Introduction
Amyloidosis refers to the extracellular accumulation
of amyloid fibrils in various tissues and organs, which may result
in the disruption of their function. Amyloid fibrils are a specific
type of protein aggregate which, upon deposition in particular
tissues, may cause serious illness that is often fatal when major
organs are involved, or when the amyloidosis is systemic (1,2).
Amyloid tumors, in contrast to systemic amyloidosis,
are localized deposits that are usually accompanied by mild
clinical symptoms (3). The
presence of these deposits has been reported in a number of
anatomical sites, including the orbit, neck, oral cavity, breasts,
heart, liver and nervous system (3,4).
Common clinical conditions associated with amyloid tumors are
long-term hemodialysis, chronic inflammation and infections,
including tuberculosis and osteomyelitis. Occasionally, patients
have been reported to have amyloid deposits in the soft tissue
(5), bladder (6) or the respiratory (7) and gastrointestinal tracts (8) without clinical symptoms.
Diabetes mellitus is a highly prevalent illness and
a number of diabetic patients require treatment with subcutaneous
insulin injections. A previous study demonstrated that insulin
injections are associated with local amyloidosis (9). Usually, these are case reports of
patients who have detected an abnormal mass in the injection site
(10–12). From these studies, it may be
hypothesized that amyloidosis may be observed regardless of the
location of the injection (13).
For example, insulin amyloids have been observed in the shoulders
(2), arm (14) and abdominal walls (14–16),
and frequently in the areas surrounding the injection site. The
formation of insulin fibrils occurs regardless of the source
(14) and type (10,11)
of insulin administered.
During the course of studying amyloid formation and
its prevention, in vitro tests on the potential toxicity of
amyloid fibrils and associated structures are usually performed on
