Introduction
Acute myocardial infarction (AMI) is one of the most
frequently occurring cardiovascular diseases and the leading cause
of morbidity and mortality in the developed as well as the
developing world (1). Over 7.5
million individuals reportedly succumb to AMI annually worldwide
(2), with United States alone
accounting for >600,000 deaths annually (3). Although formerly considered an
illness of predominantly developed countries, myocardial infarction
(MI) is becoming increasingly more common in developing countries;
although its occurrence was reported to be lower compared to that
in Western populations (4), the
prevalence and mortality rates have been increasing rapidly.
Epidemiological statistics in 2003 reported >700,000 new cases
annually in China and this increasing trend has attracted
widespread attention (5).
The research on the pathogenesis, treatment and
prognosis of AMI has progressed significantly over the last decade.
However, the underlying mechanism remains unclear, although the
risk of AMI has been suggested to be associated with exposure to
multiple risk factors (6). A large
international case-control study of risk factors for MI conducted
in 52 countries (the INTERHEART study) reported 9 easily measured
and potentially modifiable risk factors, among which 4 were
associated with lifestyle and accounted for 54.6% of the population
attributable risk. The remaining 5 factors were high blood
pressure, diabetes, abdominal obesity, social psychological factors
and lipid levels (7). A recent
study also demonstrated evidence suggesting that the prognosis of
AMI may be associated with risk factors including myocardial
ischemia, infarction times and locations, demographic data such as
age and gender and complications such as high blood pressure and
diabetes (8).
The effect of these 9 risk factors was suggested to
be consistent across all geographic regions and ethnic groups
worldwide and the management of AMI was considered one of the most
significant advances of contemporary cardiology, with reduced
mortality reported by several registries (9). However, the prevalence of these risk
factors varies among different populations (7,10)
and the availability of data on the risk factors, management and
outcome of AMI in developing countries was limited. The majority of
the registries that documented the use of various medications and
interventional procedures in AMI patients were established in
developed countries and the majority of available data from
developing countries regarding AMI management were derived from
small studies from single centers.
Being the world’s largest developing country, China
reportedly accounts for >700,000 deaths annually (11). With an aging population and a
projected substantial rise in disease rate, the burden of AMI in
China has increased significantly. However, there was no clear
concept of the factors associated with the prognosis of AMI among
Chinese patients and large population-based studies on the
potential risk factors and prognosis of AMI are scarce. The
prevalence and strength of the association of risk factors observed
in other populations may not necessarily apply to China, due to the
genetic susceptibility and environmental factors. In this study,
the potential risk factors and prognosis of AMI were investigated
among a large Chinese population and the correlations of AMI risk
factors with prognosis and hospitalization cost were analyzed.
Patients and methods
Subjects
A total of 627 AMI patients who were admitted to our
hospital between January, 2009 and December, 2012 were recruited in
this study. The inclusion criteria were as follows: i) Patients
presented with clinical symptoms of AMI, including pain radiation,
abdominal pain, chest tightness, chest pain, dizziness and nausea;
ii) dynamic changes in the electrocardiogram (ECG), such as ST
segment elevation and depression, T wave inversion, the presence of
any pathological Q wave and abnormal R wave; iii) increasing
myocardial damage; and iv) all the patients were in the acute phase
of MI.
Study design
This study was approved by the local Ethics Review
Board of our institution and all the patients and their family
members provided written informed consent prior to inclusion.
General information, such as gender, age, complications
(hypotension, high cholesterol and hyperlipidemia), infarct
location, times of hospitalization, percutaneous coronary
intervention (PCI), hospitalization time and cost, disease
diagnosis, treatment mode and prognosis, was collected. The data
were entered into Excel software and a database was set up for
statistical analysis.
Grouping
According to the different classification criteria,
the patients were divided into different subgroups. All the cases
were primarily divided into the death and non-death groups and the
latter was further subdivided into healed, improved, and non-healed
subgroups, according to the prognosis of the patients. Based on the
ECG diagnosis of the infarct location, the patients were grouped
into anterior wall, anteroseptal, inferior wall, posterior wall,
right ventricle, high lateral wall and multiple-wall MI. Moreover,
the patients were further classified according to times of
hospitalization (1, 2, and ≥3), age (≤53, 54–68 and ≥69 years) and
duration of hospitalization (≤6 and >6 days).
Statistical analysis
Statistical analysis was performed using GraphPad
Prism 6.0 software (GraphPad Software, La Jolla, CA, USA). Count
data are presented as % of total number and measurement data are
expressed as mean ± standard deviation (SD). Comparisons between
the groups were performed with the χ2 test. Data of
normal distribution and homogeneity of variance between the two
groups were compared using analysis of variance and independent
samples t-test and the remaining data were analyzed using
non-parametric test. P<0.05 was considered to indicate
statistically significant differences.
Results
Basic patient information
A total of 627 AMI patients, aged 26–90 years (mean
age ± SD, 60.56±11.66 years), including 549 men and 78 women, were
recruited in this study. The patients’ general information was
tabulated and is presented in Table
I. A total of 279 patients (44.50%) had high blood pressure,
146 (23.29%) had a history of diabetes and 27 (4.31%) had
hyperlipidemia. As regards infarct location, 267 patients were
diagnosed with anterior wall AMI, accounting for 42.58% of all AMI
patients, followed by inferior wall AMI (42.11%) and anteroseptal,
posterior wall, multiple-wall, high lateral wall and right
ventricular AMI (9.41, 1.75, 1.75, 1.28 and 1.12%, respectively).
