Introduction
Ischemic heart disease is one of the most common
causes of mortality in the world (1). Following acute coronary occlusion
with the threat of myocardial infarction, the current cardiological
protocol for acute myocardial infarction is rapid reperfusion.
Although reperfusion is required to salvage ischemic tissue, it is
associated with cellular damage due to the activation of
deleterious signaling cascades (2). A number of studies have shown that
ischemic preconditioning is an innate protective strategy that
markedly reduces ischemia-reperfusion (I/R) injury (3–5).
This, however, is not acceptable as a clinical tool due to
practical difficulties associated with the local induction of
cardiac ischemia, ethical reasons and the fact that the index
ischemic episode is often unpredictable. Therefore, it is necessary
to search for a novel approach, one that is more suitable for the
clinical scenario.
Pharmacological preconditioning can simulate
ischemic preconditioning and markedly reduce injury from I/R.
Furthermore, this method is associated with an easy execution. To
date, numerous drugs that can prevent the myocardium from I/R
injury (6–8) are available.
Dang-gui-si-ni-tang (DGSN) decoction is a classical
formula in Traditional Chinese Medicine that originated from a
medical textbook known as the ‘Treatise on Cold-Induced Febrile
Diseases’, which dates back to 200 C.E. DGSN is treatment for
coronary heart disease. Studies have indicated that glycyrrhizic,
ferulic and cinnamic acids are the active components in the DGSN
decoction (9–11). In addition, the majority of these
studies have reported that glycyrrhizic, cinnamic and ferulic acids
have a protective effect against I/R injury. The protective
mechanism of glycyrrhizic acid on I/R injury was found to be
associated with its antioxidant (12–14),
anti-inflammatory (15) and
anti-apoptosis effects (16), as
well as its inhibition of lipid peroxide (17). Cinnamic acid exerts cytoprotection
by acting as an antioxidant and anti-inflammatory agent (18–20).
Ferulic acid can also inhibit oxidative stress, inflammation
(21) and cell apoptosis (22) and modulate mitochondrial function
(23). These mechanisms are
associated with the alleviation of I/R injury. Considering that
glycyrrhizic, cinnamic and ferulic acids are major components of
the DGSN decoction, which is used to treat coronary heart diseases
(9–11), we hypothesized that different
combinations of the active ingredients in the DGSN decoction may
also have a similar therapeutic effect.
The aims of this study were fourfold. Firstly, we
aimed to verify whether glycyrrhizic, cinnamic and ferulic acids
could be absorbed into the serum of rats following oral
administration of the DGSN decoction. We then aimed to investigate
the effects of pretreament with glycyrrhizic, cinnamic and ferulic
acids and peoniflorin on superoxide dismutase (SOD) activity and
malondialdehyde (MDA) levels in the myocardium of a rat model of
I/R injury, and to utilize an L16 (44) orthogonal
experiment to find the optimal active combination. Thirdly, we
aimed to investigate the protective effects of the optimal active
combination pretreatment against myocardial I/R injury in rats,
and, finally, to investigate whether the protective effects were
associated with tumor necrosis factor-α (TNFα), interleukin
(IL)-1β, IL-6 and the nuclear factor-κB (NF-κB)p65 and peroxisome
proliferator-activated α (PPARα) signaling pathways.
Materials and methods
Materials
Male Sprague Dawley (SD) rats weighing 280–400 g
were purchased from the Guangdong Experimental Animal Center
(License no. SCXK 2008-0002; Guangzhou, China). The animals were
maintained in individual cages at room temperature under
light-controlled conditions. The rats were provided with food and
water ad libitum. All animal procedures were in accordance
with the Regulations of Experimental Animal Administration issued
by the State Committee of Science and Technology of the People’s
Republic of China on November 14, 1988. Glycyrrhizic acid (purity
>98%), ferulic acid (purity >99%), peoniflorin (purity
>98%) and cinnamic acid (purity >99%) were purchased from
Nanjing Zelang Medical Technology Co., Ltd. (Nanjing, China). The
following primary antibodies, which were obtained from Santa Cruz
Biotechnology, Inc. (Santa Cruz, CA, USA) unless stated, were used:
Anti-phosphorylated (phospho)-Akt1/2 [serine (Ser)473] (cat. no.
9271; Cell Signaling Technology, Inc. Danvers, MA, USA),
anti-inhibitory(I)-κBα (cat. no. SC-101712), anti-phospho-I-κBα
(Ser32/36) (cat. no. SC-101713), anti-NF-κBp65 (cat. no. SC-7151),
anti-GAPDH (cat. no. SC-25778) and anti-PPARα (cat. no. SC-9000).
Horseradish peroxidase-conjugated goat anti-rabbit immunoglobulin G
(IgG; Heavy and Light chain) was purchased from Beijing
Biosynthesis Biotechnology Co., Ltd. (Beijing, China). SOD, MDA,
TNFα ELISA, IL-1β ELISA and intercellular adhesion molecule-1
(ICAM-1) ELISA test kits, as well as pentobarbital and
2,3,5-triphenyltetrazolium chloride (TTC), were purchased from
Nanjing Jiancheng Technology Co., Ltd. (Nanjing, China). Enhanced
chemiluminescence diagnostic, bicinchoninic acid (BCA) protein
assay and nucleoprotein and plasmosin extraction kits were
purchased from Nanjing KeyGen Biotech. Co., Ltd. (Nanjing,
China).
Preparation of the DGSN decoction
The ratio of Angelica sinensis, Radix
Paeonia, Ramulus Cinnamomi, Herba Asari Mandshurici, Radix
Glycyrrhizae, Medulla Tetrapanacis and Fructus Jujubae in DGSN was
4:3:3:1:2:2:2. The DGSN was purchased from the First Affiliated
Hospital of Guangzhou University of Traditional Chinese Medicine
(Guangzhou, China). The DGSN was boiled twice in distilled water
(1:12, w/v) for 30 min. The blended supernatants were then
condensed to a concentration of 1 g crude drug/ml. Liquid
extraction (500 μl) was mixed with 2 ml blank rat serum. The mixed
liquid was acidified with 20 μl acetic acid and extracted with 8 ml
n-butanol. Subsequent to centrifugation at 400 × g for 20 min at
4–6°C, the organic phase was transferred into an empty tube and
evaporated to dryness under nitrogen at 40°C. The residue was
dissolved in 1 ml methanol and filtered (0.22 μm; Millipore,
Billerica, MA, USA), and an aliquot (20 μl) was then injected into
the high-performance liquid chromatography (HPLC) system.
Preparation of reference compounds and
HPLC analysis
The purity of the glycyrrhizic, cinnamic and ferulic
acids and peoniflorin was >98%. The chromatographic analysis was
performed on an Agilent 1200 system (Agilent Technologies, Palo
Alto, CA, USA), which was composed of a quaternary gradient pump,
an auto sampler, a Cosmosil C-18 column (5 μM particle, 250×4.6 mm)
and an ultraviolet detector. The mobile phase was acetonitrile-0.5%
aqueous acetic acid. The analysis was performed at a flow-rate of
1.0 ml/min with detections at 320, 230, 275 and 254 nm. The
gradient solvent system is shown in Table I.
 | Table IProgram of gradient elution. |
Table I
Program of gradient elution.
| Time, min | Φ (acetonitrile),
% | V (0.5%
aqueous acetic acid), % |
|---|
| 0–12 | 15 | 85 |
| 12–30 | 50 | 50 |
| 30–33 | 15 | 85 |
| 33–38 | 15 | 85 |
All reference compounds were dissolved in dimethyl
sulfoxide to afford 50 mmol/l stock solutions separately. The
concentration of mixed standards were as follows (where G, F, P and
C stand for glycyrrhizic acid, ferulic acid, peoniflorin and
cinnamic acid, respectively): Mixed standard 1 (G:
4×10−8 mol/l, F: 2×10−8 mol/l, P:
2×10−8 mol/l and C: 2×10−8 mol/l); Mixed
standard 2 (G: 8×10−8 mol/l, F: 4×10−8 mol/l,
P: 4×10−8 mol/l and C: 4×10−5 mol/l); Mixed
standard 3 (G: 1.6×10−7 mol/l, F: 8×10−8
mol/l, P: 8×10−8 mol/l and C: 8×10−8 mol/l);
Mixed standard 4 (G: 3.2×10−7 mol/l, F:
1.6×10−7 mol/l, P: 1.6×10−7 mol/l and C:
1.6×10−7 mol/l); and Mixed standard 5 (G:
6.4×10−7 mol/l, F: 3.2×10−7 mol/l, P:
3.2×10�7 mol/l and C: 3.2×10−7 mol/l). The
mixed standards were mixed separately with 2 ml blank rat serum,
respectively; the mixed liquid was acidified with 20 μl acetic acid
and extracted with 8 ml n-butyl alcohol. Following centrifugation
at 400 × g for 20 min at 4–6°C, the organic phase was transferred
into an empty tube and evaporated to dryness under nitrogen at
40°C. The residue was dissolved in 1 ml methanol and filtered (0.22
dm; Millipore). An aliquot (20 μl) was then injected into the HPLC
system.
