Introduction
The prevalence of diabetes mellitus in China is
rapidly increasing with the aging population and ~9.7% of the adult
population (~92.4 million) have diabetes (1). Furthermore, diabetes has been
identified to be an independent risk factor for cardiovascular
disease, whereby an elevated fasting plasma glucose (FPG) level is
considered to be significant (2,3). In
the early stages of type 2 diabetes (T2D), a number of residual
β-cells remain, thus, early insulin therapy can improve β-cell
function and enhance the control of plasma glucose levels. This
reduces glucotoxicity and ultimately reduces or prevents the
development and progression of diabetes-associated cardiovascular
complications (4,5).
The American Diabetes Association and the European
Association for the Study of Diabetes emphasized the importance of
basal insulin treatment in newly diagnosed diabetes patients in
2009 (6). However, few studies
have been performed investigating whether basal insulin therapy
decreases cardiovascular events in patients with early T2D at a
high risk for cardiovascular disease. In addition, a limited number
of studies have investigated whether insulin glargine improves
β-cell function and insulin sensitivity in T2D patients. Therefore,
the aim of the present study was to investigate whether insulin
glargine was able to reduce the risk of cardiovascular events and
improve β-cell function and insulin sensitivity in T2D patients
with a high risk for cardiovascular disease. Furthermore, the
long-term efficacy and safety of insulin glargine were also
evaluated.
Patients and methods
Patients
In total, 42 patients (in- or outpatients; males,
17; females, 25; age, ≥50 years) who had recently been diagnosed
with T2D mellitus and were considered to be at a high risk for
cardiovascular disease were included in the present study. The
patients were randomly divided into an insulin-glargine group
(n=22) and standard-care group (n=20). Patients were diagnosed with
a high risk for cardiovascular disease if they exhibited any one of
the following symptoms: i) History of myocardial infarction, stroke
or revascularization; ii) angina with documented ischemic changes;
iii) albuminuria; iv) left ventricular hypertrophy identified by
electrocardiogram or echocardiogram; v) stenosis of ≥50% in the
coronary, carotid or lower extremity arteries; and vi)
ankle/brachial index of <0.9. Patients were excluded if they
exhibited diabetic ketoacidosis, hyperosmolar nonketotic
hyperglycemic coma or marked hepatorenal damage. The present study
was approved by the Ethics Committee of The First Affiliated
Hospital of Chongqing Medical University (Chongqing, China) and
written informed consent was obtained from all the
participants.
Subjects in the insulin-glargine group received a
subcutaneous injection of insulin glargine at an initial dose of 10
U/day as well as their current glycemic-control regimen (not
including thiazolidinediones). The dose of glargine was adjusted
based on the FPG level, targeting a self-measured FPG level of ≤5.3
mmol/l. Subjects in the standard-care group were administered oral
antidiabetic agents, and if necessary, insulin (not including
glargine) was also administered according to the diabetic treatment
guidelines. The target was to obtain an FPG level of ≤6.1 mmol/l
and a 2-h postprandial blood glucose (2hPG) level of ≤8.0 mmol/l.
Other drugs administered to the participants remained unchanged
throughout the follow-up. The patients were assessed every 3–6
months and the median follow-up period was 6.4 years. Levels of
plasma glucose, glycosylated hemoglobin (HbA1c) and plasma lipids
were measured and recorded at each follow-up. Patients’ weight was
measured annually for calculation of the body mass index (BMI). At
the final follow-up examination, the levels of plasma insulin and
C-peptide were detected and the homeostasis model
assessment-insulin resistance index (HOMA-IR) and the HOMA-insulin
secretion index (HOMA-β) were calculated as follows: HOMA-IR =
fasting plasma insulin × FPG/22.5; and HOMA-β = 20 × fasting plasma
insulin/(FPG - 3.5). In addition, the incidence of hypoglycemia and
adverse cardiovascular events, including cardiovascular fatality,
coronary heart disease, non-fatal myocardial infarction, angina,
stroke, revascularization and heart failure, were recorded.
