Introduction
Skin plasma cell hyperplasia is a rare chronic
disease characterized by skin lesions, superficial lymphadenopathy
and polyclonal hypergammaglobulinemia. Rashes often appear as
rufous rashes, papules, nodules and plaques accompanied by pruritus
(1). The etiology and pathogenesis
of this disease are not clear. The histopathological manifestation
is mature plasma cell infiltration in the shallow-to-deep dermis
and around the adnexa without clear abnormalities. There is no
definitively effective method available for the treatment of this
disease. A case was cured by the oral administration of acitretin
and intramuscular injection of interferon and is reported as
follows.
Case report
Patient diagnosis
The patient was a 51-year-old male whose lateral
femur of the right lower limb was injured 4–5 years earlier. In the
2 months following the trauma, local papules of sizes between 1–3
mm appeared and increased gradually to merge into infiltrative
plaques. In the last year, the infiltrative plaques had noticeably
extended. The patient was examined at the outpatient service of the
Second Hospital (Jilin University, Changchun, China) and was
suspected of having mycosis. The present study was conducted in
accordance with the Declaration of Helsinki and with approval from
the Ethics Committee of the Second Hospital, Jilin University.
Written informed consent was obtained from the patient. Following
the administration of the oral antifungal agent Lanmeishu
(terbinafine hydrochloride) at a dose of 250 mg/day for 1.5 months,
the erythema was not improved. Therefore, the patient was
transferred to another hospital for exeresis. According to the
pathology, the patient was diagnosed with tuberculosis. Following
anti-tuberculosis treatment for 3 months (0.6 g/day rifampicin and
300 mg/day isoniazid orally; and 0.75 g/day streptomycin
administered by intramuscular injection for 2 weeks and thereafter