Serum sample preparation
The 35 male rats were housed in an environmentally
controlled room and divided randomly into seven groups (five rats
in each group). The seven groups represented different time
periods, i.e. 30, 60, 90, 120, 180, 360 and 540 min). The DGSN
decoction was orally administered to the rats at a dosage of 20
g/kg. The abdominal cervical artery was then punctured under
pentobarbital sodium anesthesia and the blood (5 ml) was collected.
Each rat yielded 2 ml serum. The serum samples were processed
according to the same procedure as the standard samples. An aliquot
(20 μl) was injected into the HPLC system.
Experimental protocols
In the first set of experiments, it was investigated
whether the DGSN decoction contained the ferulic acid, peoniflorin,
cinnamic acid and glycyrrhizic acid (FPCG) combinations and, if so,
whether these active components were absorbed into the blood
following oral administration of the DGSN decoction. Animal
experiments were then performed based on an L16
(44) orthogonal design (24–26),
setting four factors with four different levels (Table II).
 | Table IIFour levels of the four active
components in the orthogonal design. |
Table II
Four levels of the four active
components in the orthogonal design.
| Glycyrrhizic acid
(mg/kg) | Ferulic acid
(mg/kg) | Peoniflorin
(mg/kg) | Cinnamic acid
(mg/kg) |
|---|
|
|
|---|
| Level | A | B | C | D |
|---|
| 1 | 0 | 0 | 0 | 0 |
| 2 | 25 | 200 | 25 | 100 |
| 3 | 50 | 300 | 50 | 200 |
| 4 | 100 | 400 | 100 | 400 |
SD rats were randomly divided into the above 16
groups (n=6 per group). Prior to surgery, the rats were
administrated different doses of the GFCP combinations for 5 days
(once a day, five doses in total). The last dose was administered
30 min prior to the surgery.
In the third set of experiments, the SD rats were
randomly divided into three groups (n=10 per group). The first
group underwent the same procedure as groups II and III, except the
suture was passed under the coronary artery without ligation (sham
group). In group II, the rats underwent 30 min ischemia followed by
2 h reperfusion. In group III, the rats were administered the FCG
combination (glycyrrhizic acid, 50 mg/kg; ferulic acid, 300 mg/kg
and cinnamic acid, 200 mg/kg) for five days prior to I/R. At the
end of the experiments, 4–5 ml blood was obtained. The serum was
separated from the blood cells by centrifugation and stored at
−80°C. For further analysis, the hearts were prepared for infarct
size measurement or the tissue was quickly frozen and stored at
−80°C.
Surgical preparations
The surgical protocol was performed according to
methods described previously (27). Briefly, rats were anesthetized with
pentobarbital (50 mg/kg, intraperitoneal), intubated and ventilated
with mechanical ventilation (tidal volume, 30 ml/kg; 70 strokes per
min). The rats were placed on heating plates to maintain core
temperature within the normal range (37.0–37.6°C) and the left
femoral vein was cannulated to inject the drugs. With the fourth
intercostal space opened, the heart was exteriorized and the
pericardium was cut. The left anterior descending coronary artery
was ligated between the left atrium and the pulmonary outflow tract
using a 6-0 silk suture. Successful ligation was verified by
regional cyanosis of the myocardial surface and ischemic ST-segment
changes in the electrocardiogram. The heart was subsequently
replaced in the thoracic cavity, the thoracic cavity was drained of
remaining air (to avoid pneumothorax) and the chest was immediately
closed. Following occlusion for 30 min, the left anterior
descending coronary artery was opened to permit reperfusion for 2
h.
Measurement of area at risk (AAR) and
infarct size (IS)
Myocardial IS and AAR were determined as described
previously (27). Briefly, at the
end of reperfusion period, the rat hearts were removed and the
aortas were quickly cannulated. Once the coronary artery ligature
was tied, the hearts were perfused with Evan’s blue at a constant
pressure (80 mmHg). The atria and the right ventricle were removed,
and the left ventricle (LV), including the septum, was cut into 2-
to 3-mm slices from the apex to the base. The perfused myocardium
was stained blue, whereas the AAR remained unstained. The AAR was
determined as the percentage of the ischemic myocardial mass
against the LV myocardial mass. The unstained myocardium was
incubated for 30 min at 37°C in TTC (1% in 0.1 mol/l phosphate
buffer, pH 7.4). The noninfarcted myocardium was deep red, in
contrast to the pale white of the infarcted myocardium. The IS was
expressed as the percentage of the infarcted myocardial mass
against the ischemic myocardial mass.
Biochemical parameters
The serum obtained from the rats was used for the
measurement of MB-isoenzyme of creatine kinase (CK-MB), TNFα,
IL-1β, IL-6 and ICAM-1 levels. CK-MB level was determined following
the homogenization of the rat myocardium in lysis buffer from
BioTeke Corporation (Beijing, China). TNFα, IL-1β, IL-6, ICAM-1
aand MDA levels, and SOD activity were determined following the
homogenization of the rat myocardium in lysis buffer from Nanjing
Jiancheng Technology Co., Ltd. In addition, the protein content of
all tissues was determined using the BCA method.
Electron microscopy
For the ultrastructural morphological study, the
samples were fixed with 2.5% glutaraldehyde solution, and then
dehydrated in a graded series of ethanol, 1%
O5O4, phosphate-buffered saline and acetone,
and embedded in Epon812 embedding medium. The ultrathin sections
were prepared on a Reichert-Jung Ultracut E ultramicrotome (Leica
Corporation, Shanghai, China), picked up on copper grids and
stained. Specimens were observed under a JEM-100CX electron
microscope (JEOL Japan Electronics Co., Ltd. Tokyo, Japan).
Histological examination
Myocardial tissues of SD rats were fixed in 10%
neutral formaldehyde for 24 h, and then each sample was dehydrated
with segments embedded in paraffin and cut into 5-μm thick sections
for staining with hematoxylin and eosin (H&E).
Western blot analysis
Rat myocardium was homogenized in lysis buffer (50
mm Tris pH 7.4, 150 mm NaCl, 1% Triton X-100, 1% sodium
deoxycholate, 0.1% SDS, EDTA and protease inhibitor cocktail) and
centrifuged at 3,000 × g for 10 min. Protein concentration was
determined using a BCA protein assay kit according to the
manufacturer’s instructions (Nanjing KeyGen Biotech. Co., Ltd.).
Equal amounts of protein (100 μg/sample) were electrophoresed by
SDS-PAGE and transferred onto a polyvinylidene difluoride membrane.
The membrane was blocked with 5% non-fat milk in 1X Tris buffered
saline and 0.1% Tween 20 at room temperature for 3 h. The membrane
was then incubated overnight at 4°C with the appropriate primary
antibody [anti-phospho-I-κBα (Ser32/36), anti-I-κBα, anti-NF-κBp65,
anti-PPARα, anti-GAPDH or anti-phospho-Akt1/2] diluted in Tris
buffered saline/Tween 20 (Tris buffered saline, 0.1% Tween 20). The
working concentrations of the anti-phospho-I-κBα (Ser32/36),
anti-I-κBα, anti-NF-κBp65, anti-PPARα, anti-pAkt1/2 and anti-GAPDH
antibodies were 1:500, 1:1,000, 1:1,000, 1:1,000, 1:500 and
1:2,000, respectively. Following incubation with
peroxidase-conjugated goat anti-rabbit IgG secondary antibodies for
1 h, the blots were developed with chemiluminescence reagent and
exposed to X-ray film. Nuclear protein was then extracted using an
extraction kit according to the manufacturer’s instructions
(Nanjing KeyGen Biotech. Co., Ltd.). Band intensities were
quantified using a densitometer analysis system (Quantity
One®, Bio-Rad, Hercules, CA, USA).