cells (17,18) or organelles (19). The subsequent step to this would be
experiments on laboratory animals that are models of the specific
amyloid-related disease (for example Alzheimer’s disease) (20–23).
However, to the best of our knowledge, an animal model for local
amyloidosis has not yet been presented. The method established in
the present study may be used as a general representation of local
amyloidosis, in a similar manner to the use of the in vitro
fibril formation of model proteins, as an indicator of the behavior
of pathogenic proteins.
Materials and methods
Animals
Eight male NMRI mice weighing 26–28 g (average
weight 27 g) were obtained from the Pasteur Institute of Tehran
(Tehran, Iran) and acclimatized to the new location for a week. All
animals were housed under standard conditions with a 12 h
dark/light cycle, 50% humidity, a temperature of 22±2°C and free
access to water and food (standard pellet feed). The present study
was approved by the Animal Ethics Committee of the Science and
Research Branch at the Islamic Azad University (Tehran, Iran).
Amyloid preparation
Regular insulin (EXIR Pharmaceutical Co., Tehran,
Iran) was diluted in 50 mM phosphate buffer (pH 7.4) to 0.5 mg/ml.
It was incubated at 57°C for 24 h whilst being stirred by Teflon
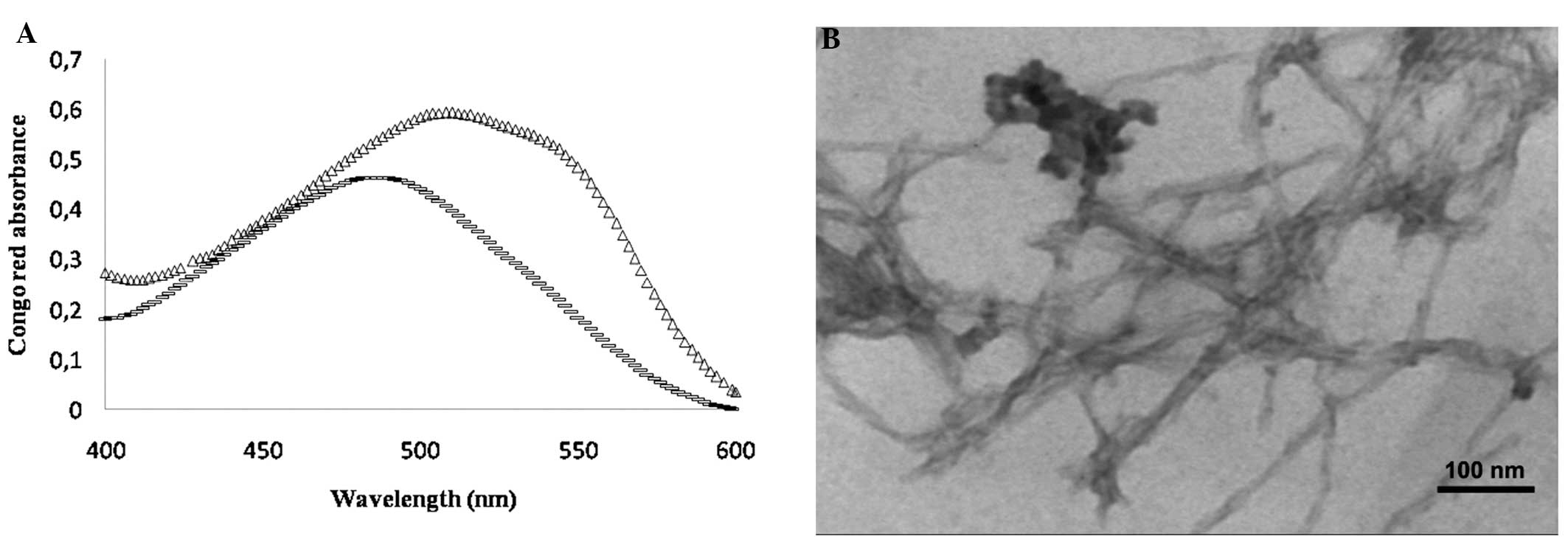
magnetic bars. To confirm the amyloid fibril formation of regular
insulin, a Congo red absorbance assay was performed according to a
previously described method (24).
Images captured under a transmission electron microscopy (TEM; CEM
902A Zeiss microscope; Carl Zeiss, Jena, Germany) were also used as
complementary proof. The Congo red kit was obtained from
Sigma-Aldrich (St. Louis, MO, USA).
Experimental groups
Eight mice were randomly divided into two groups
(n=4). The first group (control) received daily injections of
phosphate buffer (an insulin amyloid vehicle) for 21 consecutive
days. The second group (experimental) received daily injections of
