Introduction
Intramedullary schwannoma, which was first reported
by Penfild in 1932 (1), is a rare
tumour that accounts for 1.1% of all intraspinal tumours. Prior to
surgery, intramedullary schwannoma is often misdiagnosed as other
types of malignant tumour, including ependymoma, astrocytoma and
hemangioblastoma, due to its atypical imaging appearance and low
incidence. Long follow-ups of intramedullary schwannomas are
unavailable.
The present study collected the surgery and
follow-up process data of one case of intramedullary
schwannoma.
Case report
A 42-year-old patient complaining of progressive
zonesthesia in the right side of the chest, weakness and numbness
of the bilateral lower limbs for 1.5 years and dysuria and
paralysis for 1 week was admitted to Jiangmen Central Hospital. The
present study was conducted in accordance with the Declaration of
Helsinki and with the approval of the Ethics Committee of Zhujiang
Hospital, Nanfang Medical University. Written informed consent was
obtained from the patient. The physical examination revealed a
disturbance of superficial sensation, grade 2 muscle strength and
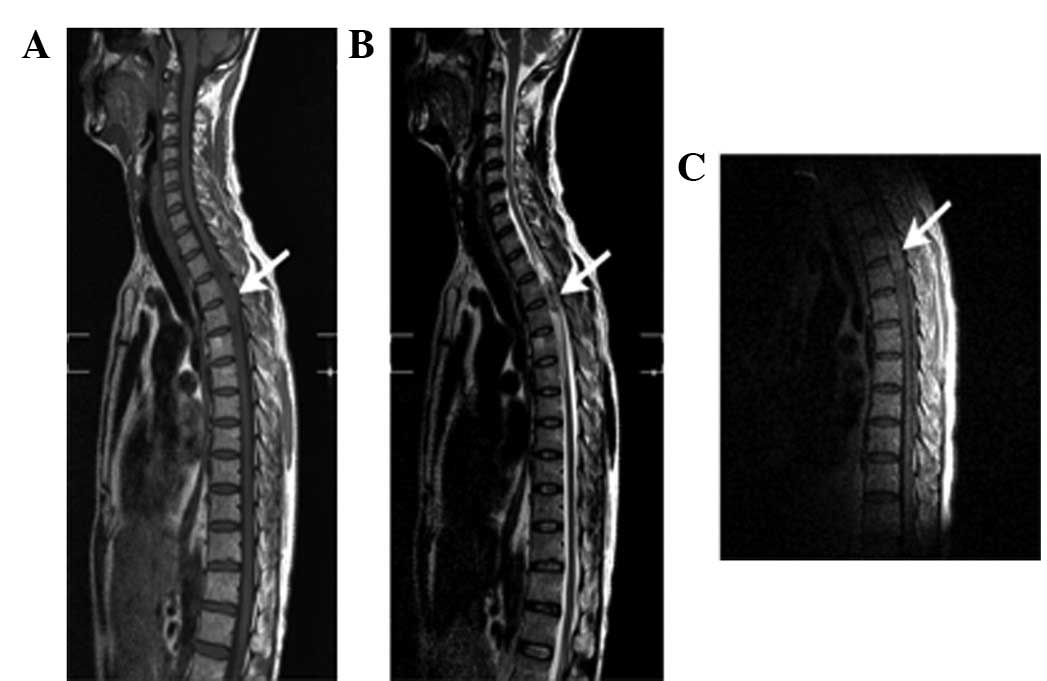
positive Babinski sign. Abnormal long ovoid T1 (Fig. 1A) and T2 (Fig. 1B) soft-tissue masses were observed
at the third and fourth thoracic vertebrae. The lesion size was
1.3x1.1x2.4 cm with a clear margin and heterogenous intensity. The
lesion showed heterogenous contrast enhancement and compression of
the adjacent subarachnoid space (Fig.
1C). The spinal cord adjacent to the lesion was swollen.
According to the MRI appearance of the lesion, astrocytoma or
ependymoma was suspected. The possibility of a malignant tumour was
also suspected due to a nodule observed on the left lung.
Tumour excision was initiated with exploration by
decompression of the vertebral bone. After the patient’s relative
signed the informed consent agreement, the surgery was performed as
follows. Sterilised methylene blue fluid was used to create a
marker for the X-ray at the third thoracic vertebra 1 day before
the surgery. General anaesthesia was used and the patient was left
in a recumbent position. A small incision was made to reveal the
vertebral disc of the third and fourth thoracic vertebrae. The
inferior third and superior fourth vertebral plates were drilled to
open a 2x2-cm bone window. The whole surgery was performed under a
microscope manufactured by Leica (Wetzlar, Germany). A tight
adhesion of the spinal dura, arachnoid and spinal cord was observed
after the spinal dura was cut. A fragile tumour supplied with rich
blood was revealed in the spinal cord and the subarachnoid space. A
malignant tumour was initially diagnosed, but the tumour was noted
to have a clear margin with the spinal cord surrounded by
proliferating small vessels. The lesion was excised completely.
