Introduction
The morbidity of anterior cruciate ligament (ACL)
injury has been reported to be ∼1 per 3,000 per year in the US
population (1). For those engaged
in football the incidence of ACL injury is ∼60 per 100,000 per year
and for skiing athletes it is 70 per 100,000 per year (2). ACL injury may lead to articularis
genus instability. Reconstruction should take place within 3
months, but if it is not then osteoarthritis may occur after 4–6
months, resulting in joint replacement and a poor quality of life.
Therefore, it is important to diagnose and treat the injury
early.
Due to the poor self-healing of the ACL, it requires
repair by allograft reconstruction, instead of a simple ACL suture.
The autologous transplantation is currently the most widely used in
clinical practice and achieves good clinical results. Using an
arthroscope, ACL reconstruction using the central third patellar
ligament (PL) has become the standard surgical treatment of ACL
injury (3). Autologous tissue,
including the semitendinosus and the tensor fascia
latae muscles, are used to reconstruct the ACL; however, these
tissues are not sufficiently strong and relax over time. Therefore,
the prospective efficacy is poor. In these surgical methods, the
ligament-tendon insertion is reconstructed into the bone; however,
the connection of tendon to bone is not reliable, as it becomes
loose or avulses. In ACL recovery using the central third PL,
bone-patellar tendon-bone (B-P-B) reconstruction allows bone-bone
direct healing. The tensile strength of B-P-B is significantly
higher than that of other tissues and the bones on both sides of
B-P-B provide fixed points of the reconstructed cruciate ligament.
The surgical process achieves bone bio-fixation and is regarded as
the best option for orthopedists with the clear advantages of
safety, accessibility and high strength (4). In clinical practice, a number of
factors may lead to surgery failure, including the shortness,
injury or pathological changes of the PL, as well as fractures in
the operative field or meniscus and articular cartilage injury. A
graft that is too long without sufficient fixation may cause
graft-tunnel mismatch (5–8); therefore, the geometric data of the
ligaments directly affect the graft and reconstruction (8).
Magnetic resonance imaging (MRI) provides good
tissue resolution and high spatial resolution, which allows the
clear imaging of bones, including the patella, femur and tibia, as
well as the ligamental structures of the patellar tendon and ACL,
with a clear boundary from peripheral tissue. Rigorous data may be
obtained from MRI images using an MRI workstation with a precision
of 0.01 mm. This is helpful for obtaining geometric data and
determining the state of the articularis genus and ligament
of the affected limb prior to surgery.
At present, the samples examined in studies of ACL
length measurement have mainly been adult cadaver articularis
genus specimens and the values reported differ greatly. The
Physical Investigation Committee of the Chinese Society for
Anatomical Science provided only data for ACL length (9) and previous MRI studies were case
reports of abnormal PL (10–13),
which are not useful for ACL repair surgery. The present study
establishes the geometric data of PL and ACL in vivo and
provides valuable imaging information for ACL reconstruction.
Materials and methods
Inclusion criteria of images
Clear MRI images of the PL and ACL were obtained
throughout the whole process with intact continuity. There were
low-band signals in sequences and faults of PL. The ACL fiber
bundles had distinctly visible fiber directions and equal signals,
while the dense fiber bundles presented low signals.
Enrollment of subjects
A total of 157 cases with PL and ACL images were
enrolled from October 2004 to March 2007. All individuals were Han
Chinese with bilateral articularis genus MRI results. There
were 79 male cases, aged 15–71 years, with a mean body weight of
64.24±4.98 kg and height of 169.63±6.06 cm and 78 female cases,
aged 15–73 years, with a mean body weight of 56.93±4.88 kg and
height of 158.73±4.52 cm. This study was conducted in accordance
with the Declaration of Helsinki and with approval from the Ethics
Committee of the First Affiliated Hospital of Xinxiang Medical
University. Written informed consent was obtained from all
participants.
Examination methods
The GE Signa 1.5 Tesla superconductive magnetic
resonance and dedicated articularis genus surface coil were
used in the present study. In the examination, the subject lay
supine with their knees placed in a comfortable position and the
center of the coil was set at the inferior margin of the patella.