by intramuscular injection twice/week), the skin lesions were not
improved. Instead, perioral and abdominal papules and tubercles of
sizes between 1–3 mm, the surgical resection site exhibited
infiltrated erythema and dark red tubercles appeared at the edge of
the surgical site. For further diagnosis and treatment, the patient
was examined at the Second Hospital, Jilin University on November
25, 2004.
According to a physical examination, the general
situation was good and the right inguinal lymph node between 5–7
mm. The patient’s routine blood, routine urine and liver function
test results were normal. The rapid plasma reagin (RPR) test and
fungal culture of the tissues were negative. An electrocardiogram
and chest X-ray showed no abnormality and neither did bone marrow
aspiration. The patient’s serum IgG was 27.80 g/l (normal range,
7.230–16.850 g/l), while IgA, IgM and complement C3 and C4 levels
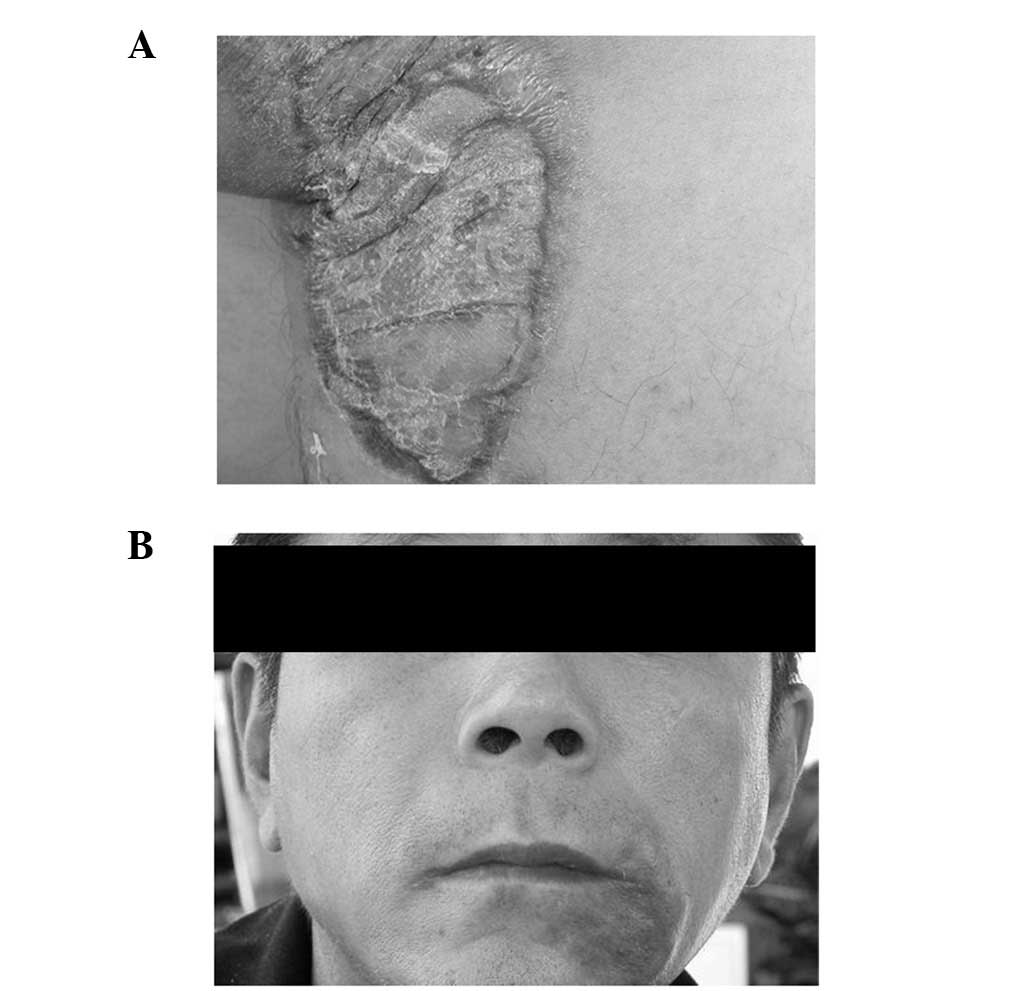
were in the normal range. A dermatological examination revealed a
scar of 8×18 cm at the lateral femur of the right lower limb. At
the center and edge of the scar, infiltrated erythema, tubercles
and slight red swelling were observed (Fig. 1A). At the abdomen, there were 5–6
papules and tubercles sized between 1–3 mm. At the left lateral
perioral region, dense light-red papules of sizes between 1–3 mm,
partially fused papules and clear basal infiltration were visible
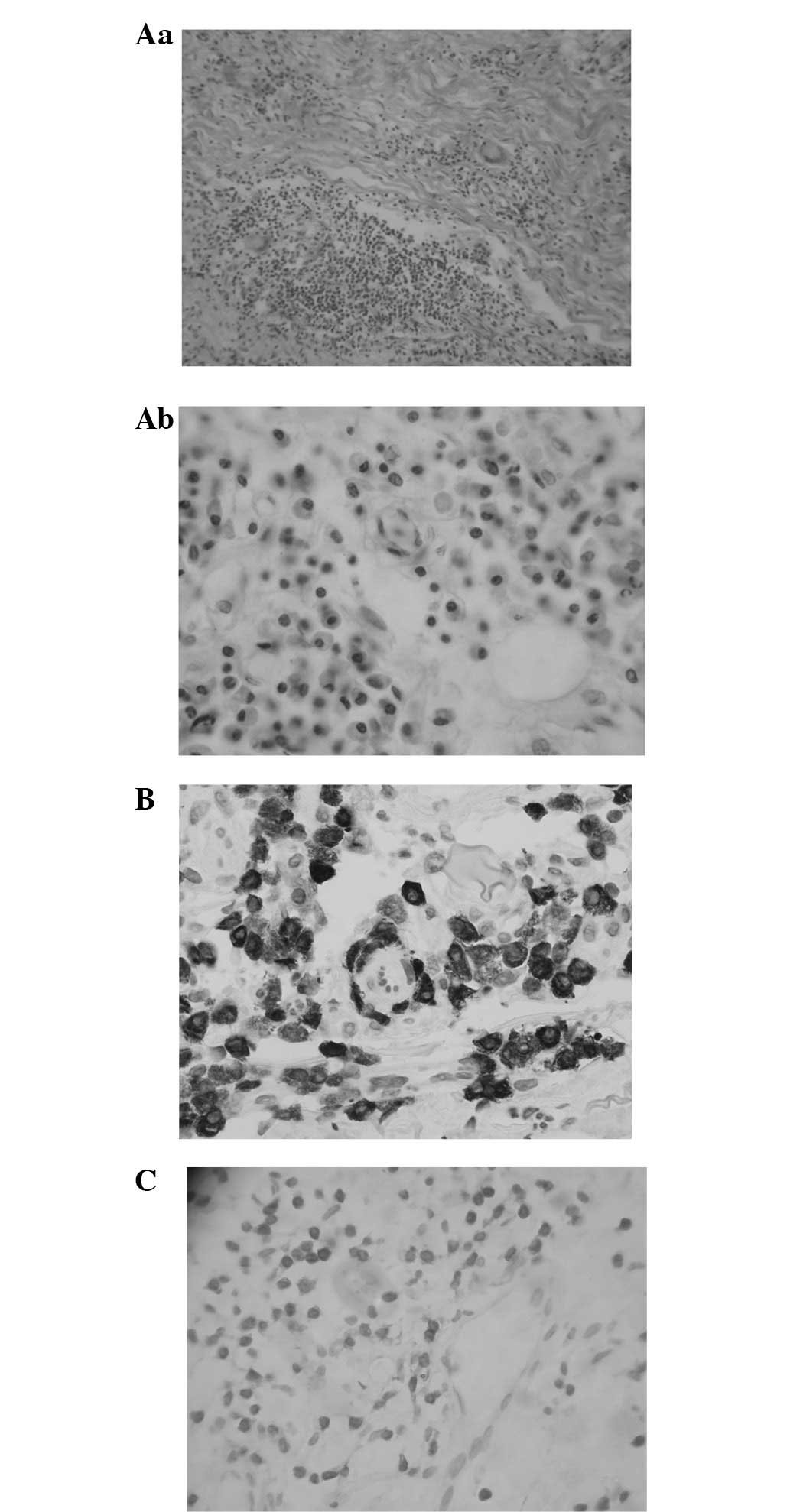
(Fig. 1B). Histopathological
examination showed dense mature plasma cell-dominant inflammatory
cell infiltration in the deep dermis and between part of
subcutaneous tissues, and small numbers of lymphocytes and
polykaryocytes (Fig. 2A). In
addition, immunopathologenetic analysis showed that the infiltrated
plasma cells were CD79a and CD138 positive (Fig. 2B and C). Consequently, the patient
was clinically diagnosed with cutaneous plasmacytosis.