amyloid fibrils (113 μl) subcutaneously for 21 consecutive days.
All groups received their normal diet during the experimental
period.
Histological processing
After 21 days, the waxy masses were excised. Tissue
sections were embedded in paraffin and hematoxylin and eosin
(H&E), as well as Congo red and Sudan black staining, were
applied to each tissue block. A light microscope (Carl Zeiss AG,
Oberkochen, Germany) was used to observe the tissue secion.
Results
Model development
The in vitro incubation of insulin under
amyloidogenic conditions resulted in the formation of insulin
fibrils. The shift observed in the absorption spectrum of Congo red
(Fig. 1), along with the TEM
images indicating the presence of distinct fibrils, were taken as
validation of insulin amyloid formation. The pre-formed amyloids
were subsequently injected into the mice.
Tumor formation
After 21 days, no abnormalities in appearance around
the injection site were observed in the control group. An abnormal
mass was detected in all mice in the experimental group. Two mice
from the experimental group were randomly selected, and a biopsy
was performed. The masses formed upon amyloid injection were waxy
bodies of a white-yellow color and a size of ~10×10×2
mm3. The masses appeared similar to the areas of
lipohypertrophy observed in human diabetic cases as previously
reported (9,25).
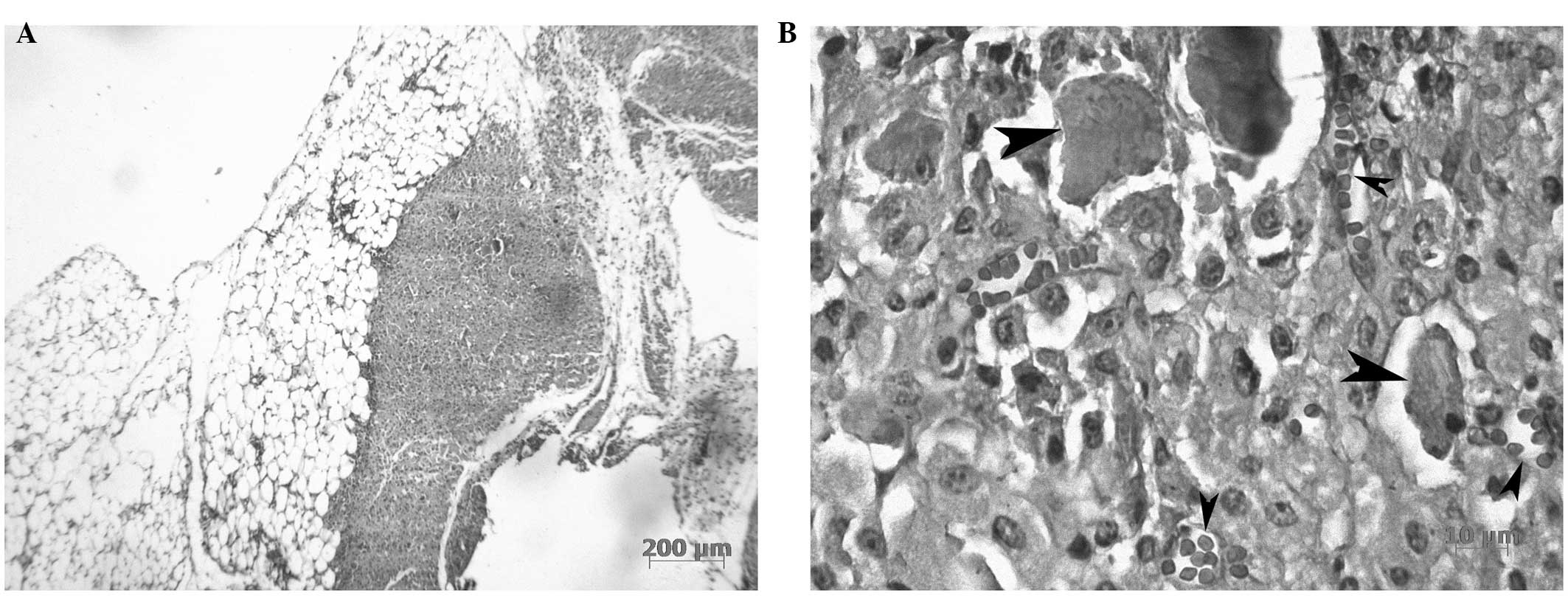
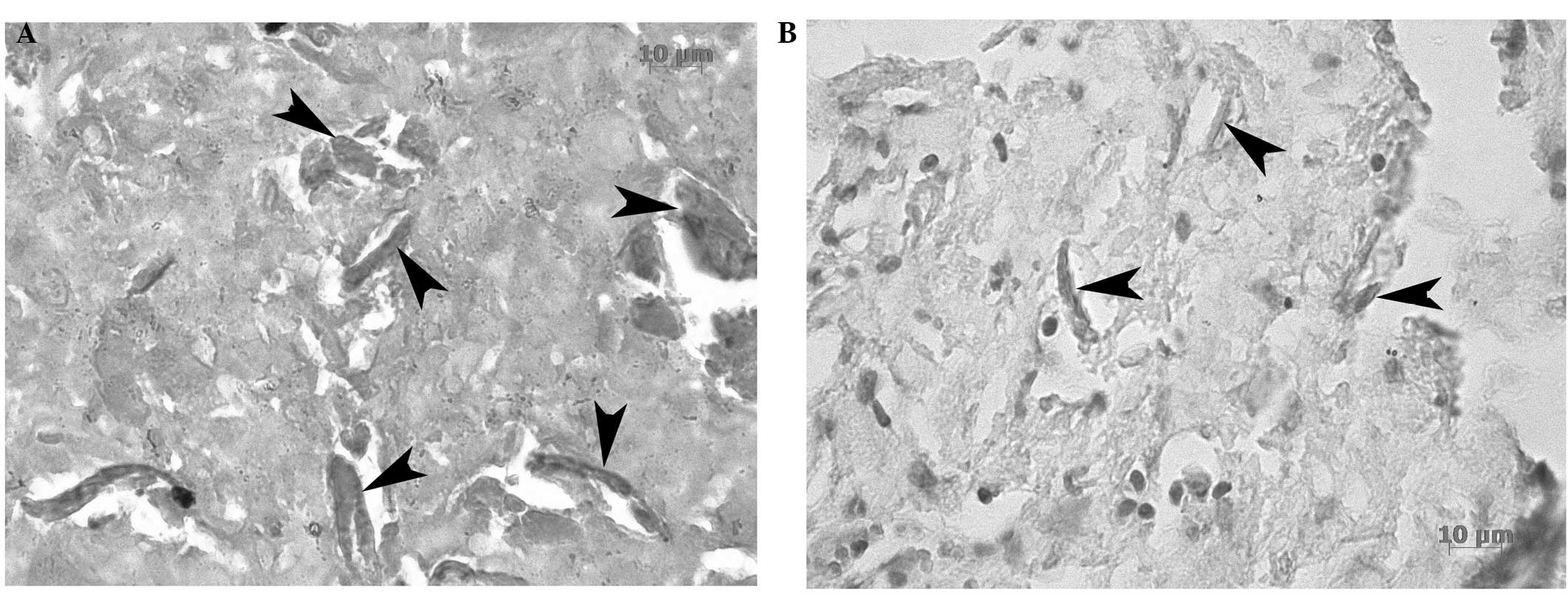
Tissue staining and analysis
Upon microscopic investigation of the tissues,
localized amyloid fibrils surrounded by connective tissue were
detected following H&E staining (Fig. 2). Congo red staining was also
performed (Fig. 3), since it is a
specific stain for the detection of amyloid structures (24). Sudan black staining confirmed that
the excised tissue included adipose tissue (Fig. 3). Based on these results, it was
concluded that an amyloid tumor containing fibrillar deposits was
formed at the injection site of the two mice.