Glucose oxidase assay
Plasma glucose levels were measured using the
glucose oxidase method. Briefly, 0.02 ml distilled water, 0.02 ml
glucose standard solution and 0.02 ml test serum were added to
three tubes (blank, standard and assay tubes), respectively. A
mixed reagent of enzyme and phenol (3 ml) was added to each tube
and mixed thoroughly by shaking. Subsequently, the three tubes were
placed into a water bath at 37°C for 15 min. The blank tube was
used to adjust the instrument to zero and the absorbance values of
the standard and assay tubes were measured at a wavelength of 505
nm on an automatic analyzer (Model 7600, Hitachi High-Technologies
Corporation, Ibaraki Prefecture, Japan). The concentration of
plasma glucose was calculated using the following formula: Serum
glucose concentration (mmol/l) = 5 × (assay tube
absorbance/standard tube absorbance). Each sample was analyzed
three times and the average values were recorded.
High performance liquid
chromatography
HbA1c concentration was measured using high
performance liquid chromatography. Whole blood samples, that had
been obtained from the patients and refrigerated at 4°C, were mixed
thoroughly and the concentration of HbA1c was determined using an
automatic HbA1c analyzer (Bio-Rad D10; Bio-Rad, Hercules, CA, USA),
according to the manufacturer’s instructions. Each sample was
assessed three times and the average values were recorded.
Chemiluminescence assay
A chemiluminescence assay was conducted to determine
the plasma insulin and C-peptide levels. Reagents that had been
refrigerated at 4°C, were placed into test plates and mixed for 15
min. A calibrating solution and control serum were added to the
test plates for the purposes of calibration and quality control.
The blood samples were centrifuged at 999 × g for 10 min and the
supernatants were transferred to sample plates and labeled for the
