Introduction
Neonatal hypoxic-ischemic encephalopathy (HIE) is
caused by a variety of conditions, including partial or complete
hypoxia, cerebral blood flow reduction and suspension-induced
neonatal brain injury caused by perinatal asphyxia (1,2). HIE
is common during the neonatal period in which the incidence rate is
1–2 per 1,000 cases. It has been reported that 15–20% of children
succumb to HIE during the neonatal period and 15–20% of the
survivors suffer from permanent neurological deficits, including
cerebral palsy and mental retardation (3,4).
Although extensive studies on HIE have been performed, an effective
therapy remains to be found (5,6).
Inflammation is one of the main causes of
hypoxic-ischemic brain damage (7,8), and
tumor necrosis factor-α (TNF-α) is one of the most important
proinflammatory cytokines. Numerous studies have shown that the
expression of TNF-α in the brain rapidly increases following
cerebral ischemia (9,10). Activated TNF-α further stimulates
the phagocytosis of immune cells and the activated immune cells
further stimulate the germination of TNF-α and other substances,
including radicals, extracellular matrix proteases, complement
factors and cell adhesion molecules. These ultimately induce a
variety of biological responses, including tissue damage, shock and
apoptosis (11,12).
Ischemia-induced nuclear factor-κB (NF-κB) has a
coordinating function in the expression and regulation of
proinflammatory genes, which includes responding quickly to a
variety of inflammatory stimuli, activating the transcription of a
variety of downstream inflammatory genes and holding the central
position in the inflammatory response (13,14).
NF-κB is the promoter and enhancer of a number of inflammatory
mediator genes, including TNF-α, as it contains κB sites that are
able to regulate the induction and expression of inflammatory genes
(15). This is an important signal
for the inflammatory cascade reaction to mediate cerebral ischemia
reperfusion. Therefore, inhibiting the cascade reaction of
inflammatory injury may reduce cell death, gliosis, edema and
apoptosis, indicating that NF-κB has an important function in
hypoxic-ischemic brain injury.
Progesterone (PROG) has been shown to protect brain
tissues against hypoxic-ischemic brain damage (16–18).
Studies on the cerebral protective effects of PROG by Li et
al demonstrated the effects of PROG in reducing edema following
brain injury, which included reducing calcium overload and
inhibiting neuronal apoptosis (19–21).
Previous studies concerning the protective effects of PROG in the
brain have focused on adult rats. Therefore, the present study
explored the involvement of TNF-α and NF-κB in the neuroprotective
mechanisms of PROG in a neonatal rat model of hypoxic-ischemic
brain injury.
Materials and methods
Animals and grouping
A total of 30 Wistar rats, aged 7 days and weighing
14.1±2.0 g, were provided by Xinxiang Medical Experimental Animal
Center (Xinxiang, China). The rats were randomly divided into three
groups with 10 rats in each group. In the sham group, neck
incisions were performed without hypoxic-ischemic treatment. In the
hypoxic-ischemic (model) group, hypoxic-ischemic treatment was
performed, in order to establish animal models. In the drug
prevention (PROG) group, the animals were administered 8 mg/kg PROG
solution intraperitoneally 30 min prior to the induction of
hypoxia-ischemia (21). PROG was
purchased from Sigma-Aldrich (batch 0130; St. Louis, MO, USA). The
solution was mixed with 0.5 mg/ml sesame oil prior to use. The
study was carried out in strict accordance with the recommendations
in the Guide for the Care and Use of Laboratory Animals of the
National Institutes of Health (Eighth edition, 2011). The animal
use protocol was reviewed and approved by the Institutional Animal
Care and Use Committee of Xinxiang Medical University (Xinxiang,
China).
Animal model preparation
As described previously (22,23),
newborn Wistar rats were anesthetized with 5% isoflurane. The left
common carotid artery was isolated and ligated with a silk thread.
Following recovery and feeding for 2 h, rats without rotary motion
were separated. The remaining rats were placed in a closed
container at 37°C with 8% O2 and 92% N2
introduced at 1.5 l/min for 2.5 h to induce hypoxia-ischemia.
