Introduction
Leiomyomas are the most common esophageal
mesenchymal neoplasms, even though their occurrence is rare.
Patients with esophageal leiomyomas are usually asymptomatic. The
most common symptoms, when present, include epigastric discomfort,
dysphagia, regurgitation, gastrointestinal bleed, diarrhea and
weight loss. Esophageal leiomyomas are occasionally detected
incidentally during the examination of other gastrointestinal
diseases, of which the majority are identified during endoscopic
examination or upper gastrointestinal radiography (1–4).
Considering the tumor size and position, patient’s symptoms,
general condition and comorbidities, surgical treatment should be
determined. In the present study, the case of an esophageal
leiomyoma is reported, which was incidentally detected on a plain
chest radiograph performed during an annual survey of
mass-screening for lung cancer.
Case report
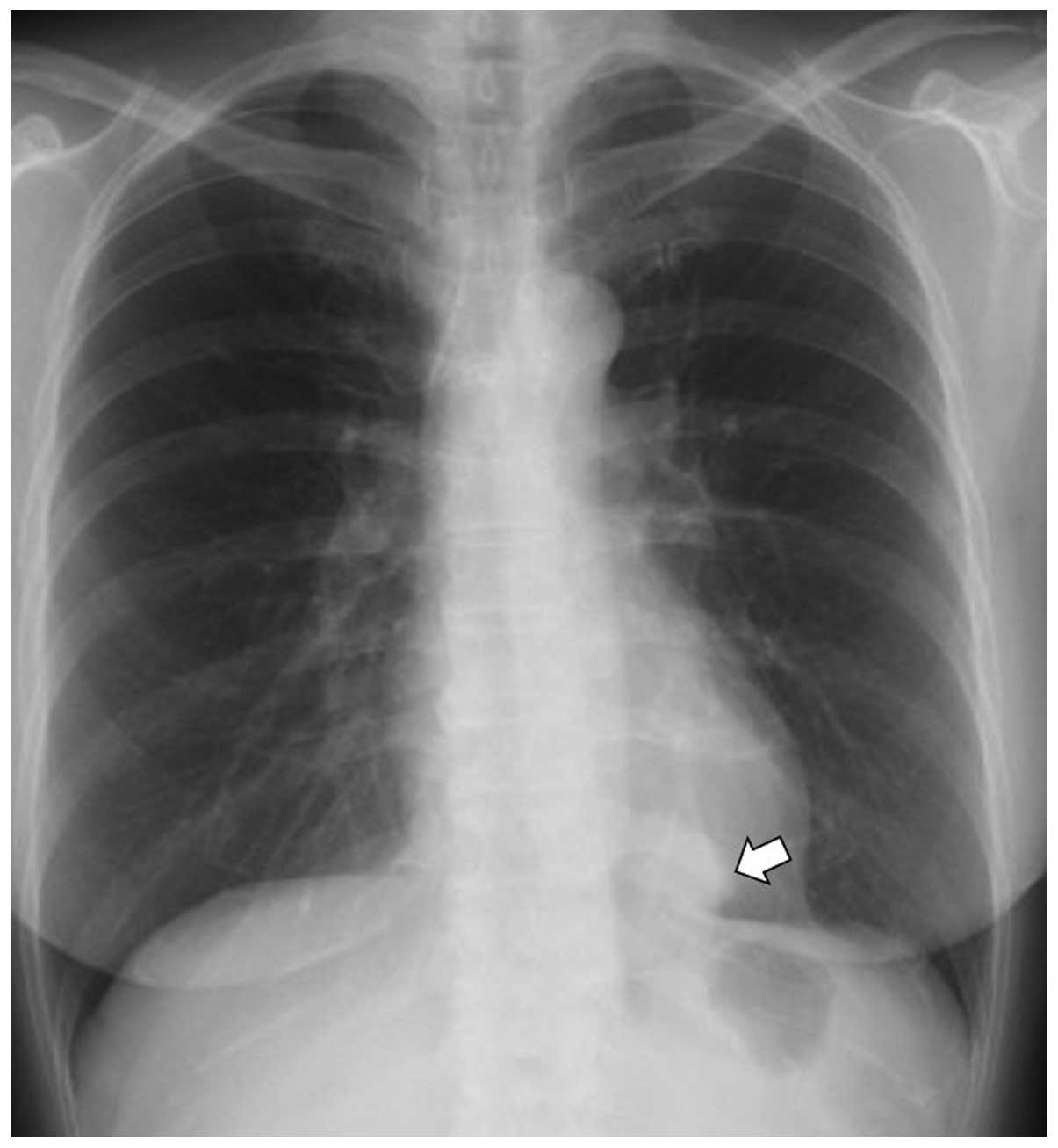
A 55-year-old female was referred to the Mito
Medical Center (Mito, Japan) following the detection of a nodule on
a chest radiograph performed during an annual survey of
mass-screening (Fig. 1). The