Among all patients, 556 (88.7%) ultimately underwent PCI treatment.
The majority of the patients (566/627) were recorded as being
hospitalized for the first time (90.27%), 42 (6.70%) for the second
time and 19 (3.03%) for the third time or more. The hospitalization
time ranged between 0 and 58 days, with an average of 6.74±5.68
days. The cost of hospitalization ranged from 1,639 up to 299,184
Yuan, with an average cost of 57,594±37,396 Yuan.
 | Table IGeneral information of patients with
acute myocardial infarction (AMI). |
Table I
General information of patients with
acute myocardial infarction (AMI).
| Variables | Patient no.
(n=627) | % |
|---|
| Age (years) |
| Mean ± SD | 60.56±11.66 | |
| Range | 26–90 | |
| Male patients | 549 | 87.56 |
| Infarct location |
| Anterior wall | 267 | 42.58 |
| Inferior wall | 264 | 42.11 |
| Anteroseptal | 59 | 9.41 |
| Posterior wall | 11 | 1.75 |
| Multiple-wall | 11 | 1.75 |
| High lateral
wall | 8 | 1.28 |
| Right ventricle | 7 | 1.12 |
| Times of
hospitalization |
| 1 | 566 | 90.27 |
| 2 | 42 | 6.70 |
| ≥3 | 19 | 3.03 |
| Complications |
| Diabetes
mellitus | 146 | 23.29 |
| High blood
pressure | 279 | 44.50 |
| Hyperlipidemia | 27 | 4.31 |
| Duration of
hospitalization (days) |
| Mean ± SD | 6.74±5.68 | |
| Range | 0–58 | |
| Number of patients
receiving PCI | 556 | 88.7 |
| Hospitalization
costs (Yuan) |
| Mean ± SD | 57,594±37,396 | |
| Range | 1,639–299,184 | |
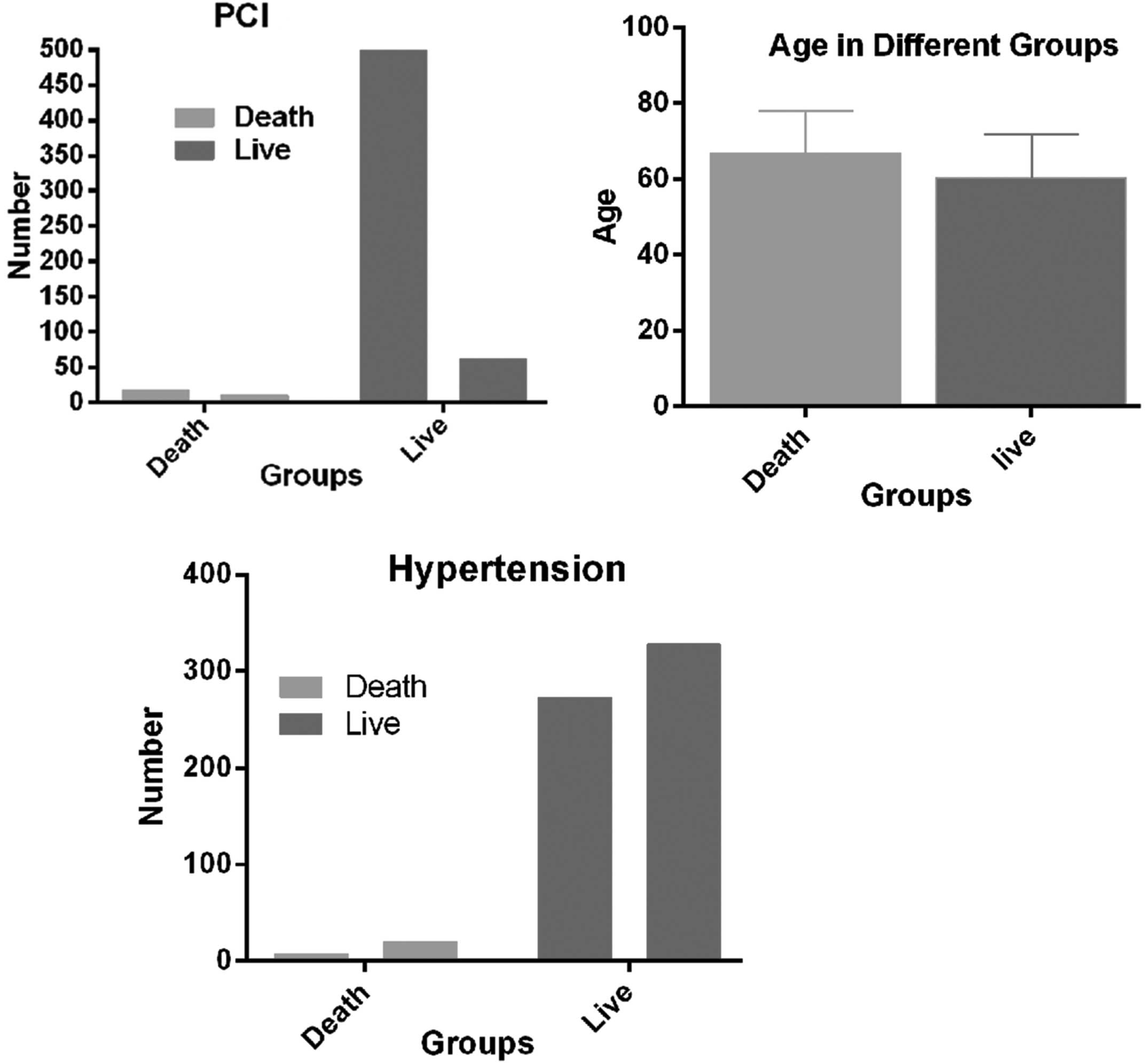
Comparison of relevant factors between
death and non-death groups
As presented in Table
II, 27 patients succumbed during follow-up (aged 39–89 years).