assay. Each sample was analyzed three times and the average values
were recorded. The samples were analyzed by an automated
chemiluminescent immunoassay analyzer (ADVIA Centaur, Bayer,
Leverkusen, Germany).
Automatic biochemical analysis
Plasma lipid levels were assessed using an automatic
biochemical analyzer. Patient blood samples were centrifuged at 999
× g for 10 min and the supernatants were analyzed to determine the
content of total cholesterol, triglycerides and high density and
low density lipoproteins, according to the manufacturer’s
instructions. Each sample was assessed three times and the average
values were recorded.
Statistical analysis
Statistical analysis was performed using SPSS 17.0
software (SPSS, Inc., Chicago, IL, USA) and the normally
distributed and continuous variables are presented as the mean ±
standard deviation. Variations from the baseline values and
intergroup comparisons were analyzed using the Student’s t-test
(paired and unpaired, respectively). HOMA-β and HOMA-IR values were
compared between the two groups using the Student’s t-test
following logarithmic transformation. The Wilcoxon rank sum test
was used for intergroup comparisons of non-normally distributed
variables, including the incidence of hypoglycemia and
cardiovascular events. Comparisons of plasma insulin and C-peptide
levels between the two groups were conducted using repeated
measures design analysis of variance. P<0.05 was considered to
indicate a statistically significant difference.
Results
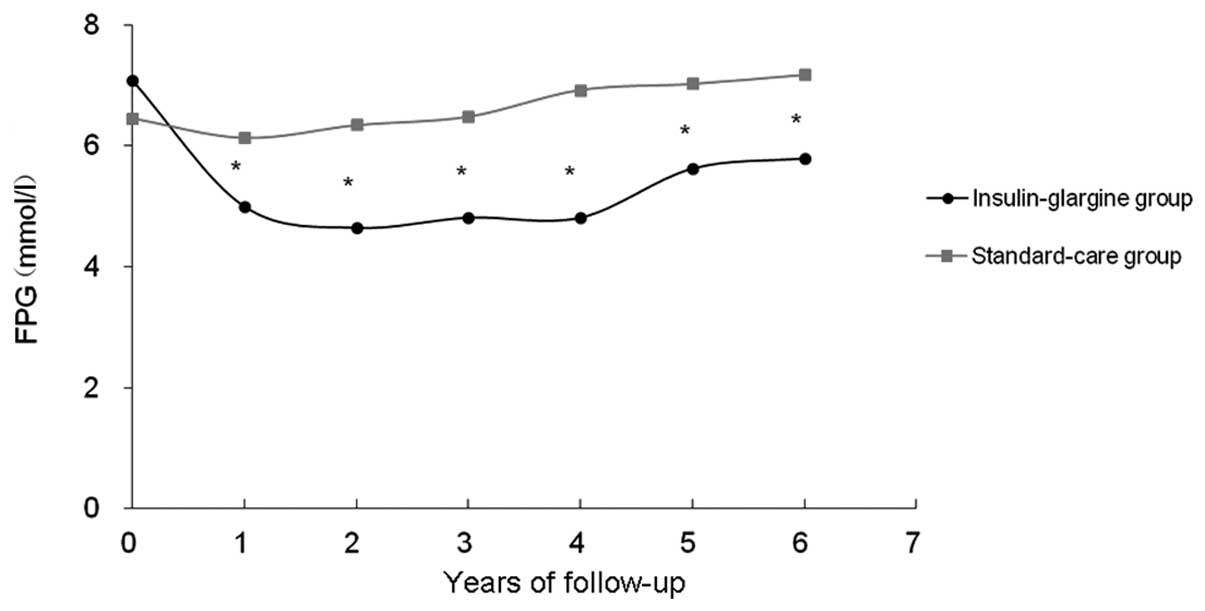
Insulin glargine treatment reduces the
level of FPG
The baseline characteristics of the subjects are
shown in Table I. Overall, the
baseline demographics were considered to be relatively uniform
between the two groups (P>0.05). To measure the levels of FPG,
HbA1c and 2hPG, a glucose oxidase assay and high performance liquid