mass-screening was performed one month prior to this study. The
patient did not present any symptoms, such as dysphagia or
epigastric pain, had never smoked and had no previous medical
history. Physical examination was unremarkable and the results of
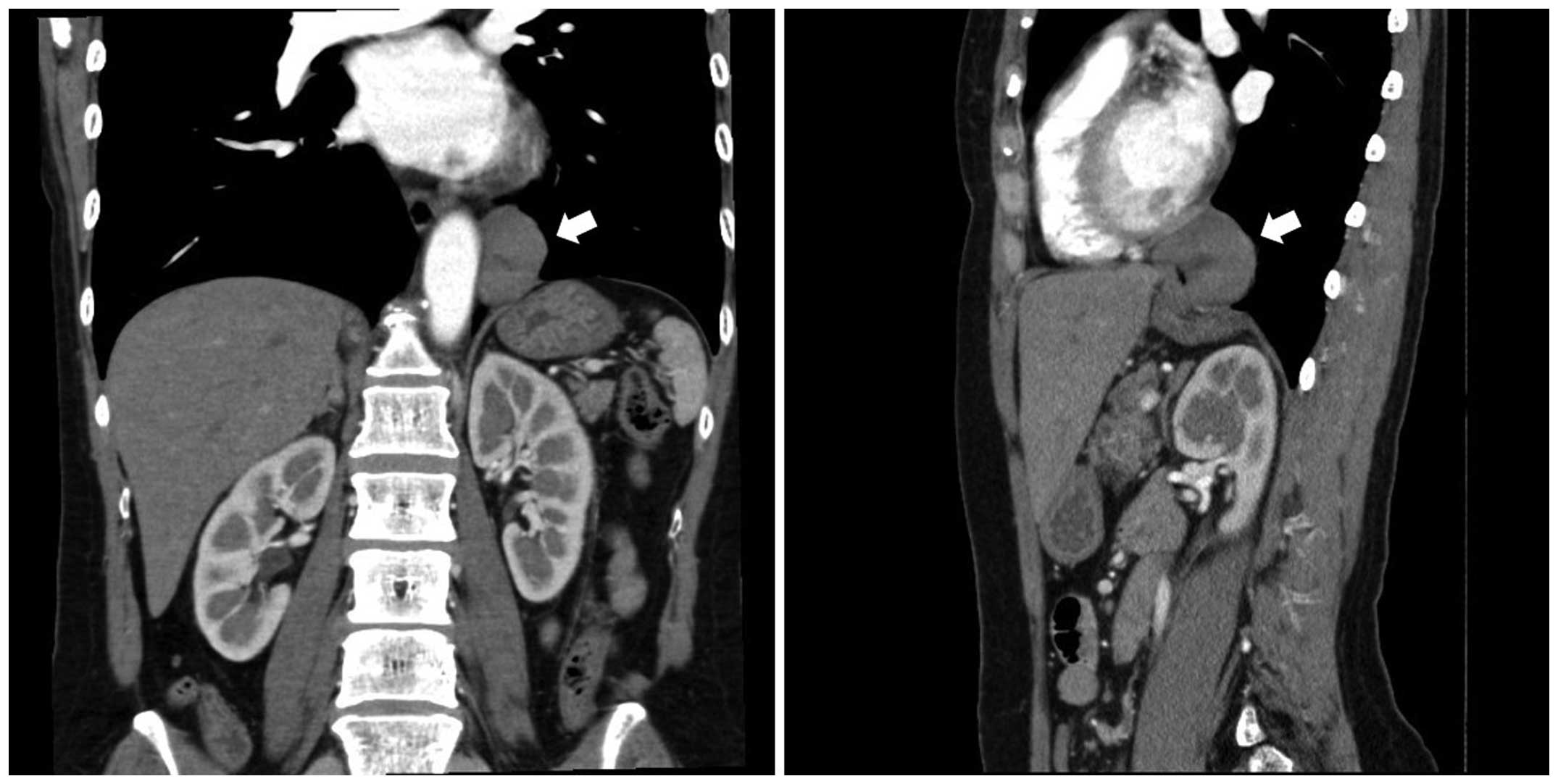
standard laboratory tests were normal. A chest and abdominal
computed tomography (CT) scan (Aquilion 64; Toshiba, Tokyo, Japan)
detected a nodule measuring 5 cm in diameter at the distal
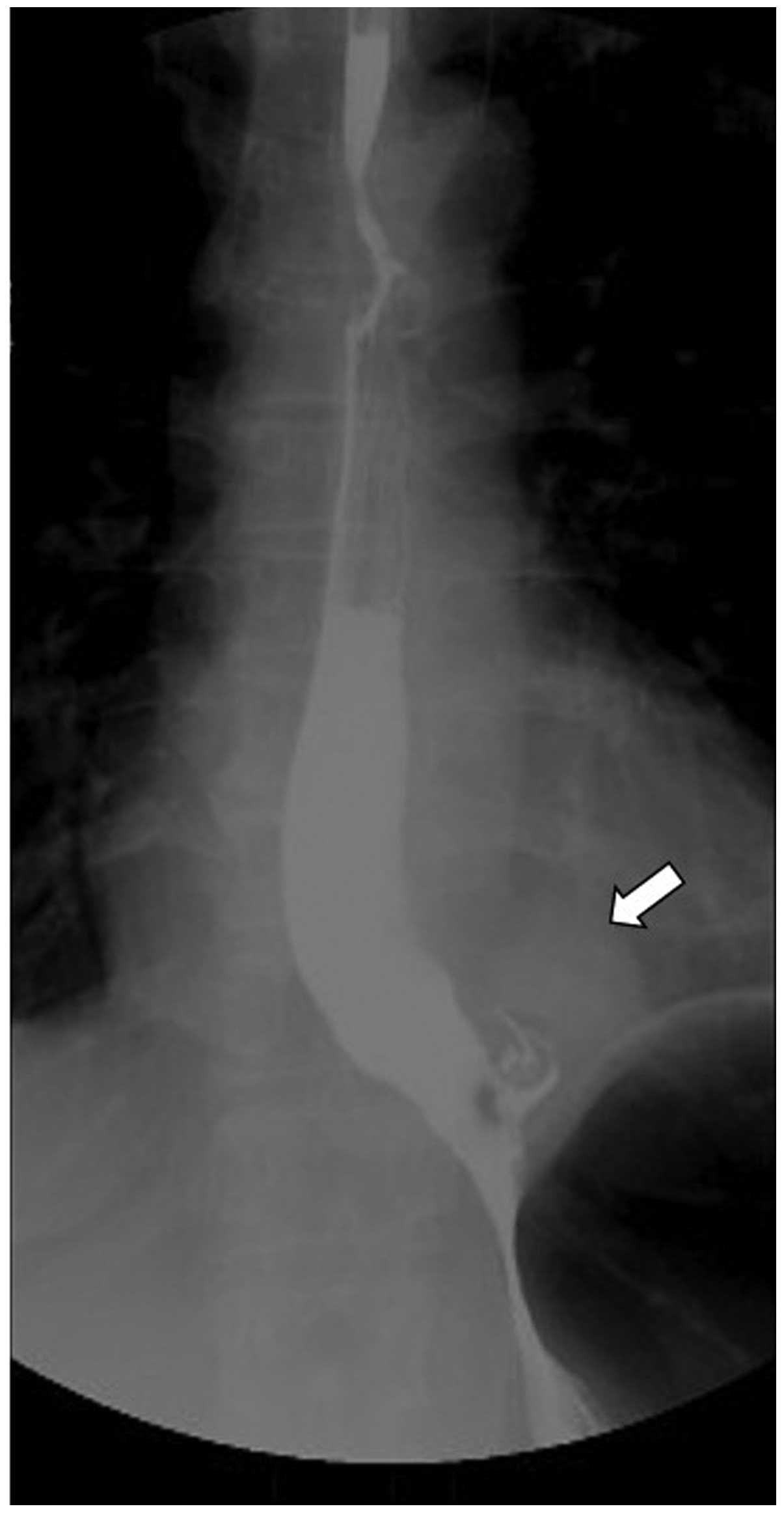
esophagus, without invading the cardia of the stomach (Fig. 2). An upper gastrointestinal tract