The hospitalization time ranged between 0 and 26 days and the
hospitalization cost was estimated to be between 2,731 and 298,100
Yuan. There were 600 patients in the non-death group, aged 26–90
years, with a hospitalization time of 1–58 days. The
hospitalization cost ranged between 1,639 and 299,184 Yuan. There
were significant age differences between the death and non-death
groups (P=0.0039), with the age of patients in the death group
being significantly higher compared to that of the non-death group.
The final status of the patients was also found to be significantly
correlated with high blood pressure (P=0.047) and PCI treatment
(P<0.001). The proportion of patients suffering from high blood
pressure was significantly lower in the death group compared to
that in non-death group, while the number of patients undergoing
PCI treatment was significantly higher in the non-death group. By
contrast, there were no significant differences in hospitalization
time, hospitalization cost, gender, infarct location, times of
hospitalization, diabetes and hyperlipidemia between the two groups
(P>0.05; Table II and Fig. 1).
 | Table IIComparison of 8 death relevant
factors between the death group and non-death group. |
Table II
Comparison of 8 death relevant
factors between the death group and non-death group.
| Relevant
factors | Non-death group,
no. (%)(n=600) | Death group, no.
(%)(n=27) | P-value |
|---|
| Age (years), mean ±
SD | 60.28±0.47 | 65.89±2.14 | 0.0039a |
| Male patients | 526 | 23 | 0.76 |
| Infarct
location | | 0.14 | |
| Anterior wall | 251 (41.8) | 16 (59.3) | |
| Inferior wall | 256 (42.7) | 8 (29.6) | |
| Anteroseptal | 59 | (9.83) 0 | |
| Posterior
wall | 10 (1.67) | 1 (3.7) | |
| Multiple-wall | 11 (1.83) | 0 | |
| High lateral
wall | 7 (1.17) | 1 (3.7) | |
| Right
ventricle | 6 (1) | 1 (3.7) | |
| Times of
hospitalization | | 0.39 | |
| 1 | 543 (90.5) | 23 (85.2) | |
| 2 | 40 (6.67) | 2 (7.4) | |
| ≥3 | 17 (2.83) | 2 (7.4) | |
| Complications | | 1.00 | |
| Diabetes | 140 (23.3) | 6 (22.2) | |
| High blood
pressurea | 272 (45.3) | 7 (25.9) | 0.047a |
|
Hyperlipidemia | 26 (4.3) | 1 (3.7) | 1.00 |