The scan parameters were as follows: echo time (TE), 10 msec;
repetition time (TR), 575 msec; echo train length (ETL), 2;
bandwidth (BW), 20.83; field of vision (FOV), 16; slice thickness
(ST), 4 mm; S-interval, 1 mm; frequency coding (Freq), 384; phase
encoding (Phase), 256 and excitation number (Nex), 2.
PL and ACL measurement
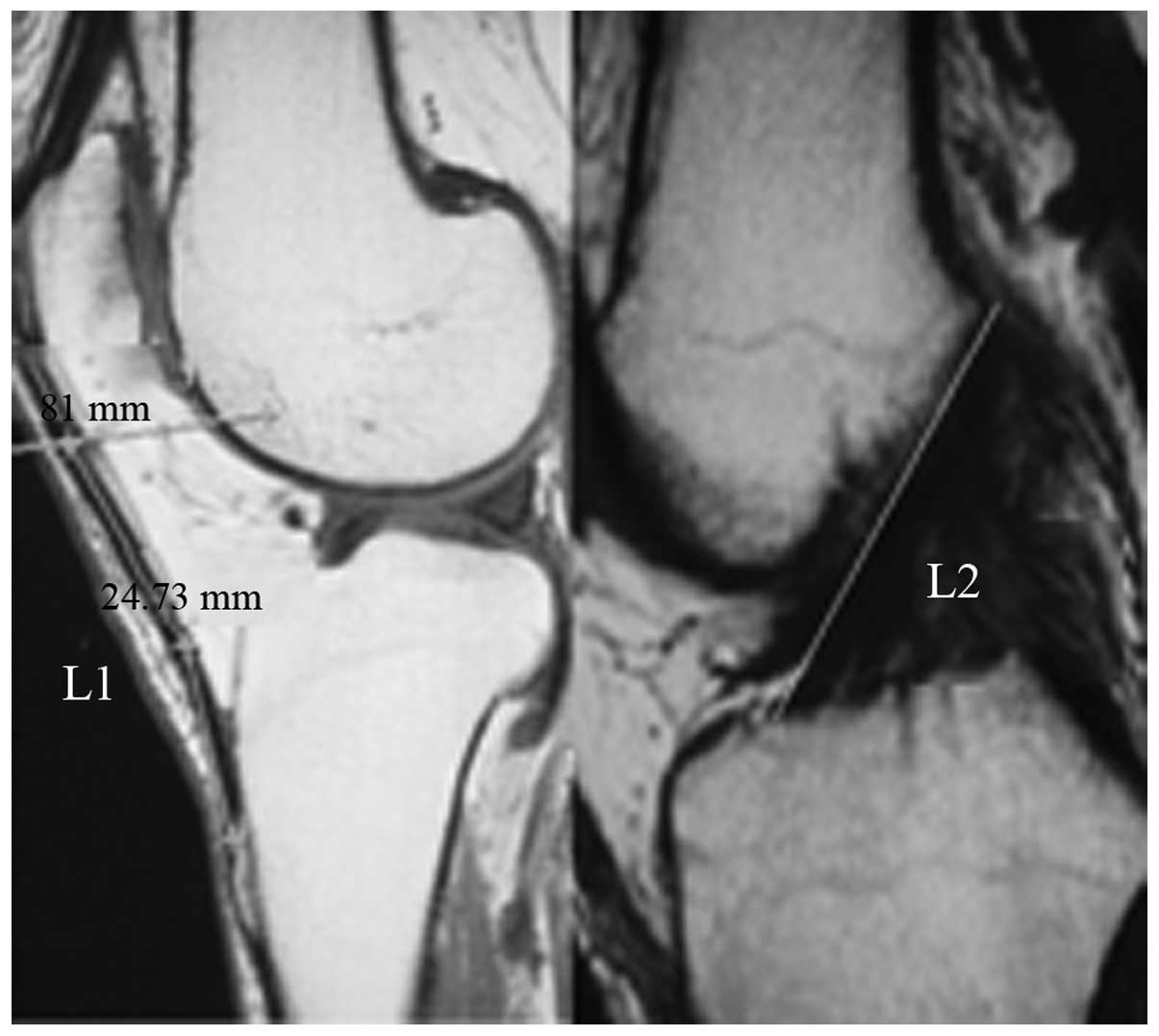
PL length in the oblique sagittal position (L1) was
from the lower edge of the patella to the tibial tubercle. In the
ACL length (L2) measurement, the starting point was the top of the
lateral intercondylar notch in the femoral attachment and the end
was the front facies ossea of the eminentia
intercondylaris in the tibial attachment point (L2 line). We
calculated the ratio of L1 and L2 (L1/L2; Fig. 1).