Statistical analysis
Data are presented as the mean ± standard deviation.
Statistical analysis for the experimental groups was performed
using SPSS for Windows version 13.0 (SPSS, Inc., Chicago, IL, USA).
Differences among groups were compared with one-way analysis of
variance (ANOVA) followed by the Dunnett’s test. Differences were
considered statistically significant when P<0.05. The variance
analysis was applied in the orthogonal experiment.
Results
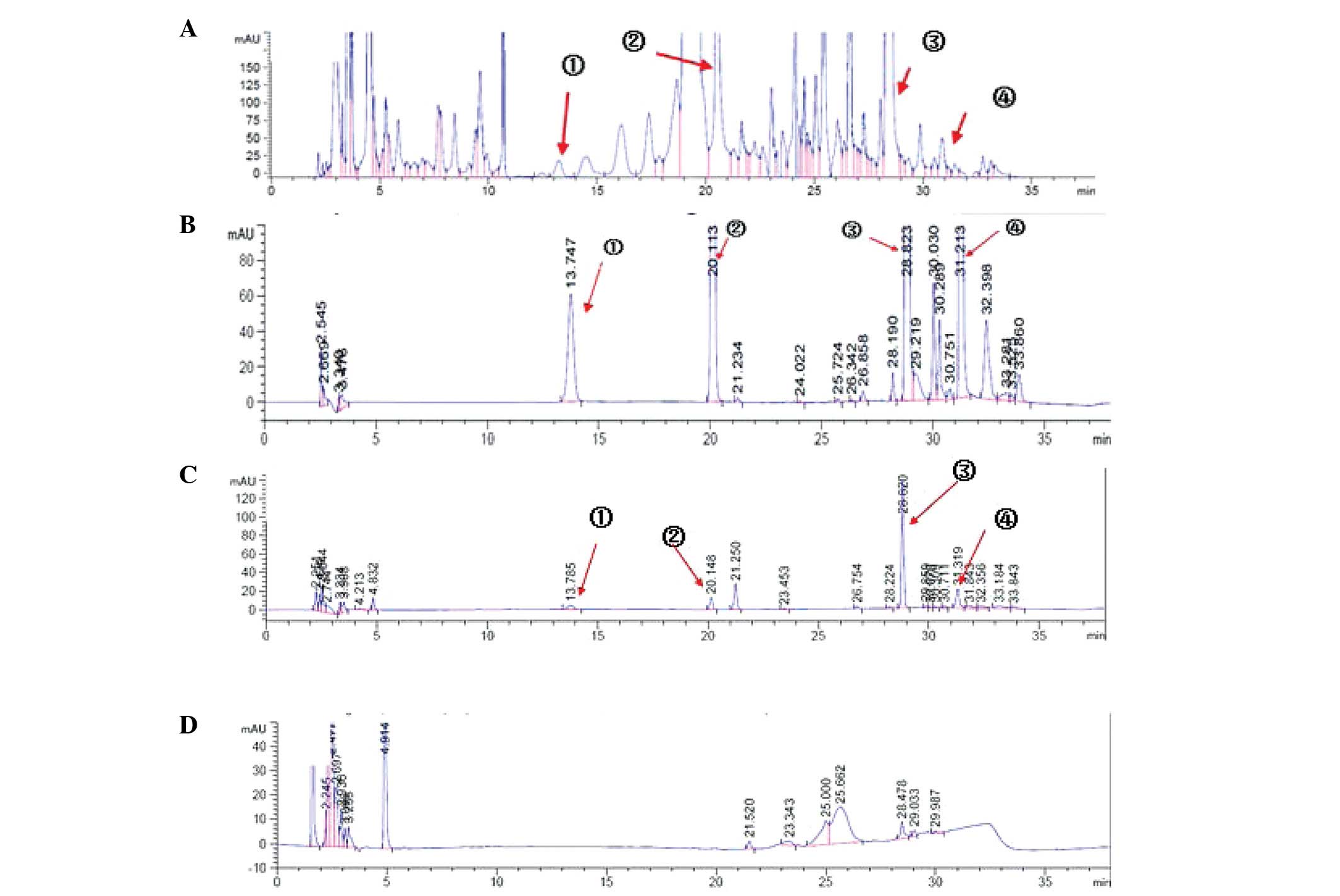
Detection of serum components by HPLC
following oral administration of DGSN
The results (Fig.
1A–D) showed the DGSN decoction contained FPCG detected in
serum of rats following oral administration of the DGSN decoction
by HPLC analysis.
Orthogonal-design experiment results
In the orthogonal experiments (Tables III–VI), SOD activity was assessed using the
xanthine oxidase method and MDA levels were measured using the
thiobarbituric acid-reactive-substances assay. Through ANOVA and
the orthogonal experiment intuitionistic approach, it was found
that glycyrrhizic acid was the most effective component at
increasing SOD activity in the rat myocardium following I/R;
ferulic acid, peoniflorin and cinnamic acid were second-most,
third-most and least effective, respectively. The optimal drug
combination was glycyrrhizic acid (50 mg/kg), cinnamic acid (0
mg/kg), ferulic acid (0 mg/kg) and peoniflorin (0 mg/kg). In
addition, it was found that cinnamic acid was the most effective
component at reducing MDA levels in the rat myocardium following
I/R; ferulic acid, peoniflorin and glycyrrhizic acid were
second-most, third-most and least effective, respectively. The
optimal drug combination was cinnamic acid (200 mg/kg), ferulic
acid (300 mg/kg), peoniflorin (0 mg/kg) and glycyrrhizic acid (0
mg/kg). Taking both sets of results into consideration, the
combination of glycyrrhizic acid (50 mg/kg), cinnamic acid (200
mg/kg) and ferulic acid (300 mg/kg) (FCG) was regarded as optimal.
This not only lowered the content of MDA, but also increased the
activity of SOD.
 | Table IIIEffect of FPCG on increasing
superoxide dismutase activity in the rat myocardium following
ischemia-reperfusion. |
Table III
Effect of FPCG on increasing
superoxide dismutase activity in the rat myocardium following
ischemia-reperfusion.
| Source of
variation | Mean-square | F | P-value | n |
|---|
| Ferulic acid | 130.805 | 1.958 | 0.155 | 6 |
| Peoniflorin | 22.190 | 0.332 | 0.802 | 6 |
| Cinnamic acid | 15.898 | 0.238 | 0.869 | 6 |
| Glycyrrhizic
acid | 322.778 | 4.833 | 0.012 | 6 |
 | Table VIEffect of FPCG on reducing MDA levels
in the rat myocardium following ischemia-reperfusion. |
Table VI
Effect of FPCG on reducing MDA levels
in the rat myocardium following ischemia-reperfusion.
| Group | Glycyrrhizic
acid | Ferulic acid | Peoniflorin | Cinnamic acid | MDA (nmol/mg) |
|---|
| 1 | 1 | 1 | 1 | 1 | 0.99±0.11 |
| 2 | 3 | 3 | 1 | 3 | 0.43±0.07 |
| 3 | 4 | 4 | 1 | 4 | 0.48±0.31 |
| 4 | 2 | 2 | 1 | 2 | 0.43±0.12 |
| 5 | 2 | 4 | 3 | 1 | 1.19±0.03 |
| 6 | 4 | 3 | 2 | 1 | 0.66±0.11 |
| 7 | 3 | 2 | 4 | 1 | 0.65±0.20 |
| 8 | 1 | 4 | 4 | 3 | 0.58±0.32 |
| 9 | 4 | 1 | 4 | 2 | 0.54±0.05 |
| 10 | 1 | 3 | 3 | 2 | 0.45±0.12 |
| 11 | 2 | 3 | 4 | 4 | 0.40±0.07 |
| 12 | 2 | 1 | 2 | 3 | 0.58±0.12 |
| 13 | 3 | 1 | 3 | 4 | 0.73±0.14 |
| 14 | 3 | 4 | 2 | 2 | 0.89±0.23 |
| 15 | 4 | 2 | 3 | 3 | 0.48±0.12 |
| 16 | 1 | 2 | 2 | 4 | 0.86±0.30 |
| K1 | 0.72 | 0.71 | 0.58 | 0.62 | - |
| K2 | 0.65 | 0.61 | 0.75 | 0.58 | - |
| K3 | 0.67 | 0.48 | 0.71 | 0.52 | - |
| K4 | 0.54 | 0.78 | 0.54 | 0.87 | - |
| Rj | 0.18 | 0.30 | 0.21 | 0.36 | - |
Effect of FCG pretreatment on biochemical
parameters induced by I/R injury
TNFα, IL-1β, IL-6 and ICAM-1 levels were detected by
ELISA assay, and the presence of CK-MB was revealed by enzyme rate
assay. As shown in Tables VII
and VIII, the levels of TNFα,
IL-1β, IL-6, ICAM-1 and CK-MB were increased significantly in the
myocardium of rats with I/R injury as compared with those in the
myocardium of sham-operated rats. However, administering FCG
pretreatment for five days before the I/R injury significantly
decreased the serum levels of TNFα, IL-1β, IL-6, ICAM-1 and CK-MB
as compared with the levels in the I/R group without
pretreatment.
