Introduction
Age-related macular degeneration (AMD) is a disease
of the ocular fundus characterized by the degeneration of the
choroidal capillaries, retinal pigment epithelium (RPE) and neural
retina. AMD is the leading cause of blindness in older adults
(>50 years-old) in Western countries (1). With living standards improving in
China, the incidence of AMD is also increasing.
Traditionally, AMD may be classified into dry and
wet forms by physicians. The dry form, or central geographic
atrophy, accounts for 15–20% of AMD cases, where vision loss is
ultimately caused by the loss of photoreceptors. Wet AMD, also
known as neovascular or exudative AMD, results from choroidal
neovascularization (CNV) and affects 80–85% of those with AMD. The
wet form causes the more severe loss of vision. In the natural
course of the disease, 10–20% of dry AMD cases become wet AMD
cases, and 42% of patients with monocular wet AMD develop binocular
wet AMD within five years (2).
Recently, a large-scale epidemiological study
(n=100,000) undertaken in Shanghai First People’s Hospital
(Shanghai, China) reported that the prevalence of AMD in
individuals aged >45 years was 16%; wet AMD alone was 15%
(3). AMD is the most common
manifestation of CNV, and CNV usually leads to repeated macular
bleeding, exudation and scarring, seriously damaging central visual
acuity. As a result, investigation into the pathogenesis of AMD is
urgently required and important for the prevention or delaying of
AMD progression (4–7).
The present study included an epidemiological survey
of ocular diseases in an adult population (>45 years old) in
Youyi Road Community, Baoshan District, Shanghai, China, conducted
to determine the prevalence of AMD in the region. For this purpose,
routine ocular examinations were utilized, namely fundus
photography, fundus fluorescein angiography (FFA) and ocular
optical coherence tomography (OCT). Patients found to have early
and intermediate-stage AMD were further recruited for follow-up
observation. In these patients, the clinical and imaging
characteristics of various stages of AMD were investigated, as well
as the CNV characteristics of different etiologies. The present
study aimed to further the understanding of the pathomorphological
and functional variations of CNV in AMD patients, and optimize the
guidance for the treatment of AMD.
Materials and methods
Subject recruitment
The study was a prospective, population-based study
investigating the pathomorphological and functional variations of
CNV in AMD patients in a Chinese population. In total, 1,813 adult
citizens aged >45 years were recruited through probability
sampling from Youyi Road Community, Baoshan District, Shanghai,
China between April 2005 and June 2005 for an epidemiological
survey. All the participants provided written informed consent. The
study was approved by the local Ethics Committee of Shuguang
Hospital (Baoshan branch, Shanghai, China) and was conducted in
accordance with the Declaration of Helsinki.
Ocular examination
All the participants underwent a preliminary
assessment of near and far visual acuity, slit-lamp biomicroscopy
and a dilated fundus examination with direct ophthalmoscopy and a
90D handheld lens. For those subjects with suspected early and
mid-stage AMD, further ocular examinations, including fundus
photography, FFA and fast macular map and line scans using OCT,
were performed. The best corrected visual acuity was assessed
monocularly with linear logMAR charts, if the subject had an
uncorrected visual acuity of <1.0 (less than 20/20 vision).
Pupillary dilation was induced with three cycles of 0.5%
tropicamide (one drop per eye), administered 5 min apart. Fundus
photography, FFA and OCT were performed synchronously using a
Zeiss-Stratus OCT Model 3000 and an FF450 IR fundus camera (Carl
Zeiss AG, Oberkochen, Germany).