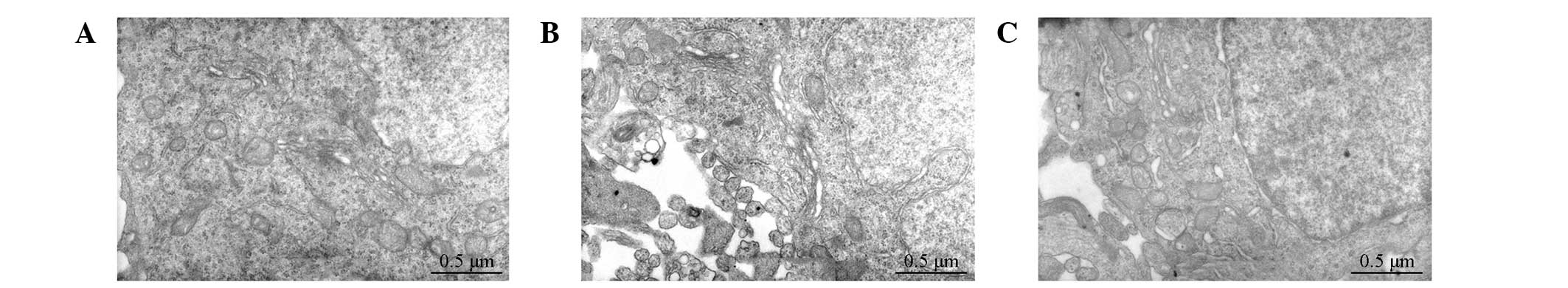
Ultrastructural changes of the
hippocampus in the experimental groups
Following the induction of hypoxia-ischemia for 24
h, the brains of three rats from each group were quickly placed in
2.5% glutaraldehyde at 4°C for 4 h for fixing. The brains were then
rinsed with phosphate-buffered saline and fixed again with 1%
osmium tetroxide for 1.5 h. Next, the brains were washed with
distilled water, dehydrated with a gradient series of ethanol and
acetone, embedded in epoxy resin and cut into ultrathin sections.
The ultrastructures of the hippocampal neurons were electron
stained and then, using a Hitachi H-7500 transmission electron
microscope (Hitachi, Ltd., Tokyo, Japan), were observed and images
captured.
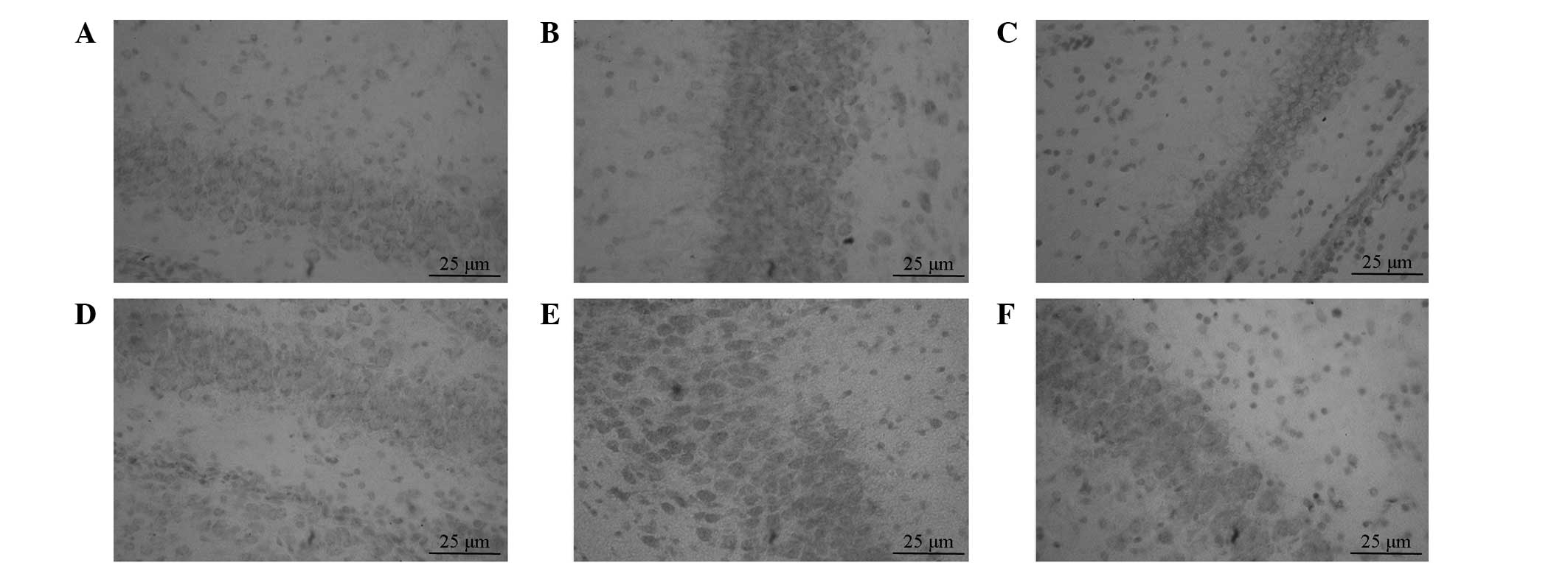
Immunohistochemical staining and image
analysis to determine TNF-α and NF-κB expression levels in the rat
hippocampal tissues of each group
Following the induction of hypoxia-ischemia for 24
h, brain tissues were rapidly obtained and fixed in 4%
paraformaldehyde overnight. The tissues were then conventionally
dehydrated and embedded in paraffin. The optic chiasm continuous
coronal slices were cut into 4-μm pieces, dewaxed, dried and stored
at room temperature for immunohistochemical staining of hippocampal
TNF-α and NF-κB.