Treatment process
Intramuscular injections of interferon at 1 million
U/day and oral dosages of triamcinolone (fluoxyprednisolone) at 16
mg/day were administered. Triamcinolone was administered for 1
month and interferon was administered for ∼3 months. Over this
time, the color of the erythema on the thigh lightened, the texture
softened and the dark-red tubercles at the edge disappeared. Also,
the abdominal tubercles disappeared completely. Subsequently,
interferon at 1 million U/day was continuously administered by
intramuscular injection for 6 months. Additionally, the oral
administration of acitretin capsules was performed for 3 months but
was then discontinued due to dry mouth and stomach discomfort. At
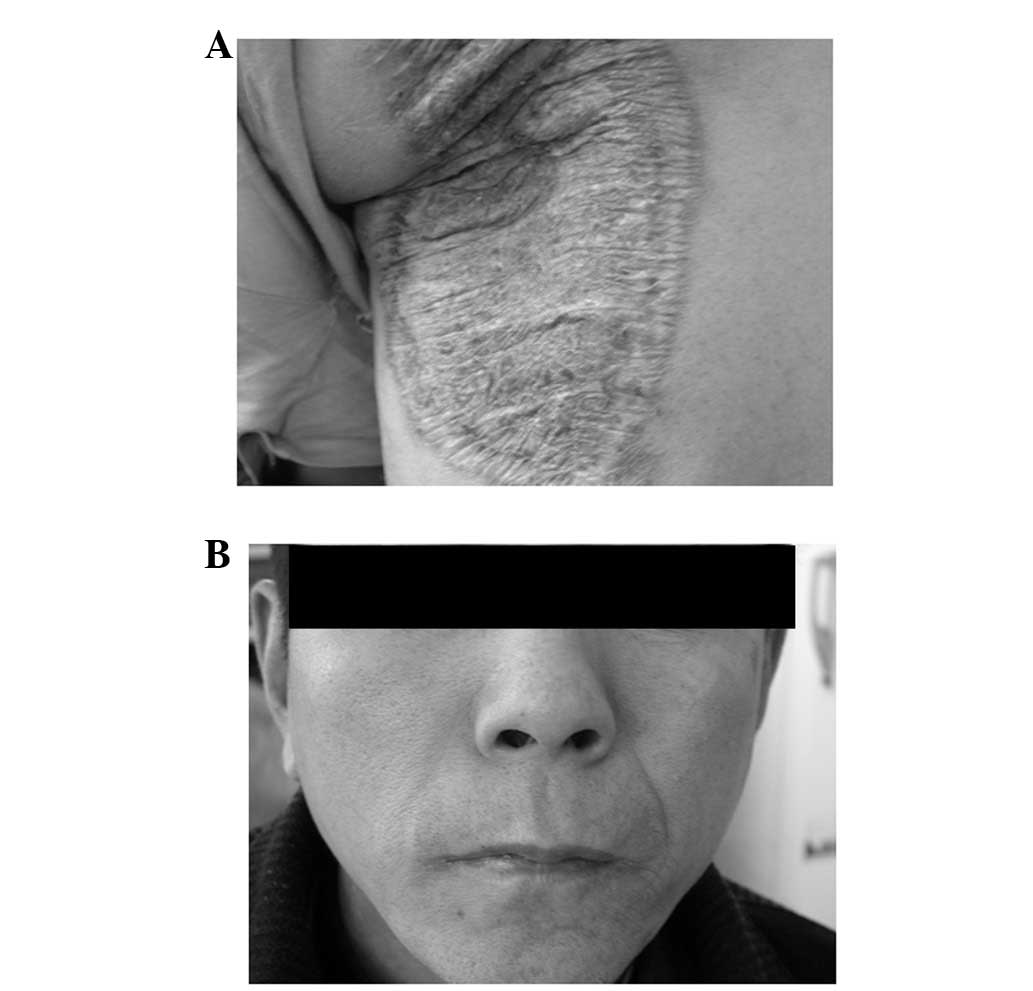
the right lateral femur, only the surgery scar remained and no
infiltrative erythema or inflammatory tubercles were observed. The
perioral and abdominal erythema also disappeared completely
(Fig. 3A and B) and the erythema
did not recur in the 1.5 year follow-up.