chromatography were conducted. Following treatment, the mean FPG
level in the insulin-glargine group demonstrated a constant overall
reduction from 7.07 to 5.79 mmol/l over the 6.4-year treatment
period (P<0.01; Fig. 1),
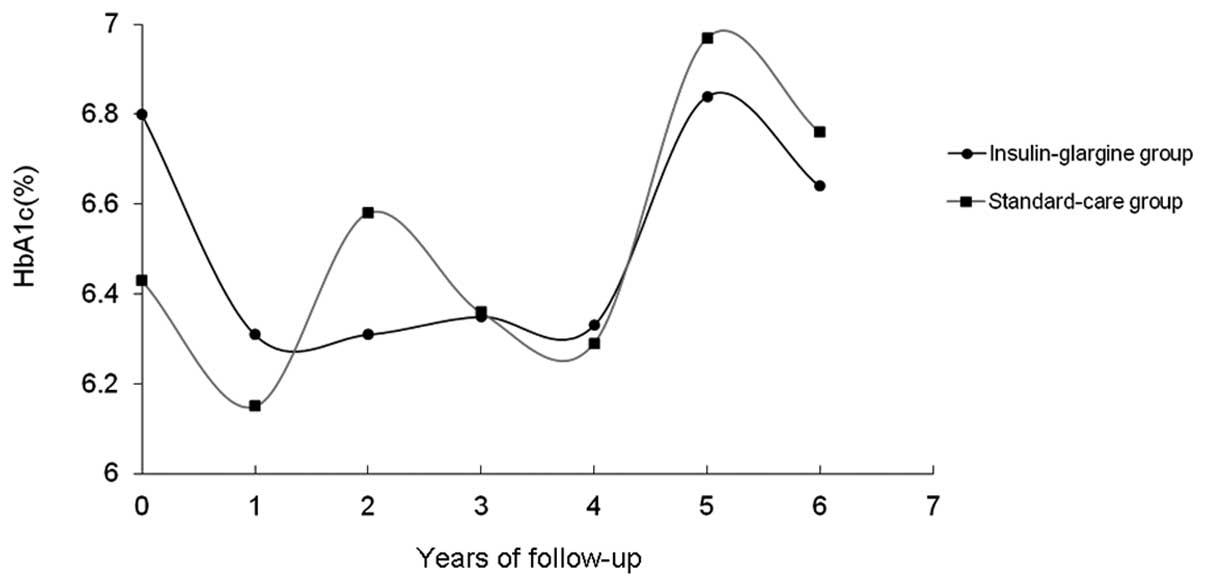
however, the mean HbA1c level did not alter significantly (Table II and Fig. 2). By contrast, the FPG and HbA1c
levels in the standard-care group did not indicate a significant
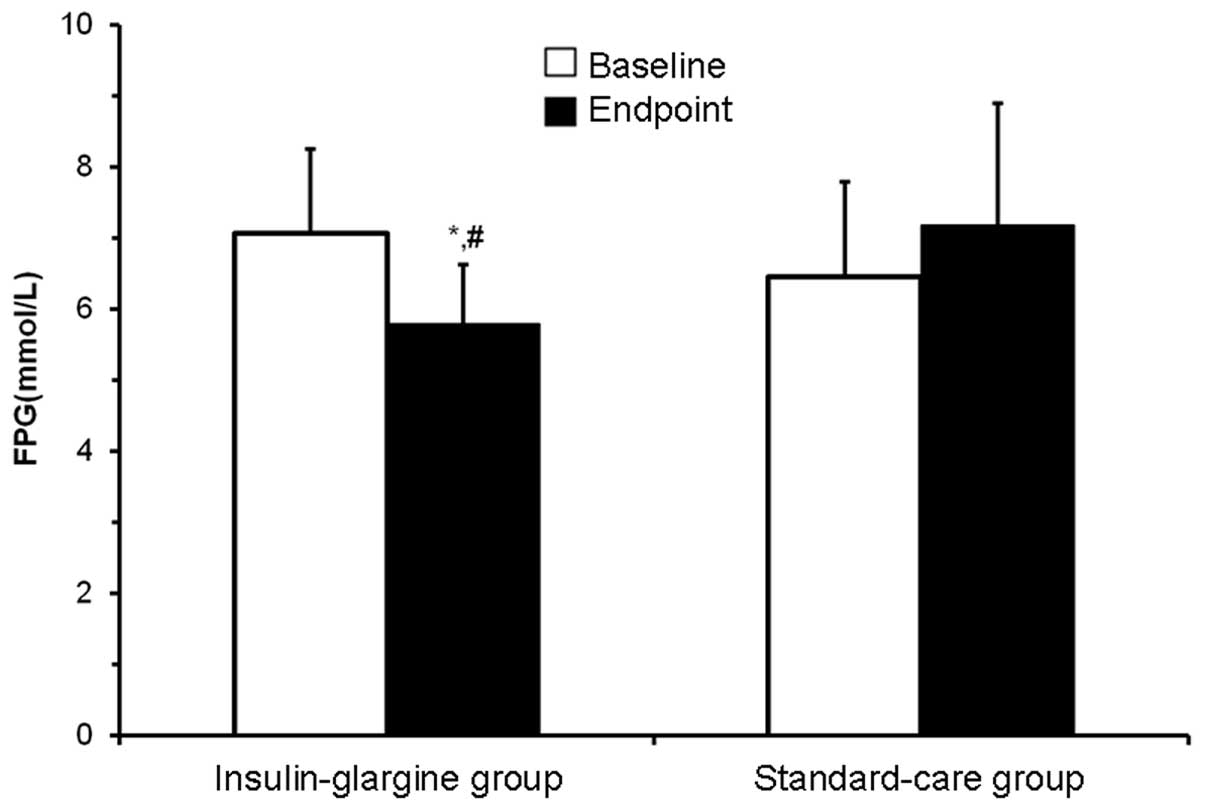
difference prior to and following treatment (Figs. 1 and 2). Through comparing the data at the
endpoints between the two groups, it was identified that the FPG
level in the insulin-glargine group (5.79±0.83 mmol/l) was
significantly lower than the level in the standard-care group
(7.17±1.77 mmol/l; P<0.05), however, the levels of HbA1c and
2hPG did not differ between the two groups (Table III and Fig. 3). In addition, the FPG level in the
insulin-glargine group was significantly lower than the level
observed in the standard-care group during the follow-up period
(P<0.05; Table II and Fig. 1). These observations indicated that
insulin glargine treatment influenced the reduction in FPG levels,
but exhibited no effect on the levels of HbA1c or 2hPG.
 | Table IBaseline demographic characteristics
of the subjects. |
Table I
Baseline demographic characteristics
of the subjects.
| Variable | Insulin-glargine
group (n=22) | Standard-care group
(n=20) |
|---|
| Age (years) | 62.8±6.3 | 62.7±5.8 |
| Male:female | 10:12 | 7:13 |
| BMI
(kg/m2) | 24.32±2.51 | 24.90±2.78 |
| FPG (mmol/l) | 7.07±1.18 | 6.45±1.36 |
| HbA1c (%) | 6.80±0.79 | 6.43±1.13 |
| TC (mmol/l) | 4.71±0.96 | 4.82±1.28 |
| TG (mmol/l) | 1.51±1.03 | 1.87±1.68 |
| HDL (mmol/l) | 1.15±0.22 | 1.22±0.30 |
| LDL (mmol/l) | 2.78±0.72 | 2.79±1.04 |
 | Table IIGlycemic indices during the trial. |
Table II
Glycemic indices during the trial.
