Introduction
Cholelithiasis is a global disease. According to a
previous study (1), China has a
large population of patients with cholelithiasis, including those
who have been diagnosed and those to whom the diagnosis is unknown.
A large proportion of patients with typical symptoms require a
laparoscopic cholecystectomy (LC), which has been regarded as the
‘gold standard’ approach for several years; however, the existence
of postcholecystectomy syndromes (2,3) such
as chronic abdominal discomfort, alkaline reflux gastritis,
dyspepsia and steatorrhea, has focused attention on gallbladder
preservation.
Conventional open gallbladder-preserving surgery may
remove the calculus from the gallbladder but a long incision is
necessary and the absence of a clear macroscopic view may lead to a
high incidence of residual stone (4). Laparoscopic gallbladder-preserving
surgery (L-GPS), however, is less invasive, and endoscopic surgery
makes it possible to observe the inner surface of the gallbladder,
which leads to a satisfying cosmetic result and may assist with
further exploration and the removal of the existing calculus.
Materials and methods
Patients
A total of 517 consecutive patients (402 female and
115 male), aged 21–67 years (average, 36 years), who were diagnosed
with cholelithiasis or cholelithiasis with polypus, underwent L-GPS
in the Second Affiliated Hospital of Soochow University (Suzhou,
China) between April 2009 and March 2014. A total of 143 patients
underwent totally laparoscopic GPS (TL-GPS) and 365 patients
received laparoscopy-assisted GPS (LA-GPS), with nine conversions
to LC. One hundred and fifty-six patients had suffered from acute
episodes of biliary colic at least once and 361 patients were
asymptomatic or had non-specific upper abdominal discomfort.
Sixty-eight patients had between one and three concurrent polypi.
For all patients, a bland diet was demanded and a series of
preoperative preparations, such as any necessary application of
antibiotics or cholaneresis treatments, were adopted. Until
clinical symptoms were apparently palliated, an ultrasonic
examination was required for disease assessment. The present study
was approved by the Ethics Committee of The Second Affiliated
Hospital of Soochow University and all procedures were carried out
in accordance with the Declaration of Helsinki. Informed, written
consent was obtained from all patients (or patients’ families)
prior to their inclusion in the study.
Surgical equipment
Major equipment used included the
mini-laparoscope-camera system (Karl Storz Endoscopy-America, Inc.,
El Segundo, CA, USA), an inflexible cholecystoscope (CHiAO,
Guangzhou, China) and a soft choledochoscope (Olympus, Tokyo,
Japan). The supporting equipment (CHiAO) included a stone basket,
biopsy forceps, electrocoagulation bar and a suction trunk.
Surgical procedure
Patients underwent surgery under general anesthesia
in the supine position, hands by the side. A 6-mm sub-umbilical
incision was made, through which a pneumoperitoneum was created
with simultaneous CO2 insufflation (12–14 mmHg). A
trocar was then implanted and the mini-laparoscope was inserted to
explore the gallbladder and extrahepatic bile duct.
