Introduction
Benign tracheobronchial obstructions, arising from
trauma or tumours, result in a persistent cough, asthma-like
wheezing, dyspnea and ventilatory failure. These obstructions
significantly affect quality of life and therefore, appropriate
treatment is required. Although the successful treatment of
tracheal stenosis using steroid regimens has been demonstrated
(1), the mainstay of treatment for
symptomatic lesions is surgery, including sleeve resection
(2,3), however this is not without risk to
the patient. Interventional bronchology techniques, including argon
plasma coagulation (APC), cryotherapy, tracheal dilation and
stenting, are widely employed as effective treatments for patients
with central airway obstruction or less serious lesions (4,5). The
choice of therapy depends on tumour size, pathology, wall invasion
depth, anatomical location, degree of symptoms, patient
co-morbidities and operator experience and expertise (6). However, the occurrence of repeated
stenosis is relatively frequent, which is the principal long-term
problem of interventional bronchology techniques (7).
Case report
A 36-year-old male was admitted to Daping Hospital
(Chongqing, China) following a workplace accident. A chest
radiograph exhibited multiple rib fractures and lung contusions.
The patient underwent surgery and was readmitted to hospital one
month later due to difficulty breathing. The patient had no history
of chronic lung disease or cyanosis and no related medical history.
This study was conducted in accordance with the declaration of
Helsinki and was approved by the Ethics Committee of the Third
Military Medical University (Chonqing, China). The participant
provided written informed consent for involvement in this
study.
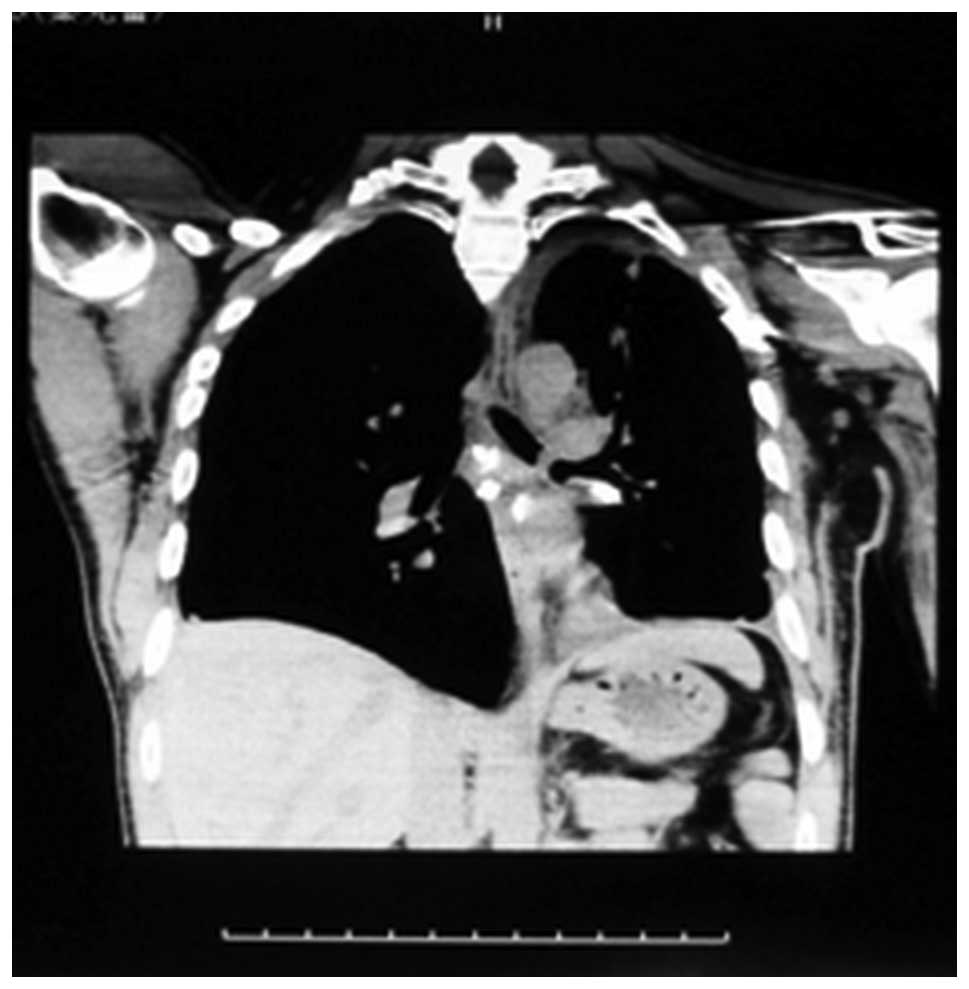
A physical examination revealed reduced breath
sounds and mild wheezing in the left zone. A computed axial
tomography angiogram of the chest demonstrated total occlusion of
the left mainstem bronchus due to a soft tissue mass and
atelectasis of the left upper lobe (Fig. 1). The vocal cords, trachea, carina
and right bronchial tree were observed to be normal and flexible
bronchoscopy was performed. A pedicle neoplasm with complete
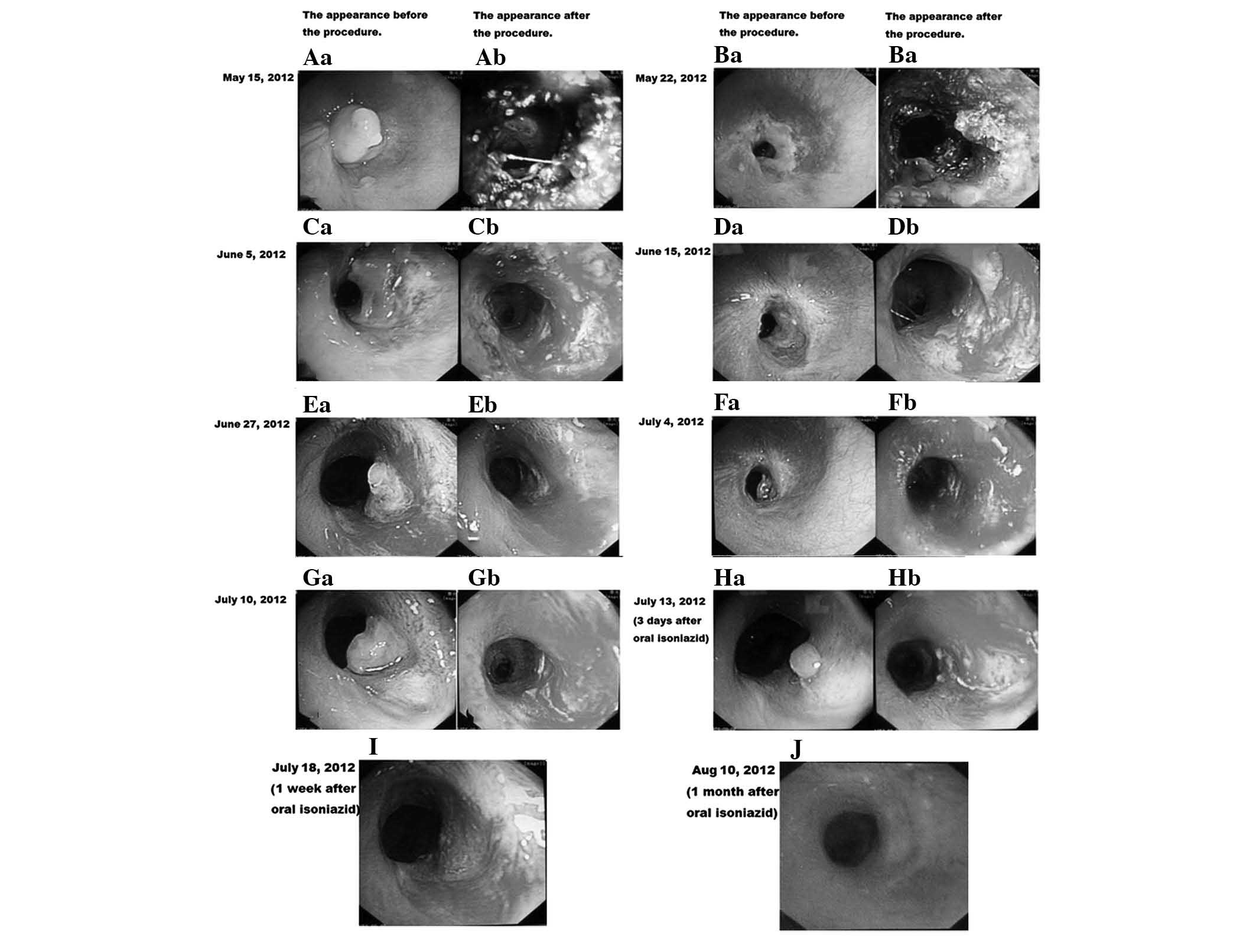
occlusion of the left mainstem bronchus was confirmed (Fig. 2Aa). The neoplasm was biopsied and
the specimen was sent for histological examination, revealing
inflammatory infiltration and fibrosis.