| FPG (mmol/l) | HbAlc (%) |
|---|
|
|
|
|---|
| Follow-up | Insulin-glargine
group (n=22) | Standard-care group
(n=20) | Insulin-glargine
group (n=22) | Standard-care group
(n=20) |
|---|
| Baseline | 7.07±1.18 | 6.45±1.36 | 6.80±0.79 | 6.43±1.13 |
| Year 1 | 4.99±0.82a | 6.13±0.97 | 6.31±0.59 | 6.15±0.64 |
| Year 2 | 4.64±0.84a | 6.34±1.07 | 6.31±0.70 | 6.58±1.00 |
| Year 3 | 4.81±0.78a | 6.48±1.25 | 6.35±0.78 | 6.36±1.01 |
| Year 4 | 4.81±0.82a | 6.92±1.23 | 6.33±0.74 | 6.29±0.84 |
| Year 5 | 5.62±0.96a | 7.02±1.63 | 6.84±0.80 | 6.97±0.94 |
| Year 6 | 5.79±0.83a | 7.17±1.77 | 6.64±0.81 | 6.76±1.15 |
 | Table IIIFPG and HbA1c levels on completion of
the trial. |
Table III
FPG and HbA1c levels on completion of
the trial.
| Variable | Insulin-glargine
group (n=22) | Standard-care group
(n=20) |
|---|
| FPG (mmol/l) | 5.79±0.83ab | 7.17±1.77 |
| HbA1c (%) | 6.64±0.81 | 6.76±1.15 |
Insulin glargine treatment affected the
levels of plasma insulin and C-peptide in the initial stages and
reduced the level of HOMA-IR, but not HOMA-β
To determine the levels of plasma insulin and
C-peptide, a chemiluminescence assay was performed. On completion
of the study, the levels of plasma insulin and C-peptide at fasting
and at 30 min following oral glucose tolerance test (OGTT) in the
insulin-glargine group were significantly lower than those observed
in the standard-care group (P<0.05), however, there were no
statistically significant differences identified between the two
groups at 60 and 120 min following OGTT. In addition, the HOMA-IR
value in the insulin-glargine group was significantly lower
compared with the standard-care group (P<0.01), whereas no
statistically significant difference was observed between the two
groups with regard to HOMA-β (Table
IV). These observations indicated that the insulin glargine
treatment affected the levels of plasma insulin and C-peptide in
the initial stages, which reduced the level of HOMA-IR, but not
that of HOMA-β.
 | Table IVLevels of plasma insulin and C-peptide
on completion of the trial. |
Table IV
Levels of plasma insulin and C-peptide
on completion of the trial.
| Plasma level | Insulin-glargine
group (n=22) | Standard-care group
(n=20) |
|---|
| FCP (ng/ml) | 1.67±1.01c | 2.59±1.13 |
| 30′ CP (ng/ml) | 3.31±1.82c | 4.84±1.87 |
| 60′ CP (ng/ml) | 5.25±2.07 | 6.21±2.42 |
| 120′ CP (ng/ml) | 6.97±2.62 | 8.41±3.27 |
| FINS (mIU/l) | 8.47±4.08c | 11.12±2.99 |
| 30′ INS (mIU/l) | 18.03±8.36c | 23.43±6.64 |
| 60′ INS (mIU/l) | 27.07±11.31 | 29.69±8.68 |
| 120′ INS (mIU/l) | 36.97±14.03 | 42.34±10.06 |
| HOMA-βa | 77.37±26.80 | 80.76±61.56 |
| HOMA-IRb | 2.56±1.32d | 3.54±1.33 |
Insulin glargine treatment may result in
hypoglycemia, but not adverse cardiovascular events
To investigate the effect of insulin glargine
treatment on the incidence of hypoglycemia and adverse
cardiovascular events, the patients were closely followed-up
throughout the 6.4 years of treatment. The incidences of
hypoglycemia in the insulin-glargine and standard-care groups were
11.7 episodes per 100 persons/year (seven individuals with a total
of 16 episodes) and 0.8 episodes per 100 persons/year (one
individual with one episode), respectively, which was identified to
be a statistically significant difference (P<0.05). By contrast,
the incidences of adverse cardiovascular events did not differ
between the two groups with 4.4 episodes per 100 persons/year in
the insulin-glargine group and 11.3 episodes per 100 persons/year
in the standard-care group (Table
V). These observations indicated that insulin glargine
treatment may lead to hypoglycemia.