| Duration of
hospitalization (days), mean ± SD | 6.73±0.23 | 6.78±1.50 | 0.10 |
| Number of patients
receiving PCI | 539 (89.8) | 17 (63.0) | <0.0001a |
| Hospitalization
costs (Yuan), mean ± SD | 57,016±1,435 | 70,442±13,654 | 0.89 |
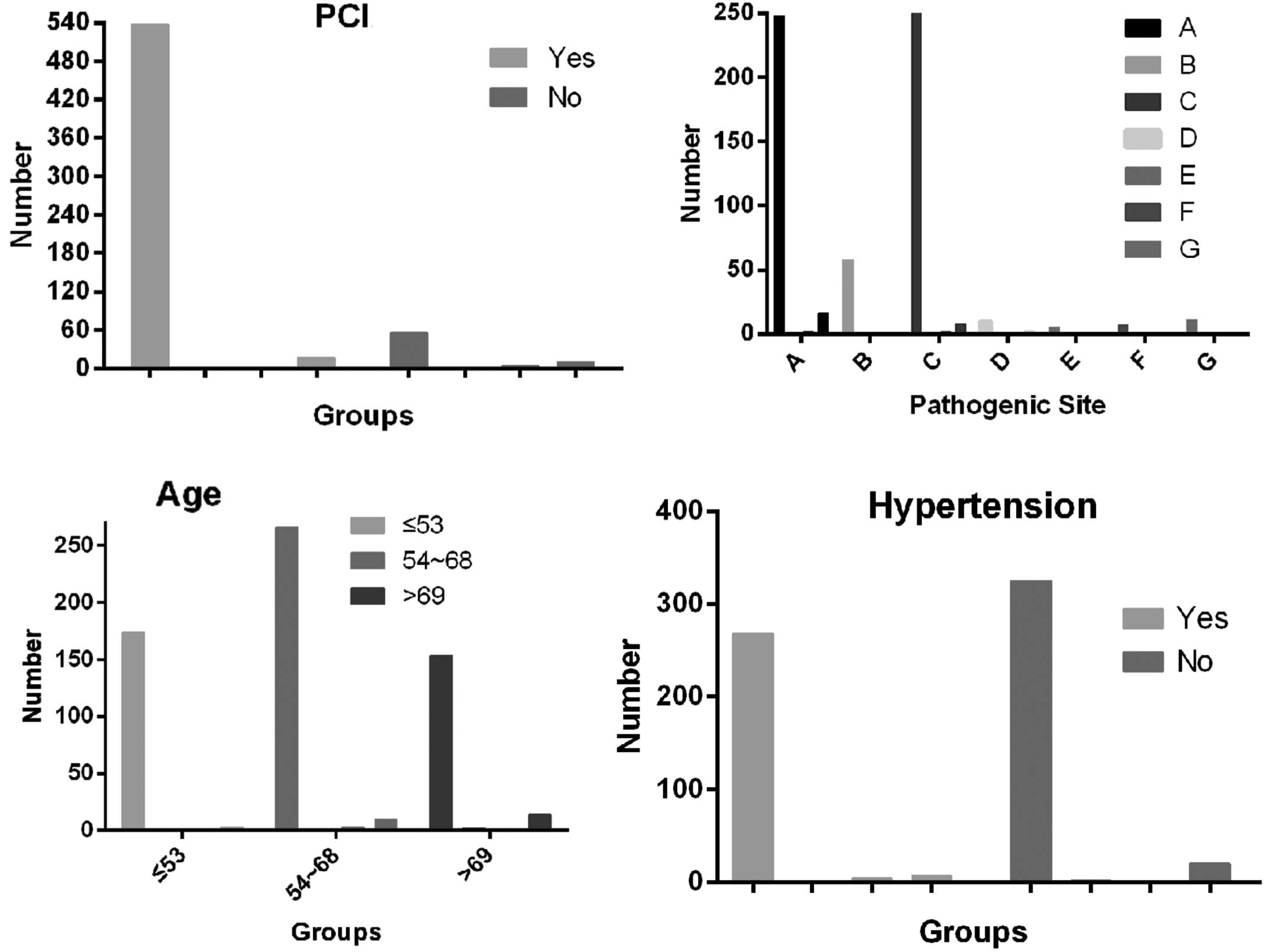
Single-factor analysis of relevant
factors in different prognostic groups
The results of the statistical analysis revealed
that relevant factors, including age (P=0.015), high blood pressure
(P=0.045), infarct location (P<0.0001) and PCI treatment
(P<0.0001), were significantly associated with prognosis, while
gender, hospitalization time, diabetes, hyperlipidemia and times of
hospitalization did not exhibit a strong correlation with prognosis
(P>0.05; Table III and
Fig. 2).
 | Table IIIComparison of 9 relevant factors
between different prognostic groups. |
Table III
Comparison of 9 relevant factors
between different prognostic groups.
| Factors affecting
prognosis | Non-death group
(n=600) | Death group
(n=27) |
|---|
|
|---|
| Healed (n=593) | Improved (n=2) | Not healed
(n=5) |
|---|
| Infarct
locationa |
| Anterior wall | 248/267 | 1/267 | 2/267 | 16/267 |
| Anteroseptal | 58/59 | 0/59 | 1/59 | 0/59 |
| Inferior wall | 254/264 | 0/264 | 2/264 | 8/264 |
| Posterior
wall | 10/11 | 0/11 | 0/11 | 1/11 |
| Right
ventricle | 5/7 | 1/7 | 0/7 | 1/7 |
| High lateral
wall | 7/8 | 0/8 | 0/8 | 1/8 |
| Multiple-wall | 11/11 | 0/11 | 0/11 | 0/11 |
| Gender |
| Male | 521/549 | 2/549 | 3/549 | 23/549 |
| Female | 72/78 | 0/78 | 2/78 | 4/78 |
| Age (years)a |
| ≤53 | 174/178 | 0/178 | 1/178 | 3/178 |
| 54~68 | 266/279 | 0/279 | 3/279 | 10/279 |
| ≥69 | 153/170 | 2/170 | 1/170 | 14/170 |
| Times of
hospitalization |
| 1 | 537/566 | 2/566 | 4/566 | 23/566 |
| 2 | 40/42 | 0/42 | 0/42 | 2/42 |
| ≥3 | 16/19 | 0/19 | 1/19 | 2/19 |
| Duration of
hospitalization (days) |
| ≤6 | 370/392 | 2/392 | 3/392 | 17/392 |
| >6 | 223/233 | 0/233 | 2/233 | 10/233 |
| Diabetes
mellitus |
| Yes | 138/146 | 0/146 | 2/146 | 6/146 |
| No | 455/481 | 2/481 | 3/481 | 21/481 |
| High blood
pressurea |
| Yes | 268/279 | 0/279 | 4/279 | 7/279 |
| No | 325/348 | 2/348 | 1/348 | 20/348 |
