Introduction
Benign prostate hyperplasia (BPH) is one of the most
common diseases affecting the health of aging males. The incidence
rate of benign prostatic hyperplasia has been the highest in recent
years and represents the aging trend (1). A study by Roehrborn et al
recorded the histological prevalence of BPH based on a review of
five studies relating age to histological findings in human male
prostate glands (2). A palpable
enlargement of the prostate has been identified in up to 20% of
males in their 60s and in 43% of males in their 80s (3). Transurethral resection of the
prostate (TURP) is presently the most common active treatment for
BPH and has been established as the gold standard surgical
procedure (4), however, the
overall complication morbidity rate of TURP is comparatively high.
To minimize the perioperative morbidity of TURP, various minimally
invasive alternatives, including laser techniques, were introduced
to clinical practice in an effort to reduce treatment-related
complications (5). Compared with
TURP, transurethral laser resection of the prostate (TULRP) has
several advantages, including a lower incidence of complications, a
minimal risk of bleeding or requirement for blood transfusion, a
decreased risk of water intoxication and decreased urethral
sphincter damage (6). Laser
prostatectomy by Holmium laser enucleation of the prostate (HoLEP)
has been introduced and promoted by Fraundorfer and Gilling over
the last decade (7). High-powered
holmium lasers have been used for the ablation and resection of the
prostate due to their excellent incisional, ablative and hemostatic
properties. The development of the transurethral tissue morcellator
has allowed the rapid removal of prostatic tissue without size
limitations on the prostatic gland. However, the HoLEP technique is
difficult to master as it has a steep learning curve and longer
surgery duration.
The 2-μm (thulium) laser resection of the
prostate-tangerine technique (TmLRP-TT) is a transurethral
procedure that uses a thulium laser fiber to dissect whole
prostatic lobes off the surgical capsule, similar to when
dissecting a tangerine. Since 2006, >600 surgical cases have
been carried out in the PLA General Hospital (Beijing, China). When
compared with TURP, TmLRP-TT has a number of advantages, including
improved spatial beam quality, more precise tissue incisions and
the ability to operate in optional continuous or pulse-wave modes
(8).
The objective of the present study was to evaluate
the results for the clinical application of the 2-μm
continuous wave (cw) laser in transurethral vaporesection of the
prostate.
Patients and methods
Patients
Between May 2007 and May 2008, a total of 115
symptomatic BPH patients from the PLA General Hospital were
enrolled in the present study. This clinical trial was registered
in PLA General Hospital, the Ethics committee approved this study
and all patients signed a written informed consent form. All works
were undertaken following the provisions of the Declaration of
Helsinki. Their symptoms were evaluated according to the
International Prostate Symptom Score (IPSS) and the quality of life
(QoL) score. All patients underwent prostate-specific antigen
(PSA), hemoglobin, urine and rectal examinations. The peak volume
of the urinary flow rate (Qmax) and the post-void residual urine
volume (PVR) were recorded and the patients with a PSA level of
>4 μg/l were subjected to a pre-operative prostate
biopsy.
The patients were divided into 2 groups according to
their prostate volume. The groups consisted of those with prostate
volumes of ≤80 ml (n=85) and those with prostate volumes of >80
ml (n=75). The assessed outcomes of the present study were the test
parameters of the patients and the surgical parameters of the
procedures. These parameters were compared prior to and
post-surgery within and between the two groups. The baseline
characteristics of the patient data are presented in Table I.
 | Table IBaseline characteristics data in
patients with BPH. |
Table I
Baseline characteristics data in
patients with BPH.
| Prostate volume
|
|---|
| Characteristics | ≤80 ml | >80 ml |
|---|
| Patients (n) | 80 | 75 |
| Patients with acute
urinary retention (n) | 12 | 9 |
| Patients with bladder
stones (n) | 8 | 4 |
| Mean prostate volume
(ml) | 63.4±13.6 | 123.7±26.7 |
| Median age
(years) | 72.0±7.2 | 72.5±9.1 |
| Median duration of
urinary tract obstruction (years) | 6.3±1.5 | 6.4±1.8 |
The test parameter indices, including PVR, Qmax,
IPSS and QoL, were also recorded prior to the surgery and at 6 and
12 months post-surgery. The blood sodium concentration (BSC) and
the hemoglobin concentration (HGC) were also measured to assess
each patient’s physical condition.