Immunohistochemical techniques were performed using
a streptavidin-biotin complex kit, according to the manufacturer’s
instructions (Beijing Biosynthesis Biotechnology, Co., Ltd.,
Beijing, China). Antiphosphate buffer was utilized as a negative
control and cells of the cytoplasm and membrane that were stained
brown were selected as positive cells. Quantitative analyses of the
immunohistochemical reaction products were expressed by mean
optical density (MOD), where the MOD values reflected the quantity
of products. The results were analyzed using a HMIAS-200 multicolor
imaging analysis system (Champion images technology Co., Ltd.,
Wuhan, China).
Three horizons were randomly selected in the dentate
gyrus: CA1, CA2 and CA3 regions. The OD values of the positive
stains were measured at a magnification of ×400. The average value
was recorded as the MOD value of the hippocampus of the rats.
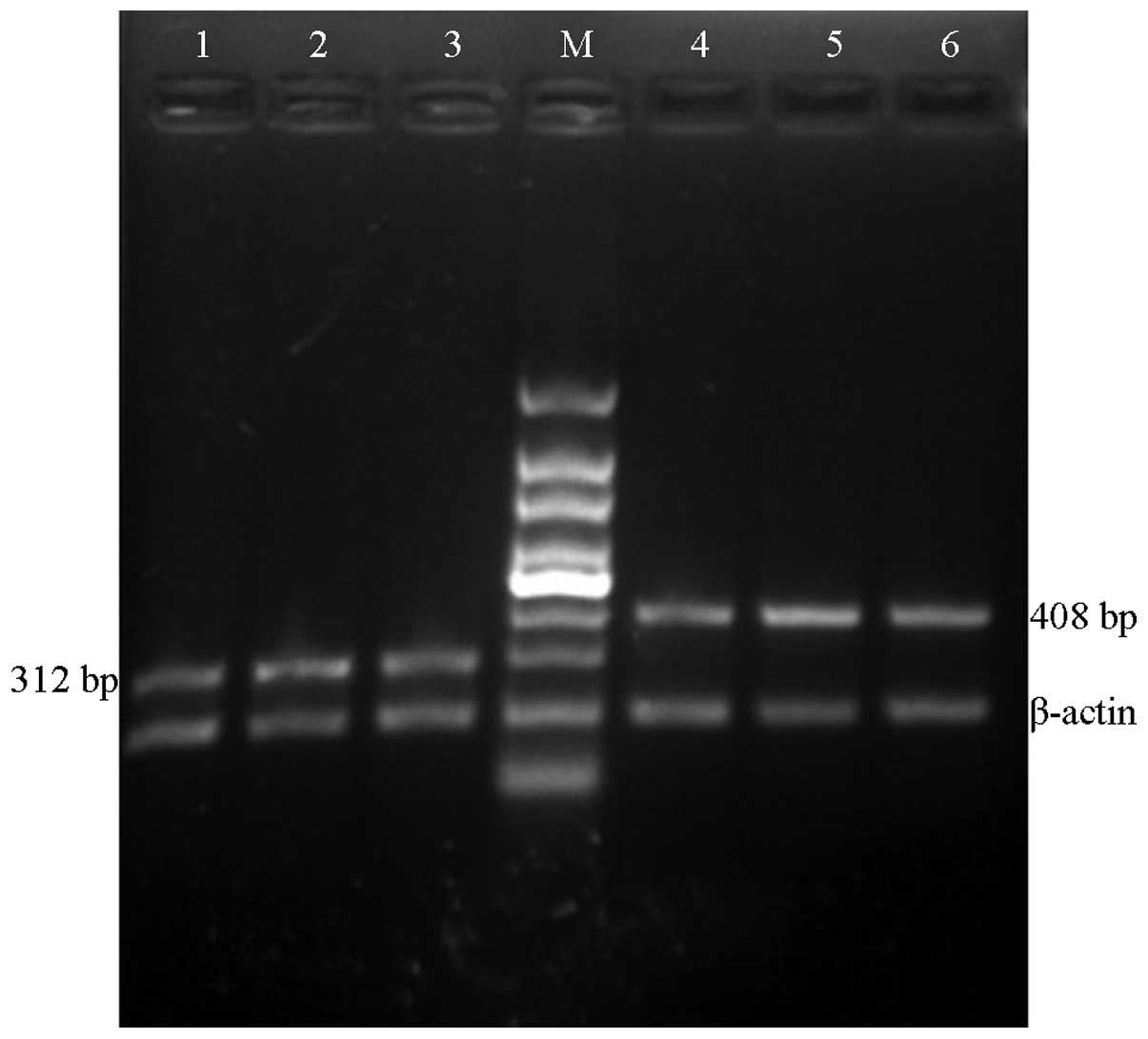
mRNA expression levels of TNF-α and NF-κB
in the rat hippocampal tissues of each group
Total RNA was extracted from the hippocampus.
Absorbance values were determined by UV spectrophotometry
(A260/A280, >1.7). Agarose gel electrophoresis revealed three
electrophoretic bands (28, 18 and 5 S), indicating that the total
RNA extracted had not been degraded and was suitable for use as a
template for reverse transcription reactions.
RNA was reverse transcribed into cDNA using a
reverse transcription kit (Takara Bio, Inc., Dalian, China), with
β-actin serving as an internal reference. The primers were
synthesized by Shanghai Sangon Biological Engineering Technology
& Services Co., Ltd (Shanghai, China). Primer compositions are
shown in Table I. The PCR
amplification cycling conditions were as follows: 95°C for 5 min,
94°C for 40 sec, 55°C for 40 sec and 72°C for 30 sec for 30 cycles,
and finally 72°C for 5 min. Following 2% agarose gel
electrophoresis, the reaction products were observed using a UV