| Hyperlipidemia |
| Yes | 26/27 | 0/27 | 0/27 | 1/27 |
| No | 567/600 | 2/600 | 5/600 | 26/600 |
| PCIa |
| Yes | 538/556 | 0/556 | 1/556 | 17/556 |
| No | 55/71 | 2/71 | 4/71 | 10/71 |
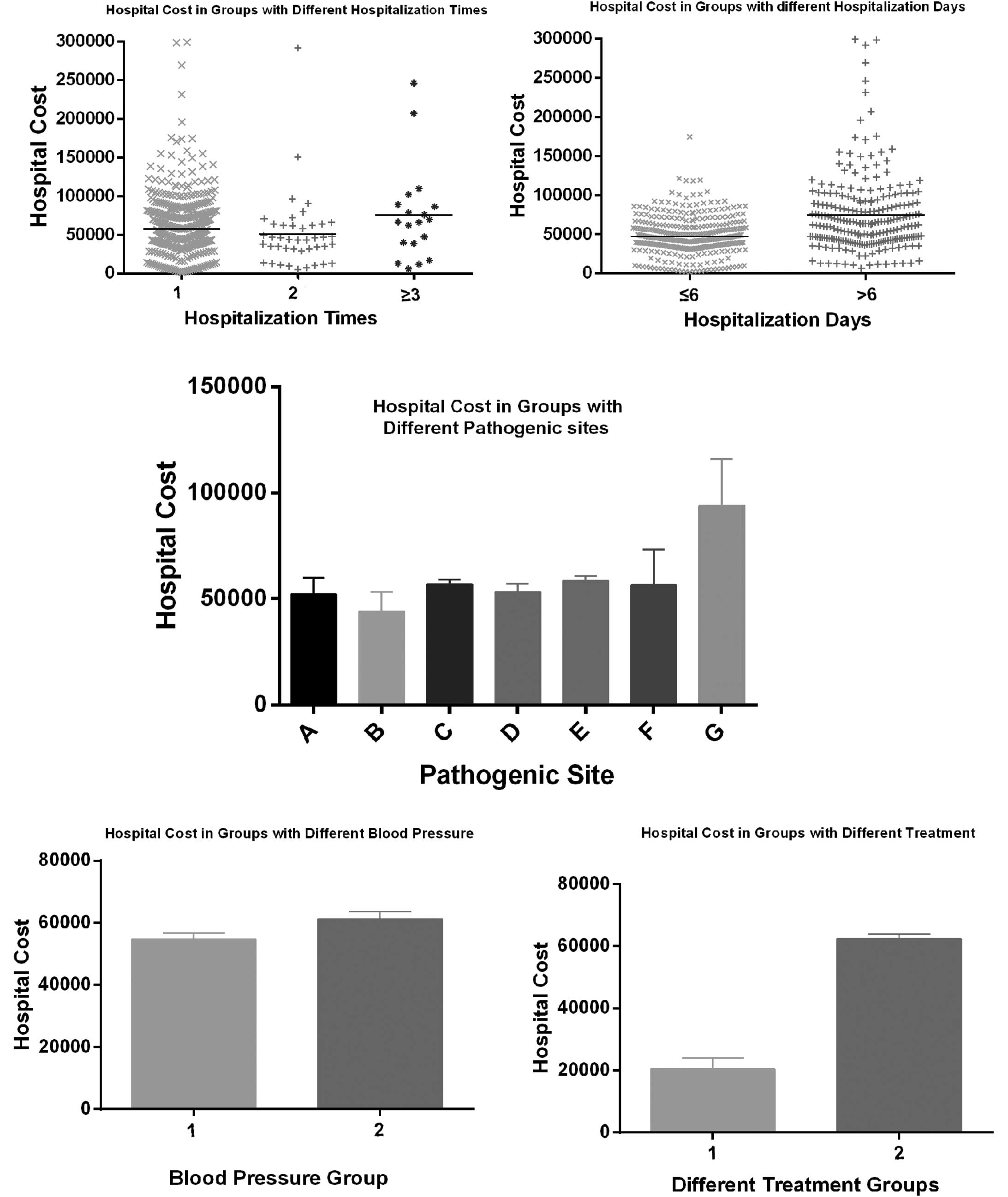
Analysis of factors affecting
hospitalization cost
According to the analysis results mentioned above,
the correlation of hospitalization costs with other relevant
factors was further investigated. The results demonstrated that
times of hospitalization (P=0.045), duration of hospitalization
(P<0.0001), high blood pressure (P=0.029), infarct location
(P=0.046) and PIC (P<0.0001) were significantly associated with
hospitalization cost, while there was no obvious correlation
between hospitalization cost and gender, age, prognosis,
hyperglycemia or hyperlipidemia (Fig.
3).
Discussion
MI has long been recognized as a complication of
grave prognosis. The characteristics of the patients hospitalized
with AMI have reportedly changed over the past 3 decades in several
aspects (8). A large
population-based study on the 9 potential risk factors of AMI and
their correlation with prognosis and hospitalization cost was
systematically performed among the Chinese population. In
comparison to other studies, our study was unique in providing
detailed data regarding potential risk factors of AMI among Chinese
individuals and their correlations with prognosis and
hospitalization cost.
The findings of the present study demonstrated that
age, high blood pressure, infarct location and PCI were the factors
significantly associated with differences in the prognosis of AMI
(P<0.05), while there was no significant correlation between
prognosis and gender, hospitalization cost, times and duration of
hospitalization. Furthermore, the correlation analysis of
hospitalization cost with relevant factors revealed a significant
association of hospitalization cost with high blood pressure,
infarct location, PCI, times and duration of hospitalization among
the study groups, whereas factors including gender, age, prognosis,
hyperglycemia and hyperlipidemia, were not found to be strongly
correlated with hospitalization cost.