Equipment
A 2-μm (thulium) laser with a rated output
power of 70 W (LISA Laser Products OHG, Katlenburg-Lindau, Germany)
was used in the cw mode throughout the procedure. The energy was
delivered through 550-μm RigiFib fibers. The laser fibers
were introduced through a continuous flushing excision mirror.
Saline irrigation was used in all the cases, with the surgery being
observed via a television monitor.
Surgical steps
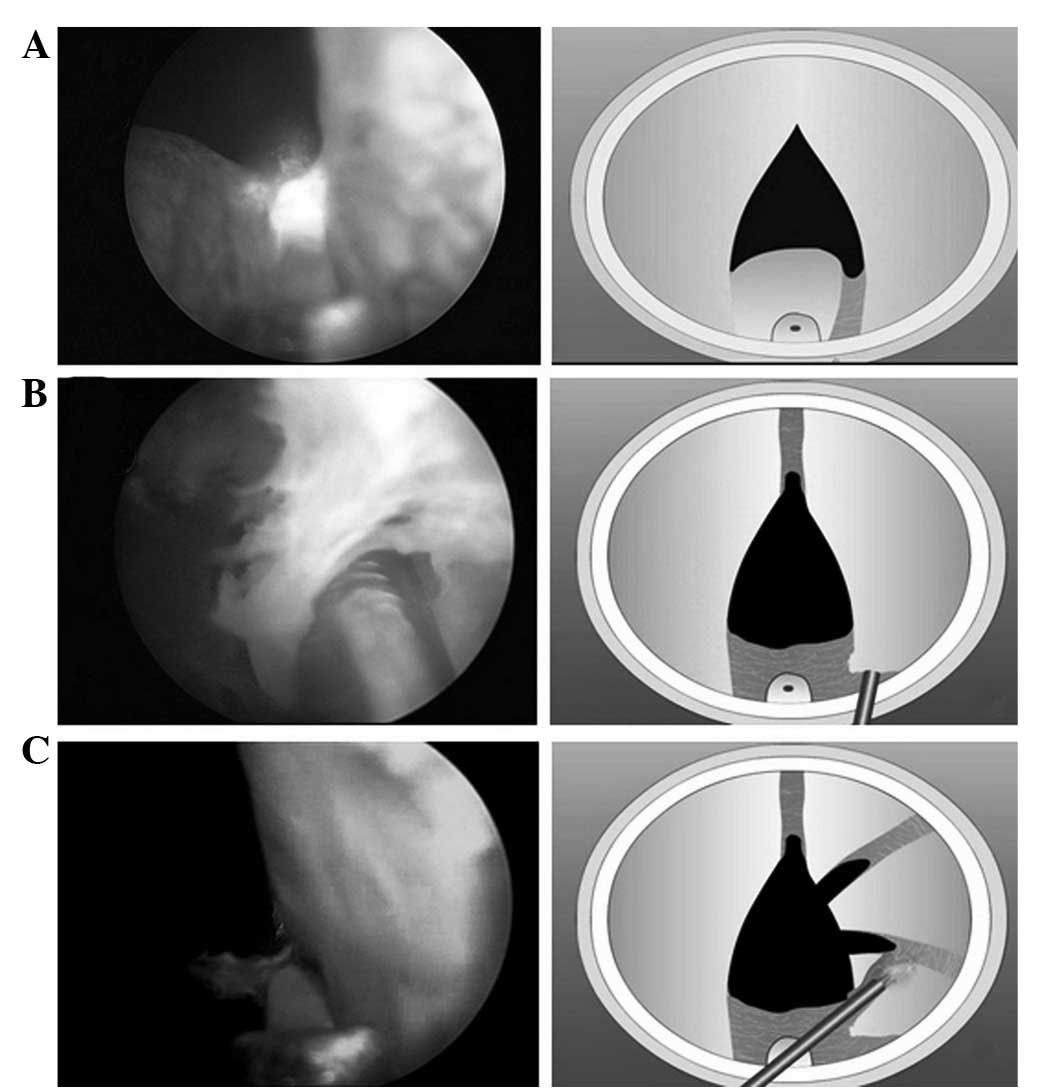
Step 1.The surgical technique was similar to
other resection procedures. Following initial incisions at 5
o’clock, 7 o’clock and 12 o’clock at the bladder neck,
vaporesection of the median lobe was initiated (Fig. 1A).
