Introduction
The laryngeal mask airway (LMA) is a relatively new
device that was brought into clinical practice in the 1980s. The
LMA avoids undergoing laryngoscopy as well as all of its adverse
effects. Additionally, it is less invasive to the respiratory tract
and tracheal oedema, which may be caused by tracheal intubation,
does not occur by using the LMA. Furthermore, it may be life saving
in patients with malformations of the upper airway after a failure
of tracheal intubation and mask ventilation. The laryngeal mask
airway (LMA) is considered to be an extremely useful alternative to
the endotracheal tube (ETT) in a number of clinical scenarios.
Compared with conventional ETTs, the LMA causes less airway
resistance, a decreased bronchoconstrictive reflex, less
atelectasis and fewer pulmonary infections (1). However, the application of the LMA in
thoracic anesthesia has been limited due to the requirement of
one-lung ventilation (OLV), which appeared impossible for the LMA.
Although reported as a useful adjunct in patients undergoing
thoracotomy (2), the LMA alone has
no possibility for OLV. In 1999, the Arndt endobronchial blocker,
designed by Dr G.A. Arndt (3,4),
emerged as a versatile alternative to double-lumen tubes (DLTs) to
facilitate OLV in thoracic anesthesia (5–8).
Previously, the combination of the LMA and the Arndt
endobronchial blocker was reported in a pediatric scoliosis case
(9). We hypothesized that the
combination could also be applied safely to thoracic cases,
bringing the advantages of fewer airway injuries, fewer
fluctuations in hemodynamics and fewer limitations for OLV,
enabling use in patients with difficult airways and in pediatric
patients.
In the present prospective pilot study, the
feasibility of OLV provided by the combination of the Arndt
endobronchial blocker and the LMA ProSeal™ was assessed, and
comparisons of the post-operative airway morbidity and the
respiratory and hemodynamic data regarding the two strategies of
OLV were performed.
Materials and methods
Patient recruitment
The study was approved by the Human Ethics Committee
of Huashan Hospital (Shanghai, China) and written informed consent
was obtained from all the patients. Fifty-five adult patients (age,
20–70 years; American Society of Anesthesiologists physical status,
I-III) who were undergoing day-case thoracic surgeries were entered
into the study prospectively. All patients were randomly allocated
to group Arndt (n=26) or group DLT (n=29). Exclusion criteria
included an age of <20 years, pre-operative hoarseness,
increased risk of aspiration, mouth opening of <2.5 cm and
surgeries predicted to have long durations.
Anesthesia procedure
Anesthetic monitoring, including
electrocardiography, pulse oximetry, capnography and non-invasive
blood pressure monitoring, was conducted prior to anesthesia
induction and during the procedure. Prior to the induction of
anesthesia, an arterial line was established for determining the
baseline of arterial blood gas, blood pressure and heart rate. All
patients were anesthetized by two chief residents who were
experienced in the use of the LMA, the Arndt endobronchial blocker
and DLT. General anesthesia was induced and maintained with target
controlled infusion using a Graseby™ 3500 syringe pump (Smith
Medical MD, Inc., St. Paul, MN, USA) of propofol at 4.0 μg/ml
(plasma concentration) and continuous infusion of 3 μg/kg/h
fentanyl and 0.8 mg/kg/h rocuronium. In group Arndt, the LMA
ProSeal (LMA North America, Inc., San Diego, CA, USA) was placed
and the patient was ventilated with pressure-controlled mode to
achieve a tidal volume of 10 ml/kg (Primus Dräger, Lübeck,
Germany). An Arndt endobronchial blocker (Cook Medical Critical
Care, Bloomington, IN, USA) was subsequently placed and guided by a
3.4-mm fiberoptic scope (FOB; BF type 3 C40; Olympus, Tokyo,
Japan). In group DLT, the patients were intubated with DLTs and
were ventilated with the same ventilator regimen. Positioning was
confirmed by the same FOB. The blood pressures were read from the
arterial line and the heart rates were recorded following placement
of the airway devices and cuff position confirmation. A manometer
for LMA (Mallinckrodt, Griesheim, Germany) was used to measure and
control the cuff pressure between 55 and 60 cmH2O. Peak
airway pressure and compliance were measured using an S/5 Compact
Anesthesia Monitor (Datex-Ohmeda, Madison, WI, USA) and recorded
while the patient was in both the supine and the lateral decubitus
positions. Subsequent to patients being positioned to the lateral
decubitus, the cuff position of the endobronchial blocker or of the
DLT’s endobronchial tube was checked again.