According to the size and the number of drusens
under the retina, dry AMD may be further classified into three
stages: Early, intermediate and advanced stages (8). Dry AMD is the most common form of AMD
in the early or intermediate stages. Early AMD was defined as the
presence of coexisting multiple small drusens (diameter, <63 μm)
and a few medium-sized drusens (63–124 μm) in the macular area. The
presence of widespread medium-sized drusens and at least one drusen
of >125 μm defined intermediate AMD. Advanced AMD was indicated
by the presence of either geographic atrophy involving the fovea or
exudative detachment induced by CNV. The subjects with early and
intermediate-stage AMD were included in the present study. Subjects
were excluded from the study if the FFA results were negative,
fundus visibility was poor due to lens opacity or other reasons or
if the patient had a history of central chorioretinitis or macular
degeneration (which is difficult to distinguish from AMD). A
trained technician performed all the scanning sessions.
Follow-up
Subjects with early and intermediate-stage AMD were
reviewed one year following the initial examination. Thereafter,
the patients were reviewed for 6–24 months depending on the stage
of AMD. Mean follow-up duration ranged from 18 to 24 months while
the interval of follow-up of each patient ranged from 6–18 months.
During the follow-up period, the following ocular examinations were
performed: Best corrected visual acuity, anterior segment analysis
by a slit-lamp, dilated fundus evaluation by direct ophthalmoscopy
and a 90D handheld lens, fundus photography, FFA and OCT. Patients
with angiogenesis or geographic atrophy were administered the
appropriate drug treatment and were withdrawn from the study.
ICGA was performed using Carl Zeiss FF-450-IR Fundus
Retinal Eye Medical Ophthalmic Camera System, 30° and 50° macular
CF and indocyanine green ICG 25 mg (LiaoYang No. 3 Pharmaceutical
factory, LiaoYang, China). After allergic test, rapid intravenous
elbow injection of ICG was performed within 5 sec. ICGA observation
duration was 30 min or more in total after injection in which the
early stage was within 5 min, 10 to 20 min as a medium stage, and
after 20 min as late stage of angiography. The results were
analyzed by two ophthalmologists independently.
Statistical analysis
All data are expressed as the mean ± standard error
of the mean. Intergroup comparisons were conducted with the
χ2 test using the SigmaStat-integrated SigmaPlot
statistical software package (V 12.0; SPSS, Inc., Chicago, IL,
USA). P<0.05 was considered to indicate a statistically
significant difference for all the analyses.
Results
Patient characteristics
A total of 1,813 subjects were initially enrolled,
however, only 1,619 individuals (89.3%) completed the study.
Participants included workers with a number of professions,
including manual labor, peasants, teachers and civil servants. The
majority of the patients belonged to China’s main ethnic group (Han
Chinese). The enrolled 1,813 subjects comprised 829 females
(45.65%) and 987 males (54.35%), ranging in age between 45 and 82
years.
AMD diagnosis
Among the 1,619 subjects who completed the study, 59
patients (3.64%, 70 eyes) were diagnosed as early and
intermediate-stage AMD, while 42 patients (2.59%, 45 eyes) were
diagnosed with advanced AMD. Exudative (wet) AMD (including macular
disciform scars) was identified in nine subjects (10 eyes), which
was 0.56% of those who completed the study and 21.4% of advanced
AMD patients. Atrophic (dry) AMD was found in 33 cases (35 eyes),
which was 2.04% of the final number of patients enrolled and 78.57%
of advanced AMD patients.
Combined FFA and OCT examination provided the
highest detection rate of AMD for early and intermediate-stage AMD
patients, which was significantly better than the detection rates
when the techniques were performed alone (all P<0.05; Tables I and II).
 | Table IComparison of three diagnostic methods
for early and intermediate-stage AMD. |
Table I
Comparison of three diagnostic methods
for early and intermediate-stage AMD.
| Diagnostic
method | Cases, n | Detected cases,
n | Detection rate,
% |
|---|
| Fundus
examination | 1619 | 39 | 2.41 |
| FFA | 1325 | 48 | 3.62 |
| OCT | 1619 | 62 | 3.83 |
| Combined FFA and
OCT | 1325 | 59 | 4.45 |
 | Table IIComparison of three diagnostic methods
for advanced-stage AMD. |
Table II
Comparison of three diagnostic methods
for advanced-stage AMD.