Schwannoma was diagnosed by frozen section
pathology. Following surgery, the numbness of the right side of the
chest and weakness of the lower limbs were reduced compared with
before the surgery.
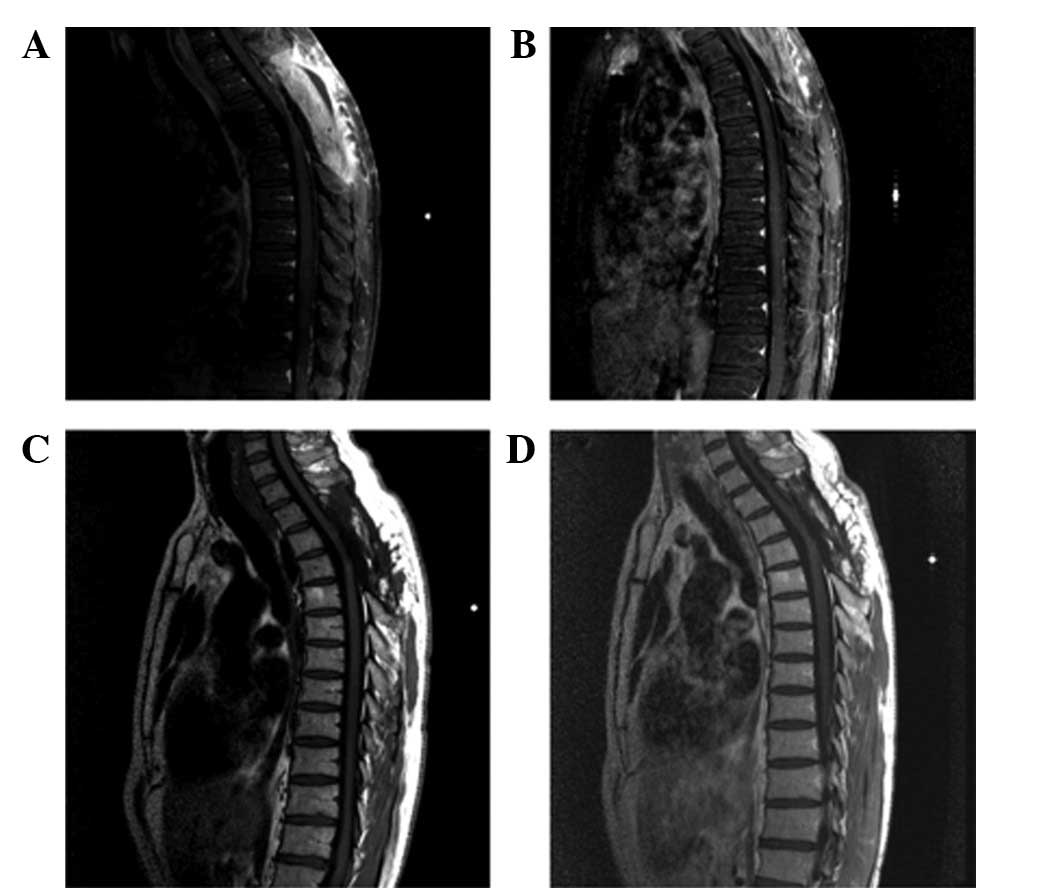
No lesion was detected using MRI during the
follow-up period at 3 (Fig. 2A), 6
(Fig. 2B), 12 (Fig. 2C) and 18 months (Fig. 2D) after the surgery. A small
ariaosis was observed in the spinal cord.
The numbness of the right side of the chest had
completely disappeared at 6 months after the surgery. The weakness
and numbness of the lower limb partially improved. Although the
patient continued to have defecation and micturition disturbances,
all symptoms had disappeared at 18 months after the surgery. A
small fluid-filled region was observed in the epidural space.
Discussion
Intramedullary schwannoma is a rare tumour that
accounts for ∼1.1% of schwannomas in the spinal canal. Up to 34
cases were included in the study of Hejazi and Hassler (2) published in 1998, whereas Qian et
al(3) observed only 82 cases
when reviewing domestic and foreign data in 2006. Ross et
al(1) noted that 60.7 and 20%
of all intramedullary schwannomas occurred in the cervical and
thoracic regions, respectively (4). This type of tumour is uncommon in
other regions. The ages of the patients in the reported cases
ranged between 11 months and 53 year.
Based on the reported cases, the main symptoms of
intramedullary schwannomas are progressive numbness, fatigue and
pain in the extremities, whereas the main physical signs are
hypertonia, decreased muscle strength, hypalgesia and
hypopselaphesia, tenden reflex attenuation and tendinous reflex.
These clinical manifestations are also common in other lesions of
the spinal cord.
Intramedullary schwannoma has no specific imaging
features (3). However, Kodama
et al(5) reported that
diagnosis of schwannoma should be considered if an intramedullary
tumour has a clear boundary in the spinal cord and intense
enhancement. Qian et al(3)
described certain changes in MR that aid the diagnosis of
intramedullary schwannoma. Firstly, the tumour exhibits
isointensity or a slightly longer T1 and isointensity or long T2
signals, often combined with cystic degeneration. Secondly, the
lesion shows intense and homogenous enhancement. Thirdly, the
margin is clear. Fourthly, the lesions are often small (normally
within three vertebrae) tumours. In 2005, Kim et al(6) revealed that slight peritumoural
oedema is one of the characteristics of intramedullary schwannomas.