Age has long been recognized as one of the
significant factors affecting the prognosis of AMI. It was reported
that >50% AMI cases in the United States were patients aged ≥65
years and 80% of the patients who succumbed to AMI were aged ≥65
years (12). Individuals aged ≥75
years, constituting 6.1% of the US population, accounted for 36% of
AMI cases and 60% of deaths (13).
Although old age per se does not necessarily predispose an
individual to disease, certain factors arising from age-related
physical, cognitive and social circumstances may contribute to a
higher susceptibility. In addition, with increasing age, the
possibility of multivascular disease, high blood pressure and other
complications also increases significantly and exacerbates the poor
prognosis (14,15).
Recent trends revealed a shift in the age
distribution of AMI patients with an increase in AMIs occurring in
patients aged ≥85 years, with the mean age increasing from 78.0 to
80.1 years (16), while a younger
trend regarding the onset of AMI was also observed (17), with the underlying reason remaining
unknown. In this study, the subjects were classified into 4 groups
according to their prognosis and age distribution. Significant
differences were demonstrated regarding age and prognosis, which
was consistent with previous results. However, there was no
significant age difference between the death and non-death groups.
The possible causes of this phenomenon are as follows: i) There was
a limited number of cases in the death group, which may result in
inadequate statistical power; ii) the non-death group was further
subgrouped and the difference between sample levels may fail to
reflect whether they were combined, resulting in mixture samples;
and iii) only representative samples from our hospital were
included, which may result in certain limitations.
A previous study in Framingham over 26 years
demonstrated that the mortality rate from coronary heart disease
among men (60%) was twice that of women (18). Accordingly, the incidence of female
AMI was also lower compared to the incidence in males, but the
mortality rate of AMI was comparatively higher in female patients
(19). Unfortunately, we were
unable to reach the same conclusion, due to the limited number of
female patients recruited.
The main mechanism underlying AMI was hypothesized
to induce acute thrombosis on the basis of coronary atherosclerotic
plaque rupture, with almost complete obstruction of the coronary
artery completely (20). The
location of the infarct was found to be an important prognostic
indicator that warrants consideration in the stratification of risk
and clinical management of MI patients (21). The prognosis of patients with
anterior MI was reported to be significantly worse compared to that
of inferior MI; in addition, anterior wall infarction was suggested
to be associated with more extensive myocardial damage compared to
inferior wall infarction (22).
Our results demonstrated that the proportion of AMIs with infarcts
of inferior and anterior location predominated in both the death
and non-death groups, which was consistent with the results of a
previous study (23). A total of
59.3% of patients who succumbed to the disease had anterior and
29.6% had inferior wall AMI. Patients with anterior AMI exhibited a
significantly higher mortality rate compared to those with inferior
infarction, suggesting that anterior wall infarcts were more
significantly associated with poor prognosis compared to inferior
wall infarcts, corroborating the results reported by Strauss et
al (24). The underlying
reason remains unclear, but it may be associated with segmental
contradiction movement, hemodynamic changes and the malignant
arrhythmia of anterior wall AMI.
PCI is currently a focal point of AMI treatment in
order to restore reperfusion of the infarct artery, rescue the
dying myocardium and preserve cardiac function (16). A previous study demonstrated that
the prognosis of AMI improved when patients underwent PCI, which
reduced the occurrence of coronary artery occlusion and patient
mortality (25). PCI may
effectively prevent and reverse the left ventricular wall muscle
remodeling following MI and improve left ventricular function.
Multiple clinical prospective randomized comparative studies
suggested that, if the patients with acute ST-elevation MI are
transferred to an intervention center for direct PCI within 3
hours, the results may be superior to those of immediate
thrombolysis treatment in the local hospital (26). In the present study, we found that
556 of the 627 AMI patients received PCI treatment during the
hospitalization period, accounting for >88.7% of all
hospitalized patients. PCI treatment reduced the mortality of AMI
from 14.1 to 3.06%, with ~96% of the patients healing from AMI
after receiving PCI. However, distal microvascular thrombotic
obstruction and ventricular remodeling may occur following PCI
(27) and additional treatment,
such as anticoagulants and antiplatelet drugs, should be considered
in combination with clinical emergency PCI. In addition, PCI may
also lead to coronary spasm, perforation and acute occlusion;
therefore, further testing is required to improve patient
performance.
As the traditional atherosclerotic risk factors,
diabetes, hypertension and dyslipidemia were considered to be
independently associated with a higher risk of in-hospital
mortality. It has been reported that crude mortality was higher
among MI patients with diabetes (11.9%) and hypertension (9.8%) and
lowest among patients with dyslipidemia (4.6%). However, these
factors were not as significant in predicting hospital mortality
following MI compared to other clinical factors, in contrast to the
general expectations of the clinicians. The inclusion of
atherosclerotic risk factors in models of hospital mortality did
not improve the predictive ability beyond other major clinical and
sociodemographic characteristics (28).
Hypertension is traditionally considered as an
important contributing factor associated with AMI occurrence and
prognosis (29). The INTERHEART
study indicated that classical risk factors contribute differently
to AMI risk in different populations (7). The prevalence of hypertension in
Chinese AMI patients was reported to be 47%, while a marginally
lower incidence of ~44.5% was detected in the present study. The
results of our study also revealed that the incidence of
hypertension was significantly different between the death and
non-death groups and it was significantly correlated with the
prognosis of AMI.