Evaluation of lung isolation
The evaluation of lung collapse and surgery exposure
was performed by a thoracic surgeon blinded to the group
assignment. Collapse of the lung was assessed as follows: 1,
spontaneous; 2, assisted with suction; 3, manual. The conditions of
surgery were rated as follows: 1, excellent (complete collapse with
perfect surgical exposure); 2, fair (total collapse, but with
residual air remaining in the lung); 3, poor (no collapse or
partial collapse with interference in surgical exposure) (10).
Bronchoscopic examination
Upon completion of surgery, all patients underwent a
bronchoscopic examination prior to emerging from anesthesia.
Findings from the bronchoscopy and laryngoscopy were classified
into bronchus, vocal cord and larynx injuries, and each injury
class was scored as follows (10):
0, no changes; 1, redness; 2, edema; and 3, hematoma.
Assessment of post-operative airway
morbidity
For the first three days after surgery,
post-operative airway morbidity was rated by the anesthesia
resident blinded to the group assignment. The assessment was
performed in accordance with that described in the study by Knoll
et al (10).
Statistical analysis
Patients were randomized using the sealed envelope
system. All patients were stratified on gender and airway
resistance information obtained from the pre-operative spirometry
examination. Statistical analysis was performed using SPSS software
version 14.0 (SPSS Inc., Chicago, IL, USA). Results were considered
statistically significant when P<0.05. Data are expressed as the
mean ± standard deviation. The independent samples t-test and
Mann-Whitney U test were used for analyzing parametric and
nonparametric data as appropriate.
Results
Fifty-five patients were enrolled in this study. The
two groups were comparable in terms of age, male/female ratio,
height, weight, pre-operative spirometry results and pre-operative
hemodynamic parameters (Table I).
In the context of the types of surgical procedures and the
establishment of airways, the two groups were comparable (Tables II and III).
 | Table IDemographic data. |
Table I
Demographic data.
| Variable | Group Arndt,
n=26 | Group DLT, n=29 |
|---|
| Age (years)a | 55±15 | 57±13 |
| Gender (M/F) | 18/8 | 17/12 |
| Height (cm)a | 166±9 | 167±9 |
| Weight (kg)a | 62±11 | 64±10 |
| FVC (%)a | 83±18 | 89±13 |
| FEV1 (%)a | 89±25 | 89±14 |
| Pre-op BP
(mmHg)a | 148±25 | 143±22 |
| Pre-op HR
(bpm)a | 75±16 | 76±10 |
| Smoking history
(n) | 16 | 14 |
| Surgery duration
(h)a | 3.3±1.7 | 3.1±2.1 |
| Anesthesia duration
(h)a | 3.7±1.9 | 4.2±1.8 |
| OLV duration
(h)a | 1.7±1.2 | 1.8±1.1 |
 | Table IIDistribution of types of surgical
procedures. |
Table II
Distribution of types of surgical
procedures.
| Type of
procedure | Group Arndt (n) | Group DLT (n) |
|---|
| VATS | 7 | 6 |
| Wedge resection | 6 | 7 |
| Lobectomy | 5 | 7 |
| Segmentectomy | 2 | 2 |
| Pneumonectomy | 1 | 1 |
| Mediastinal mass
resection | 3 | 2 |
| Esophageal
procedures | 2 | 4 |
 | Table IIIAirway parameters. |
Table III
Airway parameters.
