Introduction
Chronic obstructive pulmonary disease (COPD) is a
major cause of chronic morbidity and mortality and is predicted to
be the third leading cause of mortality worldwide by the year 2020
(1). The most significant risk
factor for COPD is cigarette smoking, and for a long time COPD was
considered as a consequence of local damage to small airways.
However, epidemiological studies have shown that the levels of a
serum marker of inflammation, C-reactive protein (CRP), are higher
in patients with stable COPD than in healthy controls (2,3). In
addition, CRP has been reported as a strong and independent
predictor of future outcomes in individuals with COPD (4). Although the hallmark feature of COPD
is airflow obstruction, it is poorly predicted by forced expiratory
volume in the first second (FEV1) only (5,6). As
CRP assays are inexpensive and convenient, CRP levels may be one of
the most valuable predictors of outcomes in stable COPD patients.
However, currently, CRP levels are usually only determined if an
exacerbation of COPD is suspected. The patients included in other
specific studies were in the acute exacerbations phase of COPD
(7–9). In addition, the association between
CRP and mortality in COPD patients remains conflicting rather than
conclusive (10–13). It was on this background that the
present study was conducted, which aimed to examine whether CRP
levels in patients with stable COPD are a significant predictor of
prognosis following adjustment for specific prognostic factors.
Materials and methods
Patients
The prospective cohort study included a total of 116
patients that had been diagnosed with COPD ≥6 months previously and
had been under treatment for ≥6 months. A diagnosis of COPD was
based on medical history, current symptoms and available pulmonary
function tests following Global Initiative for Chronic Obstructive
Lung Disease guidelines (14). To
exclude patients with asthma, subjects with a history of allergic
rhinitis or an improvement in FEV1 of >12% from the
predicted values following inhalation of a bronchodilator, were not
included. Patients with evidence of extensive pulmonary
tuberculosis, malignancy or who were suffering from psychosis were
excluded from the study. All patients with COPD were clinically
stable and none had a history of respiratory infection for at least
a 4-week period preceding the study. Approval for this study was
obtained from the Institutional Review Board for Human Studies of
Affiliated Hospital, School of Medicine, Ningbo University (Ningbo,
China) and informed consent was obtained from all participating
subjects.
CRP measurement
Fasting blood samples were obtained from the
patients whilst at rest, prior to any other test being performed.
Serum CRP levels were measured by high sensitivity
immunoturbidimetry (Beckman Coulter, Inc., Miami, FL, USA). The
results were given in units of mg/l and the analytical sensitivity
of this analysis was 0.1 mg/l. The cutoff point for the CRP
concentration was 3 mg/l, as indicated in previous studies
(10,11,15).
Follow-up
The study was conducted between August 2009 and
April 2012, with a follow-up of 32 months or until patient
mortality. The follow-up was carried out by telephoning the
patients or their next of kin and/or checking hospital records.
Critical events were recorded by the physicians in charge of the
follow-ups. Subjects who were not located at follow-up and were not
known to have succumbed to their illness were considered as
censored at the end of the study period.
Statistical Analysis
The continuous variables are presented as mean ± SD
and the categorical variables are presented as absolute numbers and
percentages. Cox regression analysis was used to examine time to
COPD mortality using hazard ratios (HR) and 95% confidence
intervals (CIs). Risk measures were adjusted for age, gender,
FEV1%pred, smoking and presence of disease. Kaplan-Meier
mortality curves were created to exhibit differences in mortality
by selected risk factors. Quantitative synthesis of all relevant
studies was performed and the methods used have been described in
detail in previous studies (16,17).
The HRs of time-to-event data were directly extracted from the
original study or were read off survival curves to estimate the
logHR and its variance, as suggested by Parmar et
al(18). The statistical
analyses were performed using SPSS, version 13.0 (SPSS, Inc.,
Chicago, IL, USA) and Review Manager 5.0.17 (Cochrane Library
Software, Oxford, UK). Two-tailed P<0.05 was considered to
indicate a statistically significant difference.
Results
A total of 116 consecutive COPD patients (including
75 males) were recruited into the study, as well as 35 healthy
subjects (including 18 males) aged over 50 years, with no evidence
of COPD. The healthy subjects were randomly selected from a
population sample of subjects living in the same area as the
patients.