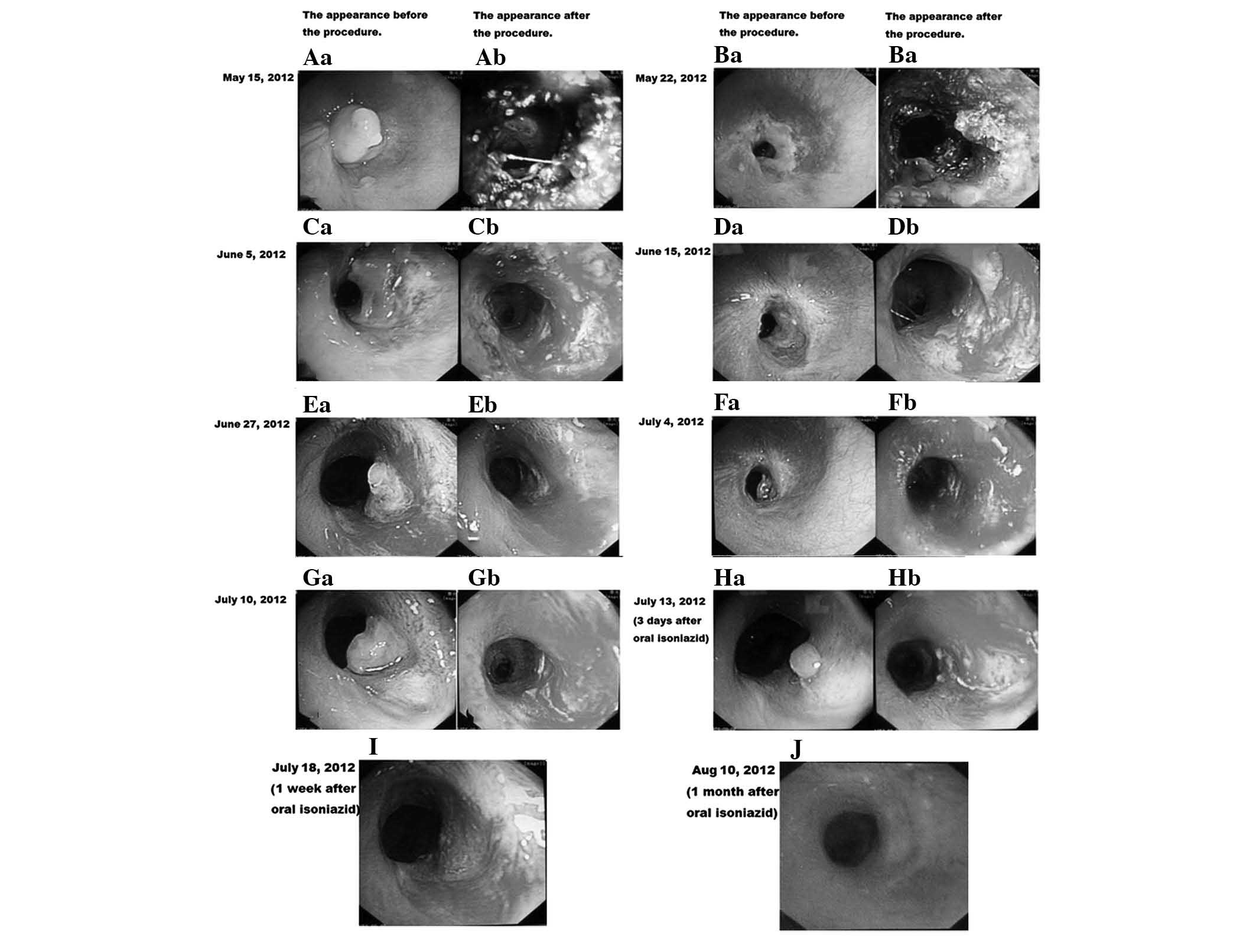 | Figure 2(Aa) A pedicle neoplasm with complete
occlusion of the left mainstem bronchus prior to the procedure.
(Ba, Bb, Ca, Cb, Da, Db, Ea, Eb, Fa, Fb, Ga and Gb) The left
mainstem bronchus was narrowed by fibrous tissue obscuring the
stent following repetitive procedures. (Ha, Hb, I and J) Restenosis
was repressed following administration of oral isoniazid. |
Rigid forceps were initially used to remove the
granulation tissue in order to avoid surgery and produce rapid
palliation of dyspnea. However, 70% of the airway remained
obstructed due to the residual granulation tissue. Thus, APC and
cryotherapy were utilised to devitalise and remove the residual
granulation tissue surrounding the stenosis. This intervention
reopened the obstructed left mainstem bronchus (Fig. 2Ab) and residual stenosis was
estimated to be <20%. The procedure took 60 min.
One week later, the dyspnea symptoms reappeared and
stenosis of the left mainstem bronchus was observed. APC and
cryotherapy were performed 15 times as the left mainstem bronchus
narrowed due to fibrous tissue obscuring the stent (Fig. 2Ba, Bb, Ca, Cb, Da, Db, Ea, Eb, Fa, Fb,
Ga and Gb). By following related previous studies (8,9),
isoniazid may regulated collagen deposition by inhibiting lysyl
oxidase (LOX), so it was possible to avoid repeated and prolonged
application of bronchoscopy with isoniazid. Oral isoniazid (~0.3g)
(Shanghai Xinyi Pharmaceutical Co., Ltd., Shanghai, China) was
