Introduction
Transient ischemic attack (TIA) is an important risk
factor for ischemic stroke. Appropriate antithrombotic therapy may
reduce the risk of stroke following TIA. Aspirin is the
antiplatelet agent most widely used to treat TIA of
noncardioembolic origin and it is able to reduce the risk of stroke
by 19% in patients who have experienced TIA or a stroke (1). However, aspirin is not able to
thoroughly control TIA in certain patients. Another antiplatelet
agent, cilostazol, may be considered as an alternative treatment in
these cases. Cilostazol is a quinolinone-derivative medication
widely used in patients with peripheral vascular disease. It is a
phosphodiesterase inhibitor which inhibits platelet aggregation.
This study reports two cases of TIA refractory to aspirin and the
effectiveness of cilostazol in these cases.
Case reports
Case 1
An 83-year-old female patient was admitted to the
Zhejiang Provincial People’s Hospital (Hangzhou, China) due to
episodes of weakness and numbness of the left extremities during
the previous 20 days. These episodes lasted ~10 min and occurred
8–10 times every day. Consciousness was never impaired and the
patient experienced no dizziness or additional complaints. The
patient had a past history of diabetes and hypertension, which were
treated with glimepiride and felodipine, respectively. Physical
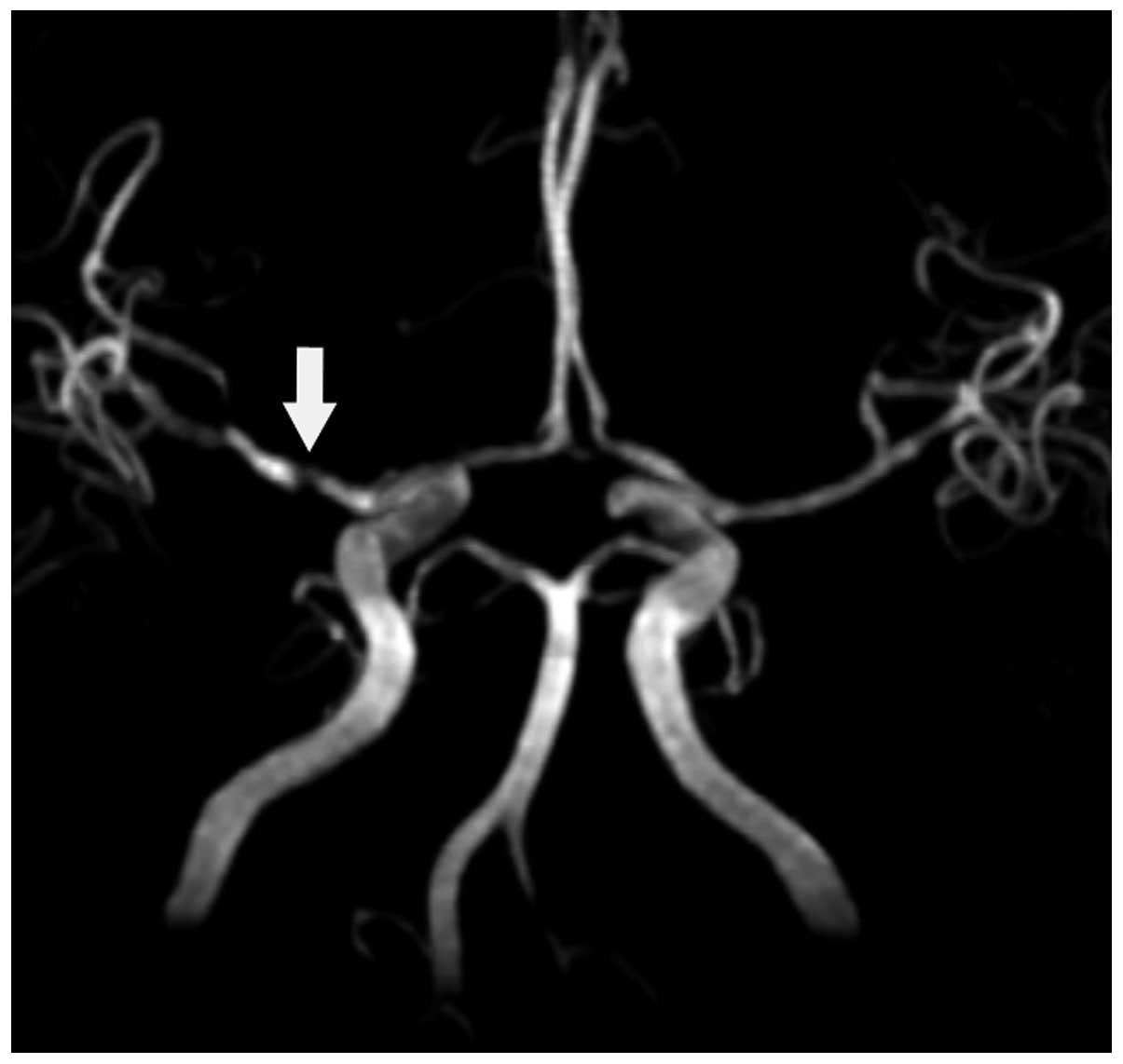
examination showed no neurological deficits. Magnetic resonance
angiography revealed severe segmental stenosis of the right middle
cerebral artery (Fig. 1). No new
infarcts were observed following diffusion-weighted magnetic
resonance imaging. Sinus rhythm was observed in the
electrocardiogram and mild aortic valve regurgitation with no
thrombus was reflected in the echocardiogram. Carotid ultrasound
showed no atherosclerotic plaques. The low density lipoprotein
cholesterol level was 2.91 mmol/l. A diagnosis of TIA was made.