Features in the MRI images were measured using the
Radworks 5.1 professional workstation. In order to ensure
reliability, all data were obtained by doctor A first, then, after
one month the length of the left patellar tendon was remeasured
independently by doctors B and C.
Statistical analysis
Data are presented as mean ± standard deviation.
Statistical analysis was performed using SPSS 13.0 (SPSS Inc.,
Chicago, IL, USA). The paired t-test was used in the common index
of left and right knee ligaments and the independent samples t-test
was applied in the comparison between males and females. Linear
regression and linear correlation analyses were used in the
dependablity statistics for PL data and body weight, body height
and ACL length. The data reliability from the same software was
identified by intra-class correlation coefficient (ICC) of the PL
length measured by doctors A, B and C. P<0.05 was considered to
indicate a statistically significant result.
Results
ICC in left patellar tendon length
The left patellar tendon lengths determined by the
three doctors were almost entirely credible, with an ICC of
0.80–1.00. The ICC was not <0.997 (Table I).
 | Table I.ICC for the measurements of left
patellar tendon length from three doctors. |
Table I.
ICC for the measurements of left
patellar tendon length from three doctors.
| Left L1 from doctor
B | Left L1 from doctor
C |
|---|
| Left L1 from doctor
A | 1.000 | 0.997 |
| Left L1 from doctor
B | | 0.997 |
L1 and L2 in 157 cases
In the 157 cases of MRI data, the L1 and L2 for the
left side of the body were not significantly different from those
of the right side (P>0.05; Table
II).
 | Table II.Comparison of left and right L1 and
L2. |
Table II.
Comparison of left and right L1 and
L2.
| Left (mm) | Right (mm) |
|---|
| N | 157 | 157 |
| L1 | 41.15±4.24 | 41.21±4.23a |
| L2 | 36.40±4.44 | 36.38±4.45a |
PL and ACL
In the MRI measurements of the left and right knees,
the lengths of the PL and ACL in males were significantly greater
than those in females (P<0.05; Table III).
 | Table III.Comparison of PL and ACL in males and
females. |
Table III.
Comparison of PL and ACL in males and
females.
| | Males
| Females
|
|---|
| Position | N | Length (mm) | N | Length (mm) |
|---|
| L1 | Left | 79 | 42.19±4.22 | 78 | 40.10±4.01a |
| Right | 79 | 42.20±4.23 | 78 | 40.20±4.02a |
| Average | 158 | 42.20±4.21 | 156 | 40.15±4.00a |
| L2 | Left | 79 | 36.99±4.12 | 78 | 35.80±4.68 |
| Right | 79 | 36.96±4.14 | 78 | 35.79±4.69 |
| Average | 158 | 36.98±4.12 | 156 | 35.80±4.67a |
Ratio of L1 and L2 (L1/L2)
There was no significant difference in L1/L2 between
the left and the right sides, by paired t-test (P>0.05, Table IV).
 | Table IV.Comparison of L1/L2 ratio between
males and females. |
Table IV.
Comparison of L1/L2 ratio between
males and females.
| L1/L2 | Male | Female | Total |
|---|
| Left | 1.15±0.09 | 1.13±0.11 | 1.14±0.10a |
| Right | 1.15±0.09 | 1.13±0.12 | 1.14±0.10a |
L1, L2 and L1/L2 in different age
ranges
The L1 of the young group (aged 15–24 years) was
significantly different from those of the post-adolescent (aged
25–64) and senior (aged ≥65 years) groups in male and female cases
(P<0.05). However, L2 and L1/L2 did not present a correlation
with age (P>0.05; Table V).
 | Table V.L1, L2 and L1/L2 in different age
stages. |
Table V.