 | Table VIIEffects of FCG pretreatment on serum
TNFα and ICAM-1 levels in the rat myocardium following
ischemia-reperfusion. |
Table VII
Effects of FCG pretreatment on serum
TNFα and ICAM-1 levels in the rat myocardium following
ischemia-reperfusion.
| Group | TNFα (ng/l) | ICAM-1 (ng/l) |
|---|
| Sham | 21.85±3.96a | 19.90±1.02a |
| I/R | 46.77±6.54 | 35.20±3.34 |
| PPC+I/R | 33.54±4.95a | 23.07±1.73a |
 | Table VIIIEffects of FCG pretreatment on serum
IL-1β, IL-6 and CK-MB levels in the rat myocardium following
ischemia-reperfusion. |
Table VIII
Effects of FCG pretreatment on serum
IL-1β, IL-6 and CK-MB levels in the rat myocardium following
ischemia-reperfusion.
| Group | IL-1β (ng/l) | IL-6 (ng/l) | CK-MB (U/l) |
|---|
| Sham | 18.29±5.32a | 12.11±2.11a | 229.45±21.08 |
| I/R | 26.44±8.24 | 34.32±6.50 | 1025.50±88.19 |
| PPC+I/R | 19.20±2.47a | 16.77±4.22a | 427.54±59.18 |
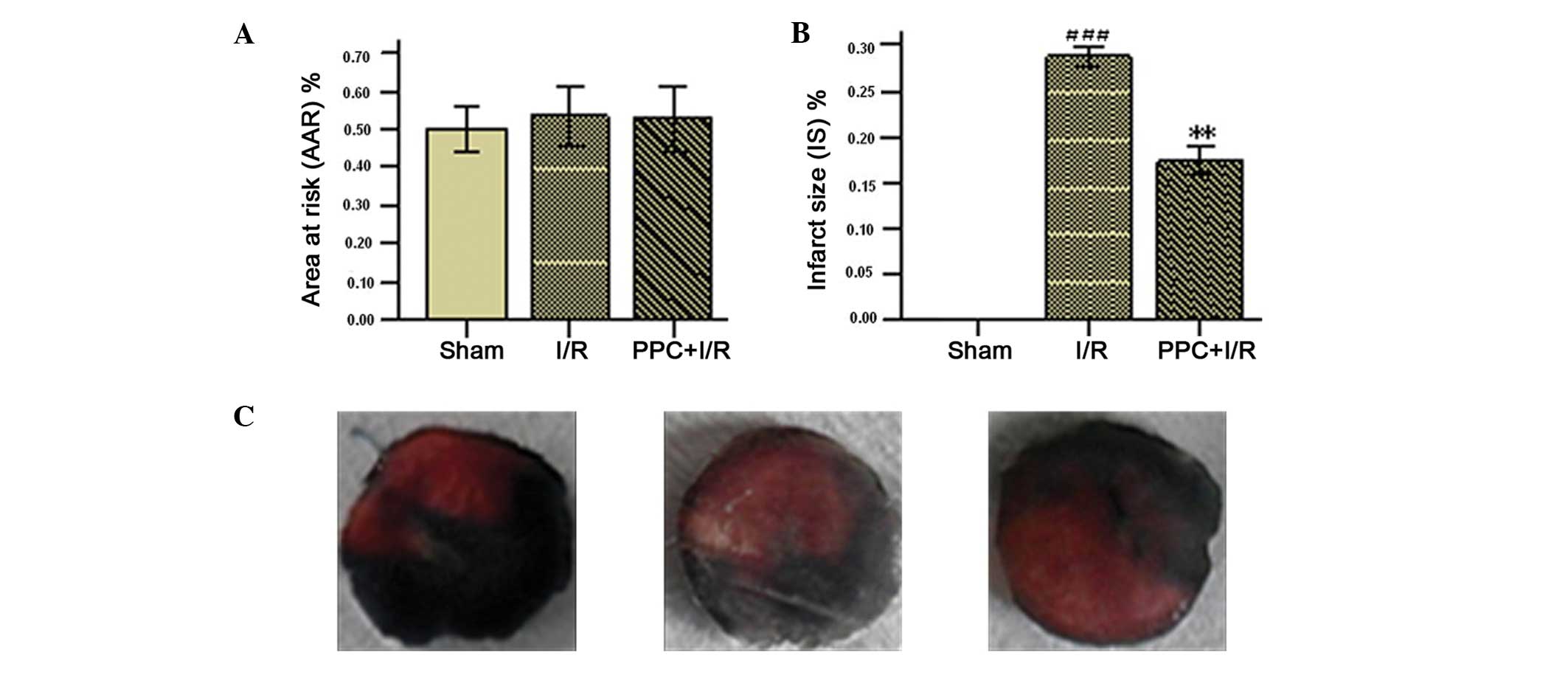
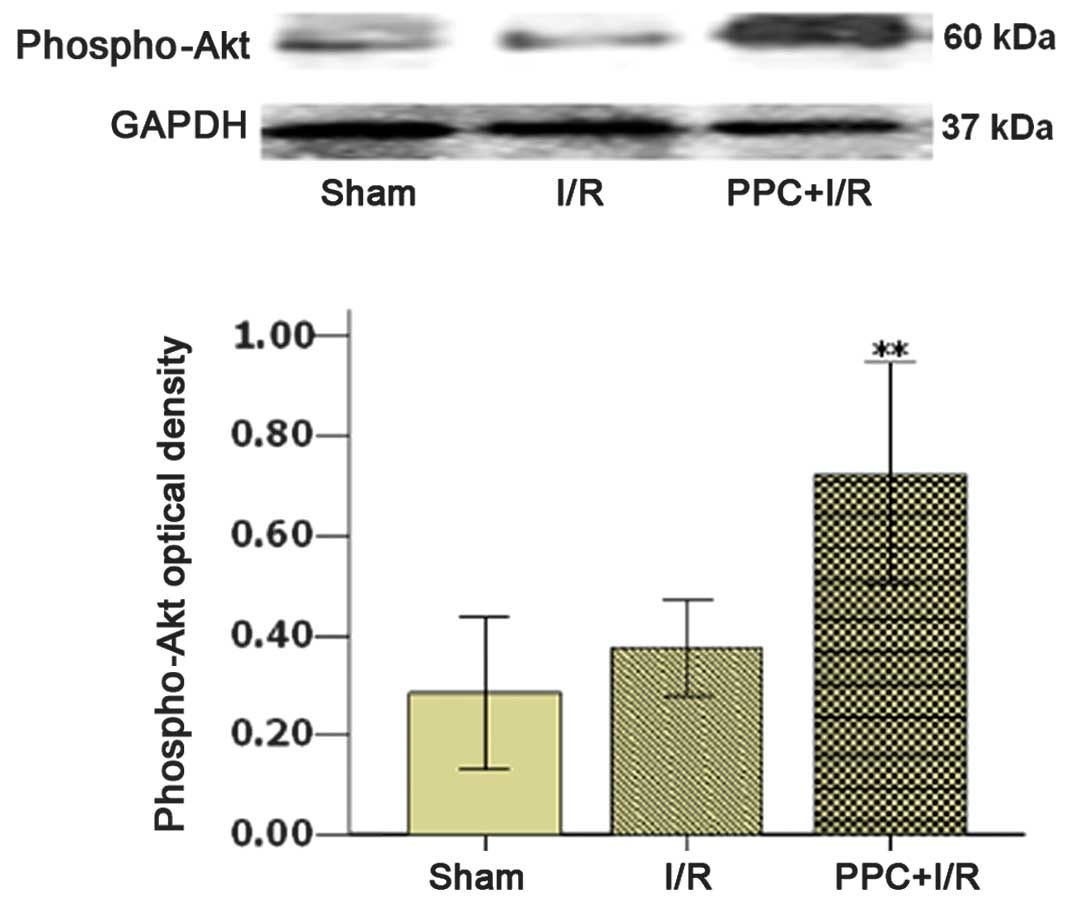
Effect of FCG pretreatment on myocardial
IS and AAR
The AAR and IS are a percentage of the LV and AAR
weights, respectively. AAR and IS were used to assess the efficacy
of the FCG combination in the protection of the rat myocardium
following I/R injury. Significant differences were not apparent
among the three groups with regard to the AAR. The values for the
IS were 0.17±0.01% in the FCG pretreatment group and 0.29±0.08% in
the I/R group. Significant differences in IS were observed between
the FCG pretreatment group (PPC plus I/R) and the I/R group
(Fig. 2A–C).