The patient was treated with 200 mg aspirin and 20
mg atorvastatin once per day for 7 days. Episodes of weakness and
numbness of the left extremities continued to occur 7–10 times per
day. Clopidogrel (75 mg) was then administered once per day;
however, episode frequency did not decrease. On the 11th day
following admission, anticoagulation therapy with low molecular
heparin (4100 U) twice a day replaced antiplatelet therapy. The
frequency of episodes decreased to once or twice a day. On the 19th
day following admission, 100 mg cilostazol was administered twice a
day in place of the anticoagulation therapy. No symptoms of TIA
were observed from then on during the three-year follow-up period,
with the exception of one episode of perioral numbness of the left
side lasting for 1 min on the first day following the adjustment of
medication.
Case 2
A 51-year-old male presented to the Zhejiang
Provincial People’s Hospital (Hangzhou, China) due to two episodes
of paroxysmal weakness of the left extremities with dysarthria
during the previous 30 h. The first episode lasted for 10 min and
the second one for 3 min. The patient had a history of hypertension
and was treated with losartan, and a history of diabetes mellitus,
which was controlled successfully with gliclazide. No neurological
deficits were found on physical examination. Diffusion-weighted
magnetic resonance imaging showed no signs of acute infarction.
Computed tomography perfusion of the brain was normal.
Ultrasonography revealed atherosclerosis of both carotid arteries.
Electrocardiogram showed sinus rhythm and no thrombus was found
following the echocardiogram. The low density lipoprotein
cholesterol level was 3.39 mmol/l. Digital subtraction angiography
reflected mild stenosis of the right internal carotid artery. The
patient was diagnosed with TIA.
Antiplatelet therapy with aspirin and
anti-atherosclerotic therapy with atorvastatin were initiated. On
the seventh day following admission, episodes of weakness of the
left extremities with dysarthria recurred. These episodes lasted
for 2–3 min each time and occurred eight times in total on that
day. The antiplatelet agent was replaced with 100 mg cilostazol
twice a day. On the first day after treatment adjustment, three
episodes of ischemia similar to the previous ones recurred.
Diffusion-weighted magnetic resonance imaging excluded new cerebral
infarction. No weakness of the limbs or dysarthria recurred from
then on during the two-year follow-up period.
Discussion
With the development of neuroimaging techniques, the
time criterion for TIA has been challenged. In one study, it was
identified that approximately one-third of patients that were
clinically diagnosed with TIA showed associated new infarcts
following MRI (2). A formal
evidence review suggested a new definition of TIA as ‘a brief
episode of neurological dysfunction caused by focal brain, spinal
cord or retinal ischemia, without acute infarction’ (3). It focuses on whether histological
damage occurs. Diffusion-weighted magnetic resonance imaging of the
two patients in the present study was normal, which supported the
diagnosis of TIA.
The early risk of ischemic stroke following TIA is
very high. The stroke risk following TIA has been estimated to be
8.0% within seven days, 11.5% within one month and 17.3% within
three months (4). Several scoring
systems have been designed to evaluate the risk of infarction
following TIA. The ABCD2 score is a popular and effective
predictor, which is based on age, blood pressure, clinical
features, the duration of symptoms and diabetes mellitus. An ABCD2
score of ≥4 is an independent predictor of the risk of stroke one
week and 90 days following the onset of TIA (5). The ABCD2 scores of the case 1 and 2
patients were 6 and 5, respectively. Both patients were at high
risk of infarction.