analyzer. The electrophoretic bands were photographed and the gray
value was obtained through computer imaging analysis. Relative
expression levels of the target gene were obtained as follows:
(gray value of the target gene zone - gray value of the gel
background)/(gray value of the β-actin zone - gray value of the gel
background).
 | Table IPrimers used for PCR. |
Table I
Primers used for PCR.
| Gene | Primer sequence | Length, bp |
|---|
| β-actin |
5′-ACGTGTCATCCGTAAGTAC-3′
5′-CTGTGGAGCGAGGGCTCAG-3′ | 198 |
| TNF-α |
5′-GCTCCCTCTCATCAGTTCCA-3′
5′-TGGAAGACTCCTCCCAGGTA-3′ | 408 |
| NF-κB |
5′-GATACCACTAAGACGCACCC-3′
5′-CGCATTCAAGTCATAGTCCC-3′ | 312 |
Statistical analysis
Statistical analyses were performed using SPSS
software, version 17.0 (SPSS, Inc., Chicago, IL, USA). All data are
expressed as mean ± SD. Single-factor analysis of variance was used
for comparisons among groups. P<0.05 was considered to indicate
a statistically significant difference.
Results
Ultrastructural changes in the
hippocampus
In the sham group, the SEM results showed normal
neuronal structures, slightly oval neuronal nuclei, evenly
distributed nuclear chromatin and normal neutrophils. The
mitochondria, rough endoplasmic reticulum, Golgi apparatus and
other organelles were visible in the cytoplasm. In the model group,
the results revealed cavitation in the neurons, irregular nuclei,
cavitation in the nuclear matrix, intracytoplasmic cavitation and
swelling of the mitochondrial cytoplasm, fragmenting cristae,
cavitation of the cytoplasmic matrix, cavitation changes in the
neutrophils and fractured axon neurofilament with dissolution. The
neuronal nuclei of the PROG group exhibited oval shapes, evenly
distributed nuclear chromatin, occasional cavitation and fracture
of the cristae, abundant rough endoplasmic reticulum and mild
cavitation changes. The neuronal nuclei of the PROG group were
arranged in neat rows (Fig.