 | Figure 2Effects of FCG on (A) myocardial AAR
and (B) IS. (C) Images of the myocardial AAR and infarct area in
the sham, I/R and PPC+I/R groups (left, center and right,
respectively). The area of infarct is white, the myocardial AAR is
deep red and the nonischemic area is blue. Data are presented as
the mean ± standard deviation; n=6. **P<0.01 vs. I/R;
###P<0.001 vs. sham, n=6. Sham, sham-operated animal
without ligation; I/R, 30 min ischemia followed by 2 h reperfusion;
PPC+I/R, administration of FCG for 5 days prior to the induction of
myocardial ischemia. FCG, ferulic acid (300 mg/kg), cinnamic acid
(200 mg/kg) and glycyrrhizic acid (50 mg/kg); AAR, area at risk;
IS, infarct size. |
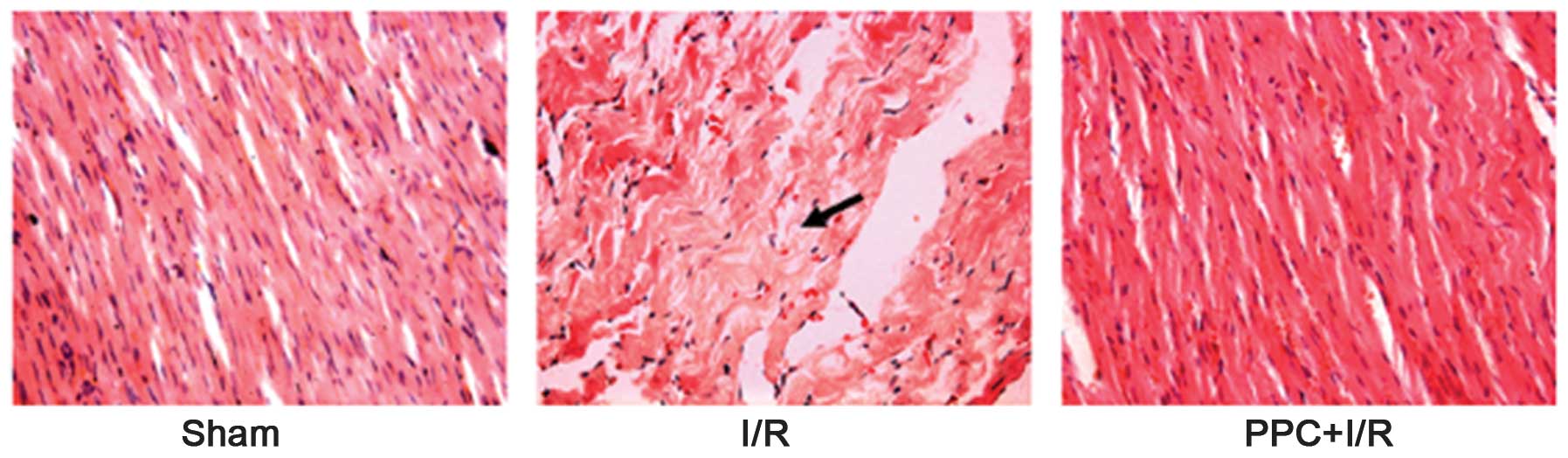
Effect of FCG pretreatment on
histological changes induced by I/R injury
The histomorphology of the cardiac muscle of the LV
of the rats was observed using H&E staining. The following
changes were found in the I/R group: Muscle fiber disarrangement,
clear hydropic degeneration, cell dropsy, dark nuclear staining,
vascular bleeding, inflammatory cell infiltration and myocardial
fiber atrophy. These morphological changes were alleviated by FCG
pretreatment (Fig. 3).
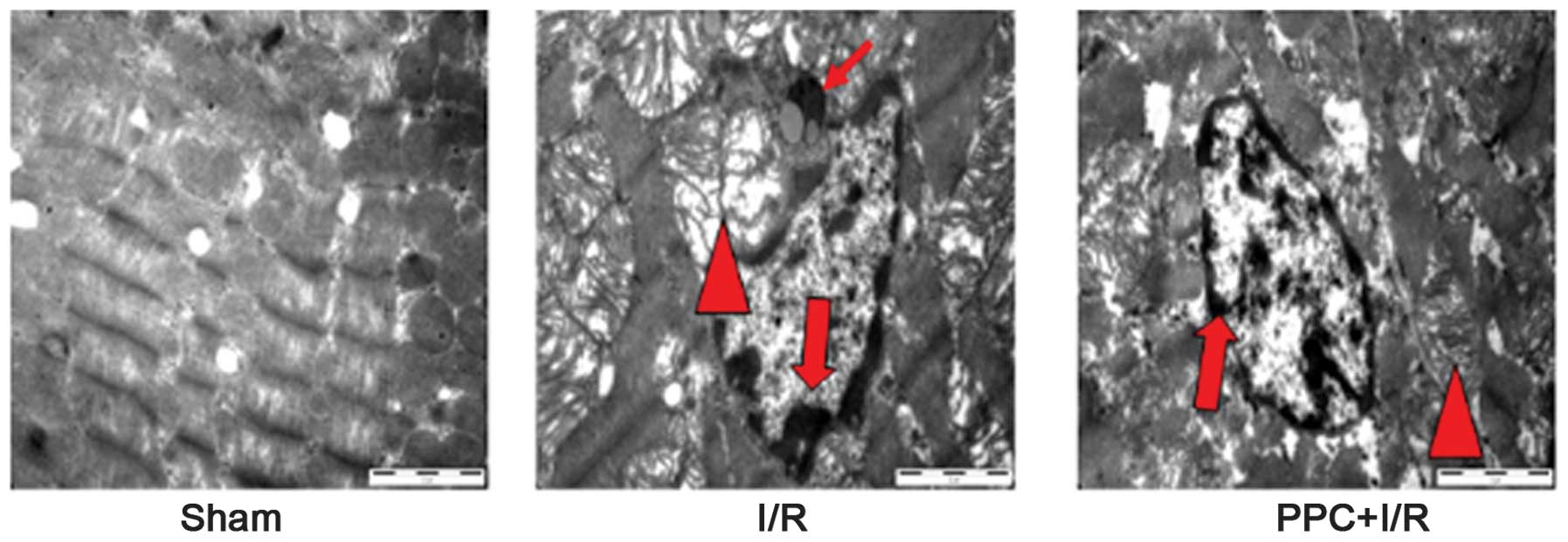
Effect of FCG pretreatment on
ultrastructural changes induced by I/R injury
The ultrastructural changes in the cardiac muscle of
the LV of the rats were observed by transmission electron
microscopy (Fig. 4). These changes
included cell swelling, mitochondrial swelling, cristae
disorganization, myofibril shrinkage and lysis, chromatin
condensation and aggregation at the periphery of the nucleus and
nuclear fragmentation. Apoptotic bodies were also observed in the
I/R group. The aforementioned ultrastructural changes were
alleviated in the PPC plus I/R group as compared with the I/R
group.