| Parameter | Group Arndt | Group DLT | P-value |
|---|
| Mallampati grade | 2.3±1.2 | 2.2±1.3 | 0.82 |
| Cormack grade | 2.5±1.4 | 2.3±1.3 | 0.72 |
| Intubation attempts
(n) | 1.2±0.1 | 1.1±0.1 | 0.59 |
| Intubation duration
(min) | 3.3±0.3 | 3.4±0.6 | 0.89 |
| Positioning attempts
(n) | 1.2±0.1 | 1.2±0.1 | 0.88 |
| Positioning duration
(min) | 5.2±0.7 | 3.0±0.4 | 0.08 |
| Adjustments (n) | 0.7±0.2 | 0.4±0.1 | 0.33 |
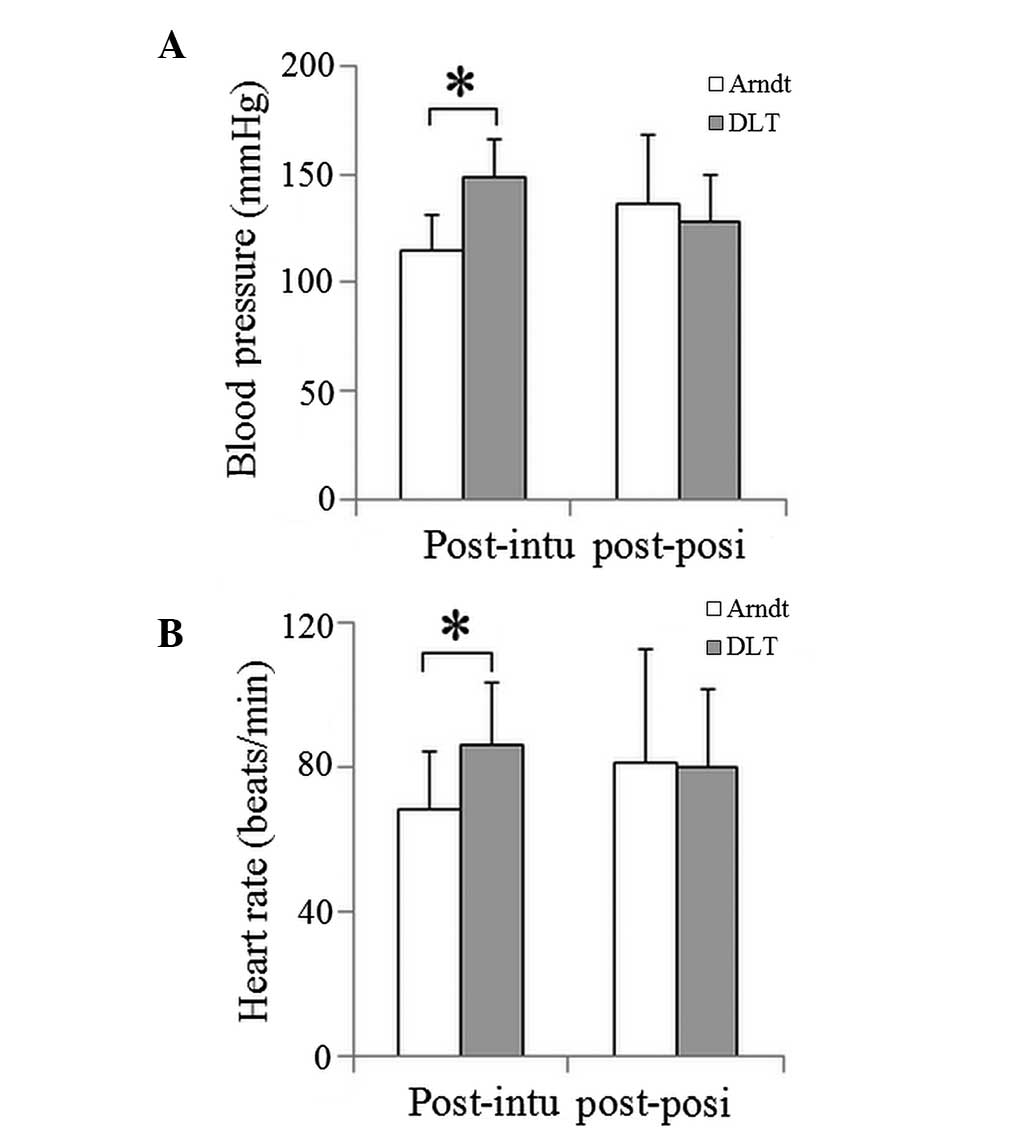
Significantly attenuated cardiovascular responses
following the insertion of the LMA and endobronchial blocker or DLT
were observed in group Arndt compared with group DLT (P<0.05)
(Fig. 1). The cardiovascular
responses induced by repositioning of the endobronchial blocker or
the DLT were similar in the two groups. The respiratory parameters
were comparable between the two groups with the exception of the
peak airway pressure 5 min after OLV (Table IV). No significant differences
were identified in oxygenation condition between the two groups
(Table V).