| Diagnostic
method | Case, n | Detected cases,
n | Detection rate,
% |
|---|
| Fundus
examination | 1619 | 50 | 3.09 |
| FFA | 1325 | 36 | 2.72 |
| OCT | 1619 | 42 | 2.59 |
| Combined FFA and
OCT | 1325 | 42 | 3.17 |
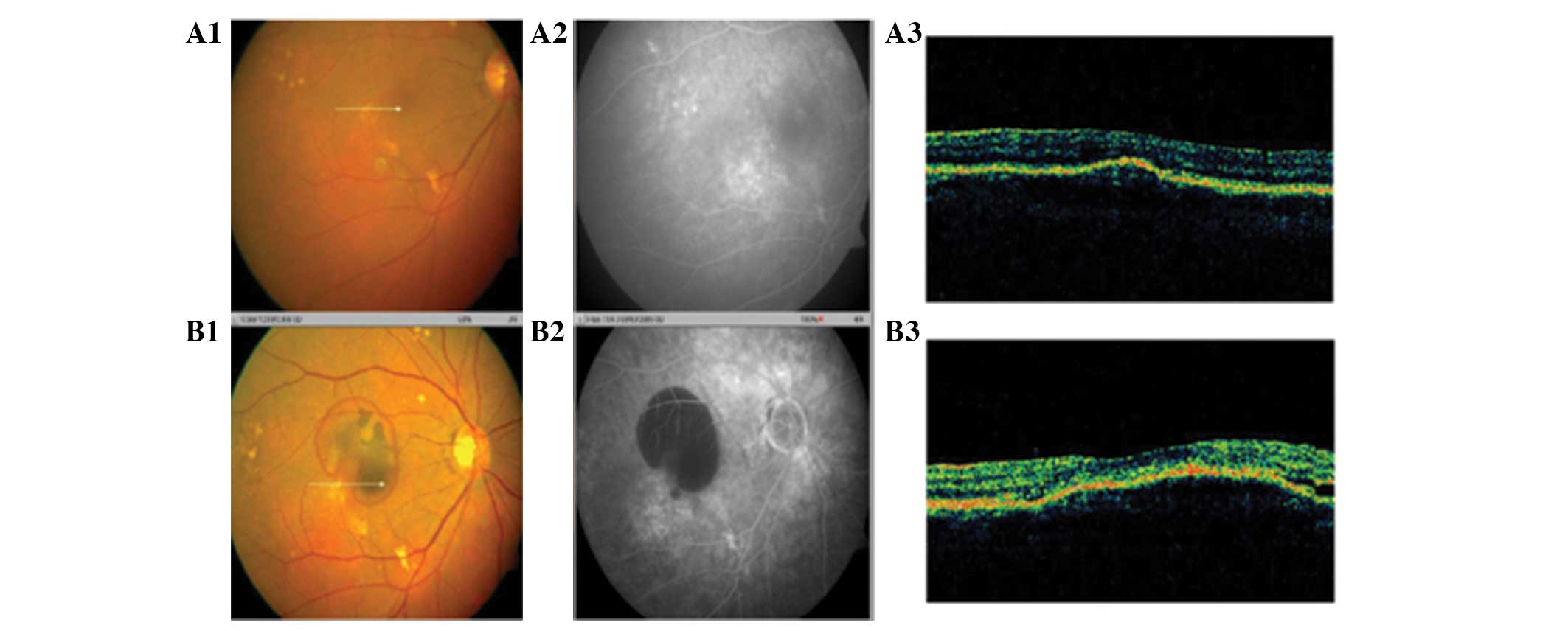
Follow-up observations
In total, 59 early and intermediate-stage AMD
patients were followed-up for 18–54 months (mean follow-up time,
38.6±11.3 months) and all underwent complete ocular examinations
during this time. Five eyes (3.62%) developed into geographic
atrophy 56 months after the initial recruitment examination (mean
duration, 43.6±9.3 months; Fig.