L1, L2 and L1/L2 in different age
stages.
| Male
| Female
|
|---|
| Age (years) | N | L1 | L2 | L1/L2 | N | L1 | L2 | L1/L2 |
|---|
| 15–24 (young) | 58 | 43.95±4.25a | 38.45±4.62 | 1.15±1.09 | 36 | 42.03±0.94a | 36.00±1.06 | 1.18±0.11 |
| 25–64
(post-adolescent) | 58 | 40.99±4.45 | 36.06±3.74 | 1.14±0.09 | 78 | 39.84±0.64 | 36.50±0.81 | 1.11±0.02 |
| ≥65 (senior) | 42 | 41.43±3.08 | 36.62±3.44 | 1.15±0.09 | 42 | 38.94±0.79 | 34.36±0.85 | 1.13±0.07 |
Correlation analysis of L1 with body
height, body weight and L2 length
L1 had no significant correlation with body height
or weight by linear correlation and regression analysis. However,
L1 was significantly correlated with the L2 of the same side
(Table VI).
 | Table VI.Correlation analysis of L1 with body
height, body weight and L2. |
Table VI.
Correlation analysis of L1 with body
height, body weight and L2.
| r-value |
|---|
| Left L1 and
height | 0.143 |
| Right L1 and
height | 0.137 |
| Left L1 and body
weight | 0.038 |
| Right L1 and body
weight | 0.031 |
| Left L1 and Left
L2 | 0.672a |
| Right L1 and Right
L2 | 0.664a |
Discussion
ACL reconstruction using the central third PL under
an arthroscope has become the standard surgical treatment for ACL
injury. In clinical practice, a number of factors lead to surgery
failure, including the shortness, injury or pathological changes of
the PL, fractures in the operating field or meniscus and articular
cartilage injury. The MRI appearance varies according to the
pathological and histological changes of the injury. Ligament data
measured by MRI are helpful to detect these abnormalities prior to
surgery.
MRI has good tissue resolution and spatial
resolution. Chen et al(14)
confirmed that the 0.2 Tesla field strength of MRI clearly shows
the ligament route in a normal knee and a lamellar anatomical
cross-section in the oblique coronal plane of a frozen knee ACL. He
et al(15) verified the
clinical value of 0.2 Tesla field strength MRI for PL data. In the
present study, all images were achieved using 1.5 Tesla MRI with
specific coils for the articularis genus. The Radworks 5.1
measuring tool was accurate to 0.01 mm; therefore, our study
obtained rigorous data with clinical value.
In the 157 cases, the ICCs were ≥0.997 for the left
PL length as measured by three doctors. Landis and Koch (16) suggested that an ICC of 0.00–0.20 is
not credible, 0.21–0.40 is generally credible, 0.41–0.60 is
averagely credible, 0.61–0.80 has good credibility and 0.80–1.00 is
almost entirely credible. Our ACL length result was similar to the
value (36.00±0.20 mm) provided by the Physical Investigation
Committee of the Chinese Society for Anatomical Science (9), which demonstrates the credibility of
the present measurements. We considered that measurement results
from Radworks 5.1 did not differ significantly between users and
data from a single once-repeated survey using these measuring tools
was credible.
In a study of an ACL autograft, Hadjicostas et
al(17) compared the PL,
semitendinosus and gracilis tendon and identified
that the latter two have potential advantages in organism
remodeling and regeneration with significant high-density collagen
fibers and fibroblasts. The gracilis and
semitendinosus tendons also have good strength; however,
they do not form the ligament attachment points with soft
tissue-bone fixation. In clinical practice, there are no
significant differences between the patellar tendon and the
semitendinosus tendon (18). Previously, a multicenter study
demonstrated that the recovery of knee stability in ACL
reconstruction with the patellar tendon is higher (20%) than with
the semitendinosus and semimembranosus tendons
(19). Noyes et al(20) reported that the tensile strength of
the ACL is 100%, the central third B-P-B is 175%, the
semitendinosus tendon is 75% and the tensor fascia
lata tendon is 35%, in biomechanics. Toumi et
al(21) observed that the
mechanical stress distribution is asymmetric in the proximal end of
the PL and the inside section is stronger than the outside.