 | Table VIncidence of hypoglycemia and adverse
cardiovascular events throughout the study. |
Table V
Incidence of hypoglycemia and adverse
cardiovascular events throughout the study.
| Variable | Insulin-glargine
group (n=22) | Standard-care group
(n=20) |
|---|
| Hypoglycemia, n
(n/100 persons/year)a | 16 (11.7)c | 1 (0.8) |
| Cardiovascular
events, n (n/100 persons/year)b | 6 (4.4) | 14 (11.3) |
Insulin glargine treatment does not
affect the levels of plasma lipids or the BMI
To assess the levels of plasma lipids, an automatic
biochemical analyzer was employed. The levels of plasma lipids in
the two groups did not change significantly from the baseline and
the difference between the two groups at the endpoint was not
identified to be statistically significant. Between the start of
the study and completion, patients’ BMIs increased by 0.15±1.95
kg/m2 in the insulin-glargine group and 0.20±1.80
kg/m2 in the standard-care group (Table VI), however, analysis between the
two groups did not identify a statistically significant difference.
These results indicated that insulin glargine treatment did not
affect the plasma lipid levels or the BMI.
 | Table VIChanges in patient BMI and levels of
plasma lipids at the baseline and endpoint. |
Table VI
Changes in patient BMI and levels of
plasma lipids at the baseline and endpoint.
| Insulin-glargine
group (n=22) | Standard-care group
(n=20) |
|---|
|
|
|
|---|
| Variable | Baseline | Endpoint | Baseline | Endpoint |
|---|
| BMI
(kg/m2) | 24.32±2.51 | 24.47±2.12 | 24.90±2.78 | 25.10±2.62 |
| TC (mmol/l) | 04.71±0.96 | 04.47±0.89 | 04.82±1.28 | 04.54±0.85 |
| TG (mmol/l) | 01.51±1.03 | 01.42±0.79 | 01.87±1.68 | 01.85±1.07 |
| HDL (mmol/l) | 01.15±0.22 | 01.23±0.21 | 01.22±0.30 | 01.33±0.31 |
| LDL (mmol/l) | 02.78±0.72 | 02.65±0.74 | 02.79±1.04 | 02.54±0.68 |
Discussion
T2D mellitus is characterized by insulin resistance
and the impaired function of β-cells. Through the application of
insulin therapy at the initial stages of T2D mellitus to improve
the control of plasma glucose levels, it may be possible to reverse
the damage on β cells, which results from hyperglycemia (7). In addition, an increased risk for
cardiovascular disease in T2D mellitus patients has been observed.
Previous studies (8,9), both foreign and domestic, have
indicated that the levels of FPG and HbA1c are closely associated
with the development and progression of cardiovascular events, and
the cardiovascular risk of patients with T2D mellitus may be
reduced by the early administration of insulin to attain or
approach the normal plasma glucose level.
Insulin glargine is a long-acting insulin analog
that can be produced via recombinant DNA technology. Insulin
glargine functions slowly and requires a long time to reduce the
plasma glucose level, without exhibiting a peak value and simulates
the physiological secretion of basal insulin (10,11).
In the present study, the FPG level in the insulin-glargine group
significantly decreased from the baseline values, and the long-term
FPG and HbA1c concentrations were maintained at near-normal levels.
Furthermore, following treatment, the FPG level in the
insulin-glargine group was significantly decreased when compared
with the level in the standard-care group. These observations are
consistent with the results of previous studies (12,13).
β-cell function in T2D mellitus patients is known to
progressively deteriorate. Therefore, previous studies have
assessed whether the early administration of insulin to improve
glucose control may result in improved insulin resistance and
β-cell function. Pistrosch et al (14) demonstrated that glargine improved
β-cell function and insulin resistance in newly diagnosed T2D
mellitus patients. However, the present study indicated that there
was no statistically significant difference in the level of HOMA-β
between the two groups. By contrast, the level of HOMA-IR in the
insulin-glargine group was significantly lower when compared with
the standard-care group. Although the insulin secretion conditions
of each participant were not measured on entry into the study, we
may hypothesize that insulin glargine treatment improves the
insulin resistance of patients with T2D mellitus; this hypothesis
is consistent with previous studies (15,16).