Diabetes mellitus is a well-established risk factor
for cardiovascular diseases and its presence alone may increase the
risk of cardiovascular events to the same extent as a previous
episode of AMI. The AFIRMAR study reported that diabetes mellitus
was independently associated with AMI in the Brazilian population
(30). According to the INTERHEART
study, a reported history of diabetes was found in 18% of AMI cases
(7) and China alone accounted for
50% of the total number of diabetics worldwide. However, the
prevalence of diabetes among Chinese AMI patients was comparable to
that in Western countries (31).
Diabetes has also been suggested to be one of the negative
predictors of long-term outcome during hospitalization (32). However, our study demonstrated a
similar incidence of diabetes between the death and non-death
groups; in addition, there was no significant correlation between
the occurrence of diabetes and the prognosis of AMI.
Moreover, a literature review revealed that the
prevalence of hypercholesterolemia was variable among patients with
AMI in different regions (33).
Hypercholesterolemia was found to be a significant risk factor for
AMI patients (34), with a direct
association between the severity of hyperglycemia and the scope of
MI and prognosis (35). However, a
previous study on AMI in an Indian population also indicated that
hypercholesterolemia was not a significant risk factor for AMI
(6) and the same result, with no
significant difference in the prognosis of AMI, was obtained by our
study, regardless of whether the hypercholesterolemia was
complicated. Further investigation is required to elucidate the
significance of this finding.
The times and duration of hospitalization were also
hypothesized to reflect the severity of the disease to some extent;
hospitalization time was longer among survivors (7.46±4.01 days)
compared to non-survivors (6.86±3.30) (36). However, no significant correlations
of prognosis with times of hospitalization and duration of hospital
stay were identified.
Our study demonstrated that times and duration of
hospitalization, high blood pressure, infarct location and PIC were
significantly associated with hospitalization cost. As previously
mentioned, the duration of hospital stay reflects the severity of
the disease, while other factors, including high blood pressure,
infarct location and PCI treatment may also be associated with the
severity of AMI, which inevitably affects the cost during the
hospital stay. However, the pursuit of a higher income and overuse
of PCI cannot be excluded.
Non-random samples are prone to bias. The AMI
patients and hospitals enrolled may not be representative of all
AMI patients and hospitals in China. In addition, although
controlling for potential confounding factors, we cannot exclude
the effect of other unmeasured factors, which may have affected
prognosis and hospitalization costs for AMI. Finally, the prognosis
of AMI patients was limited to their hospital stay and long-term
follow-up requires careful assessment.
Our study presented evidence indicating that the
risk factors affecting the prognosis of Chinese patients may differ
from those in other countries. Age, infarct location, high blood
pressure and PCI were significantly correlated with prognosis of
AMI patients, whereas hospitalization cost was affected by high
blood pressure, infarct location, PCI, times and duration of
hospitalization.
Acknowledgements
This study was supported by the Guangdong Province
Science and Technology Program (grant no. 2011B031800008).
References
|
1
|
Murray CJ and Lopez AD: Alternative
projections of mortality and disability by cause 1990–2020: Global
Burden of Disease Study. Lancet. 349:1498–1504. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Yusuf S, Reddy S, Ôunpuu S and Anand S:
Global burden of cardiovascular diseases part I: general
considerations, the epidemiologic transition, risk factors, and
impact of urbanization. Circulation. 104:2746–2753. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sodha NR, Clements RT, Feng J, et al:
Hydrogen sulfide therapy attenuates the inflammatory response in a
porcine model of myocardial ischemia/reperfusion injury. J Thorac
Cardiovasc Surg. 138:977–984. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ueshima H, Sekikawa A, Miura K, et al:
Cardiovascular disease and risk factors in Asia a selected review.
Circulation. 118:2702–2709. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Woo KS and Donnan SP: Epidemiology of
coronary arterial disease in the Chinese. Int J Cardiol. 24:83–93.
1989. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pais P, Pogue J, Gerstein H, et al: Risk
factors for acute myocardial infarction in Indians: a case-control
study. Lancet. 348:358–363. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yusuf S, Hawken S, Ôunpuu S, et al: Effect
of potentially modifiable risk factors associated with myocardial
infarction in 52 countries (the INTERHEART study): case-control
study. Lancet. 364:937–952. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dudas K, Lappas G and Rosengren A:
Long-term prognosis after hospital admission for acute myocardial
infarction from 1987 to 2006. Int J Cardiol. 155:400–405. 2012.
View Article : Google Scholar
|
|
9
|
Teixeira R, Gonçalves L and Gersh B: Acute
myocardial infarction - historical notes. Int J Cardiol.
167:1823–1834. 2013. View Article : Google Scholar
|
|
10
|
Simes RJ, O’Connell RL, Aylward PE, et al;
HERO-2 Investigators. Unexplained international differences in
clinical outcomes after acute myocardial infarction and
fibrinolytic therapy: lessons from the Hirulog and Early
Reperfusion or Occlusion (HERO)-2 trial. Am Heart J. 159:988–997.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
He J, Gu D, Wu X, et al: Major causes of
death among men and women in China. N Engl J Med. 353:1124–1134.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Miller TD, Christian TF, Hodge DO,
Hopfenspirger MR, Gersh BJ and Gibbons RJ: Comparison of acute
myocardial infarct size to two-year mortality in patients <65 to
those >or =65 years of age. Am J Cardiol. 84:1170–1175. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Rich MW: Treatment of acute myocardial
infarction. Am J Geriatr Cardiol. 10:328–336. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Singh M, Mathew V, Garratt KN, et al:
Effect of age on the outcome of angioplasty for acute myocardial
infarction among patients treated at the Mayo clinic. Am J Med.