Discussion
More than 20 proteins and 24 protein precursors that
are able to form amyloid fibrils in a comparable manner have been
reported (26,27). In vivo, the deposition of
these fibrils in the extracellular environment results in
amyloidosis (28). Usually,
soluble proteins become insoluble and are deposited as protein
aggregates which then develop into amyloids (29,30).
There are various types of amyloidosis which, in general, may be
classified as primary (AL) and secondary (AA). AL amyloidosis is
related to the deposition of immunoglobulin light chains. AA
amyloidosis occurs with chronic disease, especially when an
inflammatory process is present (2,12,31).
The disease may influence several organs, or may be limited to a
particular organ. Symptoms related to amyloidosis depend on the
organ involved (32,33).
The skin may become involved with amyloidosis at
various levels. Primary cutaneous amyloidosis occurs as nodular,
macular and lichen (or papular) amyloidosis (33,34).
In the latter two types, amyloid fibrils accumulate in the
papillary dermis. An uncommon form of amyloidosis may affect the
subcutis, dermis and vascular walls, causing local plasma cell
dyscrasia (35,36). Nodular amyloidosis has a higher
relapse rate compared with the other forms. The development of
local cutaneous disease to a systemic form is rare, but has been
reported for nodular amyloidosis (37,38).
To the best of our knowledge, no specific therapeutic treatments
currently exist for skin amyloidosis and surgical excision is the
routine treatment. The method that has been reported in the present
study may be expanded and used to test potential treatments for
these conditions.
In diabetic patients, a cutaneous amyloid tumor may
form at the site of insulin injection (11,25).
Within the tumor, lipohypertrophy, which includes the amyloid
fibrils, is usually present (11,25).
The results of the current study are in accordance with this type
of physiopathological finding. From 1983, incidences of amyloidosis
in insulin injection sites have been reported in rats (11).
As previously mentioned, there are a limited number
of published case reports about cutaneous amyloidosis caused by
repeated subcutaneous insulin administration (2,15,14).
A limited number of studies have associated cutaneous amyloidosis
with non-human insulin, such as porcine insulin, and there are even
fewer published studies investigating amyloidosis with human
insulin (2,16).
One form of cutaneous amyloidosis is related to
local subcutaneous injections of insulin, the incidence rate of
which may be underestimated when considering the high prevalence of
diabetes mellitus and insulin treatment. The simple method proposed
in the present study may be useful in investigating the
characteristics of local amyloidosis, as well in the search for
potential treatments. The exact mechanism by which insulin-induced
amyloidosis occurs remains largely unknown in the scientific
literature. Notably, in previous studies, insulin itself was
observed to have properties of lipohypertrophy, while the present
study used injections of insulin amyloid fibrils and observed the
same effect. It has been verified that long-term injection of
insulin may result in lipohypertrophy, lipoatrophy and, rarely,
infection (25). Further tests are
required to ascertain whether insulin amyloid injection may cause
the same effects. Another use for the method established in the
current study may be to investigate the tendency of various insulin
types to cause amyloidosis. Finally, irrespective of the
amyloidosis type, the present method may be used to further study
local amyloidosis.
Acknowledgements
The authors thank those who assisted in carrying out
this study, particularly Dr Aidin Dilmaghanian for providing useful
comments and for taking light-microscopic images, as well as Dr
Farnaz Banakar and Ms. Raheleh Kheirbakhsh for their valuable
assitance with regard to the in vivo experiment.
References
|
1
|
Husby G: Amyloidosis and rheumatoid
arthritis. Clin Exp Rheumatol. 3:173–180. 1985.
|
|
2
|
Sahoo S, Reeves W and DeMay RM: Amyloid
tumor: a clinical and cytomorphologic study. Diagn Cytopathol.