The underlying mechanism may be that the early administration of
glargine reduces the damage to β cells and target organs that is
caused by high plasma glucose levels, which activates the insulin
signaling pathway and improves insulin resistance. However, this
specific mechanisms requires further investigation.
Previous studies (17,18)
have demonstrated a low incidence of hypoglycemia in T2D mellitus
patients that have been treated with insulin glargine. By contrast,
the results of the present study indicated that there were more
hypoglycemic episodes in the insulin-glargine group when compared
with the standard-care group. This result may have been observed
since the FPG level in the insulin-glargine group was required to
be ≤5.3 mmol/l, which was associated with an increased insulin
glargine dose and therefore an increased risk of hypoglycemia.
T2D mellitus patients are considered to be at a
greater risk of cardiovascular disease. Holman et al
(19) demonstrated that insulin
treatment on recently diagnosed T2D mellitus patients resulted in
the improved control of plasma glucose levels, which in turn
reduced the risk of cardiovascular events. By contrast, several
large-scale studies (20–23) have indicated that hypoglycemia
induced by intensive glucose-lowering therapy, is strongly
associated with the development of cardiovascular diseases in
patients with T2D mellitus. The results of the present study
demonstrated that during the intervention period, the incidence of
hypoglycemia was significantly higher in the insulin-glargine group
as compared with the standard-care group, however, the risk of
cardiovascular events was similar between the two groups. There are
a number of possible explanations for this result. Firstly, the
relatively higher risk of hypoglycemia in the insulin-glargine
group may have resulted in an increased risk of cardiovascular
disease, which may marginally offset the protective mechanism of
glargine on the cardiovascular system. Secondly, all the
participants exhibited a high risk for cardiovascular diseases,
therefore, the benefit of glargine on the cardiovascular system in
these subjects was less likely to be observed as compared with T2D
mellitus patients that were without cardiovascular risks. Finally,
the antihypertensive agents, lipid-modulating agents and
anticoagulants that exhibit beneficial effects on the
cardiovascular system were continued throughout the treatment
period, thus, to a certain extent, the cardiovascular benefit of
insulin glargine was difficult to observe. Therefore,
interpretation of the results indicates that glargine may reduce
the incidence of cardiovascular events should the follow-up period
be extended.
In conclusion, insulin glargine treatment results in
favorable outcomes with regard to long-term glycemic control and
the improvement of insulin resistance, without increasing the risk
of cardiovascular events in patients with T2D mellitus. The
observations of the present study indicate that glargine may be
considered as an effective and safe basal insulin in clinical
applications.
Acknowledgements
The study was supported by grants from
Sanofi-Aventis (Clinical Trials Identifier: NCT00069784).
References
|
1
|
Yang W, Lu J, Weng J, et al; China
National Diabetes and Metabolic Disorders Study Group. Prevalence
of diabetes among men and women in China. N Engl J Med.
362:1090–1101. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Brunner EJ, Shipley MJ, Witte DR, Fuller
JH and Marmot MG: Relation between blood glucose and coronary
mortality over 33 years in the Whitehall Study. Diabetes Care.
29:26–31. 2006.PubMed/NCBI
|
|
3
|
Hu FB, Stampfer MJ, Solomon CG, et al: The
impact of diabetes mellitus on mortality from all causes and
coronary heart disease in women: 20 years of follow-up. Arch Intern
Med. 161:1717–1723. 2001.PubMed/NCBI
|
|
4
|
Weng J, Li Y, Xu W, et al: Effect of
intensive insulin therapy on beta-cell function and glycaemic
control in patients with newly diagnosed type 2 diabetes: a
multicentre randomised parallel-group trial. Lancet. 371:1753–1760.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
LeRoith D, Fonseca V and Vinik A:
Metabolic memory in diabetes - focus on insulin. Diabetes Metab Res
Rev. 21:85–90. 2005. View
Article : Google Scholar
|
|
6
|
Nathan DM, Buse JB, Davidson MB, et al;
American Diabetes Association; European Association for Study of
Diabetes. Medical management of hyperglycemia in type 2 diabetes: a
consensus algorithm for the initiation and adjustment of therapy: a
consensus statement of the American Diabetes Association and the
European Association for the Study of Diabetes. Diabetes Care.