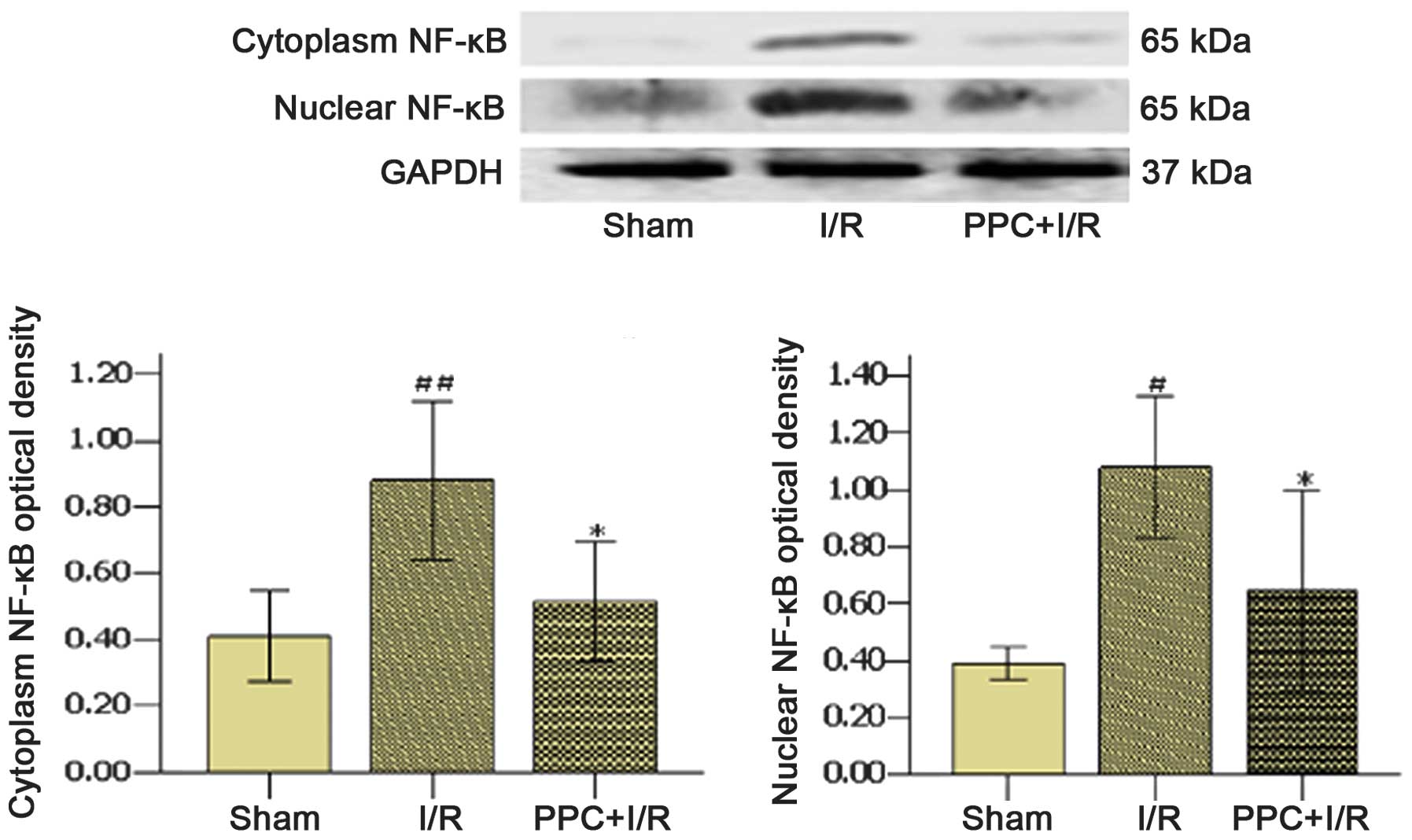
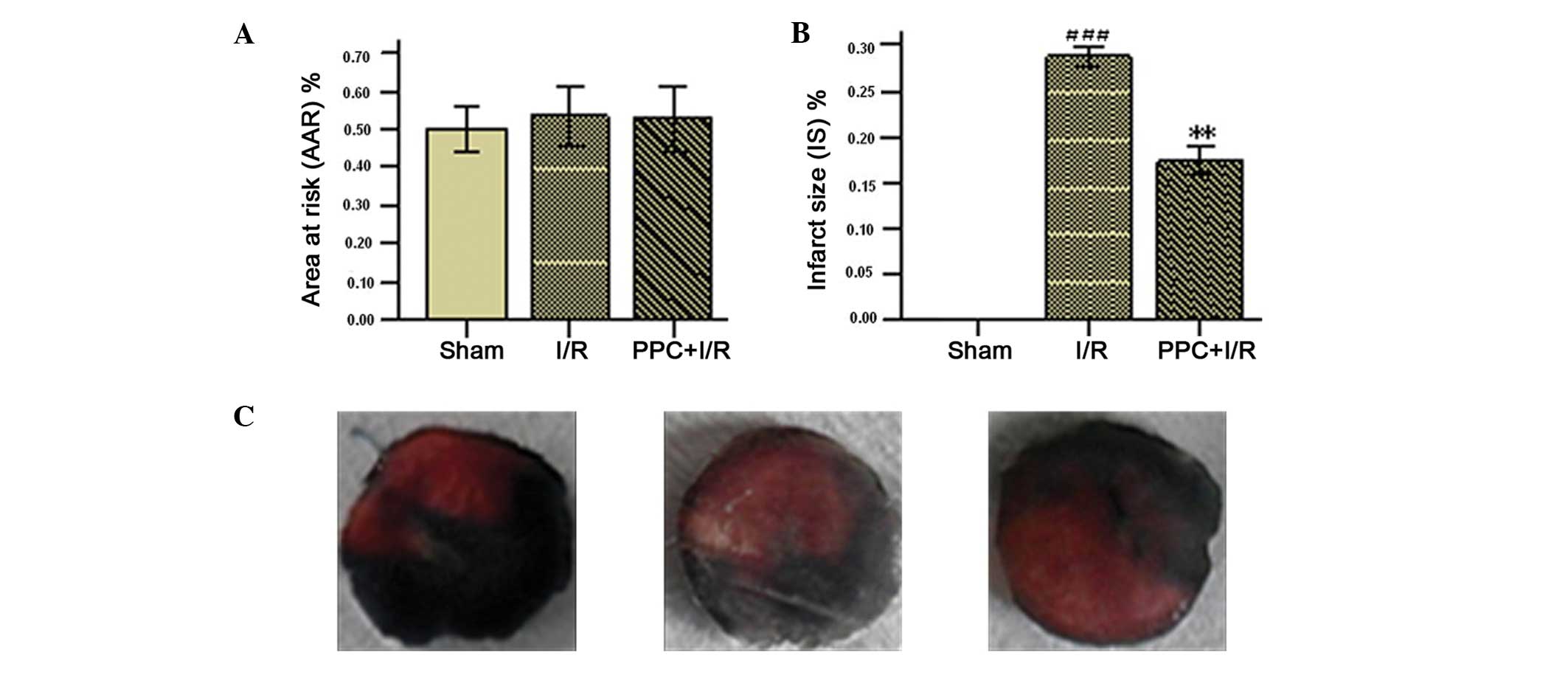
Effect of FCG pretreatment on the
expression of I-κBα, NF-κB, p65, PPARα and pAkt1/2 induced by I/R
injury
The effects of pharmacological pretreatment with FCG
on nuclear NF-κBp65, cytoplasmic NF-κBp65, IκBα, phospho-IκBα,
PPARα and phospho-Akt proteins in the myocardium of rats were
detected by western blot analysis (Figs. 5–8). Compared with the sham group, the
expression levels of NF-κBp65 and phospho-I-κB were significantly
increased in the I/R group, whereas the expression levels of I-κB
and PPARα were decreased. The levels of phospho-Akt were increased
in the I/R group, although the difference was not significant.
However, compared with the I/R group, the expression of NF-κBp65
and phospho-I-κB was significantly decreased, whereas the
expression of I-κB, PPARα and phospho-Akt was increased in the PPC
plus I/R group.
Discussion
The results of the present study showed that, while
a number of chemical constituents were contained in DGSN decoction,
a Traditional Chinese Medicine (Fig.
1A), <10 types of constituent could be absorbed into the
blood (Fig. 1C) following oral
administration of the DGSN decoction. Only the components that can
be absorbed into the blood may play a role in pharmacology.
Therefore, the objective of our study was to investigate which
components could be absorbed following oral administration of DGSN
decoction, and to then find the optimal drug cocktail composition
from the absorbable components, in order to treat I/R injury of the
rat myocardium through orthogonal experiments. The mechanism of the
optimal cocktail composition was then further explored.