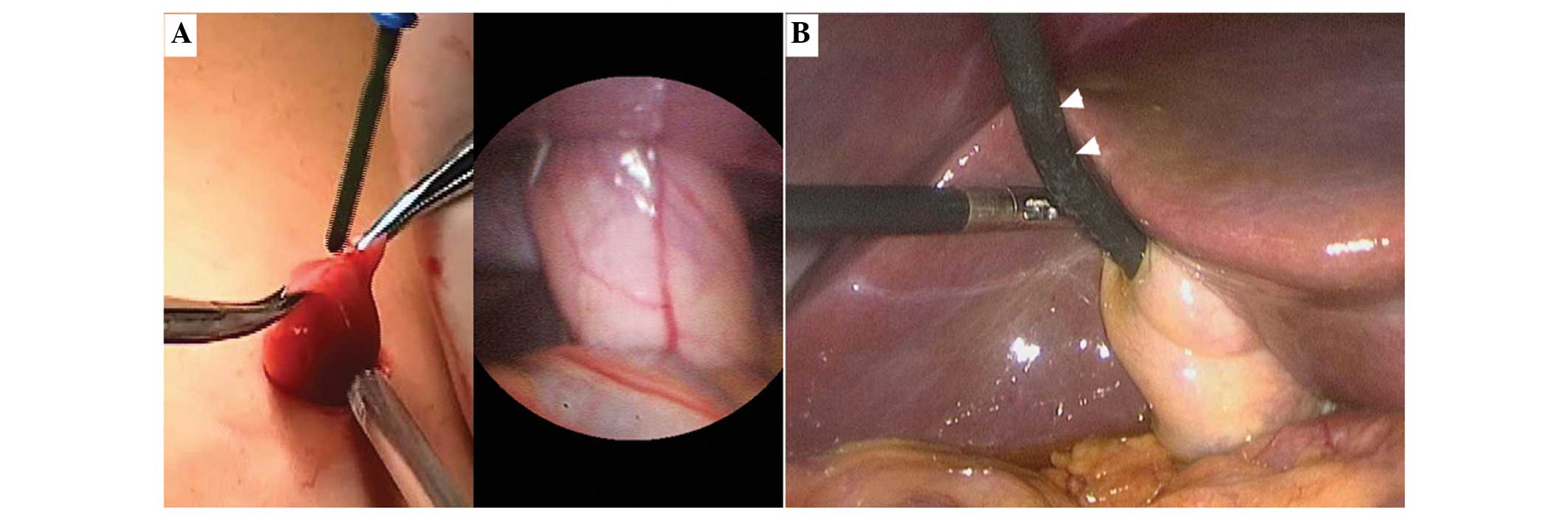
For LA-GPS, a 2.0-cm incision near to the fundus of
the gallbladder and below the right costal margin was made as
previously described (5). An
atraumatic grasper was used to pull the gallbladder out of the
abdominal wall through the incision (Fig. 1A). At the same time, the
sub-umbilical trocar was removed and the pneumoperitoneum was
released. For TL-GPS, a four-port method was used similar to LC and
the soft choledochoscope was used instead of the inflexible
cholecystoscope (Fig. 1B). A
1.0-cm incision was made on the parietal wall of the gallbladder
fundus, which could be adjusted according to the size of the
calculus. The bile was suctioned and endoscopes were inserted into
the gallbladder for further exploration with a perfusion pressure
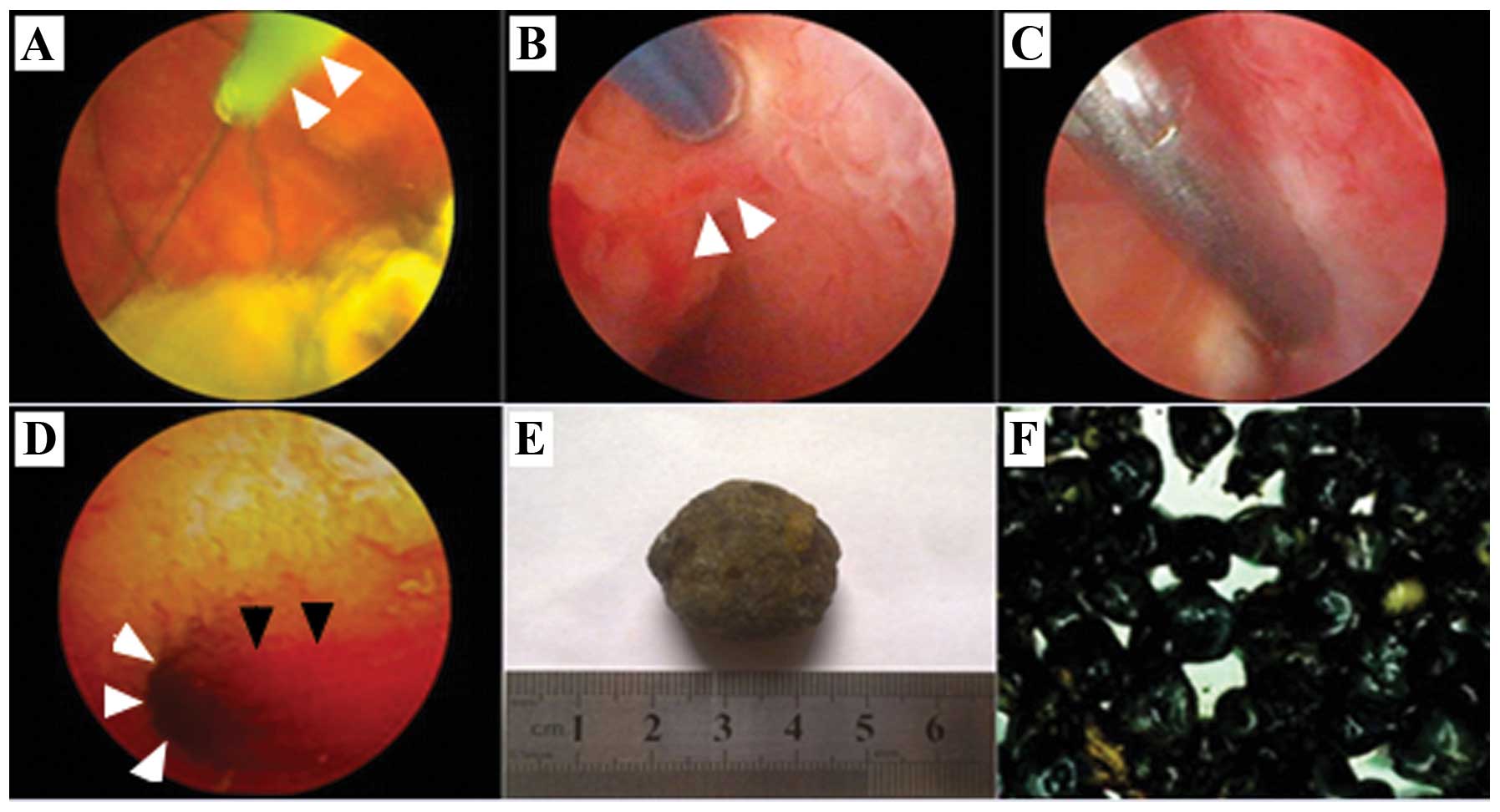
of 60 cm H2O. Calculi that were ≥0.5 cm in diameter were
removed using the basket (Fig.
2A). If the calculi were <0.5 cm, the suction trunk was used
to drain them out. The biopsy forceps were used for the removal of
any polypi <0.3 cm in diameter, whereas pre-electric coagulation
on the polypus pedicle was necessary when the polypus appeared to
be ≥0.3 cm (Fig. 2B–C). Polypus
samples were taken in slices for rapid intraoperative pathological
diagnosis to exclude the existence of gallbladder carcinoma.
Following calculus removal, further exploration was necessary until
spurting bile from the opening of the cystic duct (Fig. 2D) could be observed.
Results
The procedures were performed successfully by one
medical team, including nine cases of conversion into LC. The mean
operating time ranged from 38 to 125 min (mean time, 72 min). No
bile duct injuries occurred intra-operatively and no bile leakage
or intra-abdominal infection was observed postoperatively. Two
patients were shown to have residual sedimental stone through
ultrasonic examination. Three cases of incisional infection were
noted in the patients undergoing LA-GPS. Typical types of calculi
and the use of surgical equipment are shown in Fig. 2.
The follow-up time ranged from 3 to 54 months,
during which time six recurrences were observed in two years
postoperatively and four patients received LC. In the nine
conversion cases, one subcostal incisional hernia was seen
exhibiting a localized bulge with a diameter of 4.0 cm and two
cases with a polypus in a borderline or malignant manner were
followed up postoperatively without tumor recurrence at 24 and 36
months.
