchored a multi-hardness elastic
nucleus composed of polycarbonates in various degrees on the upper
and lower titanium plates. This modification allowed the implanted
segments to rotate by continuously centering on the physiological
rotation axis. Keels on the upper and lower titanium plates are
associated with the soleplate and facilitate bone fusion. However,
in this design, which is named Physio-L. the absence of separate
elastic components and its increased technical complexity decrease
the reliability of the system, as it lacks the buckling
stress-strain curve of the annulus fibrosus of the physiological
discs. Its elastic core has weak points and its upper and lower
titanium plates, which do not contain elastic components, readily
cause structural failure under shearing loads. The Cadisc™-L
prosthesis designed by Ranier Technology Ltd. (Cambridge, UK)
(31) is made of polycarbonate
polyurethane materials that are integrated into the structure. The
buckling stress-strain curve of the physiological discs was
incorporated; however, metals were not used in the upper and lower
plates, due to the shaping and workmanship required, which
subsequently may affect stability as it hinders bone fusion with
the prosthesis. Furthermore, it is not possible to examine the
prosthesis by X-ray, which is inconvenient during operative
installation and postoperative follow-up (32,33).
In the present study, the SIAD structure had an
integrated semi-constrained artificial disc, with a soleplate
composed of titanium and polyethylene glycol terephthalate. An
elastic ligament was anchored onto the soleplate to simulate the
annulus fibrosus and a PEEK core was used as the elastic nucleus
pulposus. Theoretically, the SIAD simulates the connection of
physiological disc fibers and limits rotation, which in turn
decreases the stresses on the zygapophysial joints and improves the
clinical effects of disc replacement.
Further studies are required to verify the
aforementioned hypothesis. At present, common mechanical research
methods include animal experiments, physical experiments, in
vitro (cadaver) experiments and computer simulations. The
animals used in previous animal experiments were non-erect and were
markedly different in structure and function compared with humans.
Physical experiments have limited value due to the lack of in
vivo structural characteristics. However, the cost of in
vitro experiments is high and finding cadavers is difficult.
Moreover, in vitro experimental conditions greatly differ
from in vivo conditions (34). Notably, Thresher and Farah were
among the first to use the FE method (FEM) in the medical field.
Since 1973, the FEM has become an effective mathematical tool in
human biomechanical studies (35).
Therefore, the present study attempted to construct an FE model of
an early-stage degenerative lumbar motion segment to simulate the
biomechanical changes. The suitability of constructing an L4–L5
segment FE model was demonstrated by calibrating with the Goto
et al(10) and Yamamoto
et al(11) standard lumbar
models.
Following SIAD implantation, the increase in
pressure on the zygapophysial joint segments was only 79% that with
NAD implantation under a 400-N applied axial load and 10-Nm moment
during extension, whereas the translation was at 65% with NAD.
Furthermore, the load on the annulus fibrosus of the SIAD
increased, which demonstrated that the semi-constrained prostheses
protected the zygapophysial joints of implanted segments during
extension (153.3 MPa vs. 193.9 MPa). Under this load, the
corresponding degree of translational stress on the zygapophysial
joints following SIAD and physiological disc implantation was
higher than that for the NAD. Therefore, the SIAD design affects
the segment functional spinal unit less than the NAD does. Under a
400-N applied axial load and a 10-Nm right rotation moment, the
stresses on the segments of the zygapophysial joints with SIAD and
NAD implants increased compared with those on joints with
physiological discs. However, the increases in the stresses and the
translation on the zygapophysial joints of the NAD were higher
compared with those of the SIAD. Therefore, the semi-constrained
design has similar mechanical characteristics to physiological
discs and helps to protect the zygapophysial joints. Under an
applied axial load of 400 N with a 5° extension or 5° rotation
moment, the stresses on the SIAD zygapophysial joints were lower
than those on the NAD. Therefore, the semi-constrained design of
the SIAD buffers the stresses on the segment motion, which
subsequently protects the zygapophysial joints.
In the present study, the incision and suture of the
anterior and posterior longitudinal ligaments, as well as the
preservation of the structure of the Annulus fibrosus, were
not considered in the calculations of the working conditions. All
working conditions were simplified as in disc replacement. This
study demonstrated that based on the FE analysis, the SIAD
protected the zygapophysial joints of the implanted segment.