108:187–192. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ruiz-Bailén M, Aguayo de Hoyos E,
Ramos-Cuadra JÁ, et al: Influence of age on clinical course,
management and mortality of acute myocardial infarction in the
Spanish population. Int J Cardiol. 85:285–296. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Vaughan Sarrazin MS, Bayman L and Cram P:
Trends during 1993–2004 in the availability and use of
revascularization after acute myocardial infarction in markets
affected by certificate of need regulations. Med Care Res Rev.
67:213–231. 2010. View Article : Google Scholar
|
|
17
|
Grahame TJ and Schlesinger RB:
Cardiovascular health and particulate vehicular emissions: a
critical evaluation of the evidence. Air Qual Atmos Health. 3:3–27.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lerner DJ and Kannel WB: Patterns of
coronary heart disease morbidity and mortality in the sexes: a
26-year follow-up of the Framingham population. Am Heart J.
111:383–390. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Griffith D, Hamilton K, Norrie J and Isles
C: Early and late mortality after myocardial infarction in men and
women: prospective observational study. Heart. 91:305–307. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Şatıroğlu O, Vural M, Uyar I and Bostan M:
Acute anterior myocardial infarction in a young male patient
homozygous for the factor V Leiden mutation. Turk Kardiyol Dern
Ars. 38:194–197. 2010.PubMed/NCBI
|
|
21
|
Hands ME, Lloyd BL, Robinson JS, de Klerk
N and Thompson PL: Prognostic significance of electrocardiographic
site of infarction after correction for enzymatic size of
infarction. Circulation. 73:885–891. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Thanavaro S, Kleiger R, Province M, et al:
Effect of infarct location on the in-hospital prognosis of patients
with first transmural myocardial infarction. Circulation.
66:742–747. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Khatri D, Islam N and Ali A: Association
between neutrophilic leucocytosis and congestive heart failure
after acute myocardial infarction. MJSBH. 9:17–24. 2010.
|
|
24
|
Strauss HD, Sobel B and Roberts R: The
influence of occult right ventricular infarction on enzymatically
estimated infarct size, hemodynamics and prognosis. Circulation.
62:503–508. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Dalby M, Bouzamondo A, Lechat P and
Montalescot G: Transfer for primary angioplasty versus immediate
thrombolysis in acute myocardial infarction a meta-analysis.
Circulation. 108:1809–1814. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Van Bavel H, Brenninkmeijer V, Van Ekelen
W, et al: Regional implementation of the NWC guideline on
ST-elevation myocardial infarction. Nethe Heart J. 13:401–407.
2005.
|
|
27
|
Bolognese L, Carrabba N, Parodi G, et al:
Impact of microvascular dysfunction on left ventricular remodeling
and long-term clinical outcome after primary coronary angioplasty
for acute myocardial infarction. Circulation. 109:1121–1126. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Canto JG, Kiefe CI, Rogers WJ, et al:
Atherosclerotic risk factors and their association with hospital
mortality among patients with first myocardial infarction (from the
National Registry of Myocardial Infarction). Am J Cardiol.
110:1256–1261. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Bedimo RJ, Westfall AO, Drechsler H,
Vidiella G and Tebas P: Abacavir use and risk of acute myocardial
infarction and cerebrovascular events in the highly active
antiretroviral therapy era. Clin Infect Dis. 53:84–91. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Piegas LS, Avezum Á, Pereira JC, et al:
Risk factors for myocardial infarction in Brazil. Am Heart J.
146:331–338. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Fox KA, Goodman SG, Klein W, et al:
Management of acute coronary syndromes. Variations in practice and
outcome; findings from the global registry of acute coronary events
(GRACE). Eur Heart J. 23:1177–1189. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kuch B, Wende R, Barac M, et al: Prognosis
and outcomes of elderly (75–84 years) patients with acute
myocardial infarction 1–2 years after the event-AMI-elderly study
of the MONICA/KORA Myocardial Infarction Registry. Int J Cardiol.
149:205–210. 2011. View Article : Google Scholar
|
|
33
|
Abdallah MH, Arnaout S, Karrowni W and
Dakik HA: The management of acute myocardial infarction in
developing countries. Int J Cardiol. 111:189–194. 2006. View Article : Google Scholar
|
|
34
|
Leor J, Goldbourt U, Reicher-Reiss H,
Kaplinsky E and Behar S: Cardiogenic shock complicating acute
myocardial infarction in patients without heart failure on
admission: incidence, risk factors, and outcome. Am J Med.
94:265–273. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Deepa M, Pasupathi P, Sankar KV, Rani P
and Kumar SS: Free radicals and antioxidant status in acute
myocardial infarction patients with and without diabetes mellitus.
Bangladesh Med Res Counc Bull. 35:95–100. 2010.PubMed/NCBI
|
|
36
|
Satar S, Seydaoglu G, Avci A, Sebe A,
Karcioglu O and Topal M: Prognostic value of thyroid hormone levels
in acute myocardial infarction: just an epiphenomenon? Am Heart
Hosp J. 3:227–233. 2005. View Article : Google Scholar : PubMed/NCBI
|