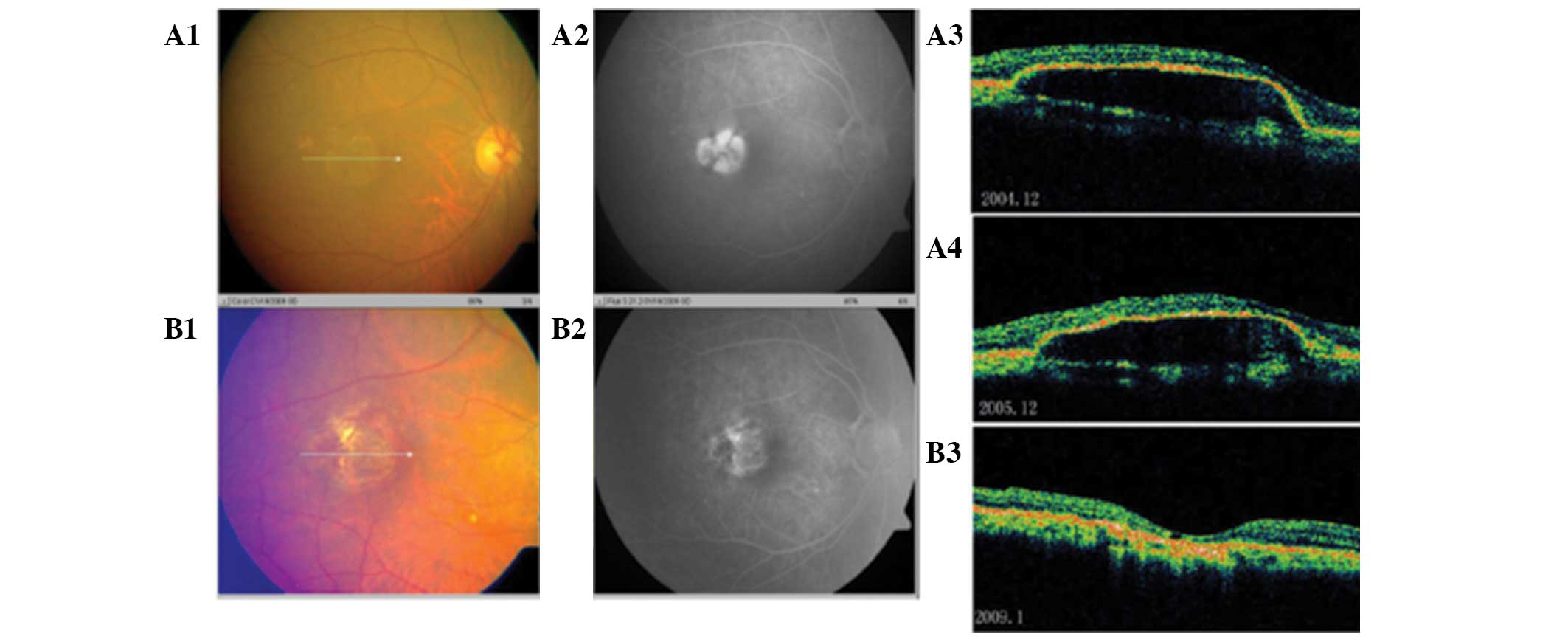
1). A total of four eyes (2.9%) developed into exudative AMD
between 22 and 37 months following the initial examination (mean
duration, 21.2±12.8 months; Fig.