Step 2. The fibre was moved
semi-circumferentially from the verumontanum in the direction of
the bladder neck, thereby undermining the tissue and cutting
chips.
It was important to cut small sections that did not
exceed the size of the inner sheath diameter so that the tissue
sections were washed out without morcellation at the end of the
procedure.
Step 3. Following the resection of the middle
lobe of the prostate, the lateral lobes were removed in a
retrograde fashion beginning at the verumontanum so that the
external sphincter was preserved in the best way (Fig. 1B).
Step 4. Vaporesection of the lateral lobes
was continued until in close proximity to the surgical prostatic
capsule (Fig. 1C).
At the end of the procedure, the resected tissue
chips were removed and a urinary catheter was inserted into the
bladder. The suprapubic bladder puncture fistulation tubes were
then removed.
Post-operative management
Peripheral blood samples were obtained from the
patients to determine the BSC and HGC. The resected tissues were
then weighed and urination and other data were recorded.
Statistical analysis
Data are presented as mean ± SD to compare the
continuous variables of Qmax, IPSS, QoL and PVR prior to and
post-surgery. P<0.05 was considered to indicate a statistically
significant difference. The SPSS software package was used to
perform the statistical tests. An analysis of correlation and
regression equation was used.
Results
No significant bleeding or changes in the hematocrit
were observed at any stage of the procedure, suggesting that the
TmLRP-TT technique was an almost bloodless procedure. No
intraoperative complications occurred. Compared with the baseline
(pre-surgery) data, there were no significant improvements in the
blood sodium and hemoglobin concentrations. In the group with a
prostate volume of ≤80 ml, 23 patients required bladder flushing
which ceased 24 h post-surgery. The median catheter indwelling time
post-surgery was 3 days (range, 1–5 days). Acute urinary retention
occurred in 5 patients 24 h subsequent to the removal of the
catheter and emergency microscopic examinations revealed that this
was caused by prostate tissue fragment obstructions. The median
duration of hospitalization in these patients was 5 days (range,
1–7 days). A secondary hemorrhage occurred in 2 patients on the
25th and 28th day post-surgery. They each received a blood
transfusion of 400 ml and following catheter indwelling and bladder
flushing, the hemorrhage stopped. Stress urinary incontinence
occurred post-surgery in 4 patients; they all recovered subsequent
to receiving acupuncture and functional exercise treatments for 3
months. Anterior urethral strictures occurred in 2 patients at 3
months post-surgery; their emiction function recovered subsequent
to receiving urethral dilation and urethroplasty separately. A
post-operative histopathological examination identified that one of
these patients had prostate cancer (Fig. 2).