The characteristics of the COPD patients are
summarized in Table I. The
majority of patients were elderly with a mean age of 71 years
(range, 47–91 years) and over half were male (65%). A number of the
patients had comorbid illnesses, including hypertension, diabetes
mellitus, chronic gastritis, cataract and coronary heart disease.
The healthy controls were matched to the COPD patients with respect
to age, gender, body mass index (BMI) and smoking status. No
significant differences were observed in these parameters between
the healthy controls and COPD patients. However, serum CRP levels
were significantly higher in the stable COPD patients than in the
control subjects (4.48±0.83 vs. 1.01±0.27 mg/l, respectively;
P<0.05).
 | Table IBaseline characteristics of the study
participants. |
Table I
Baseline characteristics of the study
participants.
| Characteristics | COPD patients
n=116 | Healthy controls
n=35 | P-value |
|---|
| Gender | | | 0.16 |
| Male | 75 | 18 | |
| Female | 41 | 17 | |
| Age, years | 71.0±9.0 | 68.9±5.1 | 0.09 |
| BMI,
kg/m2 | 24.6±3.2 | 25.8±5.7 | 0.12 |
| Smoking status | | | 0.13 |
| Current smoker | 46 | 14 | |
| Ex-smoker | 34 | 5 | |
| Never | 36 | 16 | |
| FEV1, %
predicted | 44.7±12.1 | 90.4±6.8 | <0.001 |
| Inhaled steroid,
% | 61.2 | | |
|
β2-agonist, % | 61.2 | | |