radiograph revealed an esophageal submucosal tumor (SMT) at the
distal esophagus (Fig. 3), and
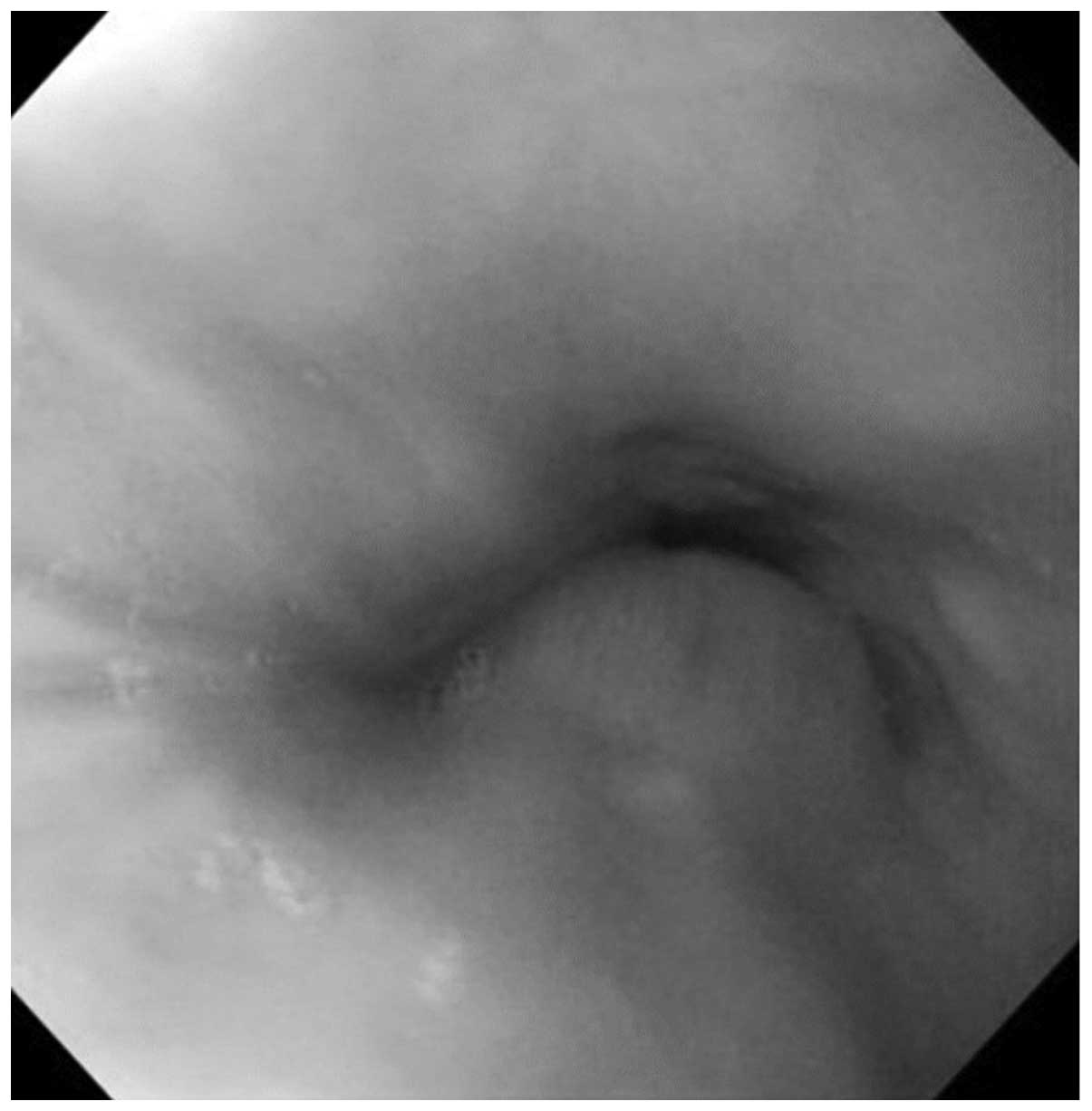
upper gastrointestinal endoscopy (GIF-H290; Olympus Corporation,
Tokyo, Japan) confirmed the diagnosis of an esophageal SMT with a
normal mucosa (Fig. 4).
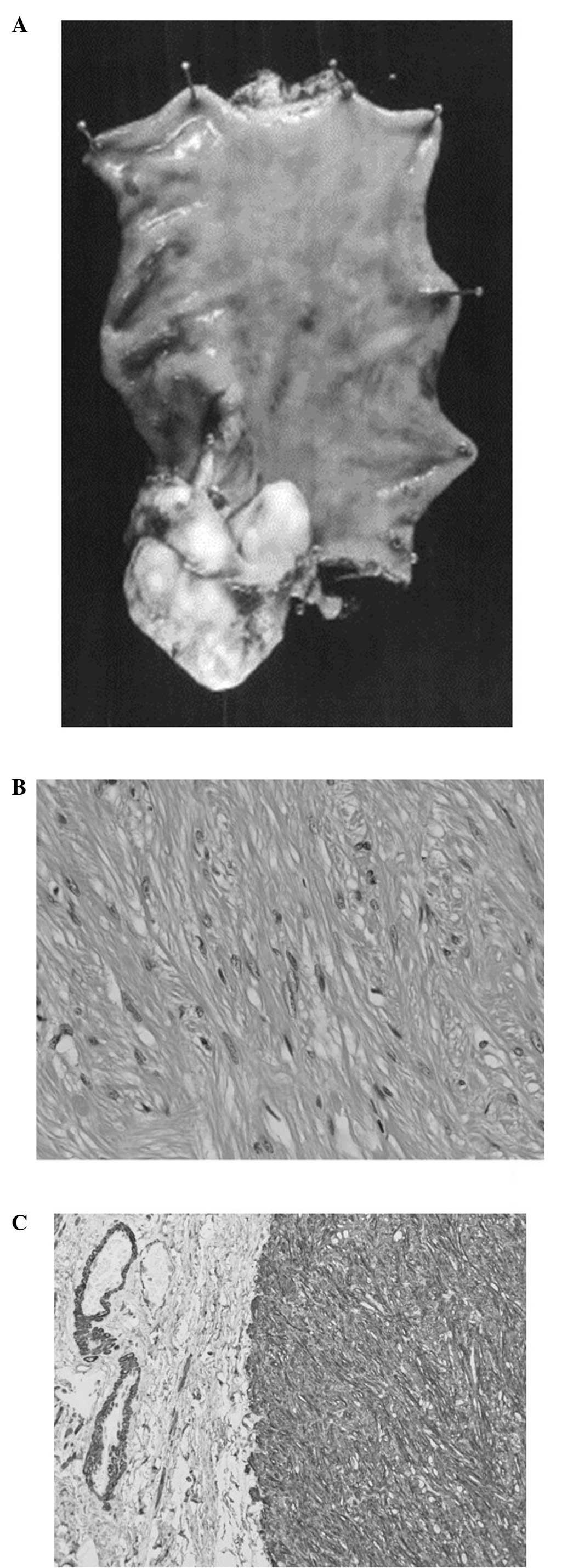
Histopathological examination of the tumor biopsy revealed spindle
cell proliferation; however, mitotic activity or cellular anaplasia
were not detected. Immunohistochemical analysis revealed diffuse
and strong positive staining for α-smooth muscle actin (Dako,
Tokyo, Japan). No enlargement of the adjacent lymph nodes or
evidence of distant metastasis were identified on the chest and
abdominal CT scans. The patient was subjected to a laparoscopic
lower esophagectomy, a proximal gastrectomy and a gastric tube
reconstruction. Macroscopic examination revealed a 50×40×28-mm
mass, while microscopic examination identified submucosal smooth
muscle tissue without mitotic activity or necrosis (Fig. 5). The patient was asymptomatic
during the three-month follow-up period. Written informed patient
consent was obtained from the patient.