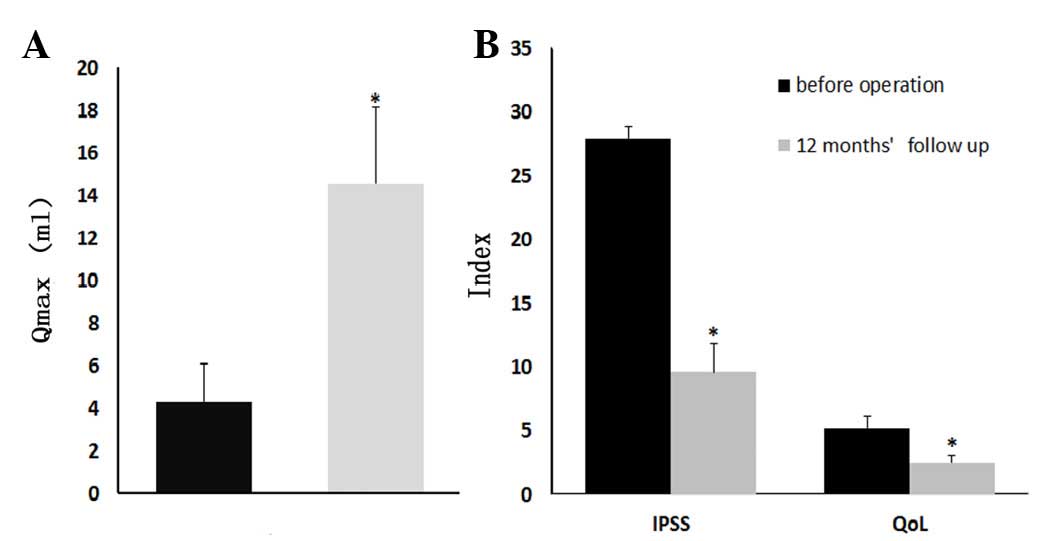
In the patients with a prostate volume of >80 ml,
there were significant improvements in the test parameters,
including the IPSS, QoL scores, Qmax and PVR urine volume. Compared
with the mean vaporization resection time of the ≤80 ml group
(76.0±26.8 min), the resection time was longer at 95.0±13.2 min and
the mean surgical clearance volume was 75.4±16.4 g (compared with
18.19±7.95). There was no sigificant difference in the
post-operative urinary catheter indwelling time or the length of
hospital stay in the two groups (shown in Table II). In total, 4 patients developed
urge incontinence and 5 patients developed secondary anterior
urethral strictures for which they all received the appropriate
treatment. The test parameters of the two patient groups and the
results of the 6-month and 1-year follow-ups are shown in Table II.
 | Table IIStatistical analysis results of
TmLRP-TT in patients with benign prostatic hyperplasia (BPH). |
Table II
Statistical analysis results of
TmLRP-TT in patients with benign prostatic hyperplasia (BPH).
| Prostate volume ≤80
ml | Prostate volume
>80 ml |
|---|
|
|
|---|
| Parameter | Pre-surgery | 6 months | 12 months | Pre-surgery | 6 months | 12 months |
|---|
| Test parameter | | | | | | |
| PSA (ng/ml) | 3.8±0.9 | 3.0±1.0 | 2.6±1.3 | | | |
| Qmax (ml/sec) | 7.2±2.7 | 18.9±3.5 | 20.1±4.4a | 4.3±1.8 | 9.5±2.6 | 14.54±3.6a |
| IPSS | 25.3±4.5 | 6.9±3.6 | 4.4±2.6a | 27.9±6.5 | 12.3±4.2 | 9.6±2.3a |
| QoL | 4.2±1.0 | 1.8±1.3 | 1.3±0.9a | 5.2±0.5 | 3.1±0.8 | 2.5±0.6a |
| PVR (ml) | 147.4±60.1 | 43.5±20.0 | 41.6±12.7a | 115.3±35.2 | 38.9±16.7 | 32.0±15.1a |
| Surgical
parameter | | | | | | |
| Average time for
vaporization resection (min) | | 76.0±26.8 | | | 95.0±13.2 | |
| Average cutting
prostate tissue volume (g) | | 18.19±7.95 | | | 75.4±16.4 | |
| Post-operative
urinary catheter indwelling time (days) | | 3.0±0.9 | | | 3.3±0.9 | |
| Length of hospital
stay (days) | | 3.9±1.6 | | | 4.8±1.8 | |
The statistical analysis results revealed that when
compared with the data recorded pre-surgery, the IPSS, QoL score,
Qmax and PVR values were significantly improved within each group
(P<0.05), but that there was no statistically significant
difference between the groups.