At present, adult cadaver articularis genus
samples have been used in a number of internal studies of ACL
length measurement and the values reported are different. The
Physical Investigation Committee of the Chinese Society for
Anatomical Science provided only the value of the ACL length and
previous MRI studies were case reports of abnormal PL. Olszewski
et al(22) observed that
the PL length was 43.33±4.21 mm in certain cases and Huang et
al(23) observed that the PL
length was 31.4–47.3 mm in 18 fresh knee specimens. Yoo et
al(24) discovered using MRI
that the PL length was 40.2±4.2 mm from the lower margin of the
patella to the tibial tubercle, the width was 30.3±2.7 mm from the
PL to the lower margin of the patella and the thickness was 3.2±0.5
mm. The authors also determined that the width was 24.0±2.8 mm from
the PL to the tibial tubercle and the thickness was 5.0±0.7 mm. In
the present study, the MRI results of the female PL were similar to
the results by Yoo et al and the MRI results of the male PL
were higher than those of the female; however, they were slightly
lower than the measurements made by Olszewski et al. A
reason for these differences may be that different materials were
used. The data in one study was measured by caliper rule with an
inherent error. Our study revealed that the PL and ACL lengths of
individuals aged 15–24 years were different from those of
individuals aged 25–64 years and ≥65 years. This difference may be
associated with the physical development of individuals aged 15–24
years, demonstrating the necessity for ligament data from different
ages to provide information for ACL reconstruction with allografts.
Brown et al(25) suggested
that PL and ACL length has no significant correlation with body
weight, height and gender and that the PL length is significantly
correlated with ACL length. The present study discovered that PL
and ACL length had no significant correlation with body weight and
height and the PL length was significantly correlated with ACL
length. However, we observed correlations between gender and PL and
ACL length.
One study suggested an ideal ‘equidistance’ status
between the tibia and femur attachment points in the graft, which
means that the distance between the two points remains fixed during
knee flexion and extension (26).
However, this theory is controversial and while a number of
scholars believe that there is such an isometric section in ACL
(27,28), others suggest that the ACL has no
absolute isometric fibers (29).
If the graft is not isometric, the graft is likely to undergo
elongation and relaxation with knee flexion and extension. Penner
et al suggested that permanent deformation would occur if
the elongation of the ligament was >5–6% (30). Therefore, ligament deformation
would occur when the length change of the graft is >2 mm in ACL
reconstruction. In order to ensure the graft length fit for ACL,
obtaining geometric data of the PL and ACL in the same age range
and the ratio of the two is necessary for clinicians to determine
the surgical program. The present study has provided this
information for clinical practice. There was no significant
difference of L1/L2 ratio in different ages and genders,
respectively.
According to the theory of ‘cruciate ligament as
four-bar linkage’ in knee kinematics, the anterior or posterior
cruciate ligament is always isometric regardless of the degree of
flexion and extension in the physiological range of the
articularis genus. Maintaining the isometric graft in knee
flexion and extension is an important biomechanical principle in
the ligament reconstruction and the isometric graft is determined
by the tunnel position of the femur and tibia. The location of the
bone tunnel is the key factor in ACL reconstruction. The present
study identified that the ratio of PL and ACL had no significant
differences between the left and right side of the body or between
males and females. Under conditions of ACL breakage and knee
instability, these data of normal PL and ACL length, and the ratio
of PL and ACL in the same age range are helpful to calculate the
tunnel length. The tunnel external aperture may be descended to
increase the tunnel gradient if the PL is too long. Following the
adjustment of the graft tension in the B-P-B, the epactal ligament
is likely to be reserved in the tibial tunnel and the bone block
will not go beyond the tunnel to affect the screw fixation, since
the femoral tunnel length is fixed. As a result, isometric fixation
and a stable joint may be achieved.
