Introduction
Candida glabrata infection following total
hip arthroplasty is a potentially devastating complication. If
identified late, removal of the prosthesis and a course of
appropriate systemic antifungal therapy are required. In knee or
hip arthropalsty surgery, there are comparatively higher risk of
infection than with smaller joints, due to the longer operation
time and the low blood flow. Only when the symptom period for the
patient was a short-time span, it is reasonable to leave the
prosthesis in the patient and use debridement to remove the
infection (1). The present study
reports a case of Candida glabrata infection that arose
under the incision following a total hip arthroplasty, in which
removal of the prosthesis was avoided. To the best of our
knowledge, this is the first report of a case of Candida
glabrata infection around an incision in which the prosthesis
has been preserved.
Case report
A 44-year-old male patient underwent a bilateral
total hip arthroplasty due to osteonecrosis of the femoral head in
a two-stage surgery. During the first stage, the patient underwent
the left total hip arthroplasty. Prior to receiving the right total
hip arthroplasty, light subcutaneous swelling and redness was
identified at the distal incision on the left side. The patient
exhibited no symptoms of prosthetic loosening or infection, such as
fever, chills, start-up pain or pain at rest. A probable infection
around the incision was suspected. A one-month course of vancomycin
was administered intravenously to the patient. Following this, the
swelling had disappeared and the patient received the right total
hip arthroplasty. However, 2 months later, the patient presented to
the West China Hospital (Chengdu, China) with a 20 day-history of
subcutaneous swelling of the left side distal incision. The patient
continued to exhibit no common symptoms of joint infection and the
active range of motion was normal. Other clinical findings included
elevated inflammation markers, including a C-reactive protein (CRP)
level of 22 mg/l (normal value, <5 mg/l) and an erythrocyte
sedimentation rate (ESR) of 44 mm/h (normal value, <21 mm/h).
Ultrasound confirmed the presence of a cyst that was not connected
with the articular cavity. The patient was diagnosed with a
superficial infection and the debridement of soft tissues was
performed. Intraoperatively, it was noted that the contents of the
cyst resembled tuberculosis (Fig.
1). Postoperatively, the patient was administered isoniazid and