Discussion
Based on an in-depth knowledge of gallbladder
function (6,7), it is suggested that GPS could provide
a favorable treatment option for cholelithiasis. As
laparoendoscopic surgery has developed, L-GPS combined with biliary
endoscopy has been proposed by several experts in China (8). Despite remaining controversial, L-GPS
warrants a trial for the following reasons: i) Without L-GPS, LC is
likely to be required due to the pathology and injury to
gallbladder function; thus, earlier medical intervention is likely
to avoid an acute attack and cholecystectomy; ii) earlier GPS could
remove all calculi, preserve the function of the gallbladder and
decrease the higher risk of cholangiolithiasis and colon cancer
following LC; and iii) in a number of European countries and China,
there is a high proportion of cholesterol calculus cases due to a
high-fat diet with limited exercise; these cases could be cured
through an endoscopic approach, and the recurrence rate of such
cholelithiasis could be reduced through modification of diet and
living habits.
For patients who are to be offered GPS, indication
judgments are of vital importance prior to surgery as there is
still no criterion of absolute indications. Satisfactory
gallbladder function of patients with cholelithiasis is essential
since the preservation of a nonfunctional gallbladder is unhelpful
and should be considered as a contraindication. An ultrasonic
examination and ‘fat meal test’ (9) can assist with function evaluation.
Patients with symptomatic cholelithiasis (gallstones combined with
polypus) are strongly recommended for GPS, as are patients with a
particular desire for the procedure; however, acute cholecystitis,
histological carcinoma or cryptogenetic obstructive jaundice are
incompatible and should be excluded from GPS indications (9,10).
In the present study, 156 patients had suffered from acute episodes
of biliary colic at least once and 68 patients had concurrent
polypus. A total of 201 patients with non-specific upper abdominal
discomfort and 153 patients who were asymptomatic were also
suggested for GPS to prevent an acute episode or chronic injury to
gallbladder function.
With regard to surgical approaches, LA-GPS and
TL-GPS are both technically feasible. Even with extended
exploration, no bile duct injury occurred during the surgeries in
the present study. LA-GPS allows the gallbladder to be pulled out
of the abdominal wall through a 2.0-cm subcostal incision (5); however, in the present study the
procedure failed in eight patients, due to a probable carcinoma,
and manipulation was confined to removing the calculus completely.
In addition, TL-GPS was suspended for one patient due to an
atrophic and nonfunctional gallbladder full of white bile. For
these nine patients LC was then performed. A high preservation rate
of 98.3% was obtained as a result of the strict indication checks;
however, three cases of subcostal incisional infection occurred
subsequent to LA-GPS, which were believed to be caused by spilt
inflammatory bile. Following controlled antibiotics use and
periodic dressing changes the incision healed well. One of the
conversion cases, a male of morbid obesity, was noted to have an
incisional hernia three months after the surgery: A longer
subcostal incision was made because of the difficulties in
gallbladder stretching and calculus removal prior to conversion
into LC; in addition, intra-abdominal hypertension during LC may
have led to muscle-slotting injuries that caused abdominal
weakness.
These cases demonstrated the advantages of TL-GPS as
it is not necessary to make a larger incision than the calculus
size and the shorter contact period of spilt bile with the incision
reduces the risk of incisional infection. Furthermore, in TL-GPS a
titanium clamp can be used to temporarily obstruct the bile flow at
the cystic duct to prevent calculus migration to the extrahepatic
bile ducts and incarceration at the neck of the gallbladder or the
bile duct opening. When complicated with extrahepatic bile duct
calculus, the simultaneous laparoscopic common bile duct
exploration can be performed, combined with
fibercholedochoscope.
Calculus residue is considered the primary cause of
cholelithiasis recurrence (11);
thus, a follow-up was carried out for the observation of
therapeutic effectiveness. In 517 patients, all macroscopic calculi
and mucosal lesions were removed. Only two patients were shown to
have sedimental residue on the third postoperative day under
ultrasonic examination, without any recurrence in three months
postoperatively. During long-term follow-up, six patients had a
recurrence, with two cases of a single stone and four cases of
several stones (recurrence rate, 1.2%). Three of the patients
showed symptoms of cholecystitis; LC was performed on four
patients. Application of the endoscope can avoid the limitations of
one surgeon’s subjective perception, which may lead to the ignoring
of tiny calculi. A magnified visual field and guidance on the
screen can provide precise information on calculus size, number,
location, appearance and characteristics, which are of great
significance. Pressure homeostasis of cholecystoscopy and the use
of a temporary obstruction of the cystic duct under the laparoscope
may also avoid calculus migration and reduce the incidence of
residues remaining. Combined with regular oral medication, such as
ursodeoxycholic acid, following surgery, L-GPS can potentially cure
cholelithiasis, with minor residue and recurrence rates.