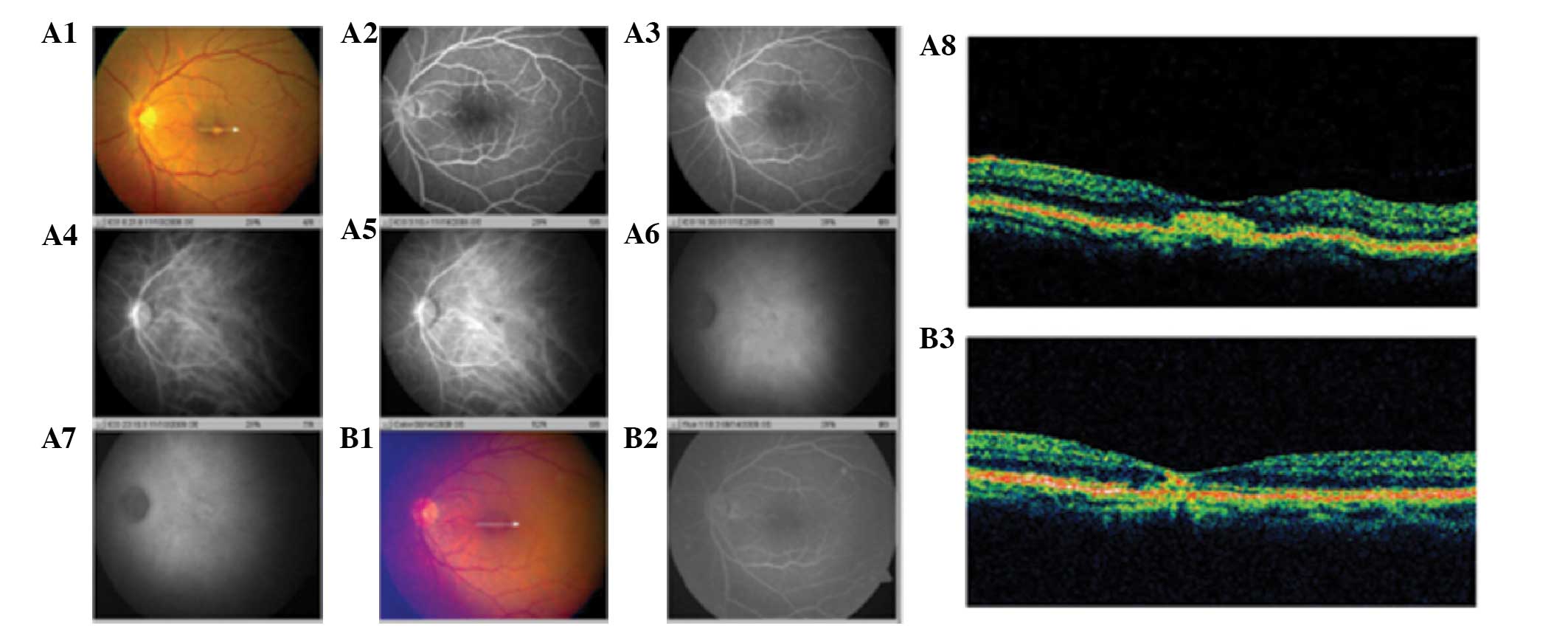
2). Calcific drusens were absorbed in one eye (0.72%) 33 months
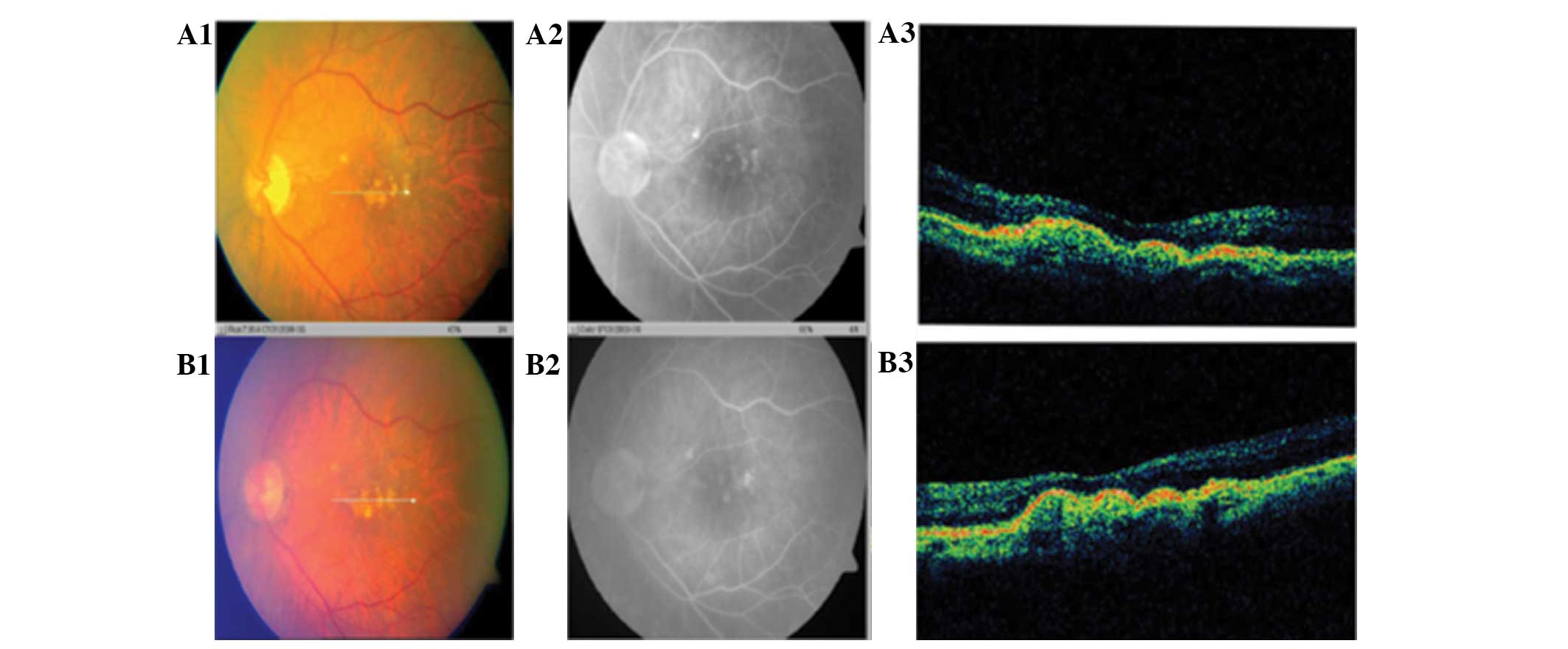
following the initial recruitment examination (Fig. 3). In 40 eyes (56.5%), increased or
fused drusens were observed between 44 and 60 months subsequent to
the initial recruitment examination (mean duration, 47.6±10.5
months; Fig. 4).
Discussion
As China becomes an aging society, the prevalence of
age-related diseases has significantly increased. AMD is one of the
leading causes of blindness and poor vision, resulting in an
inability to work or live independently, which adds a heavy burden
on the individual, the family and society. Since macular damage is
irreversible, early detection and timely treatment are important in
preventing the enlargement and coalescence of drusens and early
CNV, thereby reducing or delaying visual impairment and improving
the patients’ quality of life (9–12).
An epidemiological survey of AMD in Youyi Road
Community, Baoshan District, Shanghai, China was performed between
April 2005 and June 2005. Individuals with early and
intermediate-stage AMD were selected to investigate the
pathomorphological and functional variations of CNV in AMD patients
in a Chinese population. The natural course of AMD was
satisfactorily observed and recorded using OCT combined with FFA.
FFA is useful for assessing the range of RPE damage, while OCT can
quantify the thickness of the neurosensory retina and detect traces
of subretinal fluid and early thinning of the neural cortex in
atrophic AMD. In addition, OCT can be used to determine the degree
of damage to the photoreceptors, Bruch’s membrane and the
choriocapillary layer (CCL) (13).