In summary, MRI was used to obtain geometric
parameters of in vivo PL and ACL for non-invasive and
accurate measurements. The database of PL and ACL lengths and the
ratio of the two was established by MRI in Han Chinese subjects of
different age ranges. In individuals aged 15–24 years, the values
in males were 43.95±4.25 mm, 38.45±4.62 mm and 1.15±1.09 and in
females were 42.03±0.94 mm, 36.00±1.06 mm and 1.18±0.11,
respectively. In individuals aged 25–64 years, the values in males
were 40.99±4.45 mm, 36.06±3.74 mm and 1.14±0.09 and in females were
39.84±0.64 mm, 36.50±0.81 mm and 1.11±0.02, respectively. In
individuals aged ≥65 years, the values in males were 41.43±3.08 mm,
36.62±3.44 mm and 1.15±0.09 and in females were 38.94±0.79 mm,
34.36±0.85 mm and 1.13±0.07, respectively. Our study achieves
non-invasive measurements in a large sample and supplies image data
of the articularis genus for use in surgery and sports
medicine.
Subjects aged <15 years were not enrolled in the
present study due to insufficient numbers; therefore, further study
is required to supply the measurement data for that age group.
References
|
1.
|
Huston LJ, Greenfield ML and Wojtys EM:
Anterior cruciate ligament injuries in the female athlete.
Potential risk factors. Clin Orthop Relat Res. 372:50–63. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Miyasaka KC, Daniel DM and Stone ML: The
incidence of knee ligament injuries in the general population. Am J
Knee Surg. 4:43–48. 1991.
|
|
3.
|
Chen DY, Jiang Q and Xu ZH: Comparison of
transverse and longitudinal incisions for B-T-B graft harvesting in
reconstruction of anterior cruciate ligament. Chinese Journal of
Sports Medicine. 27:78–80. 2008.(In Chinese).
|
|
4.
|
Noyes FR, Butler DL, Grood ES, Zernicke RF
and Hefzy MS: Biomechanical analysis of human ligament grafts used
in knee ligament repairs and reconstruction. J Bone Joint Surg Am.
66:344–352. 1984.PubMed/NCBI
|
|
5.
|
Augé WK II and Yifan K: A technique for
resolution of graft-tunnel length mismatch in central third
bone-patellar tendon-bone anterior cruciate ligament
reconstruction. Arthroscopy. 15:877–881. 1999.PubMed/NCBI
|
|
6.
|
Barber FA: Flipped patellar tendon
autograft anterior cruciate ligament reconstruction. Arthroscopy.
16:483–490. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Denti M, Bigoni M, Randelli P, et al:
Graft-tunnel mismatch in endoscopic anterior cruciate ligament
reconstruction. Intraoperative and cadaver measurement of the
intra-articular graft length and the length of the patellar tendon.
Knee Surg Sports Traumatol Arthrosc. 6:165–168. 1998. View Article : Google Scholar
|
|
8.
|
Mariani PP, Calvisi V and Margheritini F:
A modified bone-tendon-bone harvesting technique for avoiding
tibial tunnel-graft mismatch in anterior cruciate ligament
reconstruction. Arthroscopy. 19:E32003. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Physical Investigation Committee of the
Chinese Society for Anatomical Sciences: Anatomic Data for Chinese
People. People’s Medical Publishing House; Beijing, China: pp.
115–116. 2002
|
|
10.
|
McLoughlin RF, Raber EL, Vellet AD, Wiley
JP and Bray RC: Patellar tendinitis: MR imaging features, with
suggested pathogenesis and proposed classification. Radiology.
197:843–848. 1995. View Article : Google Scholar
|
|
11.
|
Bernicker JP, Haddad JL, Lintner DM,
DiLiberti TC and Bocell JR: Patellar tendon defect during the first
year after anterior cruciate ligament reconstruction: appearance on
serial magnetic resonance imaging. Arthroscopy. 14:804–809.
1998.
|
|
12.
|
Wakeley CJ, Johnson DP and Watt I: The
value of MR imaging in the diagnosis of the os trigonum syndrome.