rifapentine while awaiting a microbiology report. The results of
the report showed that Candida glabrata was present. The
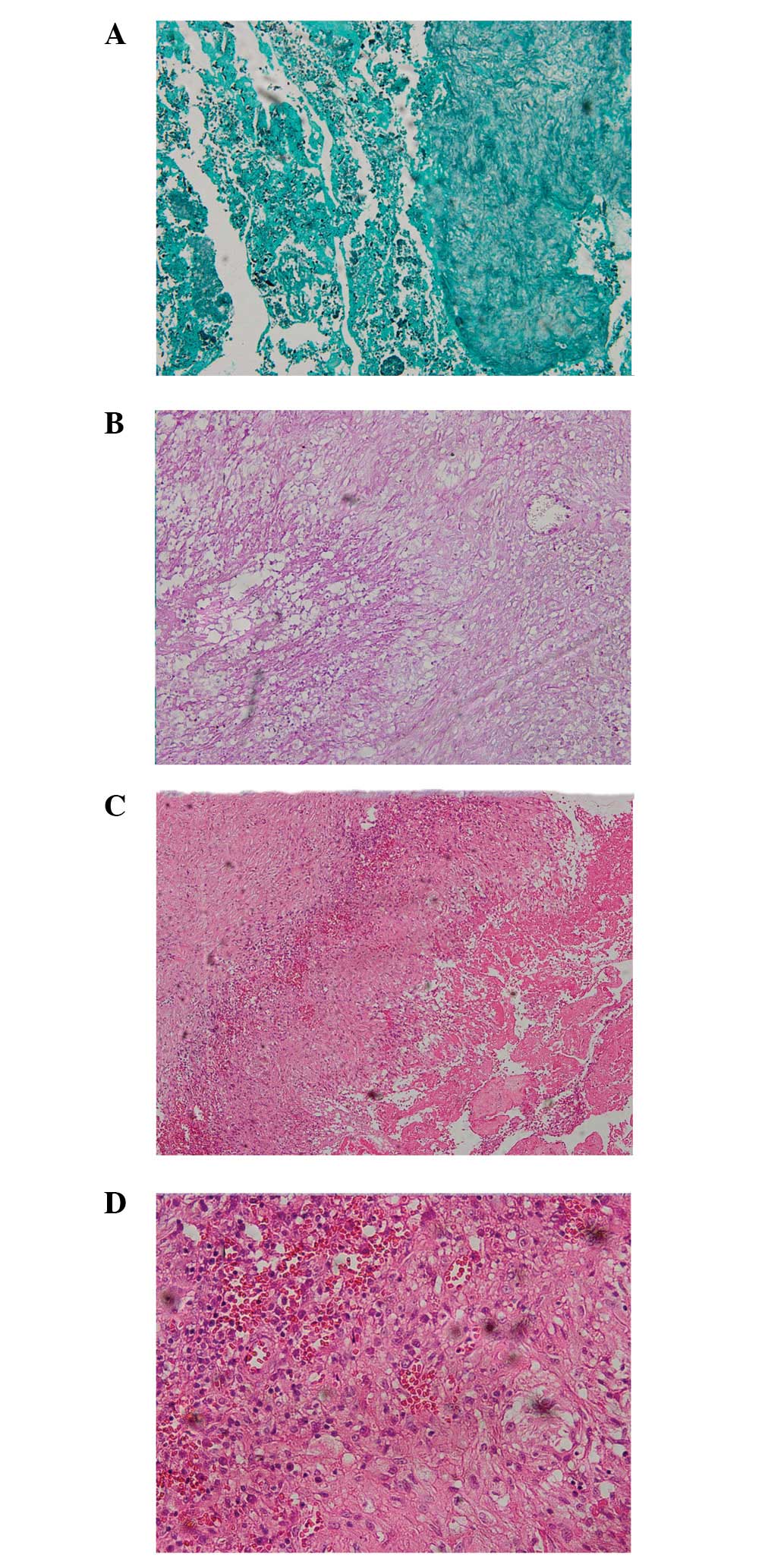
pathological section of the specimen revealed fungal infection and
chronic inflammation (Fig. 2).
Methenamine silver staining showed black Candida, PAS staining
showed purple Candida and H&E staining showed edema tissue and
inflammatory cell infiltration. The Candida glabrata isolate
showed susceptibility to itraconazole [minimum inhibitory
concentration (MIC), 2 μg/ml], amphotericin B (MIC, 0.5 μg/ml),
5-fluorocytosine (MIC, 4 μg/ml), fluconazole (MIC, 8 μg/ml) and
voriconazole (MIC, 1 μg/ml). The patient was initially administered
intravenous amphotericin B in escalating doses. When the dosage of
amphotericin B was increased up to 1 mg/kg per day, the patient
refused to continue receiving amphotericin B due to severe
gastrointestinal reactions. Consequently, the patient was switched
to voriconazole. The patient tolerated the 6-week course of
antifungal treatment without any adverse events, and the CRP level
and ESR returned to normal. The redness and swelling at the distal
operative site disappeared. Aspiration of the hip was also
negative. At the 3 month follow-up the patient did not exhibit
swelling and the range of motion of the left hip was normal.
Imageological examination showed no signs of prosthetic-loosening
or infection (Fig. 3).
Discussion
Candida glabrata infection following total
hip arthroplasty is a potentially devastating complication.
Moreover, in the absence of standardized clinical and
evidence-based guidelines, it is difficult to manage. Candida
glabrata has been historically considered as a relatively
nonpathogenic saprophyte and rarely causes serious infection in
humans. However, with widespread use of immunosuppressive drugs,
broad-spectrum antibiotics and azole antifungals, Candida
glabrata is now more frequently isolated from clinical
specimens (2). There are three
possible etiologies of Candida glabrata infection. These
include direct seeding via trauma, iatrogenic causes (surgery) and
hematogenous spread (3). In the
present case, the patient had a medical history of prolonged
antibiotic treatment. However, another potential risk factor is
that the cyst was located in the muscle layer. It is assumed there
was a large amount of dead-space in the muscle layer during the
surgery. Hematoma formation may occur within this dead-space and
may disrupt blood supply to the surrounding tissue, thus preventing
antibiotic entry (4).