| Inhaled ipratropium,
% | 53.4 | | |
| Theophylline, % | 36.2 | | |
| Comorbid illnesses,
n | | | |
| 0 | 36 | | |
| 1 | 52 | | |
| 2 | 15 | | |
| 3 | 10 | | |
| 4 | 3 | | |
| CRP, mg/l | 4.48±0.83 | 1.01±0.27 | 0.025 |
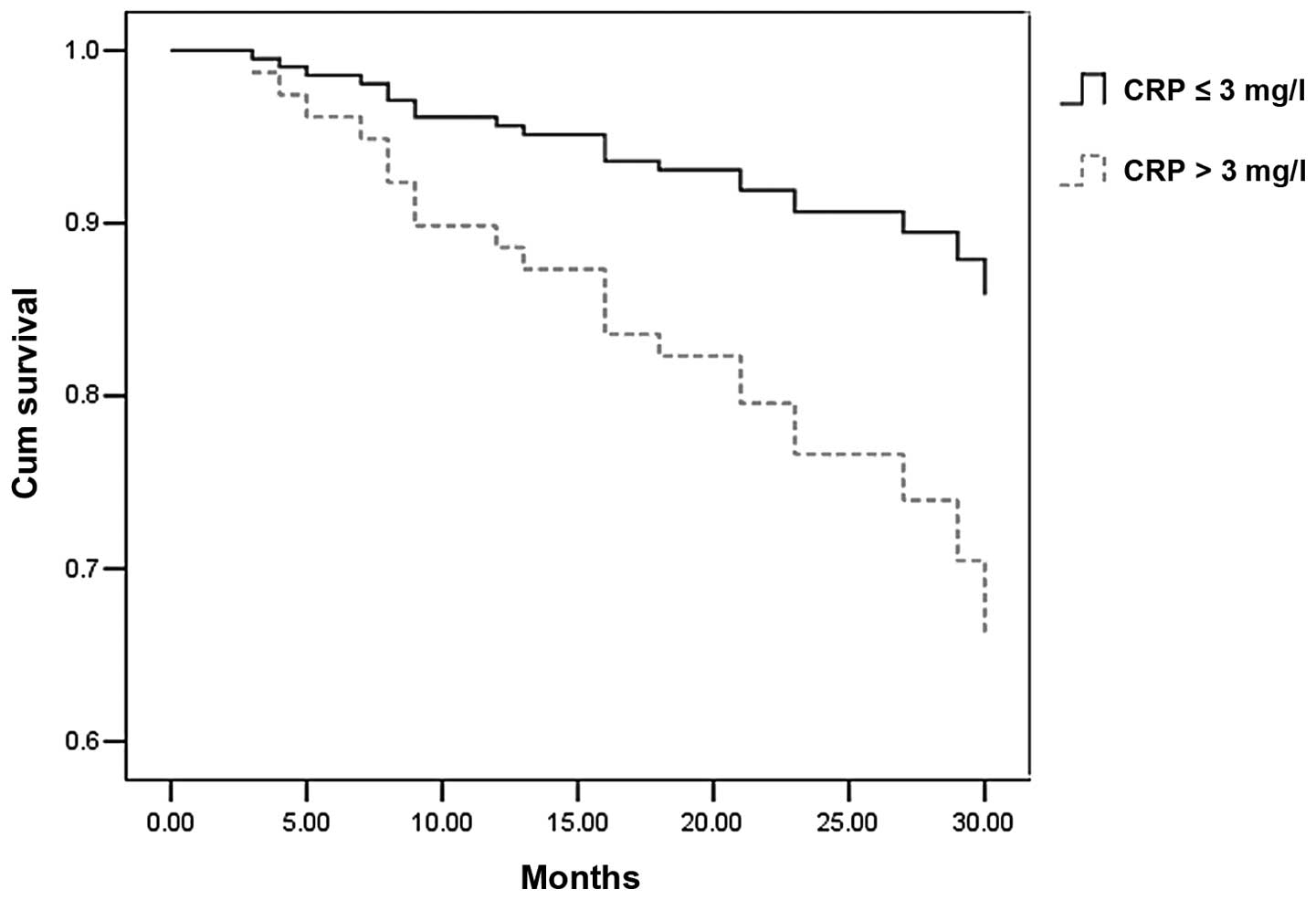
At the end of follow-up, 21 patients had succumbed
(18%). However, information concerning the cause of mortality of
four patients was not available since contact details had been
changed or through lack of cooperation from the patients’ families.
When CRP ≤3 mg/l was used as the reference category, values >3
mg/l were associated with increased mortality (HR, 2.71; 95% CI,
1.05–6.99; P<0.05). Kaplan-Meier survival curves for all-cause
mortality, according to CRP categories, are shown in Fig. 1. The clinical parameters between
survivors and nonsurvivors were also compared. Compared with
survivors, non-survivors had a high degree of airflow obstruction
(FEV1% pred, 40.5±17.9 vs. 54.6±18.0, respectively;
P<0.05) and CRP concentration (7.56±5.18 vs. 3.48±6.55 mg/l,
respectively; P<0.05). However, no significant difference in
age, gender and BMI was observed between the two groups.
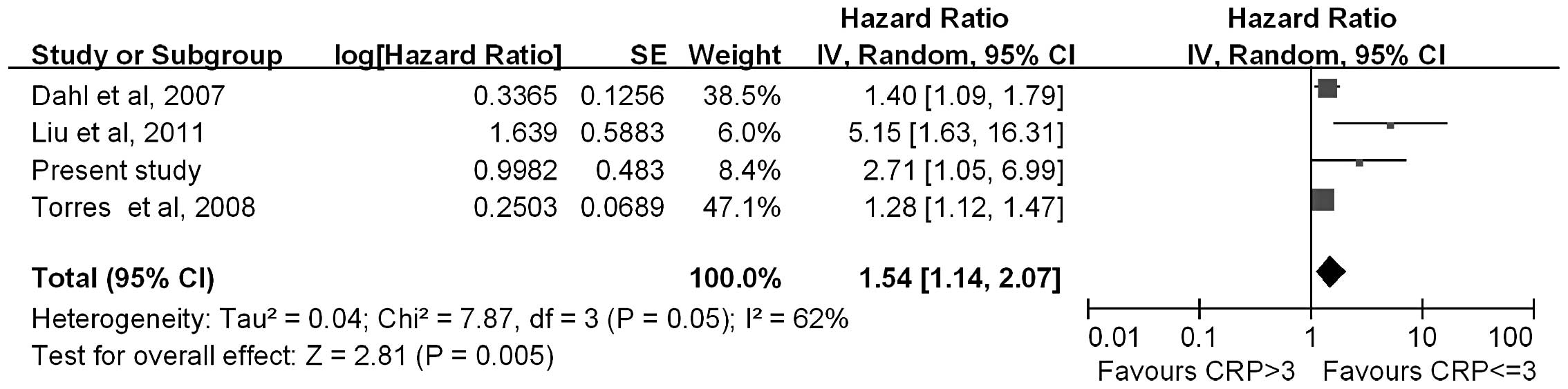
In addition, a quantitative synthesis of four
studies, comprising the current study and three published studies,
was performed (10,11,15).