A previous study has shown that urgent evaluation
and treatment may lower the risk of stroke in 90 days, subsequent
hospital bed-days, acute costs and 6-month disability (6). However, the majority of randomized
controlled trials on the secondary prevention of ischemic stroke
have included patients with TIA and infarction rather than patients
with TIA only (7,8). Therefore, the best antithrombotic
regimen for TIA remains unclear. The 9th edition of the guidelines
for antithrombotic therapy and prevention of thrombosis issued by
the American College of Chest Physicians recommended long-term
treatment with aspirin, clopidogrel, aspirin/extended-release
dipyridamole or cilostazol in patients with a history of
noncardioembolic ischemic stroke or TIA (9). The Chinese Acute Stroke Trial (CAST)
(10) and the International Stroke
Trial (IST) (11) demonstrated
that initiating antiplatelet therapy with aspirin soon after the
onset of acute ischemic stroke reduced the risk of recurrent stroke
or death. The Fast assessment of stroke and TIA to prevent early
recurrence (FASTER) trial (12)
implied that a combination of aspirin and clopidogrel may be more
effective than aspirin alone following TIA or a minor stroke within
90 days.
The effects of anticoagulation therapy for
non-cardiac TIA have not been fully evaluated. In the IST (11), heparin significantly decreased
recurrent ischemic stroke following cerebral infarction, but
increased hemorrhage with no net benefit. Therefore, heparin is not
recommended for routine use following ischemic stroke. It should
only be considered in patients at high risk of early
recurrence.
The patient of case 1 had TIA of non-cardiac origin.
Aspirin alone or aspirin in combination with clopidogrel were not
effective. Anticoagulation therapy with low molecular heparin
decreased the frequency of ischemic episodes with complete
remission following antiplatelet therapy with cilostazol. In case
2, eight episodes of weakness of the left extremities with
dysarthria recurred while the patient was treated with aspirin.
Following the change of the antiplatelet agent to cilostazol, no
ischemic episodes recurred, with the exception of three on the
first day.
Cilostazol is a phosphodiesterase type 3 inhibitor,
which increases the cyclic adenosine monophosphate concentration
inside platelets, which subsequently potentiates the inhibitory
signals of glycoprotein, IIb–IIIa. No randomized controlled trials
evaluating the role of cilostazol in the prevention of ischemic
stroke following TIA have been published. However, the effects of
cilostazol as a secondary prevention after ischemic stroke have
been evaluated. Compared with aspirin, cilostazol is equal to or
more effective in the secondary prevention of stroke after
noncardioembolic stroke (13). It
is particularly effective for lacunar infarction and ischemic
stroke with hypertension or diabetes mellitus (14). In a pilot study, intracranial
hemorrhage was observed to be less common in patients treated with
cilostazol than in those treated with aspirin (15). However, cilostazol caused a greater
incidence of side-effects, including headache, diarrhea,
palpitations, dizziness and tachycardia. An escalation regimen of
cilostazol starting from 50 mg twice a day for an initial 4 days
followed by 100 mg twice a day may increase tolerability (16).
Cilostazol was particularly efficacious for the two
patients with TIA in the present study. Cilostazol not only
inhibits platelet aggregation, but also has an effect of
vasodilation by increasing the production of nitric oxide and
reducing intracellular calcium ion concentrations (17). Moreover, it protects the
endothelium and inhibits smooth muscle proliferation of the
vascular walls (18).
In conclusion, cilostazol was particularly effective
for the two patients with TIA in the present study. It may be
efficacious in the prevention of ischemic stoke following TIA of a
non-cardiac origin that is not responsive to aspirin.
Acknowledgements
This study was supported by the Project of the
Department of Science and Technology of Zhejiang Province (grant
no. 2012C21014).