 | Table IVRespiratory parameters of the two
groups. |
Table IV
Respiratory parameters of the two
groups.
| PAP (mmHg) | Lung compliance
(ml/cmH2O) |
|---|
|
|
|
|---|
| Time | Group Arndt | Group DLT | Group Arndt | Group DLT |
|---|
| DLV 1 | 16.9±3.7 | 18.4±3.3 | 42.1±14.1 | 47.7±11.9 |
| DLV 2 | 19.3±3.8 | 19.7±3.4 | 35.7±7.8 | 41.5±9.4 |
| OLV 5 | 19.3±3.6a | 19.7±3.6 | 35.7±7.8 | 41.5±9.5 |
| OLV 20 | 24.6±4.8 | 25.0±3.9 | 25.7±9.8 | 27.8±7.6 |
| OLV 60 | 24.7±4.9 | 25.5±3.8 | 25.7±8.9 | 25.8±6.7 |
| DLV 5 | 24.9±4.3 | 26.3±3.3 | 26.0±8.8 | 26.3±7.4 |
| DLV 10 | 20.4±4.9 | 19.9±4.7 | 43.0±17.8 | 42.4±13.7 |
| DLV 20 | 22.2±5.2 | 21.1±4.5 | 37.6±17.7 | 41.2±12.8 |
 | Table VOxygenation and lung isolation of the
two groups. |
Table V
Oxygenation and lung isolation of the
two groups.
| Evaluation
measure | Arndt | DLT | P-value |
|---|
| Pre-op
PaO2/FiO2 | 400±52 | 362±62 | 0.15 |
| OLV 20
PaO2/FiO2 | 209±89 | 184±82 | 0.29 |
| DLV 20
PaO2/FiO2 | 461±60 | 454±65 | 0.65 |
| Average exposure
score | 1.2±0.4 | 1.1±0.3 | 0.35 |
| Average lung
collapse score | 1.2±0.6 | 1.1±0.4 | 0.54 |
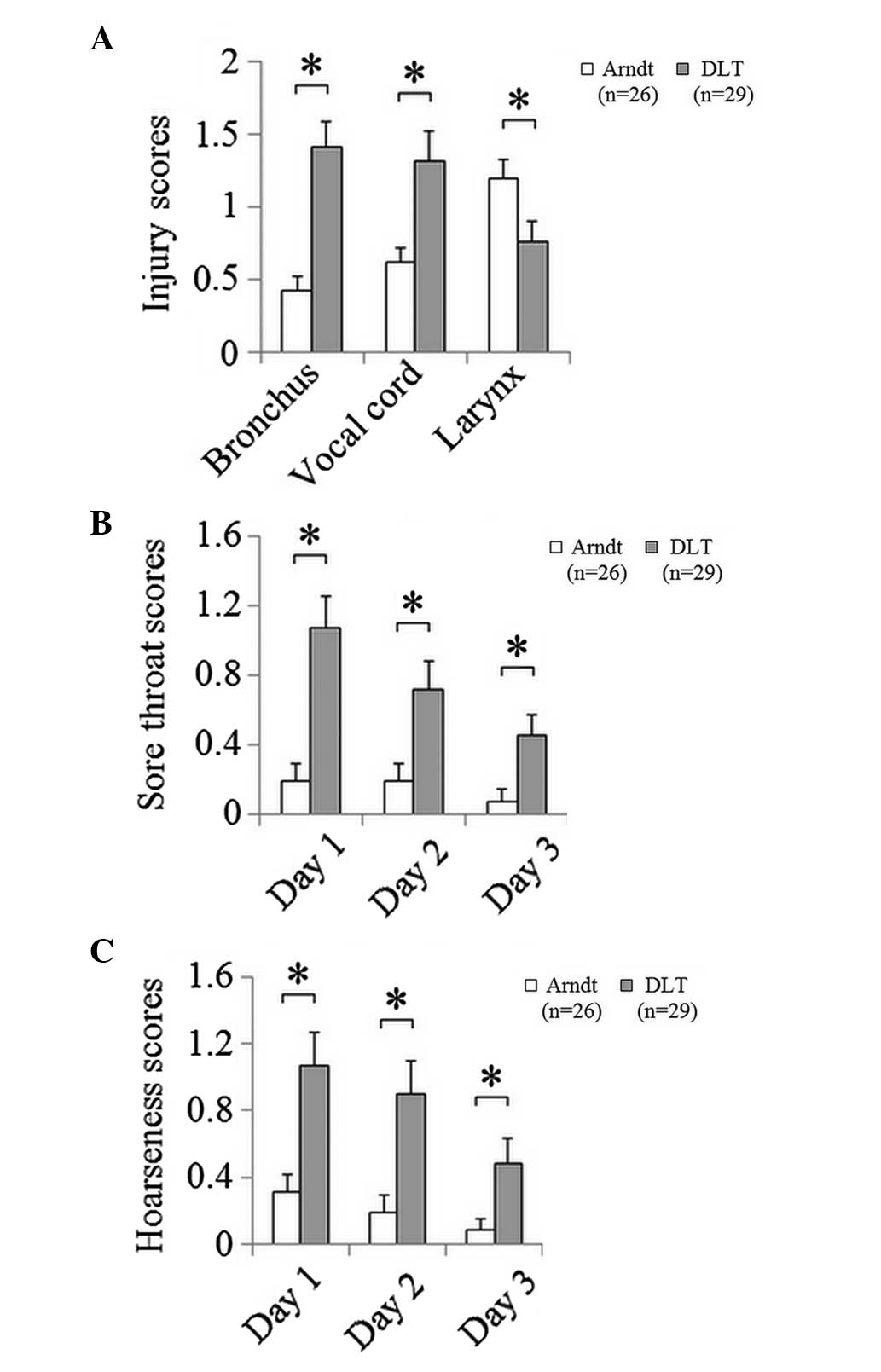
Bronchoscopic examination revealed that the injury
scores of the bronchus and vocal cords were significantly higher in
group DLT than those in group Arndt, while the larynx injury score
was lower in group DLT (Fig. 2A).
The incidences of post-operative (three days after surgery) sore
throat and hoarseness were significantly lower in group Arndt than
those in group DLT (Fig. 2B and
C).
Discussion
DLTs are the most widely used devices for OLV;
however, they have been reported to be associated with potential
bronchus injury and sore throat (10). In cases of difficult airways, the
intubation process of DLT may be further complicated when switching
from a single-lumen tube with the help of the tube exchanger. The