Among these studies, the median duration of the follow-ups ranged
between 3 and 10 years. Risk measures were frequently adjusted for
age, gender, FEV1%pred and smoking. As shown in Fig. 2, the HR of mortality in patients
with a CRP >3 mg/l was 1.54 (95% CI, 1.14–2.07) compared with
those with CRP ≤3 mg/l.
Discussion
The present study was performed to evaluate whether
circulating CRP levels are a biomarker of systemic inflammation and
a significant predictor of future COPD outcomes. In this study,
serum CRP levels were found to be significantly higher in stable
COPD patients than in well-matched healthy control subjects. The
results obtained are consistent with previous studies, indicating
the presence of systemic inflammation in patients with stable COPD
(2,3).
A number of independent predictors of future COPD
outcomes have been identified previously, including exercise
capacity (19), biomarkers of
systemic inflammation (20), BMI
(21,22), smoking status (23), severity of dyspnea (24), FEV1(5) and PaO2(23). Among these, the best studied and
most convenient to evaluate is serum CRP levels.
The present study showed that increased serum CRP
levels are a strong predictor of COPD mortality. Liu et al
determined that a serum CRP concentration of >3 mg/l was a
poorer prognostic variable of COPD compared with a CRP
concentration ≤3 mg/l (11). In
the study by Dahl et al, the HR of mortality due to COPD was
2.2-fold higher in patients with a high CRP level than in those
with a low CRP level (15). The
observations in the present study are in agreement with these
studies. However, de Torres et al reported that CRP levels
are not associated with survival status (10).
Considering the inconsistent results between
previous studies, a quantitative synthesis of the evidence, using
rigorous methods, was performed. Meta-analysis was conducted on
four studies with 1,750 subjects to evaluate the association
between serum CRP levels and mortality in patients with COPD. This
meta-analysis indicated that a high level of serum CRP is
associated with an increased risk of mortality in COPD
patients.
At present, CRP levels are only determined if an
exacerbation of COPD is suspected. The results of the present study
have several implications, showing that stable COPD patients had a
higher level of CRP than healthy controls, indicating the presence
of systemic inflammation in COPD. As high sensitivity CRP assays
are inexpensive and convenient, it is important for clinicians to
use CRP values in stable COPD patients. The study also found that a
high level of serum CRP is associated with an increased risk of
mortality in COPD patients. These results indicate that selection
of serum CRP concentration as a prognostic biomarker in stable COPD
patients may be useful for physicians.
However, there were limitations in this study that
should be acknowledged. Firstly, although the patients were
clinically stable, serum CRP concentration may fluctuate slightly
over time, which may affect the validity of CRP levels as a
predictor marker. Secondly, various drugs and treatments among
patients appear to have an unpredictable effect on serum CRP
concentration.
In conclusion, the present study confirms that
circulating CRP levels are higher in stable COPD patients than in
healthy individuals and are a significant long-term predictor of
future COPD outcomes in individuals with airway obstruction. These
observations highlight the significance of high sensitivity CRP
assays in patients with stable COPD.
Acknowledgements
This study was partly supported by grants from the
Social Development Science and Technology Project (no. 2011C50025),
Natural Science Foundation (no. 2012A610257) and the Social
Development Science and Technology Project of Ningbo (no.
2011C50073).
References
|
1
|
Murray CJ and Lopez AD: Mortality by cause
for eight regions of the world: Global Burden of Disease Study.
Lancet. 349:1269–1276. 1997. View Article : Google Scholar
|
|
2
|
Karadag F, Kirdar S, Karul AB and Ceylan
E: The value of C-reactive protein as a marker of systemic
inflammation in stable chronic obstructive pulmonary disease. Eur J
Intern Med. 19:104–108. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
He Z, Chen Y, Chen P, Wu G and Cai S:
Local inflammation occurs before systemic inflammation in patients
with COPD. Respirology. 15:478–484. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Man SF, Connett JE, Anthonisen NR, Wise
RA, Tashkin DP and Sin DD: C-reactive protein and mortality in mild
to moderate chronic obstructive pulmonary disease. Thorax.