The clinical staging criteria of the Age-Related Eye
Disease Study do not include a clear definition of vision. It is
increasingly recognized that patients with early and
intermediate-stage AMD without macular involvement can usually
maintain good eyesight. Furthermore, visual impairment is usually
gradual and severity varies with the lesion site. As a result,
classification of AMD is less meaningful if stages of its
pathogenesis are based on vision. Thus, we hypothesize that it is
more practical in clinical practice to base the severity of AMD on
the fundus phenotype as viewed by OCT and FFA, rather than declined
vision.
OCT and FFA were combined to diagnose and follow-up
patients with early and intermediate-stage AMD, focusing on the
organic and functional changes observed in the macular area of the
photoreceptors, RPE and CCL. Detection via combined OCT and FFA
provides a more accurate and objective assessment of AMD damage.
Fundus photography revealed that there were two eyes (2.9%) that
developed exudative changes, including unclear drusen borders and
proliferating pigments, among the 59 patients (70 eyes) with early
and intermediate-stage AMD that were followed-up for 18–54 months.
The aforementioned cases presented with central blocked
fluorescence in the center of the drusens, fuzzy weak fluorescence
around the drusens and mild enhanced fluorescence in advanced
stages of FFA imaging. As exudative changes advanced, the original
drusens became obscure and large areas of subretinal or
subpigmental hemorrhages appeared in the fundus images. In
addition, the bleeding site was blocked, fluorescein leakage had
occurred due to neovascularization and fluorescence accumulation in
cavities of pigment epithelial detachment and neurosensory retinal
detachment were observed through FFA. OCT showed wide range of dome
bands within the RPE/CCL area (14,15).
When geographic atrophy occurred, RPE serous detachment in the
macular area, over a range of one pupillary distance, was observed
in the fundus images, FFA and OCT scans. During the follow-up, RPE
detachment was gradually absorbed, the pigments were deposited and
eventually the photoreceptors, RPE and choroidal capillaries became
thinner.
In conclusion, FFA is a valuable tool for making a
definitive diagnosis of AMD, however, the invasiveness of the
procedure limits the usage on a single patient. OCT is a
noninvasive test that can provide an in vivo, objective and
precise measurement of macular and retinal nerve fiber layer
thickness. OCT has become popular and is used widely in clinical
practice worldwide. The advantages and characteristics of this
technique have been thoroughly described previously (16–18).
OCT enables ophthalmologists to diagnose retinal diseases by
detecting small changes in retinal and macular morphology,
including the thickness and volume. As a result, OCT is an easier
and more comfortable method to follow-up patients with early and
intermediate-stage AMD, and the facilitation of OCT in the
diagnosis of retinal diseases contributes to a positive
significance in clinical practice.
Acknowledgements
The study was supported by grants from the Projects
of Shanghai Municipal Health Bureau Key Specialty Construction (no.
ZK2012A03), the Science and Technology Commission of Baoshan
District, Shanghai (no. 08-E-6) and the Integrative Medicine
Hospital Key Specialty Construction of Baoshan District, Shanghai
(no. ZXYZK2012A03).
References
|
1
|
Stevens GA, White RA, Flaxman SR, et al;
Vision Loss Expert Group. Global prevalence of vision impairment
and blindness: magnitude and temporal trends, 1990–2010.
Ophthalmology. 120:2377–2384. 2013.
|
|
2
|
de Jong PT: Age-related macular
degeneration. N Engl J Med. 355:1474–1485. 2006.
|
|
3
|
Zou H, Zhang X, Xu X and He Z:
Epidemiology survey of rhegmatogenous retinal detachment in Beijing
districts, Shanghai. Zhonghua Yan Ke Za Zhi. 38:580–583. 2002.(In
Chinese).
|
|
4
|
Klein R, Klein BE, Tomany SC, Meuer SM and
Huang GH: Ten-year incidence and progression of age-related
maculopathy: The Beaver Dam eye study. Ophthalmology.