Discussion
Esophageal SMTs are occasionally detected
incidentally during the examination of other gastrointestinal
diseases (1–4). In these cases, the majority have been
identified by upper gastrointestinal tract radiography (2) or endoscopy (1,3,4).
Esophageal leiomyomas may appear as a posterior mediastinal mass on
chest radiographs (5–7); thus, are identified as an incidental
radiographic finding (8,9). In the present study, the right lower
lung nodule was initially suspected to be a primary lung cancer
tumor, an arteriovenous malformation or a gastrointestinal stromal
tumor due to the nodule shape and position.
Common symptoms of an esophageal leiomyoma include
dysphagia, epigastric pain and retrosternal pain or burning.
However, the leiomyoma grows slowly and half of the patients do not
present any symptoms unless the tumor is intramural (5,7).
Bleeding is common in patients with gastric leiomyomas, whereas
esophageal leiomyomas do not ulcerate and rarely bleed (7,10).
The patient in the current study did not show any symptoms, such as
dysphagia or epigastric pain.
The diameter of esophageal leiomyomas has been
reported to be <5 cm in 49% of cases, 5–9 cm in 33.7% of cases
and >10 cm in 17.3% of cases (11). Several studies have recommended the
observation of asymptomatic patients with lesions of <5 cm at
the tumor’s largest diameter, as well as when the preoperative
analysis excluded malignancy (11,12).
However, other studies have reported that malignancy is unable to
be completely excluded prior to surgery (5,10).
In the present study, the patient did not present any symptoms or
evidence of malignancy in the specimens biopsied, although sections
of the tumor were >5 cm in diameter. Therefore, a surgical
resection of the tumor was performed.
Community-based lung cancer screening using chest
radiography is well-established in Japan (13–15),
allowing residents aged ≥40 years to undergo an annual chest
radiography. This screening program has been supported by the
Japanese national government under the Health and Medical Services
Law for the Aged since 1987 (16).
Participants who are suspected of having lung cancer following a
chest X-ray or sputum cytology are offered further examinations to
confirm the diagnosis during a secondary evaluation. However, a
number of diseases other than primary lung tumors have been
diagnosed through the mass-screening program, most commonly benign
lung, metastatic lung and mediastinal tumors (17–19).
To the best of our knowledge, the current study
presents the first case of an esophageal leiomyoma detected on a
chest radiograph during a mass-screening program. In conclusion, a
mass lesion adjacent to the gastrointestinal tract that is detected
on a chest radiograph may potentially indicate a rare disease.
Therefore, further investigation with upper gastrointestinal
radiography and gastroendoscopy should be performed.
References
|
1
|
Shim CS, Lee JS, Kim JO, et al: A case of
primary esophageal B-cell lymphoma of MALT type, presenting as a
submucosal tumor. J Korean Med Sci. 18:120–124. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Montesi A, Pesaresi A, Graziani L,
Salmistraro D, Dini L and Bearzi I: Small benign tumors of the
esophagus: radiological diagnosis with double-contrast examination.