DGSN effectively treats coronary heart diseases.
Cinnamic, glycyrrhizic and ferulic acids, and peoniflorin can be
detected in DGSN decoction (9–11),
and in the serum of rats following the oral administration of DGSN
decoction (Fig. 1A–D). A number of
studies have reported that glycyrrhizic (28), ferulic (29,30)
and cinnamic (31,32) acids can alleviate damage following
I/R injury, respectively. Therefore, it may be hypothesized that
the optimal drug combination for treating rat myocardial I/R injury
may be derived from the components of DGSN.
In multifactor experiments, an orthogonal experiment
design enables the hierarchical status of the factors and the
interaction among the factors to be established, which facilitates
the determination of the ideal combination of multiple factors with
as few sampling experiments as possible. In pharmacodynamic studies
of multiple factors, the optimal drug combinations can be revealed
by orthogonal experiment design. The L16 (44)
orthogonal design was selected in the present study to find an
optimal cocktail drug combination from the components absorbed
following the oral administration of DGSN decoction. The strength
of effect as well as correlations among components in the cocktail
drug combinations were detected. SOD activity and MDA levels
represent an evaluation index to measure the effectiveness among
these components and cocktail drug combinations, since these
indexes can respond to the damage degrees of oxidative stress and
inflammation. Reperfusion is essential for myocardial tissue
survival. However, its effect on ischemic myocardium is two-fold,
as it can trigger oxidative tissue damage and inflammation
(23,27,33,34).
Furthermore, the inflammatory response and oxidative damage are
important causes of myocardial I/R injury (35). The MDA content can respond to the
degree of lipid peroxidation, and the modulation of antioxidant
enzymes, such as SOD and catalase, can protect against oxidative
cardiac disorders (36,37).
In the present study, the L16 (44)
orthogonal experiment intuitionistic analytical approach was used
to find the most effective component at reducing MDA levels in the
rat myocardium following I/R. The most effective component was
cinnamic acid, followed by ferulic acid, peoniflorin and
glycyrrhizic acid. However, ANOVA showed that only cinnamic acid
and ferulic acid were capable of significantly decreasing the
content of MDA (Table V). In
addition, it was found that the most effective component at
increasing SOD activity in the rat myocardium following I/R was
glycyrrhizic acid, followed by ferulic acid, peoniflorin and
cinnamic acid. However, ANOVA showed that only glycyrrhizic acid
significantly increased the activity of SOD (Table III). Summarizing the results of
the SOD activity and MDA level analysis, FCG was revealed to be the
optimal drug combination, consisting of glycyrrhizic (50 mg/kg),
cinnamic (200 mg/kg) and ferulic (300 mg/kg) acid. This combination
not only reduced the content of MDA, but also increased the
activity of SOD.
 | Table VEffect of FPCG on reducing
malondialdehyde levels in the rat myocardium following
ischemia-reperfusion. |
Table V
Effect of FPCG on reducing
malondialdehyde levels in the rat myocardium following
ischemia-reperfusion.
| Source of
variation | Mean-square | F | P-value | n |
|---|
| Ferulic acid | 0.167 | 3.32 | 0.032 | 6 |
| Peoniflorin | 0.119 | 2.367 | 0.090 | 6 |
| Cinnamic acid | 0.231 | 4.582 | 0.009 | 6 |
| Glycyrrhizic
acid | 0.067 | 1.337 | 0.280 | 6 |
In the present study the second step was to explore
the mechanism underlying the effect of FCG on I/R injury. The
effects could be observed in a number of aspects, including
myocardial IS, myocardial tissue construction, cell ultrastructure,
inflammatory and biochemical parameters, signaling pathways of the
inflammatory response and oxidative damage. The results showed that
FCG could decrease myocardial IS (Fig.
2). The following changes were also revealed: Muscle fiber
disarrangement, clear hydropic degeneration, cell dropsy, dark
nuclear staining, vascular bleeding and inflammatory cell
infiltration. These changes were significantly alleviated by FCG
pretreatment compared with the I/R group. In addition, the cardiac
muscle ultrastructural changes were observed via transmission
electron microscopy (Fig. 4).
These included cell swelling, mitochondrial swelling, cristae
disorganization, myofibril shrinkage and lysis. Chromatin
condensation and aggregation at the periphery of the nucleus and
nuclear fragmentation were shown to be significantly alleviated by
FCG pretreatment compared with the I/R group.
NF-κB is an important transcriptional regulatory
factor and plays an important role in myocardial I/R injury.
Furthermore, NF-κB has a close association with the inflammatory
response and oxidative damage. I/R injury can cause a rapid
phosphorylation of I-κBα and degradation of I-κBα (I-κBα is the
inhibitory protein of NF-κB activation). This leads to the
activation of NF-κB translocation into the nucleus and the
transcription of other downstream inflammatory factors, including
TNFα, IL-1β, IL-6 and ICAM-1 (38–40).
PPARα is an important regulatory factor of NF-κB (41,42)
that, following activation by its ligands, can suppress the
activation and nuclear translocation of NF-κB (43), repress the expression of
inflammatory factors and increase the expression of SOD (41,44–46).
PPARα is closely associated with the Akt signal transduction
pathway (47). In the present
study, the expression levels of TNFα, IL-1β, IL-6, ICAM-1, NF-κBp65
and phospho-I-κBα were detected to be significantly increased in
the I/R group, while the expression levels of I-κBα, PPARα were
significantly decreased. The levels of phospho-Akt were increased
in the I/R group compared with the sham group, although the
difference was not significant. However, compared with the I/R
group, the expression levels of TNFα, IL-1β, IL-6 and ICAM-1
significantly decreased with FCG pretreatment. Furthermore, the
expression levels of NF-κBp65 and phospho-I-κBα significantly
decreased, and the expression of I-κBα, PPARα and phospho-Akt
increased. The results of this study suggested that FCG
pretreatment protected the myocardium from I/R injury by activating
Akt and PPARα, decreasing I-κBα phosphorylation and further
repressing NF-κBp65. However, the results did not confirm that the
protective effect of FCG pretreatment against I/R injury in the rat
myocardium was exerted by the direct activation of Akt. The
activation of Akt can facilitate FCG to activate PPARα and further
inhibit the phosphorylation of I-κBα to downregulate the expression
and activity of NF-κBp65. However, it is not known whether FCG can
directly inhibit the expression of NF-κBp65 through the interaction
of Akt, PPARα, I-κBα and NF-κB. Further studies are in
progress.
In conclusion, we have found and validated that
cinnamic acid, glycyrrhizic acid and ferulic acid are present in
DGSN decoction, and can be absorbed into the blood of rats
following oral administration of DGSN decoction. The optimal drug
combination, FCG, is a mixture of glycyrrhizic (50 mg/kg), cinnamic
(200 mg/kg) and ferulic (300 mg/kg) acid. FCG was shown to not only
lower the content of MDA but also increase the activity of SOD, as
demonstrated by the L16 (44) orthogonal design.
These findings show that FCG may alleviate myocardial I/R injury.
It was suggested that FCG acted by significantly decreasing the
levels of TNFα, IL-1β, IL-6 and ICAM-1 in the serum. This
significantly decreased the myocardial AAR and IS and alleviated
the changes in myocardial tissue construction and cell
ultrastructure observed by H&E staining and transmission
electron microscopy. In addition, FCG significantly increased the
expression of I-κBα, PPARα and phospho-Akt, and decreased the
expression levels of NF-κBp65 and phospho-I-κBα. Accordingly, the
results of the present study indicated that the FCG drug
combination protected the myocardium from I/R injury through
modulation of the Akt, PPARα and NF-κB pathways.
Acknowledgements
The authors would like to thank the National Natural
Science Foundation of China for partially supporting this study
(nos. 30672679 and 81173189).