1).
Immunohistochemical staining of TNF-α and
NF-κB in the rat hippocampal tissues of each group
Immunohistochemical results showed that the positive
expression of TNF-α in the cytoplasm of the hippocampal neurons in
the sham group was low, with light staining. The number of positive
cells in the model group was significantly increased compared with
that in the sham group (P<0.05). However, in the PROG group the
number of cells expressing TNF-α was significantly decreased
compared with that in the model group (P<0.05). The results are
shown in Fig. 2A–C and Table II.
 | Table IIMOD values of TNF-α and NF-κB in the
hippocampus (mean ± SD). |
Table II
MOD values of TNF-α and NF-κB in the
hippocampus (mean ± SD).
| Group | TNF-α | NF-κB |
|---|
| Sham | 0.20±0.02 | 0.23±0.03 |
| Model | 0.53±0.04a | 0.63±0.04a |
| PROG | 0.32±0.03b | 0.38±0.03b |
In the sham group, NF-κB expression in the cytoplasm
of hippocampal neurons was exhibited in a small number of cells.
The number of positive cells in the model group was significantly
increased compared with that in the sham group (P<0.05), and
NK-κB expression was observed in the cytoplasm and the nucleus.
However, in the PROG group the number of positive cells was
significantly decreased when compared with that in the model group
(P<0.05). The results are shown in Fig. 2D–F and Table II.
Immunohistochemical results indicated that the
protein expression levels of TNF-α and NF-κB in the brain tissue
increased following hypoxic-ischemic brain damage. However, PROG
was capable of reducing the expression levels.
PROG reduces TNF-α and NF-κB mRNA
expression levels in hippocampal tissues
The specific bands of TNF-α and NF-κB mRNA were 408
and 312 bp, respectively. Quantitative polymerase chain reaction
(qPCR) results showed that the TNF-α and NF-κB mRNA expression
levels, as indicated by the gray values, in the sham group were
low. The TNF-α and NF-κB mRNA expression levels in the model group
were significantly higher compared with those in the sham group
(P<0.05), but were significantly lower in the PROG group
compared with those in the model group (P<0.01; Fig. 3 and Table III).
 | Figure 3TNF-α and NF-κB mRNA expression levels
in the hippocampal tissues of rats. PCR-amplified product bands of
TNF-α were 408 bp, bands of NF-κB were 312 bp and bands of β-actin
were 198 bp. Lanes 1, 2 and 3: NF-κB expression in the sham, model
and PROG groups, respectively. Lanes 4, 5 and 6: TNF-α expression
in the sham, model and PROG groups, respectively. TNF-α, tumor
necrosis factor-α; NF-κB, nuclear factor-κB; PROG, progesterone;
PCR, polymerase chain reaction. |
 | Table IIIRelative TNF-α and NF-κB mRNA levels
in the brain tissues of neonatal rats (mean ± SD). |
Table III
Relative TNF-α and NF-κB mRNA levels
in the brain tissues of neonatal rats (mean ± SD).
| Group | TNF-α | NF-κB |
|---|
| Sham | 0.46±0.04 | 0.48±0.06 |
| Model | 0.88±0.05a | 0.96±0.11a |
| PROG | 0.51±0.05b | 0.56±0.10b |
These results indicate that TNF-α and NF-κB mRNA
expression levels in brain tissues increase as a result of
hypoxic-ischemic brain damage. In addition, PROG exerts a
neuroprotective effect by reducing the expression levels.
Discussion
The results of the present study indicated that the
mRNA and protein expression levels of TNF-α and NF-κB in the
hippocampus of neonatal rats increased following hypoxia-ischemia
for 24 h. However, PROG pretreatment reduced the mRNA and protein
expression levels of TNF-α and NF-κB, indicating that PROG reduces
the inflammatory response following hypoxic-ischemic injury. Thus,
by inhibiting the inflammatory response, PROG exhibits an important
protective effect against HIE.
The protective role of PROG on the nervous system
has been of significant interest. Chen et al (24) demonstrated with a brain injury
model that PROG and its reduction products (5α-dihydro-progesterone
or allopregnanolone) accumulated around the lesions following
injury, indicating that PROG may have a protective effect against
brain injury. In brain injury, PROG inhibits the exudation of
macrophages and the secretion of TNF-α, interleukin-1 (IL-1) and
other cytokines. Specific pathological processes associated with
inflammatory factors, including complement factors, nuclear factor
(NF) and nitric oxide synthase, are also regulated by PROG
(25). The neuroprotective effects
of PROG are able to reduce cerebral edema, lipid peroxidation,
neuronal death and abnormity, promote stability of the blood-brain
barrier and improve cognition following traumatic brain injury and
other diseases (26). However,
PROG and allopregnanolone reportedly aggravate hypoxic-ischemic
brain damage in immature rats (27).