American Society of Anesthesiologists and the European
Resuscitation Council have published algorithms naming the LMA as a
primary option for the management of difficult and failed airways
(11–13). Enabling OLV to be performed with
the LMA would mean that difficult airways could be easily handled.
However, the LMA alone is not able to provide OLV for thoracic
surgeries. The Arndt endobronchial blocker has been demonstrated to
be a useful technique that produces comparable surgical exposure in
thoracotomy when combined with a conventional single-lumen tube.
The present study evaluated the possibility of the combined use of
the LMA and Arndt endobronchial blocker as an alternative OLV
strategy in thoracic surgeries.
In this study, it was revealed that the combination
of the LMA and the Arndt endobronchial blocker was able to provide
effective surgical exposure via OLV, and additionally was
associated with reduced fluctuations in hemodynamic response
(Fig. 1), fewer airway injuries
and less post-operative sore throat and hoarseness (Fig. 2).
The instant surge of blood pressure or heart rate of
patients receiving DLTs may be attributed to the sudden contact of
the tube tip with the bronchial wall during intubation. The
increase may be more extreme in patients with chronic hypertension,
which is a common pre-existing physical condition in patients
undergoing thoracotomy. Episodes of intra-operative hypertension or
hypotension and tachycardia may predispose the patient to adverse
post-operative neurological or cardiac outcomes, including
increased risk of stroke or myocardial infarction. Maintaining
maximum hemodynamic stability is one of the principle goals of
anesthetic management. However, hemodynamic fluctuations are
difficult to avoid during or following direct laryngoscopy and
tracheal intubation. The LMA has particular appeal in such cases.