109:1767–1779. 2002.
|
|
5
|
Friedman DS, O’Colmain BJ, Muñoz B, et al;
Eye Diseases Prevalence Research Group. Prevalence of age-related
macular degeneration in the United States. Arch Ophthalmol.
122:564–572. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Seddon JM, Ajani UA, Sperduto RD, et al:
Dietary carotenoids, vitamins A, C, and E, and advanced age-related
macular degeneration. Eye Disease Case-Control Study Group. JAMA.
272:1413–1420. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tan JS, Wang JJ, Flood V, Rochtchina E,
Smith W and Mitchell P: Dietary antioxidants and the long-term
incidence of age-related macular degeneration: the Blue Mountains
Eye Study. Ophthalmology. 115:334–341. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ferris FL, Davis MD, Clemons TE, et al;
Age-related Eye Disease Study (AREDS) Research Group. A simplified
severity scale for age-related macular degeneration: AREDS Report
No 18. Arch Ophthalmol. 123:1570–1574. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fung AE, Lalwani GA, Rosenfeld PJ, et al:
An optical coherence tomography-guided, variable dosing regimen
with intravitreal ranibizumab (Lucentis) for neovascular
age-related macular degeneration. Am J Ophthalmol. 143:566–583.
2007. View Article : Google Scholar
|
|
10
|
Lalwani GA, Rosenfeld PJ, Fung AE, et al:
A variable-dosing regimen with intravitreal ranibizumab for
neovascular age-related macular degeneration: year 2 of the PrONTO
Study. Am J Ophthalmol. 148:43–58. 2009.PubMed/NCBI
|
|
11
|
Funk M, Karl D, Georgopoulos M, et al:
Neovascular age-related macular degeneration: intraocular cytokines
and growth factors and the influence of therapy with ranibizumab.
Ophthalmology. 116:2393–2399. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gass JD: Biomicroscopic and
histopathologic considerations regarding the feasibility of
surgical excision of subfoveal neovascular membranes. Am J
Ophthalmol. 118:285–298. 1994. View Article : Google Scholar
|
|
13
|
Petrarca R, Dugel PU, Nau J, Slakter JS,
Jaffe GJ and Jackson TL: Macular epiretinal brachytherapy in
treated age-related macular degeneration (MERITAGE): Month 12
optical coherence tomography and fluorescein angiography.
Ophthalmology. 120:328–333. 2013. View Article : Google Scholar
|
|
14
|
Souied EH, Delcourt C, Querques G, et al:
Oral docosahexaenoic acid in the prevention of exudative
age-related macular degeneration: the Nutritional AMD Treatment 2
study. Ophthalmology. 120:1619–1631. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Morrison MA, Silveira AC, Huynh N, et al:
Systems biology-based analysis implicates a novel role for vitamin
D metabolism in the pathogenesis of age-related macular
degeneration. Hum Genomics. 5:538–568. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Paunescu LA, Schuman JS, Price LL, et al:
Reproducibility of nerve fiber thickness, macular thickness, and
optic nerve head measurements using StratusOCT. Invest Ophthalmol
Vis Sci. 45:1716–1724. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hess DB, Asrani SG, Bhide MG, Enyedi LB,
Stinnett SS and Freedman SF: Macular and retinal nerve fiber layer
analysis of normal and glaucomatous eyes in children using optical
coherence tomography. Am J Ophthalmol. 139:509–517. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Medeiros FA, Zangwill LM, Bowd C and
Weinreb RN: Comparison of the GDx VCC scanning laser polarimeter,
HRT II confocal scanning laser ophthalmoscope, and stratus OCT
optical coherence tomograph for the detection of glaucoma. Arch
Ophthalmol. 122:827–837. 2004. View Article : Google Scholar : PubMed/NCBI
|