Skeletal Radiol. 25:133–136. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Shalaby M and Almekinders LC: Patellar
tendinitis: the significance of magnetic resonance imaging
findings. Am J Sports Med. 27:345–349. 1999.PubMed/NCBI
|
|
14.
|
Chen W, Lu M, Wang J, et al: The
comparative study of the anterior cruciate ligament in oblique
coronal thin anatomical section and MRI. Chin J Radiol. 42:80–83.
2008.
|
|
15.
|
He CA, Lou LX, Guo Z, Liang W, Li XS and
Cheng XG: Length ratio of patellar tendon and patella measured on
MR images. Radiologic Practice. 6:670–672. 2008.
|
|
16.
|
Landis JR and Koch GG: The measurement of
observer agreement for categorical data. Biometrics. 33:159–174.
1977. View
Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Hadjicostas PT, Soucacos PN, Paessler HH,
Koleganova N and Berger I: Morphologic and histologic comparison
between the patella and hamstring tendons grafts: a descriptive and
anatomic study. Arthroscopy. 23:751–756. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Marder RA, Raskind JR and Carroll M:
Prospective evaluation of arthroscopically assisted anterior
cruciate ligament reconstruction. Patellar tendon versus
semitendinosus and gracilis tendons. Am J Sports Med. 19:478–484.
1991. View Article : Google Scholar
|
|
19.
|
Yunes M, Richmond JC, Engels EA and
Pinczewski LA: Patellar versus hamstring tendons in anterior
cruciate ligament reconstruction: A meta-analysis. Arthroscopy.
17:248–257. 2001. View Article : Google Scholar
|
|
20.
|
Noyes FR, Butler DL, Paulos LE and Grood
ES: Intra-articular cruciate reconstruction. I: Perspectives on
graft strength, vascularization, and immediate motion after
replacement. Clin Orthop Relat Res. 172:71–77. 1983.
|
|
21.
|
Toumi H, Higashiyama I, Suzuki D, et al:
Regional variations in human patellar trabecular architecture and
the structure of the proximal patellar tendon enthesis. J Anat.
208:47–57. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Olszewski AD, Miller MD and Ritchie JR:
Ideal tibial tunnel length for endoscopic anterior cruciate
ligament reconstruction. Arthroscopy. 14:9–14. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Huang HY and Liu JF: The length of
transfer cruciate ligament from patellar ligament and its
significance. Chinese Journal of Clinical Anatomy. 18:19–20.
2000.(In Chinese).
|
|
24.
|
Yoo JH, Yi SR and Kim JH: The geometry of
patella and patellar tendon measured on knee MRI. Surg Radiol Anat.
29:623–628. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Brown JA, Brophy RH, Franco J, et al:
Avoiding allograft length mismatch during anterior cruciate
ligament reconstruction: patient height as an indicator of
appropriate graft length. Am J Sports Med. 35:986–989. 2007.
View Article : Google Scholar
|
|
26.
|
Sidles JA, Larson RV, Garbini JL, Downey
DJ and Matsen FA III: Ligament length relationships in the moving
knee. J Orthop Res. 6:593–610. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
Sapega AA, Moyer RA, Schneck C and
Komalahiranya N: Testing for isometry during reconstruction of the
anterior cruciate ligament. Anatomical and biomechanical
considerations. J Bone Joint Surg Am. 72:259–267. 1990.PubMed/NCBI
|
|
28.
|
Arms SW, Pope MH, Johnson RJ, Fischer RA,
Arvidsson I and Eriksson E: The rehabilitation and biomechanics of
anterior cruciate reconstruction. Am J Sports Med. 12:8–18. 1984.
View Article : Google Scholar
|
|
29.
|
Zavras TD, Race A, Bull AM and Amis AA: A
comparative study of ‘isometric’ points for anterior cruciate
ligament graft attachment. Knee Surg Sports Traumatol Arthrosc.
9:28–33. 2001.
|
|
30.
|
Penner DA, Daniel DM, Wood P and Mishra D:
An in vitro study of anterior cruciate ligament graft placement and
isometry. Am J Sports Med. 16:238–243. 1988. View Article : Google Scholar : PubMed/NCBI
|