References
|
1
|
Antithrombotic Trialists’ (ATT)
Collaboration. Aspirin in the primary and secondary prevention of
vascular disease: collaborative meta-analysis of individual
participant data from randomised trials. Lancet. 373:1849–1860.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fazekas F, Fazekas G, Schmidt R, Kapeller
P and Offenbacher H: Magnetic resonance imaging correlates of
transient cerebral ischemic attacks. Stroke. 27:607–611. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Easton JD, Saver JL, Albers GW, et al:
Definition and evaluation of transient ischemic attack: a
scientific statement for healthcare professionals from the American
Heart Association/American Stroke Association Stroke Council;
Council on Cardiovascular Surgery and Anesthesia; Council on
Cardiovascular Radiology and Intervention; Council on
Cardiovascular Nursing; and the Interdisciplinary Council on
Peripheral Vascular Disease. The American Academy of Neurology
affirms the value of this statement as an educational tool for
neurologists. Stroke. 40:2276–2293. 2009.
|
|
4
|
Coull AJ, Lovett JK and Rothwell PM;
Oxford Vascular Study. Population based study of early risk of
stroke after transient ischaemic attack or minor stroke:
implications for public education and organisation of services.
BMJ. 328:3262004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Johnston SC, Rothwell PM, Nguyen-Huynh MN,
et al: Validation and refinement of scores to predict very early
stroke risk after transient ischaemic attack. Lancet. 369:283–292.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Luengo-Fernandez R, Gray AM and Rothwell
PM: Effect of urgent treatment for transient ischaemic attack and
minor stroke on disability and hospital costs (EXPRESS study): a
prospective population-based sequential comparison. Lancet Neurol.
8:235–243. 2009. View Article : Google Scholar
|
|
7
|
Wang Y, Wang Y, Zhao X, et al: Clopidogrel
with aspirin in acute minor stroke or transient ischemic attack. N
Engl J Med. 369:11–19. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Diener HC, Bogousslavsky J, Brass LM, et
al: Aspirin and clopidogrel compared with clopidogrel alone after
recent ischaemic stroke or transient ischaemic attack in high-risk
patients (MATCH): randomised, double-blind, placebo-controlled
trial. Lancet. 364:331–337. 2004. View Article : Google Scholar
|
|
9
|
Eikelboom JW, Hirsh J, Spencer FA, Baglin
TP and Weitz JI: Antiplatelet drugs: Antithrombotic Therapy and
Prevention of Thrombosis, 9th ed: American College of Chest
Physicians Evidence-Based Clinical Practice Guidelines. Chest.
141(2 Suppl): e89S–e119S. 2012. View Article : Google Scholar
|
|
10
|
CAST (Chinese Acute Stroke Trial)
Collaborative Group. CAST: randomised placebo-controlled trial of
early aspirin use in 20,000 patients with acute ischaemic stroke.
Lancet. 349:1641–1649. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
International Stroke Trial Collaborative
Group. The International Stroke Trial (IST): a randomised trial of
aspirin, subcutaneous heparin, both, or neither among 19435
patients with acute ischaemic stroke. Lancet. 349:1569–1581. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kennedy J, Hill MD, Ryckborst KJ, Eliasziw
M, Demchuk AM and Buchan AM; FASTER Investigators. Fast assessment
of stroke and transient ischaemic attack to prevent early
recurrence (FASTER): a randomised controlled pilot trial. Lancet
Neurol. 6:961–969. 2007. View Article : Google Scholar
|
|
13
|
Shinohara Y, Katayama Y, Uchiyama S, et
al; CSPS 2 group. Cilostazol for prevention of secondary stroke
(CSPS 2): an aspirin-controlled, double-blind, randomised
non-inferiority trial. Lancet Neurol. 9:959–968. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Shinohara Y, Gotoh F, Tohgi H, et al:
Antiplatelet cilostazol is beneficial in diabetic and/or
hypertensive ischemic stroke patients. Subgroup analysis of the
cilostazol stroke prevention study. Cerebrovasc Dis. 26:63–70.
2008. View Article : Google Scholar
|
|
15
|
Huang Y, Cheng Y, Wu J, et al; Cilostazol
versus aspirin for secondary ischaemic stroke prevention (CASISP)
cooperation investigators. Cilostazol as an alternative to aspirin
after ischaemic stroke: a randomised, double-blind, pilot study.
Lancet Neurol. 7:494–499. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nishiyama K, Seyama H, Okano H, et al:
Escalation regimen of cilostazol for acute brain infarction. Intern
Med. 50:1559–1563. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chi YW, Lavie CJ, Milani RV and White CJ:
Safety and efficacy of cilostazol in the management of intermittent
claudication. Vasc Health Risk Manag. 4:1197–1203. 2008.PubMed/NCBI
|
|
18
|
Otsuki M, Saito H, Xu X, et al: Cilostazol
represses vascular cell adhesion molecule-1 gene transcription via
inhibiting NF-kappaB binding to its recognition sequence.
Atherosclerosis. 158:121–128. 2001. View Article : Google Scholar : PubMed/NCBI
|