Therefore, application of the design may improve the clinical
therapeutic effects of artificial discs.
References
|
1
|
Swanson KE, Lindsey DP, Hsu KY, Zucherman
JF and Yerby SA: The effects of an interspinous implant on
intervertebral disc pressures. Spine (Phila Pa 1976). 28:26–32.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sengupta DK: Dynamic stabilization devices
in the treatment of low back pain. Neurol India. 53:466–474. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shono Y, Kaneda K, Abumi K, McAfee PC and
Cunningham BW: Stability of posterior spinal instrumentation and
its effects on adjacent motion segments in the lumbosacral spine.
Spine (Phila Pa 1976). 23:1550–1558. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Meyers KN, Campbell DA, Lipman JD, et al:
Dynamics of an intervertebral disc prosthesis in human cadaveric
spines. HSS J. 3:164–168. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ha SK, Kim SH, Kim DH, Park JY, Lim DJ and
Lee SK: Biomechanical study of lumbar spinal arthroplasty with a
semi-constrained artificial disc (Activ L) in the human cadaveric
spine. J Korean Neurosurg Soc. 45:169–175. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Austen S, Punt IM, Cleutjens JP, et al:
Clinical, radiological, histological and retrieval findings of
Activ-L and Mobidisc total disc replacements: a study of two
patients. Eur Spine J. 4:S513–S520. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rohlmann A, Mann A, Zander T and Bergmann
G: Effect of an artificial disc on lumbar spine biomechanics: a
probabilistic finite element study. Eur Spine J. 18:89–97. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kim KT, Lee SH, Suk KS, Lee JH and Jeong
BO: Biomechanical changes of the lumbar segment after total disc
replacement: Charite®, Prodisc® and
Maverick® using finite element model study. J Korean
Neurosurg Soc. 47:446–453. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yao QQ, Wang LM, Gui JC, et al: Three
dimension finite element model of the earlier-period degeneration
lumbar motion segments reconstructed from CT images. Acta
Universitatis Medicinalis Nanjing. 27:1084–1087. 2007.(In
Chinese).
|
|
10
|
Goto K, Tajima N, Chosa E, et al: Effects
of lumbar spinal fusion on the other lumbar intervertebral levels
(three-dimensional finite element analysis). J Orthop Sci.
8:577–584. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yamamoto I, Panjabi MM, Crisco T and
Oxland T: Three-dimensional movements of the whole lumbar spine and
lumbosacral joint. Spine (Phila Pa 1976). 14:1256–1260. 1989.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fujiwara A, Lim TH, An HS, et al: The
effect of disc degeneration and facet joint osteoarthritis on the
segmental flexibility of the lumbar spine. Spine (Phila Pa 1976).
25:3036–3044. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Aghayev E, Röder C, Zweig T, Etter C and
Schwarzenbach O: Benchmarking in the SWISSspine registry: results
of 52 Dynardi lumbar total disc replacements compared with the data
pool of 431 other lumbar disc prostheses. Eur Spine J.
19:2190–2199. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chou WY, Hsu CJ, Chang WN and Wong CY:
Adjacent segment degeneration after lumbar spinal posterolateral
fusion with instrumentation in elderly patients. Arch Orthop Trauma
Surg. 122:39–43. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
McMillan DW, McNally DS, Garbutt G and
Adams MA: Stress distributions inside intervertebral discs: the
validity of experimental ‘stress profilometry’. Proc Inst Mech Eng.
210:81–87. 1996.PubMed/NCBI
|
|
16
|
Simpson EK, Parkinson IH, Manthey B and
Fazzalari NL: Intervertebral disc disorganization is related to
trabecular bone architecture in the lumbar spine. J Bone Miner Res.