administered once daily, prior to breakfast, for two weeks. On the
third day, flexible bronchoscopy revealed a small granulation
nodule on the sidewall of the trachea; this was frozen and removed
by cryotherapy (Fig. 2Ha and Hb).
Repeat flexible bronchoscopy was performed one week and one month
following oral isoniazid administration (Fig. 2I and J). No recurrence of bronchial
stenosis was observed. In addition, isoniazid appeared to be safe
and did not result in any detectable liver lesions or renal damage.
The patient was followed up for one year and no tracheal narrowing
was observed.
Discussion
Benign tracheobronchial obstruction in adults
commonly result from tracheotomy procedures, intubation trauma or
following blunt chest trauma (10). Additional causes include severe
inflammation, autoimmune disorders and inhalation injuries.
Tracheobronchial stenosis, arising from benign or malignant
diseases, is often associated with dyspnea, ventilatory failure and
obstructive pneumonia. If hypertrophic and keloid scarring are not
actively treated they may lead to more serious stenosis or
obstruction. Segmental and lobar atelectasis may emerge and result
in suffocation due to airway obstruction. Bobocea et
al(3) hypothesised that
bronchial rupture as a result of blunt chest trauma (involving
chest wall compression, traction on the carina and the sudden
increase in intraluminal pressure) leads to granulation tissue
formation that may result in progressive bronchial obstruction with
distal infection and permanent parenchymal damage.