Numerous animal models of neonatal HIE are
available. The HIE model prepared by common carotid artery ligation
plus hypoxia (8% O2 + 92% N2, 2.5 h) in the
present study is stable and reliable (22,23).
Pathological changes mainly manifest as neuronal loss in the
lesions. Studies on various animal models with hypoxic-ischemic
brain injury have indicated that the hippocampus is the part of the
brain most sensitive to ischemic injury (28,29).
In the present study, pathological structural changes in the
hippocampus of neonatal rats in each group were observed with
electron microscopy. The results showed that neuronal structures in
the sham group were generally normal, whereas neurons in the model
group had cavitation changes due to hypoxic-ischemic neuronal
damage. However, hypoxic-ischemic neuronal damage was ameliorated
and cavitation reduced following the administration of PROG.
Hypoxic-ischemic brain injury is associated with
numerous factors. For example, injury inflammation is one of the
main causes of hypoxic-ischemic brain injury (7,8). The
upregulation of inflammatory cytokines, chemokines and adhesion
molecules constitutes the basis of transforming hypoxic-ischemic
injury into inflammatory injury. TNF-α is mainly produced by
activated monocytes-macrophages derived from nerve cells,
astrocytes, microglia, ependymal cells, vascular endothelial cells
and white blood cells in the central nervous system (30). Barone et al (31) established permanent and transient
cerebral artery occlusion models in spontaneously hypertensive
rats. Injecting TNF-α in the forebrain led to a dose-dependent
increase in cerebral infarct size and neurological function
deficits. By contrast, injecting TNF-α monoclonal antibodies in the
brain prior to this reversed the brain damage induced by exogenous
TNF-α. However, specific studies have shown that TNF-α exerts a
protective effect on brain ischemic tissues. Guo et al
pretreated rats with transient ischemia of the brain, and found
that the expression levels of TNF-α in the brain increased, which
significantly reduced ischemic cerebral infarction and the cerebral
edema volume following ischemia (32).
NF-κB was identified in 1986 and was termed NF-κB
since it specifically binds with κB sequences in the immunoglobulin
κ chain gene (33). The expression
of NF-κB in the hippocampal cortex and other brain regions of the
central nervous system has a wide biological significance,
particularly in the process of brain injury and brain degenerative
diseases (34). In a resting
state, NF-κB combines with its inhibitor, IκB, to form a complex
that exists in the cytoplasm and has no biological activity.
However, during ischemia and hypoxia, virus infection, mechanical
injury, radiation and other stressful conditions, NF-κB is
activated and initiates the transcription of involved target genes,
resulting in pathophysiological processes, including inflammation,
immune response, apoptosis and free radical damage (35,36).
Hypoxic-ischemic injury activates a large number of
inflammatory cytokines, including TNF-α and IL-1. These then
activate NF-κB, leading to the enhancement of transcription and
expression of inflammatory cytokine genes. Thus, NF-κB is a key
factor in the regulation of inflammation (37,15).
In the present study, immunohistochemical staining
and qPCR results demonstrated that the mRNA and protein expression
levels of TNF-α and NF-κB in the hippocampal tissues increased
following 24-h hypoxic-ischemic brain injury. PROG pretreatment
reduced the expression of inflammatory mediators, which is
consistent with previous experimental data (38).
Therefore, evident brain damage emerges following
hypoxic-ischemic brain injury for 24 h. The levels of inflammatory
mediators in the brain tissues also increase. PROG, as a preventive
medication, may relieve inflammation following hypoxic-ischemic
brain injury. Therefore, the present study demonstrates the
protective effect of PROG on neuronal hypoxic-ischemic brain damage
and provides a new method of prevention against HIE among
neonates.
Acknowledgements
The study was supported by grants from the Funding
Program for Young Backbone Teachers in Colleges and Universities of
Henan (no. 2012GGJS-134), the Bid Projects in Key Research Areas of
Xinxiang Medical University (no. ZD2011-37), the Education
Department of Henan Science Research Program (no. 2008A180029) and
the National Natural Science Foundation of China (no.