28:325–328. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
3
|
Aono J, Yamagata K and Yoshida H: Local
amyloidosis in the hard palate: a case report. Oral Maxillofac
Surg. 13:119–122. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Weiss SW and Goldblum JR: Enzinger and
Weiss’s Soft Tissue Tumors. 4th edition. Mosby Elsevier;
Philadelphia, PA, USA: 2001
|
|
5
|
Krishnan J, Chu WS, Elrod JP and Frizzera
G: Tumoral presentation of amyloidosis (amyloidomas) in soft
tissues. A report of 14 cases. Am J Clin Pathol. 100:135–144.
1993.PubMed/NCBI
|
|
6
|
Khan SM, Birch PJ, Bass PS, Williams JH
and Theaker JM: Localized amyloidosis of the lower genitourinary
tract: a clinicopathological and immunohistochemical study of nine
cases. Histopathology. 21:143–147. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ihling C, Weirich G, Gaa A and Schaefer H:
Amyloid tumors of the lung - an immunocytoma? Pathol Res Pract.
192:446–452. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Deans GT, Hale RJ, McMahon RF and Brough
WA: Amyloid tumour of the colon. J Clin Pathol. 48:592–593. 1995.
View Article : Google Scholar
|
|
9
|
Sie MP, van der Wiel HE, Smedts FM and de
Boer AC: Human recombinant insulin and amyloidosis: an unexpected
association. Neth J Med. 68:138–140. 2010.PubMed/NCBI
|
|
10
|
Dische FE, Wernstedt C, Westermark GT,
Westermark P, Pepys MB, Rennie JA, Gilbey SG and Watkins PJ:
Insulin as an amyloid-fibril protein at sites of repeated insulin
injections in a diabetic patient. Diabetologia. 31:158–161. 1988.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Störkel S, Schneider HM, Müntefering H and
Kashiwagi S: Iatrogenic, insulin-dependent, local amyloidosis. Lab
Invest. 48:108–111. 1983.PubMed/NCBI
|
|
12
|
Swift B: Examination of insulin injection
sites: an unexpected finding of localized amyloidosis. Diabet Med.
19:881–882. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Muzaffar M and Ahmad A: The mechanism of
enhanced insulin amyloid fibril formation by NaCl is better
explained by a conformational change model. PloS One. 6:e279062011.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yumlu S, Barany R, Eriksson M and Röcken
C: Localized insulin-derived amyloidosis in patients with diabetes
mellitus: a case report. Hum Pathol. 40:1655–1660. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Albert SG, Obadiah J, Parseghian SA,
Yadira Hurley M and Mooradian AD: Severe insulin resistance
associated with subcutaneous amyloid deposition. Diabetes Res Clin
Pract. 75:374–376. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Shikama Y, Kitazawa J, Yagihashi N, Uehara
O, Murata Y, Yajima N, Wada R and Yagihashi S: Localized
amyloidosis at the site of repeated insulin injection in a diabetic
patient. Intern Med. 49:397–401. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
El-Agnaf OM, Jakes R, Curran MD, Middleton
D, Ingenito R, Bianchi E, Pessi A, Neill D and Wallace A:
Aggregates from mutant and wild-type α-synuclein proteins and NAC
peptide induce apoptotic cell death in human neuroblastoma cells by
formation of β-sheet and amyloid-like filaments. FEBS letters.
440:71–75. 1998.
|
|
18
|
Hertel C, Hauser N, Schubenel R,
Seilheimer B and Kemp JA: β-amyloid-induced cell toxicity:
enhancement of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium
bromide-dependent cell death. J Neurochem. 67:272–276. 1996.
|
|
19
|
Meratan AA, Ghasemi A and Nemat-Gorgani M:
Membrane integrity and amyloid cytotoxicity: a model study
involving mitochondria and lysozyme fibrillation products. J Mol
Biol. 409:826–838. 2011. View Article : Google Scholar
|
|
20
|
Maurice T, Lockhart BP and Privat A:
Amnesia induced in mice by centrally administered β-amyloid
peptides involves cholinergic dysfunction. Brain Res. 706:181–193.
1996.
|
|
21
|
Morimoto K, Yoshimi K, Tonohiro T, Yamada
N, Oda T and Kaneko I: Co-injection of β-amyloid with ibotenic acid
induces synergistic loss of rat hippocampal neurons. Neuroscience.