Discussion
Advances in laser technology have led to the
development of new laser treatments. HoLEP or green light laser
photo-selective vaporization of the prostate (PVP) are new laser
prostatectomies that require a shorter inpatient hospitalization
period, cause fewer short-term adverse events and result in less
bleeding than TURP (9). However,
until the effectiveness of the holmium laser and the handling and
safety properties of the green-light laser are combined, an ideal
laser cannot be identified. The 2-μm cw laser vaporesection
of the prostate has been established as a new technology for the
treatment of BPH (10–12). The RevoLix cw laser is a new
surgical laser at a wavelength of 2013 nm or ∼2 μm. The
2-μm cw laser may have several advantages over other laser
procedures as it has an improved spatial beam quality, operates in
cw pulse modes, is capable of more rapid vaporization, makes
precise incisions in the prostate tissue and uses normal saline as
the irrigation fluid. The most significant difference is that its
energy is delivered as a cw rather than a pulsed wave (13).
The surgeon uses the output end of the fiber in a
reciprocating motion that follows a ‘U’ shape when operating the
conventional 2-μm laser; this technique is difficult with a
steep learning curve, longer surgical time and a relatively low
removal efficiency. This has been improved by split-vaporization
resection of the prostate; this has the technical characteristics
of a ‘W’-shaped superficial vaporization mark trench, multiple
segmentation, a scanning type vaporization, a thin layer resection
plus stripping and vaporization dressing of the wounds, resulting
in an efficient and safe surgical mode.
Resection with the 2-μm cw laser allows
TURP-like chips of tissue to be cut and the resection time to be
shortened as a result of using the simultaneous vaporization
component of the laser. The efficient hemostasis and improved
vision from the 2-μm cw laser treatment of BPH may reduce
bleeding and surgical risk. Therefore, the advantages of the
2-μm cw laser vaporesection procedure are that it is a safe,
efficient, bloodless and promising surgical procedure for the
treatment of BPH (14). The
experience and results gained by the present study from the 6- and
12-month follow-up of 155 patients showed that the vaporization
resection method for treating BPH patients is reliably safe and
that the post-operative indices, including the IPSS, QoL and Qmax,
were significantly improved compared with those prior to surgery.
These results are similar to other previous studies (15–17).
Transurethral evaporation and visual laser ablation of the prostate
were effective in relieving the symptoms of benign prostatic
hyperplasia (18).
Strong biological tissue vaporization is the
prominent characteristic of the 2-μm laser (19). In this study, we acquired positive
correlation between the collected prostatic tissue quality and the
prostate gland specimen quality (data not shown), thus proved using
2-μm laser enable manipulation and destruction of biological
tissue of BPH with unprecedented precision and selectivity.
The most noteworthy findings in the present study
were the observations that patients undergoing transurethral
vaporesection of the prostate using the 2-μm laser had a
decreased rate of repeat surgeries and were 3 times more likely to
have a decreased peak volume of urinary flow rate (7.2±2.7 versus
20.1±4.4, respectively, P<0.01), this shows the superiority of
2-μm laser vaporesection in the treatment of BPH.
References
|
1
|
Wu SL, Li NC, Xiao YX, et al: Natural
history of benign prostate hyperplasia. Chin Med J (Engl).
119:2085–2089. 2006.PubMed/NCBI
|
|
2
|
Roehrborn CG, Issa MM, Bruskewitz RC, et
al: Transurethral needle ablation for benign prostatic hyperplasia:
12-month results of a prospective, multicenter U.S. study. Urology.