Gastrointest Radiol. 8:207–212. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kobayashi N, Kikuchi S, Shimao H, et al:
Benign esophageal schwannoma: report of a case. Surg Today.
30:526–529. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
De Rezende L, Lucendo AJ and
Alvarez-Argüelles H: Granular cell tumors of the esophagus: report
of five cases and review of diagnostic and therapeutic techniques.
Dis Esophagus. 20:436–443. 2007.PubMed/NCBI
|
|
5
|
Aurea P, Grazia M, Petrella F and
Bazzocchi R: Giant leiomyoma of the esophagus. Eur J Cardiothorac
Surg. 22:1008–1010. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Peters JH and DeMeester TR: Esophagus and
diaphragmatic hernia. Schwartz’s Principles of Surgery. Brunicardi
FC, Andersen KD, Billiar RT, Dunn LD, Hunter GC and Pollock RE: 8th
edition. McGraw-Hill; New York, NY: pp. 9062005
|
|
7
|
Jang KM, Lee KS, Lee SJ, et al: The
spectrum of benign esophageal lesions: imaging findings. Korean J
Radiol. 3:199–210. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Miettinen M, Sarlomo-Rikala M, Sobin LH
and Lasota J: Esophageal stromal tumors: a clinicopathologic,
immunohistochemical, and molecular genetic study of 17 cases and
comparison with esophageal leiomyomas and leiomyosarcomas. Am J
Surg Pathol. 24:211–222. 2000. View Article : Google Scholar
|
|
9
|
Miettinen M and Lasota J: Gastrointestinal
stromal tumors - definition, clinical, histological,
immunohistochemical, and molecular genetic features and
differential diagnosis. Virchows Arch. 438:1–12. 2001. View Article : Google Scholar
|
|
10
|
Hatch GF 3rd, Wertheimer-Hatch L, Hatch
KF, et al: Tumors of the esophagus. World J Surg. 24:401–411. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Priego P, Lobo E, Alonso N, Gil Olarte MA,
Pérez de Oteyza J and Fresneda V: Surgical treatment of esophageal
leiomyoma: an analysis of our experience. Rev Esp Enferm Dig.
98:350–358. 2006.(In English and Spanish).
|
|
12
|
Punpale A, Rangole A, Bhambhani N, et al:
Leiomyoma of esophagus. Ann Thorac Cardiovasc Surg. 13:78–81.
2007.
|
|
13
|
Nishii K, Ueoka H, Kiura K, et al: A
case-control study of lung cancer screening in Okayama Prefecture,
Japan. Lung Cancer. 34:325–332. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tsukada H, Kurita Y, Yokoyama A, et al: An
evaluation of screening for lung cancer in Niigata Prefecture,
Japan: a population-based case-control study. Br J Cancer.
85:1326–1331. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kanashiki M, Tomizawa T, Yamaguchi I, et
al: Volume doubling time of lung cancers detected in a chest
radiograph mass screening program: Comparison with CT screening.
Oncol Lett. 4:513–516. 2012.PubMed/NCBI
|
|
16
|
Masuda M and Kojima K: Japanese Social
Security for the Elderly from a Viewpoint of Life Cycles. Review of
Population and Social Policy. 10. National Institute of Population
and Social Security Research; Tokyo: pp. 37–54. 2001
|
|
17
|
Mizutani E, Morita R and Kitamura S:
Arteriovenous hemangioma in the middle mediastinum: report of a
case. Surg Today. 41:846–848. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yamashita R, Kosugi M, Kobayashi C,
Toribatake Y, Kitano Y and Annen Y: A case of dumb-bell-like
neurilemmoma of the posterior mediastinum. Nihon Kyobu Geka Gakkai
Zasshi. 37:2001–2004. 1989.(In Japanese).
|
|
19
|
Dohba S, Kondoh M, Fujita H, et al: A case
of 19th year pulmonary metastasis after radical mastectomy for
breast cancer. Kyobu Geka. 53:1129–1132. 2000.(In Japanese).
|