16:681–687. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Whitecloud TS 3rd, Castro FP Jr, Brinker
MR, Hartzog CW Jr, Ricciardi JE and Hill C: Degenerative conditions
of the lumbar spine treated with intervertebral titanium cages and
posterior instrumentation for circumferential fusion. J Spinal
Disord. 11:479–486. 1998.
|
|
18
|
Schmidt R, Obertacke U, Nothwang J, et al:
The impact of implantation technique on frontal and sagittal
alignment in total lumbar disc replacement: a comparison of
anterior versus oblique implantation. Eur Spine J. 19:1534–1539.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Katsimihas M, Bailey CS, Issa K, et al:
Prospective clinical and radiographic results of CHARITÉ III
artificial total disc arthroplasty at 2- to 7-year follow-up: a
Canadian experience. Can J Surg. 53:408–4145. 2010.
|
|
20
|
Vicars R, Hyde PJ, Brown TD, et al: The
effect of anterior-posterior shear load on the wear of ProDisc-L
TDR. Eur Spine J. 19:1356–1362. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Schmidt H, Midderhoff S, Adkins K and
Wilke HJ: The effect of different design concepts in lumbar total
disc arthroplasty on the range of motion, facet joint forces and
instantaneous center of rotation of a L4–5 segment. Eur Spine J.
18:1695–1705. 2009.PubMed/NCBI
|
|
22
|
Robinson Y and Sandén B: Spine imaging
after lumbar disc replacement: pitfalls and current
recommendations. Patient Saf Surg. 3:152009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Berg S, Tullberg T, Branth B, Olerud C and
Tropp H: Total disc replacement compared to lumbar fusion: a
randomised controlled trial with 2-year follow-up. Eur Spine J.
18:1512–1519. 2009.PubMed/NCBI
|
|
24
|
Sasso RC, Foulk DM and Hahn M:
Prospective, randomized trial of metal-on-metal artificial lumbar
disc replacement: initial results for treatment of discogenic pain.
Spine (Phila Pa 1976). 33:123–131. 2008. View Article : Google Scholar
|
|
25
|
Nie WZ, Zhang XA and Wang CT: Biomechanics
Research on Artificial Disk of Maverick. Beijing Biomedical
Engineering. 28:4–7. 2009.(In Chinese).
|
|
26
|
Valdevit A and Errico TJ: Design and
evaluation of the FlexiCore metal-on-metal intervertebral disc
prosthesis. Spine J. 4:276S–288S. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yue JJ, Bertagnoli R, McAfee PC and An HS:
Motion Preservation Surgery of the Spine. 1st edition. Elsevier;
Philadelphia, PA: pp. 25–28. 2008
|
|
28
|
Nie L, Hou Y and Cheng L: Spinal motor
function reconstruction surgery-spinal non-fusion theory and
surgical techniques. Shandong Science and Technology Press; Jinan:
pp. 91–95. 2008, (In Chinese).
|
|
29
|
Nie L, Hou Y and Cheng L: Spinal motor
function reconstruction surgery-spinal non-fusion theory and
surgical techniques. Shandong Science and Technology Press; Jinan:
pp. 84–91. 2008, (In Chinese).
|
|
30
|
McNally D, Naylor J and Johnson S: An in
vitro biomechanical comparison of Cadisc™-L with natural lumbar
discs in axial compression and sagittal flexion. Eur Spine J.
21(Suppl 5): S612–S617. 2012.PubMed/NCBI
|
|
31
|
Yue JJ, Bertagnoli R, McAfee PC and An HS:
Chapter 3. Motion Preservation Surgery of the Spine. 1st edition.
Elsevier; Philadelphia, PA: pp. 29–31. 2008
|
|
32
|
Moumene M and Geisler FH: Comparison of
biomechanical function at ideal and varied surgical placement for
two lumbar artificial disc implant designs: mobile-core versus
fixed-core. Spine (Phila Pa 1976). 32:1840–1851. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Rohlmann A, Mann A, Zander T and Bergmann
G: Effect of an artificial disc on lumbar spine biomechanics: a
probabilistic finite element study. Eur Spine J. 18:89–97. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Zhong ZC, Wei SH, Wang JP, Feng CK, Chen
CS and Yu CH: Finite element analysis of the lumbar spine with a
new cage using a topology optimization method. Med Eng Phys.
28:90–98. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Zhong ZC, Wei SH, Wang JP, Feng CK, Chen
CS and Yu CH: Finite element analysis of the lumbar spine with a
new cage using a topology optimization method. Med Eng Phys.
28:90–98. 2006. View Article : Google Scholar : PubMed/NCBI
|