51:415–421. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
de la Rosette JJ, de Wildt MJ, Alivizatos
G, Froeling FM and Debruyne FM: Transurethral microwave
thermotherapy (TUMT) in benign prostatic hyperplasia: placebo
versus TUMT. Urology. 44:58–63. 1994.PubMed/NCBI
|
|
4
|
Madersbacher S, Alivizatos G, Nordling J,
Sanz CR, Emberton M and de la Rosette JJ: EAU 2004 guidelines on
assessment, therapy and follow-up of men with lower urinary tract
symptoms suggestive of benign prostatic obstruction (BPH
guidelines). Eur Urol. 46:547–554. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gupta N, Sivaramakrishna, Kumar R, Dogra
PN and Seth A: Comparison of standard transurethral resection,
transurethral vapour resection and holmium laser enucleation of the
prostate for managing benign prostatic hyperplasia of >40 g. BJU
Int. 97:85–89. 2006.
|
|
6
|
Kuntz RM: Current role of lasers in the
treatment of benign prostatic hyperplasia (BPH). Eur Urol.
49:961–969. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fraundorfer MR and Gilling PJ: Holmium:
YAG laser enucleation of the prostate combined with mechanical
morcellation: preliminary results. Eur Urol. 33:69–72. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fried NM and Murray KE: High-power thulium
fiber ablation of urinary tissues at 1.94 microm. J Endourol.
19:25–31. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Araki M, Lam PN and Wong C: High-power
potassium-titanyl-phosphate laser photoselective vaporization
prostatectomy for symptomatic benign prostatic hyperplasia. J
Endourol. 22:1311–1314. 2008. View Article : Google Scholar
|
|
10
|
Fu WJ, Hong BF, Yang Y, et al: Two micron
continuous wave laser vaporesection for the treatment of benign
prostatic hyper-plasia. Asian J Androl. 10:341–342. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fu WJ, Hong BF, Yang Y, et al:
Vaporesection for managing benign prostatic hyperplasia using a
2-microm continuous-wave laser: a prospective trial with 1-year
follow-up. BJU Int. 103:352–356. 2009.PubMed/NCBI
|
|
12
|
Luo GH, Xia SJ and Sun ZL: In vitro
comparison of the vapore-section of human benign prostatic
hyperplasia using 70- and 120-W 2-μm lasers. Asian J Androl.
13:636–639. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fu WJ, Zhang X, Yang Y, et al: Comparison
of 2-microm continuous wave laser vaporesection of the prostate and
transurethral resection of the prostate: a prospective
nonrandomized trial with 1-year follow-up. Urology. 75:194–199.
2010.PubMed/NCBI
|
|
14
|
Pal RP and Khan MA: Intermediate-term
efficacy of Tm: YAG laser prostate vaporesection for bladder outlet
obstruction: initial experience from a UK teaching hospital. Urol
Int. 88:39–42. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Malek RS, Kuntzman RS and Barrett DM:
Photoselective potassium-titanyl-phosphate laser vaporization of
the benign obstructive prostate: observations on long-term
outcomes. J Urol. 174:1344–1348. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Elzayat EA and Elhilali MM: Laser
treatment of symptomatic benign prostatic hyperplasia. World J
Urol. 24:410–417. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Vavassori I, Hurle R, Vismara A, Manzetti
A and Valenti S: Holmium laser enucleation of the prostate combined
with mechanical morcellation: two years of experience with 196
patients. J Endourol. 18:109–112. 2004.PubMed/NCBI
|
|
18
|
Xia SJ: Two-micron (thulium) laser
resection of the prostate-tangerine technique: a new method for BPH
treatment. Asian J Androl. 11:277–281. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bach T, Herrmann TR, Ganzer R, Burchardt M
and Gross AJ: RevoLix vaporesection of the prostate: initial
results of 54 patients with a 1-year follow-up. World J Urol.
25:257–262. 2007.PubMed/NCBI
|