61:849–853. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Waschki B, Kirsten A, Holz O, et al:
Physical activity is the strongest predictor of all-cause mortality
in patients with chronic obstructive pulmonary disease: a
prospective cohort study. Chest. 140:331–342. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Celli BR, Cote CG, Marin JM, et al: The
body-mass index, airflow obstruction, dyspnea, and exercise
capacity index in chronic obstructive pulmonary disease. N Engl J
Med. 350:1005–1012. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Stolz D, Christ-Crain M, Morgenthaler NG,
et al: Copeptin, C-reactive protein, and procalcitonin as
prognostic biomarkers in acute exacerbation of COPD. Chest.
131:1058–1067. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Murphy SA, Haja Mydin H, Fatah S and
Antunes G: Predicting end-of-life in patients with an exacerbation
of COPD by routine clinical assessment. Respir Med. 104:1668–1674.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lacoma A, Prat C, Andreo F, et al: Value
of procalcitonin, C-reactive protein, and neopterin in
exacerbations of chronic obstructive pulmonary disease. Int J Chron
Obstruct Pulmon Dis. 6:157–169. 2011.PubMed/NCBI
|
|
10
|
de Torres JP, Pinto-Plata V, Casanova C,
et al: C-reactive protein levels and survival in patients with
moderate to very severe COPD. Chest. 133:1336–1343. 2008.PubMed/NCBI
|
|
11
|
Liu SF, Wang CC, Chin CH, Chen YC and Lin
MC: High value of combined serum C-reactive protein and BODE score
for mortality prediction in patients with stable COPD. Arch
Bronconeumol. 47:427–432. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Miniati M, Monti S, Bottai M, Cocci F,
Fornai E and Lubrano V: Prognostic value of C-reactive protein in
chronic obstructive pulmonary disease. Intern Emerg Med. 6:423–430.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Man SF, Xing L, Connett JE, et al:
Circulating fibronectin to C-reactive protein ratio and mortality:
a biomarker in COPD? Eur Respir J. 32:1451–1457. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Rabe KF, Hurd S, Anzueto A, et al: Global
strategy for the diagnosis, management, and prevention of chronic
obstructive pulmonary disease: GOLD executive summary. Am J Respir
Crit Care Med. 176:532–555. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Dahl M, Vestbo J, Lange P, Bojesen SE,
Tybjaerg-Hansen A and Nordestgaard BG: C-reactive protein as a
predictor of prognosis in chronic obstructive pulmonary disease. Am
J Respir Crit Care Med. 175:250–255. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cao C, Fang JJ, Ying T, et al: Vascular
endothelial growth factor +936C/T and +405G/C polymorphisms and
cancer risk: a meta-analysis. Arch Med Res. 41:548–557. 2010.
|
|
17
|
Cao C, Ying T, Fang JJ, et al:
Polymorphism of vascular endothelial growth factor -2578C/A with
cancer risk: evidence from 11263 subjects. Med Oncol. 28:1169–1175.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Parmar MK, Torri V and Stewart L:
Extracting summary statistics to perform meta-analyses of the
published literature for survival endpoints. Stat Med.
17:2815–2834. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Prescott E, Almdal T, Mikkelsen KL,
Tofteng CL, Vestbo J and Lange P: Prognostic value of weight change
in chronic obstructive pulmonary disease: results from the
Copenhagen City Heart Study. Eur Respir J. 20:539–544. 2002.
View Article : Google Scholar
|
|
20
|
Schembri S, Anderson W, Morant S, et al: A
predictive model of hospitalization and death from chronic
obstructive pulmonary disease. Respir Med. 103:1461–1467. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Coxson HO, Chan IH, Mayo JR, Hlynsky J,
Nakano Y and Birmingham CL: Early emphysema in patients with
anorexia nervosa. Am J Respir Crit Care Med. 170:748–752. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Cao C, Wang R, Wang J, Bunjhoo H, Xu Y and
Xiong W: Body mass index and mortality in chronic obstructive
pulmonary disease: a meta-analysis. PLoS One. 7:e438922012.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Nizet TA, van den Elshout FJ, Heijdra YF,
van de Ven MJ, Mulder PG and Folgering HT: Survival of chronic
hypercapnic COPD patients is predicted by smoking habits,
comorbidity, and hypoxemia. Chest. 127:1904–1910. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Nishimura K, Izumi T, Tsukino M and Oga T:
Dyspnea is a better predictor of 5-year survival than airway
obstruction in patients with COPD. Chest. 121:1434–1440.
2002.PubMed/NCBI
|