The optimal treatment for tracheobronchial
obstructions remains undefined. Previously, patients with central
airway obstructions were managed by surgery; however, for
tracheobronchial obstruction, surgery is complex and may be
traumatic (11). Furthermore,
numerous patients are unsuitable for surgery as a result of poor
lung function. In addition, specific patients may be affected by
recurrent stenosis due to scarring and granulation tissues at the
surgical site (12). With the
development of interventional pulmonology in the last 20 years,
interventional bronchology techniques, including
neodymium-yttrium-aluminium-garnet laser irradiation,
electrocautery, APC, cryotherapy, tracheal dilatation and airway
stenting (10,13) allow for palliative techniques that
alleviate central airway obstruction (14). As a single method is not able to
solve all clinical issues, various interventional modalities are
frequently combined to reduce complications and enhance the
duration of the treatment effect (15). The choice of therapy is often
dependent on the preference of the physician and local
resources.
Management of a left bronchial obstruction malignant
lesion using a combination of therapies, including APC with
cryotherapy, was observed in this case study. APC produces a
discontinuous current between the probe and tissue by iodinating
argon, which exhibits a homeostatic effect. Cryotherapy freezes and
leads to necrosis of the neoplasm, does not induce hypoxemia,
lowers the risk of perforation, is not flammable and does not
produce fumes. APC combined with cryotherapy, as applied in this
case, rapidly reopened the occluded airway, reduced surgical
duration and prevented severe haemorrhaging (16). However, the repeated stenosis of
the opened airway due to scarring and subepithelial fibrosis was
problematic, thus, oral isoniazid was administered for two weeks as
a fibroblast inhibitor. No granulation or scar tissue was observed
one month and one year following the procedure. Furthermore no
adverse reactions were observed suggesting that isoniazid therapy
is safe.
Previous studies have revealed that mitomycin,
corticosteroid and 5-fluorouracil also reduce the recurrence rate
of stenosis (17,18). However, these drugs are complex to
administer in clinical applications due to significant toxicity,
including myelosuppression. Carrington et al(8) observed that isoniazid was capable of
inhibiting LOX by competing for its obligatory cofactor, pyridoxal
phosphate, and thus, regulated collagen deposition. Udupa (19) observed that isoniazid inhibits LOX
activity and decreases tensile strength and collagen content. In
addition, Udupa previously reported that isoniazid decreases the
mechanical strength of collagen by inhibiting LOX and interfering
with electrostatic interactions between collagen and the ground
substance; which is important in wound healing and scar formation.
Isoniazid has been shown to be a potent inhibitor of human
fibroblasts at a concentration of 3 mg/kg and has been administered
successfully in patients with lesions exhibiting a delayed healing
process (20). Further studies are
required to determine whether isoniazid suppresses granulation and
scar tissue formation. This case study presents a novel potential
application of isoniazid, however further investigation is required
to demonstrate the importance of using isoniazid.
In conclusion, isoniazid reduces granulation tissue
and prevents recurrent stenosis. However, further randomised
control studies are required to investigate the possibility of
interventional bronchology techniques combined with isoniazid
treatment for the management of tracheobronchial obstructions. The
administration of isoniazid may abate the requirement for
repetitive bronchoscopies and invasive reconstructive surgery.
References
|
1
|
Braidy J, Breton G and Clément L: Effect
of corticosteroids on post-intubation tracheal stenosis. Thorax.
44:753–755. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kleiss IJ, Verhagen AF, Honings J,
Schuurbiers OC, van der Heijden HF and Marres HA: Tracheal surgery
for benign tracheal stenosis: Our experience in sixty-three
patients. Clin Otolaryngol. 38:343–347. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bobocea AC, Matache R, Codreşi M, Bolca C
and Cordoş I: Sleeve resection of right main bronchus for
posttraumatic bronchial stenosis. Pneumologia. 60:225–228. 2011.(In
Romanian).
|
|
4
|
Du Rand IA, Barber PV, Goldring J, et al:
BTS Interventional Bronchoscopy Guideline Group: Summary of the
British Thoracic Society guidelines for advanced diagnostic and
therapeutic flexible bronchoscopy in adults. Thorax. 66:1014–1015.