Routine treatment usually includes the surgical
removal of all bioprosthetic components. Early-onset infections may
be eradicated by debridement and a long course of parenteral
antibiotics. Antibiotic therapy is based on the definitive
microbiological diagnosis and the sensitivity to the antibiotics.
Generally, 6 weeks of parenteral antibiotics are recommended for
prosthetic joint infections (5).
Postoperatively, the patient did not exhibit symptoms of infection,
including fever, vomiting and groin pain. The radiograph of the
bilateral hip did not reveal the presence of any aseptic loosening
of a component of the prosthesis. Ultrasound confirmed that the
cyst was not connected with the articular cavity. The active range
of motion of the left hip was invariably normal postoperatively.
Repeated aspiration of the left hip was negative. Consequently, the
decision was made to retain the prosthesis.
The appropriate course of antibiotic treatment was
selected, based on the sensitivity of the infection to specific
antibiotic agents. The protocols for the treatment of infections
associated with hip arthroplasty, which include 6 weeks of
parenteral treatment, have been demonstrated previously (6–8). Due
to the severe gastrointestinal reactions of the patient to
amphotericin B, voriconazole was administered instead. This was the
antifungal drug to which the infection had the second highest
susceptibility in the present case. Following 6 weeks of
voriconazole treatment, normalization of CRP and ESR was
achieved.
Candida glabrata infection following total
hip arthroplasty is extremely rare. This infection is generally
asymptomatic or gives rise to mild signs of infection in the early
stages. If identified late, diffusion of the infection may result
in irreversible deformity and pain with severe osteoarticular
destruction (9). Thus, early
diagnosis and treatment are important in the management of
Candida glabrata. If there are minimal signs of infection
following arthroplasty, close co-operation between the clinician
and laboratory are required in order to identify the infectious
agent.
The present case illustrates the significance of
postoperative follow-up and the experience of the clinician. If a
patient presents abnormal symptoms without signs of common
infection following hip arthroplasty, the possibility of a fungal
infection should be considered.
References
|
1
|
Tattevin P, Crémieux AC, Pottier P, Huten
D and Carbon C: Prosthetic joint infection: when can prosthesis
salvage be considered? Clin Infect Dis. 29:292–295. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fidel PL Jr, Vazquez JA and Sobel JD:
Candida glabrata: review of epidemiology, pathogenesis, and
clinical disease with comparison to C. albicans. Clin Microbiol
Rev. 12:80–96. 1999.PubMed/NCBI
|
|
3
|
Gaston G and Ogden J: Candida glabrata
periprosthetic infection: a case report and literature review. J
Arthroplasty. 19:927–930. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hall RL, Frost RM, Vasukutty NL, et al:
Candida glabrata: an unusual fungal infection following a total hip
replacement. BMJ Case Reports. 2012.2012:
|
|
5
|
Goldenberg DL: Septic arthritis. Lancet.
351:197–202. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Masterson EL, Masri BA and Duncan CP:
Instructional Course Lectures, The American Academy of Orthopaedic
Surgeons - Treatment of infection at the site of total hip
replacement. J Bone Joint Surg. 79:1740–9. 1997.
|
|
7
|
Hanssen AD and Rand JA: Instructional
Course Lectures, The American Academy of Orthopaedic Surgeons -
Evaluation and treatment of infection at the site of a total hip or
knee arthroplasty. J Bone Joint Surg Am. 80:910–22. 1998.
|
|
8
|
McDonald DJ, Fitzgerald RH Jr and Ilstrup
DM: Two-stage reconstruction of a total hip arthroplasty because of
infection. J Bone Joint Surg Am. 71:828–834. 1989.PubMed/NCBI
|
|
9
|
Kauffman CA: Fungal infections. Proc Am
Thorac Soc. 3:35–40. 2006. View Article : Google Scholar
|