31070938).
References
|
1
|
Doi K, Sameshima H, Kodama Y, Furukawa S,
Kaneko M and Ikenoue T; Miyazaki Perinatal Data Groups. Perinatal
death and neurological damage as a sequential chain of poor
outcome. J Matern Fetal Neonatal Med. 25:706–709. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Northington FJ, Chavez Valdez R and Martin
LJ: Neuronal cell death in neonatal hypoxia-ischemia. Ann Neurol.
69:743–758. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Vannucci SJ and Hagberg H:
Hypoxia-ischemia in the immature brain. J Exp Biol. 207:3149–3154.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sasaoka N, Kawaguchi M, Kawaraguchi Y, et
al: Isoflurane exerts a short-term but not a long-term
preconditioning effect in neonatal rats exposed to a
hypoxic-ischaemic neuronal injury. Acta Anaesthesiol Scand.
53:46–54. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Boggio PS, Coutinho de Macedo E,
Pascual-Leone A, Tormos Muñoz JM, Schwartzman JS and Fregni F:
Neuromodulation in hypoxic-ischemic injury. Brain Stimul.
2:179–181. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhao P and Zuo Z: Isoflurane
preconditioning induces neuroprotection that is inducible nitric
oxide synthase-dependent in neonatal rats. Anesthesiology.
101:695–703. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Liu F and McCullough LD: Inflammatory
responses in hypoxic ischemic encephalopathy. Acta Pharmacol Sin.
34:1121–1130. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kasdorf E and Perlman JM: Hyperthermia,
inflammation, and perinatal brain injury. Pediatr Neurol. 49:8–14.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bonestroo HJ, Nijboer CH, van Velthoven
CT, Kavelaars A, Hack CE, van Bel F and Heijnen CJ: Cerebral and
hepatic inflammatory response after neonatal hypoxia-ischemia in
newborn rats. Dev Neurosci. 35:197–211. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Walberer M, Rueger MA, Simard ML, Emig B,
Jander S, Fink GR and Schroeter M: Dynamics of neuroinflammation in
the macrosphere model of arterio-arterial embolic focal ischemia:
an approximation to human stroke patterns. Exp Transl Stroke Med.
2:222010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Baker SJ and Reddy EP: Modulation of life
and death by the TNF receptor superfamily. Oncogene. 17:3261–3270.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chung HS, Kim SN, Jeong JH and Bae H: A
novel synthetic compound
4-acetyl-3-methyl-6-(2-bromophenyl)pyrano[3,4-c]pyran-1,8-dione
inhibits the production of nitric oxide and proinflammatory
cytokines via the NF-κB pathway in lipopolysaccharide-activated
microglia cells. Neurochem Res. 38:807–814. 2013.PubMed/NCBI
|
|
13
|
Nijboer CH, Heijnen CJ, Groenendaal F, May
MJ, van Bel F and Kavelaars A: A dual role of the NF-kappa B
pathway in neonatal hypoxic-ischemic brain damage. Stroke.
39:2578–2586. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Su JR, Zhao ZC, Chen WL and Wang X: The
effect of activated nuclear factor-kappaB in pathogenesis of acute
pancreatitis. Zhonghua Yi Xue Za Zhi. 83:1497–1500. 2003.(In
Chinese).
|
|
15
|
Gesslein B, Håkansson G, Gustafsson L,
Ekström P and Malmsjö M: Tumor necrosis factor and its receptors in
the neuroretina and retinal vasculature after ischemia-reperfusion
injury in the pig retina. Mol Vis. 16:2317–2327. 2010.PubMed/NCBI
|
|
16
|
Pettus EH, Wright DW, Stein DG and Hoffman
SW: Progesterone treatment inhibits the inflammatory agents that
accompany traumatic brain injury. Brain Res. 1049:112–119. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Singh M and Su C: Progesterone-induced
neuroprotection: factors that may predict therapeutic efficacy.
Brain Res. 1514:98–106. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Baudry M, Bi X and Aguirre C:
Progesterone-estrogen interactions in synaptic plasticity and
neuroprotection. Neuroscience. 239:280–294. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Li DL, Zhao HG, Wang DX and Ding YF:
Effect of progesterone on cerebral cortex edema in rats exposed to
focal ischemia/reperfusion. Zhongguo Ying Yong Sheng Li Xue Za Zhi.