The use of the LMA was reported to result in an attenuated
cardiovascular response compared with that found with direct
laryngoscopy and endotracheal intubation (14). In the present study, it was shown
that the hemodynamic responses of group Arndt during LMA and
endobronchial blocker insertion were less fluctuated than those of
DLT intubation.
The results of the present study demonstrated that,
with the exception of injuries to the larynx, post-operative airway
injuries were significantly lower in group Arndt than group DLT.
Incidences of sore throat and hoarseness were also notably lower in
group Arndt than group DLT. These findings were consistent with
those of Knoll et al (10),
who compared the airway injury caused by DLT or the Arndt
endobronchial blocker. The LMA ProSeal may cause laryngopharyngeal
mucosal injury not only by the intensity of the LMA cuff pressure
but also in a time-dependent manner. A histological study
demonstrated that prolonged use of the LMA ProSeal in the pig for
<9 h was associated with no or mild alterations in the
laryngopharyngeal mucosa, whereas clear signs of mucosal injury
were observed after ≥12 h use (15). In the present study, due to the
fact that the cuff pressure of the LMA was monitored and controlled
by manometry, the higher risk of larynx injuries in group Arndt may
have been caused by the prolonged use of the LMA due to the
surgical time. Therefore, surgeries of long duration may not be
recommended for the combination of the LMA and endobronchial
blocker. However, for those less invasive day-case thoracic
surgeries spreading rapidly throughout the world, this method may
exhibit its advantages over DLTs.
Although not quantified, reduced secretions were
observed in this study. Using this novel combination, it remains
possible to perform tracheal suctioning through the internal
channel of the FOB. In the present study, the FOB was advanced
through the ventilation port of the LMA, the vocal cords and then
to the trachea and bronchus. The process is relatively complicated,
but suctioning can be performed under direct visualization.
However, there was seldom requirement for suctioning in patients in
the LMA group.
Complications resulting from the use of LMAs are
known to be rare and were only present in 0.15% of >11,000
patients of all ages over a two-year period in a previous survey
(16). When combined with the
Arndt endobronchial blocker to achieve OLV, there may be concerns
over the high pulmonary inflation pressures due either to increased
airway resistance or to low lung compliance during OLV, which may
lead to inadequate ventilation and gastric distension. It was
reported in a previous study that the oropharyngeal leak pressure
of the LMA ProSeal was 32 cmH2O (range, 12–40
cmH2O) (17). In the
present study, the peak airway pressure during OLV was 24.7±4.8
cmH2O in the Arndt group, which is far below the leak
pressure of the LMA ProSeal. Certain patients, even with body
weight <90 kg, may have an inadequate seal with a size 4 LMA,
and would require a change to a size 5 LMA. This has been supported
by a number of previous reports (18,19).
Following the correction of the inadequate seal of the LMA at the
beginning of anesthesia, the OLV process could be performed without
further complications.
The intubation parameters did not demonstrate any
significant difference between the two groups in the present study.
All the anesthesiologists involved in this study were more familiar
with the DLT technique, despite being trained in the combination
technique for several cases previously. It can be predicted that
once the combination technique is completely mastered, fewer
difficulties may be experienced during the airway establishing
process of thoracic anesthesia. However, further studies in this
respect are warranted.
In conclusion, the combination of the LMA and the
Arndt endobronchial blocker can facilitate airway establishment,
even for patients with difficult airways, in addition to causing
fewer hemodynamic fluctuations in the intubation process and
leading to lower incidences of post-operative sore throat and
hoarseness. With these advantages, this novel combination is likely
to serve as an effective alternative OLV strategy for thoracic
surgeries, particularly for those minimally invasive day-case
surgeries that are gaining increasing attention throughout the
world.
Acknowledgements
This study was supported by a grant from the
Shanghai Natural Science Foundation (no. 13ZR1452200).
References
|
1
|
Sener M, Bilen A, Bozdogan N, Kilic D and
Arslan G: Laryngeal Mask Airway insertion with total intravenous
anesthesia for transsternal thymectomy in patients with myasthenia
gravis: report of 5 cases. J Clin Anesth. 20:206–209. 2008.