In conclusion, the adoption of GPS reflects the
important application of minimally invasive endoscopic surgery in
treating biliary diseases. GPS provides a complementary approach to
cure cholelithiasis. L-GPS is effective and TL-GPS is feasible for
cholelithiasis and is particularly favorable in the prevention of
incisional complications.
Acknowledgements
The authors would like to acknowledge support from
the Operating Room of the Second Affiliated Hospital of Soochow
University. The authors also acknowledge help from Dr Jie Chen and
Dr Ming Li for their support in sample collection and
photography.
References
|
1
|
Huang ZQ: Cholelithiasis. Zhong Guo Yi
Kan. 46:3–8. 2011.(In Chinese).
|
|
2
|
Lum YW, House MG, Hayanga AJ and
Schweitzer M: Postcholecystectomy syndrome in the laparoscopic era.
J Laparoendosc Adv Surg Tech A. 16:482–485. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Troppoli DV and Cella LJ Jr: The
postcholecystectomy syndrome. Ann Surg. 137:250–254. 1953.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yoon YS, Han HS, Shin SH, Cho JY, Min SK
and Lee HK: Laparoscopic treatment for intrahepatic duct stones in
the era of laparoscopy: laparoscopic intrahepatic duct exploration
and laparoscopic hepatectomy. Ann Surg. 249:286–291. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wei S: The clinical application of the
hard gallbladder endoscope combined with soft choledochoscope in
the surgery of laparoscopic microscopic trauma for the removal of
calculi and preservation of gallbladder. J Laparoendosc Adv Surg
Tech A. 23:106–108. 2013. View Article : Google Scholar
|
|
6
|
Stathopoulos P, Zundt B, Spelsberg FW,
Kolligs L, Diebold J, Goke B and Jungst D: Relation of gallbladder
function and Helicobacter pylori infection to gastric mucosa
inflammation in patients with symptomatic cholecystolithiasis.
Digestion. 73:69–74. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Qiao T, Zhang BS and Chen XR: Physiology
of gallbladder and biliary tract. The Exploration And Practice Of
Gallbladder-Preservation Cholelithotomy/Polypectomy With Chiao
Cholecystoscope Military. Medical Science Press; Beijing: pp.
24–36. 2012
|
|
8
|
Liu JS, Li JZ, Zhao QK, et al: The
analysis of follow-up results of 612 cases of choleecystolithiasis
treated with the minimal invasive operation with gallbladder
preserved via choledochoscopy. Zhonghua Wai Ke Za Zhi. 47:279–281.
2009.(In Chinese). PubMed/NCBI
|
|
9
|
Qiao T, Zhang BS and Chen XR:
Gallbladder-retention cholelithotomy/polypectomy by CHiAO
gallbladder endoscopy. The Exploration And Practice Of
Gallbladder-Preservation Cholelithotomy/Polypectomy With Chiao
Cholecystoscope Military. Medical Science Press; Beijing: pp.
145–177. 2012
|
|
10
|
Qiao T, Zhang BS, Feng YY, Wang XQ, Wang
XF and Huang YM: Appilition of mini compact nephroscope in
ehdecystolithotomy (eholecystopolyptectomy) with gallbladder
preserved. Zhong Guo Nei Jing Za Zhi. 13:1302–1304. 2007.(In
Chinese).
|
|
11
|
Shen L, Liu Y and Wen H: The exploration
of the value of minimally invasive surgery for preservation of
gallbladder with gallbladder wall calculus. Zhong Guo Nei Jing Za
Zhi. 15:572–575. 2009.(In Chinese).
|