2011.
|
|
5
|
Gao H, Ding X, Wei D, Cheng P, Su X, Liu H
and Zhang T: Endoscopic management of benign tracheobronchial
tumors. J Thorac Dis. 3:255–261. 2011.PubMed/NCBI
|
|
6
|
Alazemi S, Lunn W, Majid A, et al:
Outcomes, health-care resources use, and costs of endoscopic
removal of metallic airway stents. Chest. 138:350–356.
2010.PubMed/NCBI
|
|
7
|
Jeong BH, Um SW, Suh GY, Chung MP, Kwon
OJ, Kim H and Kim J: Results of interventional bronchoscopy in the
management of postoperative tracheobronchial stenosis. J Thorac
Cardiovasc Surg. 144:217–222. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Carrington MJ, Bird TA and Levene CI: The
inhibition of lysyl oxidase in vivo by isoniazid and its reversal
by pyridoxal. Effect on collagen cross-linking in the chick embryo.
Biochem J. 221:837–843. 1984.PubMed/NCBI
|
|
9
|
Weinreich J, Agren MS, Bilali E, Kleinman
HK, Coerper S, Königsrainer A and Beckert S: Effects of isoniazid
and niacin on experimental wound-healing. Surgery. 147:780–788.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gompelmann D, Eberhardt R and Herth FJ:
Interventional pulmonology procedures: an update. Panminerva Med.
55:121–129. 2013.PubMed/NCBI
|
|
11
|
Thistlethwaite PA, Renner J, Duhamel D,
Makani S, Lin GY, Jamieson SW and Harrell J: Surgical management of
endobronchial inflammatory myofibroblastic tumors. Ann Thorac Surg.
91:367–372. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Shiraishi T, Yanagisawa J, Higuchi T, et
al: Tracheal resection for malignant and benign diseases: surgical
results and perioperative considerations. Surg Today. 41:490–495.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Oki M and Saka H: Double Y-stenting for
tracheobronchial stenosis. Eur Respir J. 40:1483–1488. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Casal RF, Iribarren J, Eapen G, et al:
Safety and effectiveness of microdebrider bronchoscopy for the
management of central airway obstruction. Respirology.
18:1011–1015. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ernst A, Feller-Kopman D, Becker HD and
Mehta AC: Central airway obstruction. Am J Respir Crit Care Med.
169:1278–1297. 2004. View Article : Google Scholar
|
|
16
|
Schumann C, Hetzel M, Babiak AJ, et al:
Endobronchial tumor debulking with a flexible cryoprobe for
immediate treatment of malignant stenosis. J Thorac Cardiovasc
Surg. 139:997–1000. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Garg M, Gogia P, Manoria P and Goyal R:
Bronchoscopic management of benign bronchial stenosis by
electrocautery and balloon dilatation. Indian J Chest Dis Allied
Sci. 54:41–43. 2012.PubMed/NCBI
|
|
18
|
Guven M, Turan F, Eyibilen A, Akbaş A and
Erkorkmaz Ü: A comparison of the efficacy of
5-fluorouracil/triamcinolone, carnitine and dexamethasone therapy
on wound healing in tracheal injury: potential for preventing
tracheal stenosis? Eur Arch Otorhinolaryngol. 269:201–206. 2012.
View Article : Google Scholar
|
|
19
|
Udupa SL: Inhibition of lysyl oxidase by
isoniazid and its effect on wound healing. Indian J Exp Biol.
33:278–280. 1995.PubMed/NCBI
|
|
20
|
Martyn JW and Campbell HH: Isoniazid and
wound healing. Can Med Assoc J. 88:229–233. 1963.PubMed/NCBI
|