Discussion
Cutaneous plasmacytosis is a rare benign mature
plasma cell proliferation disorder, commonly occurring in
middle-aged and elderly individuals in Asian populations,
particularly in Japan (2,3). The male to female incidence ratio is
1:0.6, age of incidence is between 20 and 62 years old and median
incidence age is 37 years old. The incidence rate of lymph node
disease is 38% and the incidence rate of polyclonal
hypergammaglobulinemia is 93% (3).
The disease has also been observed in countries other than Japan,
including China (4). Its clinical
manifestations include multiple erythema, from dark-red to purplish
red in color, which may fuse. Also, polyclonal immunoglobulin
hyperplasia usually appears. Histopathological changes manifest as
dense mature plasma cell-dominant inflammatory cell infiltration
which appears in the deep dermis and between part of subcutaneous
tissues and the infiltrated cells are not atypical. This is
accompanied by infiltration of lymphocytes and histiocytes
(5). In the clinic, it must be be
differentiated from plasma cell-dominant granulomatous disease and
cutaneous plasmacytoma. For the present patient, the syphilis serum
reaction was negative, fungal culture showed negative results and
anti-tuberculosis and antifungal therapies were ineffective.
Therefore, deep mycosis, syphilis and tuberculosis were excluded.
In addition, the pathologically infiltrated cells were mature
plasma cells without atypia and bone marrow aspiration showed no
abnormality. Consequently, primary and secondary cutaneous
plasmacytoma were also excluded. According to clinical and
pathological examinations and the presence of inguinal
lymphadenectasis and hypergammaglobulinemia, the cutaneous
plasmacytosis diagnosis was correct. There is no definitive and
conclusive method for the treatment of this disease at present. In
China, Lin (4) reported that the
treatment of a case of cutaneous plasmacytosis with corticosteroids
and azathioprine had an unsatisfactory effect. Furthermore, there
have been studies on the application of phototherapy (6) and topical tacrolimus ointment
(7) in the treatment of this
disease where more satisfactory results were achieved. After the
present patient received oral administrations of triamcinolone
tablets and acitretin capsules for one month and interferon by
intramuscular injection for 9 months, the skin lesions were cured.
Reexamination showed that the serum immunoglobulin levels were all
within the normal range. In the 4-year follow-up, no skin lesions
recurred and a clinical cure was achieved. Consequently, the
present case may be used for future reference.
References
|
1
|
Haque M, Hou JS, Hisamichi K, Tamada K,
Cusack CA, Abdelmalek M, Brown RE and Vonderheid EC: Cutaneous and
systemic plasmacytosis vs. cutaneous plasmacytic castleman disease:
review and speculations about pathogenesis. Clin Lymphoma Myeloma
Leuk. 11:453–461. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jayaraman AG, Cesca C and Kohler S:
Cutaneous plasmacytosis: A report of five cases with
immunohistochemical evaluation for HHV-8 expression. Am J
Dermatopathol. 28:93–98. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Uhara H, Saida T, Ikegawa S, et al:
Primary cutaneous plasmacytosis: report of three cases and review
of the literature. Dermatology. 189:251–255. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lin BZ: Cutaneous plasmacytosis: A case
report. J Clinical Dermatology. 5:313–314. 1995.
|
|
5
|
López-Estebaranz JL, Rodriguez-Peralto JL,
Ortiz Romero PL, Vanaclocha F and Iglesias Díez L: Cutaneous
plasmacytosis: report of a case in a white man. J Am Acad Dermatol.
31:897–900. 1994.PubMed/NCBI
|
|
6
|
Tzung TY, Wu KH, Wu JC and Tseng HH:
Primary cutaneous plasmacytosis successfully treated with topical
photodynamic therapy. Acta Derm Venereol. 85:542–543.
2005.PubMed/NCBI
|
|
7
|
Miura H, Itami S and Yoshikawa K:
Treatment of facial lesion of cutaneous plasmacytosis with
tacrolimus ointment. J Am Acad Dermatol. 49:1195–1196. 2003.
View Article : Google Scholar : PubMed/NCBI
|