View Article : Google Scholar
|
|
2
|
Ferson DZ, Nesbitt JC, Nesbitt K, et al:
The laryngeal mask airway: a new standard for airway evaluation in
thoracic surgery. Ann Thorac Surg. 63:768–772. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Arndt GA, Buchika S, Kranner PW and
DeLessio ST: Wire-guided endobronchial blockade in a patient with a
limited mouth opening. Can J Anaesth. 46:87–89. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Arndt GA, DeLessio ST, Kranner PW,
Orzepowski W, Ceranski B and Valtysson B: One-lung ventilation when
intubation is difficult - presentation of a new endobronchial
blocker. Acta Anaesthesiol Scand. 43:356–358. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Arndt GA, Kranner PW, Rusy DA and Love R:
Single-lung ventilation in a critically ill patient using a
fiberoptically directed wire-guided endobronchial blocker.
Anesthesiology. 90:1484–1486. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kabon B, Waltl B, Leitgeb J, Kapral S and
Zimpfer M: First experience with fiberoptically directed
wire-guided endobronchial blockade in severe pulmonary bleeding in
an emergency setting. Chest. 120:1399–1402. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Espí C, García-Guasch R, Ibáñez C,
Fernández E and Astudillo J: Selective lobar blockade using an
arndt endobronchial blocker in 2 patients with respiratory
compromise who underwent lung resection. Arch Bronconeumol.
43:346–348. 2007.(In Spanish).
|
|
8
|
Li PY, Gu HH and Liang WM: Sequential
one-lung ventilation using one Arndt endobronchial blocker in a
pediatric patient undergoing bilateral, video-assisted
thoracoscopic surgery (VATS). J Clin Anesth. 21:4642009. View Article : Google Scholar
|
|
9
|
Li P, Liang W and Gu H: One-lung
ventilation using Proseal laryngeal mask airway and Arndt
endobronchial blocker in paediatric scoliosis surgery. Br J
Anaesth. 103:902–903. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Knoll H, Ziegeler S, Schreiber JU,
Buchinger H, Bialas P, et al: Airway injuries after one-lung
ventilation: a comparison between double-lumen tube and
endobronchial blocker: a randomized, prospective, controlled trial.
Anesthesiology. 105:471–477. 2006. View Article : Google Scholar
|
|
11
|
No authors listed. Practice guidelines for
management of the difficult airway. A report by the American
Society of Anesthesiologists Task Force on Management of the
Difficult Airway. Anesthesiology. 78:597–602. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Benumof JL: Laryngeal mask airway and the
ASA difficult airway algorithm. Anesthesiology. 84:686–699. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kroesen G: Guidelines for the advanced
management of the airway and ventilation during resuscitation. A
statement by the airway and ventilation management working group of
the European Resuscitation Council, 1996 (Resuscitation
1996;31:201–230). Resuscitation. 35:89–90. 1997.PubMed/NCBI
|
|
14
|
Marietta DR, Lunn JK, Ruby EI and Hill GE:
Cardiovascular stability during carotid endarterectomy:
endotracheal intubation versus laryngeal mask airway. J Clin
Anesth. 10:54–57. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Goldmann K, Dieterich J and Roessler M:
Laryngopharyngeal mucosal injury after prolonged use of the ProSeal
LMA in a porcine model: a pilot study. Can J Anaesth. 54:822–828.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Verghese C and Brimacombe JR: Survey of
laryngeal mask airway usage in 11,910 patients: safety and efficacy
for conventional and nonconventional usage. Anesth Analg.
82:129–133. 1996.PubMed/NCBI
|
|
17
|
Keller C, Brimacombe J, Kleinsasser A and
Brimacombe L: The Laryngeal Mask Airway ProSeal(TM) as a temporary
ventilatory device in grossly and morbidly obese patients before
laryngoscope-guided tracheal intubation. Anesth Analg. 94:737–740.
2002.
|
|
18
|
Brimacombe JR: Positive pressure
ventilation with the size 5 laryngeal mask. J Clin Anesth.
9:113–117. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Patki J and Reddy KCN: Six hours positive
pressure ventilation with size 5 laryngeal mask in a 55-kg patient.
Indian J Anaesth. 54:174–175. 2010. View Article : Google Scholar : PubMed/NCBI
|