However, another study did not agree with this finding (3).
Owing to its low incidence and lack of clinical and
imaging manifestation, intramedullary schwannoma is often
misdiagnosed as other types of intramedullary tumour such as
ependymoma, astrocytoma, hemangioblastoma and subependymoma, among
others (1,3,6).
No widely accepted explanation is available for the
occurrence of intramedullary schwannoma. The origin of the tumour
has multiple factors. Several possibilities based on the study by
Liu et al(4) for the origin
of the lesion are as follows: i) schwannoma cells in the posterior
spinal cord nerve root; ii) schwannoma cells located along the
blood vessels and peripheral nerves of the spinal cord; iii)
schwannoma cells dislocated during the closure of the neural crest
in the fourth week of embryonic development; iv) pia mater cells
from the mesoderm; v) the peripheral fibres of vagus nerves in the
spinal cord; and vi) a traumatic spinal cord injury or a chronic
disorder of the central nervous system (1,7,8).
The traditional surgical approach for removing
occupying lesions in the spinal canal causes adverse effects in
three column structures. The spinous process, supraspinal and
interspinous ligaments, vertebral arch, vertebral plate,
ligamentum flavum and facet joint are cut during central and
posterior rhizotomies, resulting in spinal instability and thus
significantly affecting the lives of patients.
According to Denis’s three-column principle
(9), minimally invasive
hemilaminectomy should be used as the treatment method for
space-occupying lesions instead of central and posterior
rhizotomies to maintain the stability of the vertebral column
(10). In the presence of clear
peripheral oedema, malignant tumours diagnosed prior to surgery
should be treated using central and posterior rhizotomies. In
addition, a biopsy should be performed to confirm the diagnosis or
to partly excise the tumour. These procedures affect the stability
of the vertebral column.
This case was preoperatively diagnosed as an
ependymoma or astrocytoma. Minimally invasive hemilaminectomy was
performed on the space-occupying lesion in the spinal cord with
clear boundaries and intense enhancement. The possibility of
endoscopic resection was also considered. The surgery was
considered to be successful. All the benign tumours were removed
and central and posterior rhizotomies were avoided. The patient
recovered well after the surgery and intramedullary schwannoma did
not recur during the two-year follow-up period.
Therefore, depending on the patient’s condition,
doctors may consider a case to be a possible intramedullary
schwannoma and perform minimally invasive hemilaminectomy if no
confirmed diagnosis has been acheived prior to the surgery,
particularly when differential diagnosis exists among ependymoma,
astrocytoma and hemangioblastoma and if the space-occupying lesion
in the spinal cord had clear boundaries and exhibited intense
enhancement. The necessity of cutting the spinous process,
ligamentum flavum and bi-vertebral plate may then be decided after
the biopsy results are known. In this way, the spinal instability
resulting from the traditional surgical procedure of excision
during central and posterior rhizotomies, which are preoperatively
applied to patients diagnosed with malignant tumours, may be
avoided.
References
|
1.
|
Ross DA, Edwards MSB and Wilson CB:
Intermedullary neurilemomas of the spinal cord: report of two cases
and review of the literature. Neurosurgery. 19:458–464. 1986.
View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Hejazi N and Hassler W: Microsurgical
treatment of intramedullary spinal cord tumors. Neurol Med Chri
(Tokyo). 38:266–273. 1998. View Article : Google Scholar
|
|
3.
|
Qian YF, Wang WQ and Yu YQ: Two cases of
intramedullary schwannoma. Chinese J Radiol. 12:1337–1338.
2006.
|
|
4.
|
Liu L, Wang GW and Yang J: 1 Case report
of intra-medullary schwannoma and review of literature. Journal of
Chinese Neurotumor. 5:42–44. 2007.
|
|
5.
|
Kodama Y, Terae S, Hida K, et al:
Intramedullary schwannoma of the spinal cord: report of two cases.
Neuroradiology. 43:567–571. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Kim SD, Nakagawa H, Mizuno J and Inoue T:
Thoracic subpial intramedullary schwannoma involving a ventral
nerve root: a case report and review of the literature. Surg
Neurol. 63:389–393. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Aryanpur J and Long DM: Schwannoma of the
medulla oblongata. Case report. J Neurosurg. 69:446–499. 1988.
View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Riffaud L, Morandi X, Massengo S, et al:
MRI of the intramedullary spinal schwannomas: case report and
review of the literature. Neruoradiology. 42:275–279. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Denis F: The three column spine and its
significance in the classification of acute thoracolumbar spinal
injuries. Spine (Phila Pa 1976). 8:817–831. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Xu RX, Ke YS, Zhang SZ, et al: Analysis of
intravertebral canal tumors in 296 cases. Journal of First Military
Medical University. 19:130–132. 1999.(In Chinese).
|