84:479–487. 1998.
|
|
22
|
Piermartiri TC, Vandresen-Filho S, de
Araújo Herculano B, Martins WC, Dal’agnolo D, Stroeh E, Carqueja
CL, Boeck CR and Tasca CI: Atorvastatin prevents hippocampal cell
death due to quinolinic acid-induced seizures in mice by increasing
Akt phosphorylation and glutamate uptake. Neurotox Res. 16:106–115.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Prediger RD, Franco JL, Pandolfo P,
Medeiros R, Duarte FS, Di Giunta G, Figueiredo CP, Farina M,
Calixto JB, Takahashi RN and Dafre AL: Differential susceptibility
following β-amyloid peptide-(1–40) administration in C57BL/6 and
Swiss albino mice: Evidence for a dissociation between cognitive
deficits and the glutathione system response. Behav Brain Res.
177:205–213. 2007.
|
|
24
|
Klunk WE, Pettegrew J and Abraham DJ:
Quantitative evaluation of congo red binding to amyloid-like
proteins with a β-pleated sheet conformation. J Histochem Cytochem.
37:1273–1281. 1989.PubMed/NCBI
|
|
25
|
Wallymahmed ME, Littler P, Clegg C,
Haqqani MT and Macfarlane IA: Nodules of fibrocollagenous scar
tissue induced by subcutaneous insulin injections: a cause of poor
diabetic control. Postgrad Med J. 80:732–733. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Westermark P, Araki S, Benson MD, Cohen
AS, Frangione B, Masters CL, Saraiva MJ, Sipe JD, Husby G, Kyle RA
and Selkoe D: Nomenclature of amyloid fibril proteins: Report from
the meeting of the International Nomenclature Committee on
Amyloidosis; August 8–9, 1998; Part 1: Amyloid. 6. pp. 63–66.
1999
|
|
27
|
Westermark P, Benson MD, Buxbaum JN, Cohen
AS, Frangione B, Ikeda S, Masters CL, Merlini G, Saraiva MJ and
Sipe JD: Amyloid fibril protein nomenclature - 2002. Amyloid.
9:197–200. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Cortés A: Primary cutaneous amyloidosis.
Dermatologica. 139:109–114. 1969.
|
|
29
|
Kumar V, Abbas AK, Fausto N and Aster JC:
Robbins and Cotran Pathologic Basis of Disease. 8th edition.
Saunders Elsevier; Philadelphia, PA, USA: 2010
|
|
30
|
Rooban T, Saraswathi T, Al Zainab FH, Devi
U, Eligabeth J and Ranganathan K: A light microscopic study of
fibrosis involving muscle in oral submucous fibrosis. Indian J Dent
Res. 16:131–134. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Lasagna-Reeves CA, Clos AL, Midoro-Hiriuti
T, Goldblum RM, Jackson GR and Kayed R: Inhaled insulin forms toxic
pulmonary amyloid aggregates. Endocrinology. 151:4717–4724. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Hazenberg BP, van Gameren II, Bijzet J,
Jager PL and van Rijswijk MH: Diagnostic and therapeutic approach
of systemic amyloidosis. Neth J Med. 62:121–128. 2004.PubMed/NCBI
|
|
33
|
Yamamoto T: Amyloidosis in the skin.
Amyloidosis - an Insight to Disease of Systems and Novel Therapies.
Güvenç IA: InTech; Rijecka, Croatia: pp. 91–104. 2011
|
|
34
|
Touart DM and Sau P: Cutaneous deposition
diseases. Part I. J Am Acad Dermatol. 39:149–171. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Moon AO, Calamia KT and Walsh JS: Nodular
amyloidosis: review and long-term follow-up of 16 cases. Arch
Dermatol. 139:1157–1159. 2003.PubMed/NCBI
|
|
36
|
Truhan AP, Garden JM and Roenigk HH Jr:
Nodular primary localized cutaneous amyloidosis:
immunohistochemical evaluation and treatment with the carbon
dioxide laser. J Am Acad Dermatol. 14:1058–1062. 1986. View Article : Google Scholar
|
|
37
|
Steciuk A, Dompmartin A, Troussard X,
Verneuil L, Macro M, Comoz F and Leroy D: Cutaneous amyloidosis and
possible association with systemic amyloidosis. Int J Dermatol.
41:127–132. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Woollons A and Black MM: Nodular localized
primary cutaneous amyloidosis: a long-term follow-up study. Br J
Dermatol. 145:105–109. 2001. View Article : Google Scholar : PubMed/NCBI
|