32:193–203. 2009. View Article : Google Scholar
|
|
7
|
Hu Y, Li L, Xu Y, et al: Short-term
intensive therapy in newly diagnosed type 2 diabetes partially
restores both insulin sensitivity and beta-cell function in
subjects with long-term remission. Diabetes Care. 34:1848–1853.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lawes CM, Parag V, Bennett DA, et al; Asia
Pacific Cohort Studies Collaboration. Blood glucose and risk of
cardiovascular disease in the Asia Pacific region. Diabetes Care.
27:2836–2842. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gerstein HC and Rosenstock J: Insulin
therapy in people who have dysglycemia and type 2 diabetes
mellitus: can it offer both cardiovascular protection and beta-cell
preservation? Endocrinol Metab Clin North Am. 34:137–154. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Younis N, Soran H and Bowen-Jones D:
Insulin glargine: a new basal insulin analogue. QJM. 95:757–761.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang F, Carabino JM and Vergara CM:
Insulin glargine: a systematic review of a long-acting insulin
analogue. Clin Ther. 25:1539–1577. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fonseca V, Gill J, Zhou R and Leahy J: An
analysis of early insulin glargine added to metformin with or
without sulfonylurea: impact on glycaemic control and
hypoglycaemia. Diabetes Obes Metab. 13:814–822. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Suzuki D, Toyoda M, Kondo M, et al:
Efficacy of long-acting insulin analog insulin glargine at high
dosage for basal-bolus insulin therapy in patients with type 2
diabetes. Tokai J Exp Clin Med. 37:35–40. 2012.PubMed/NCBI
|
|
14
|
Pistrosch F, Köhler C, Schaper F, Landgraf
W, Forst T and Hanefeld M: Effects of insulin glargine versus
metformin on glycemic variability, microvascular and beta-cell
function in early type 2 diabetes. Acta Diabetol. 50:587–595. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Xie Y, Mo C, Jin P, et al: The influence
of short-term intensive insulin therapy on β-cell function in newly
diagnosed type 2 diabetes. Chin J Diabetes. 16:225–227. 2008.
|
|
16
|
Zeng L, Lu H, Deng H, Mu P, Li X and Wang
M: Noninferiority effects on glycemic control and β-cell function
improvement in newly diagnosed type 2 diabetes patients: basal
insulin monotherapy versus continuous subcutaneous insulin infusion
treatment. Diabetes Technol Ther. 14:35–42. 2012.
|
|
17
|
Toyoda M, Kimura M, Yamamoto N, Miyauchi
M, Umezono T and Suzuki D: Insulin glargine improves glycemic
control and quality of life in type 2 diabetic patients on
hemodialysis. J Nephrol. 25:989–995. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Delgado E; LAUREL Spain study
investigators. Outcomes with insulin glargine in patients with type
2 diabetes previously on NPH insulin: evidence from clinical
practice in Spain. Int J Clin Pract. 66:281–288. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Holman RR, Paul SK, Bethel MA, Matthews DR
and Neil HA: 10-year follow-up of intensive glucose control in type
2 diabetes. N Engl J Med. 359:1577–1589. 2008.PubMed/NCBI
|
|
20
|
Zoungas S, Patel A, Chalmers J, et al;
ADVANCE Collaborative Group. Severe hypoglycemia and risks of
vascular events and death. N Engl J Med. 363:1410–1418. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gerstein HC, Miller ME, Byington RP, et
al; Action to Control Cardiovascular Risk in Diabetes Study Group.
Effects of intensive glucose lowering in type 2 diabetes. N Engl J
Med. 358:2545–2559. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Patel A, MacMahon S, Chalmers J, et al;
ADVANCE Collaborative Group. Intensive blood glucose control and
vascular outcomes in patients with type 2 diabetes. N Engl J Med.
358:2560–2572. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Duckworth W, Abraira C, Moritz T, et al;
VADT Investigators. Glucose control and vascular complications in
veterans with type 2 diabetes. N Engl J Med. 360:129–139. 2009.
View Article : Google Scholar : PubMed/NCBI
|