17:327–329. 2001.(In Chinese).
|
|
20
|
Li DL and Han H: Effect of progesterone on
the expression of GLUT in the brain following hypoxic-ischemia in
newborn rats. Zhongguo Ying Yong Sheng Li Xue Za Zhi. 24:353–355.
2008.(In Chinese).
|
|
21
|
Wang X, Zhang J, Yang Y, Dong W, Wang F,
Wang L and Li X: Progesterone attenuates cerebral edema in neonatal
rats with hypoxic-ischemic brain damage by inhibiting the
expression of matrix metalloproteinase-9 and aquaporin-4. Exp Ther
Med. 6:263–267. 2013.PubMed/NCBI
|
|
22
|
Rice JE 3rd, Vannucci RC and Brierley JB:
The influence of immaturity on hypoxic-ischemic brain damage in the
rat. Ann Neurol. 9:131–141. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Taniguchi H and Andreasson K: The
hypoxic-ischemic encephalopathy model of perinatal ischemia. J Vis
Exp. 19:9552008.
|
|
24
|
Chen G, Shi J, Ding Y, Yin H and Hang C:
Progesterone prevents traumatic brain injury-induced intestinal
nuclear factor kappa B activation and proinflammatory cytokines
expression in male rats. Mediators Inflamm. 2007:934312007.
View Article : Google Scholar
|
|
25
|
Sarkaki AR, Khaksari Haddad M, Soltani Z,
Shahrokhi N and Mahmoodi M: Time- and dose-dependent
neuroprotective effects of sex steroid hormones on inflammatory
cytokines after a traumatic brain injury. J Neurotrauma. 30:47–54.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Aggarwal R, Medhi B, Pathak A, Dhawan V
and Chakrabarti A: Neuroprotective effect of progesterone on acute
phase changes induced by partial global cerebral ischaemia in mice.
J Pharm Pharmacol. 60:731–737. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Tsuji M, Taguchi A, Ohshima M, Kasahara Y
and Ikeda T: Progesterone and allopregnanolone exacerbate
hypoxic-ischemic brain injury in immature rats. Exp Neurol.
233:214–220. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Gustavsson M, Wilson MA, Mallard C,
Rousset C, Johnston MV and Hagberg H: Global gene expression in the
developing rat brain after hypoxic preconditioning: involvement of
apoptotic mechanisms? Pediatr Res. 61:444–450. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Rouse DJ, Hirtz DG, Thom E, et al; Eunice
Kennedy Shriver NICHD Maternal-Fetal Medicine Units Network. A
randomized, controlled trial of magnesium sulfate for the
prevention of cerebral palsy. N Engl J Med. 359:895–905. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
O’Connor JJ: Targeting tumour necrosis
factor-α in hypoxia and synaptic signalling. Ir J Med Sci.
182:157–162. 2013.
|
|
31
|
Barone FC, Arvin B, White RF, et al: Tumor
necrosis factor-alpha. A mediator of focal ischemic brain injury.
Stroke. 28:1233–1244. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Guo M, Lin V, Davis W, et al: Preischemic
induction of TNF-alpha by physical exercise reduces blood-brain
barrier dysfunction in stroke. J Cereb Blood Flow Metab.
28:1422–1430. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Sen R and Baltimore D: Inducibility of
kappa immunoglobulin enhancer-binding protein NF-kappaB by
posttranslational mechanism. Cell. 47:921–928. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kaufmann JA, Bickford PC and Taglialatela
G: Free radical-dependent changes in constitutive Nuclear factor
kappa B in the aged hippocampus. Neuroreport. 13:1917–1920. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Lee HJ, Oh TH, Yoon WJ, et al: Eutigoside
C inhibits the production of inflammatory mediators (NO, PGE(2),
IL-6) by down-regulating NF-kappaB and MAP kinase activity in
LPS-stimulated RAW 264.7 cells. J Pharm Pharmacol. 60:917–924.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Brown KD, Claudio E and Siebenlist U: The
roles of the classical and alternative nuclear factor-kappaB
pathways: potential implications for autoimmunity and rheumatoid
arthritis. Arthritis Res Ther. 10:2122008. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Hayden MS and Ghosh S: Shared principles
in NF-kappaB signaling. Cell. 132:344–362. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Wang X, Zhang J, Si D, et al: Progesterone
inhibits the expression of cycloxygenase-2 and interleukin-1β in
neonatal rats with hypoxic ischemic brain damage. Int J Neurosci.
124:42–48. 2014.PubMed/NCBI
|