Abbreviations:
|
MDA
|
malondialdehyde
|
|
SOD
|
superoxide dismutase
|
|
TNFα
|
tumor necrosis factor-α
|
|
IL-1β
|
interleukin-1β
|
|
IL-6
|
interleukin-6
|
|
ICAM-1
|
intercellular adhesion molecule 1
|
|
PPARα
|
peroxisome proliferator-activated
receptor α
|
|
I-κBα
|
inhibitory-κBα
|
|
NF-κB
|
nuclear factor-κB
|
|
CK-MB
|
MB-isoenzyme of creatine kinase
|
|
DGSN
|
Dang-gui-si-ni-tang
|
References
|
1
|
Murray CJ and Lopez AD: Alternative
projection of mortality and disability by cause 1990–2020: Global
Burden of Disease Study. Lancet. 349:1498–1504. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Yellon DM and Hausenloy DJ: Myocardial
reperfusion injury. N Engl J Med. 357:1121–1135. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Murry CE, Jennings RB and Reimer KA:
Preconditioning with ischemia: a delay of lethal cell injury in
ischemic myocardium. Circulation. 74:1124–1136. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Philipp S, Yang XM, Cui L, et al:
Postconditioning protects rabbit hearts through a protein kinase
C-adenosine A2b receptor casade. Cardiovasc Res. 70:308–314. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tissier R, Cohen MV and Downey JM:
Protecting the acutely ischemic myocardium beyond reperfusion
therapies: are we any closer to realizing the dream of infarct size
elimination? Arch Mal Coeur Vaiss. 100:794–802. 2007.PubMed/NCBI
|
|
6
|
Gross ER, Hsu AK and Gross GJ:
Opioid-induced cardioprotection occurs via glycogen synthase kinase
beta inhibition during reperfusion in intact rat hearts. Circ Res.
94:960–966. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tissier R, Waintraub X, Couvreur N, et al:
Pharmacological postconditioning with the phytoestrogen genistein.
J Mol Cell Cardiol. 42:79–87. 2007. View Article : Google Scholar
|
|
8
|
Efthymiou CA, Mocanu MM and Yellon DM:
Atorvastatin and myocardial reperfusion injury: new pleiotropic
effect implicating multiple prosurvival signaling. J Cardiovasc
Pharmacol. 45:247–252. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gao YQ, Zhao GP and Jiang RW:
Determination of ferulic acid serum concentration in Danggui Sini
Decotion by HPLC and its pharmacokinetics in rats. Zhong Cheng Yao.
33:419–422. 2011.(In Chinese).
|
|
10
|
Gao YQ, Wu J, Jiang RW and Zhao GP:
Determination of cinnamic acid and glycyrrhizic acid in rat serum
and its pharmacokinetics after oral administration of Dangguisini
decoction. Zhong Yao Cai. 34:408–411. 2011.(In Chinese). PubMed/NCBI
|
|
11
|
Zhao X, Gu Y, Song XX, et al: Simultaneous
determination of four main components in Dangguisini decoction.
Shenyang Yao Ke Da Xue Xue Bao. 13:200–203. 2008.(In Chinese).
|
|
12
|
Nagai T, Egashira T, Yamanaka Y and Kohno
M: The protective effect of glycyrrhizin against injury of the
liver caused by ischemia-reperfusion. Arch Environ Contam Toxicol.
20:432–436. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Abdugafurova MA, Li VS, et al:
Antioxidative properties of glycyrrhyzic acid salts and their
effect on the liver monooxygenase system. Vopr Med Khim. 36:29–31.
1990.(In Russian). PubMed/NCBI
|
|
14
|
Yokozawa T, Liu ZW and Chen CP: Protective
effects of Glycyrrhizae radix extract and its compounds in a renal
hypoxia (ischemia)-reoxygenation (reperfusion) model.
Phytomedicine. 6:439–445. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kilgore KS, Tanhehco EJ, Park JL, et al:
Reduction of myocardial infarct size in vivo by carbohydrate-based
glycomimetics. J Pharmacol Exp Ther. 284:427–435. 1998.PubMed/NCBI
|
|
16
|
Nagai T, Egashira T, Kudo Y, Yamanaka Y
and Shimada T: Attenuation of dysfunction in the
ischemia-reperfused liver by glycyrrhizin. Jpn J Pharmacol.
58:209–218. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cartron E, Carbonneau MA, et al: Specific
antioxidant activity of caffeoyl derivatives and other natural
phenolic compounds: LDL protection against oxidation and decrease
in the proinflammatory lysophosphatidylcholine production. J Nat
Prod. 64:480–486. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Banskota AH, Nagaoka T, Sumioka LY, et al:
Antiproliferative activity of the Netherlands propolis and its
active principles in cancer cell lines. J Ethnopharmacol. 80:67–73.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Neto CC: Cranberry and blueberry: evidence
for protective effects against cancer and vascular diseases. Mol
Nutr Food Res. 51:652–664. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Huang X, Qin F, Zhang HM, et al:
Cardioprotection by Guanxin II in rats with acute myocardial
infarction is related to its three compounds. J Ethnopharmacol.
121:268–273. 2009. View Article : Google Scholar
|
|
21
|
Yogeeta SK, Raghavendran HR, Gnanapragasam
A, et al: Ferulic acid with ascorbic acid synergistically
extenuates the mitochondrial dysfunction during beta-adrenergic
catecholamine induced cardiotoxicity in rats. Chem Biol Interact.
163:160–169. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wolfrum S, Richardt G, Dominiak P, et al:
Apstatin, a selective inhibitor of aminopeptidase P, reduces
myocardial infarct size by a kinin-dependent pathway. Br J
Pharmacol. 134:370–374. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Murota S, Fujita H, Wakabayashi Y and
Morita I: Cell adhesion molecule mediates endothelial cell injury
caused by activated neutrophils. Keio J Med. 45:207–211. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
López-Cacho JM, González-R PL, et al:
Robust optimization of alginate-Carbopol 940 bead formulations.
ScientificWorldJournal. 2012:6056102012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zhou J, Sun JB, Zheng P, et al: Orthogonal
array design for optimization of hollow-fiber-based liquid-phase
microextraction combined with high-performance liquid
chromatography for study of the pharmacokinetics of magnoflorine in
rat plasma. Anal Bioanal Chem. 403:1951–1960. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Xu Y, Zhang Y, Li Y, et al: Growth
promotion of Yunnan pine early seedlings in response to foliar
application of IAA and IBA. Int J Mol Sci. 13:6507–6520. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Cerqueira NF, Hussni CA and Yoshida WB:
Pathophysiology of mesenteric ischemia/reperfusion: a review. Acta
Cir Bras. 20:336–343. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Burley DS, Ferdinandy P and Baxter GF:
Cyclic GMP and protein kinase-G in myocardial
ischaemia-reperfusion: opportunities and obstacles for survival
signaling. Br J Pharmacol. 152:855–869. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chen HP, Liao ZP, Huang QR and He M:
Sodium ferulate attenuates anoxia/reoxygenation-induced calcium
overload in neonatal rat cardiomyocytes by NO/cGMP/PKG pathway. Eur
J Pharmacol. 603:86–92. 2009. View Article : Google Scholar
|
|
30
|
Howes MJ, Perry NS and Houghton PJ: Plants
with traditional uses and activities, relevant to the management of
Alzheimer’s disease and other cognitive disorders. Phytother Res.
17:1–18. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Point D, Coudert P, Leal F, et al:
Antioxidant activity of some ascorbic and cinnamic acids
derivatives. Farmaco. 53:85–88. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Jeong HG, You HJ, Park SJ, et al:
Hepatoprotective effects of 18beta-glycyrrhetinic acid on carbon
tetrachloride-induced liver injury: inhibition of cytochrome P450
2E1 expression. Pharmacol Res. 46:221–227. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Jaeschke H: Mechanisms of liver injury. II
Mechanisms of neutrophil-induced liver cell injury during hepatic
ischemia-reperfusion and other acute inflammatory conditions. Am J
Physiol Gastrointest Liver Physiol. 290:G1083–G1088. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Spanos CP, Papaconstantinou P, Spanos P,
et al: The effect of L-arginine and aprotinin on intestinal
ischemia-reperfusion injury. J Gastrointest Surg. 11:247–255. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Sima N, Lü W and Xie X: Early proteins E6
and E7 of human papillomavirus may attenuate ischemia-reperfusion
injury. Med Hypotheses. 76:607–609. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Olanders K, Sun Z, Börjesson A, et al: The
effect of intestinal ischemia and reperfusion injury on ICAM-1
expression, endothelial barrier function, neutrophil tissue influx,
and protease inhibitor levels in rats. Shock. 18:86–92. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Venardos KM, Perkins A, Headrick J and
Kaye DM: Myocardial ischemia-reperfusion injury, antioxidant enzyme
systems and selenium: a review. Curr Med Chem. 14:1539–1549. 2007.
View Article : Google Scholar
|
|
38
|
Di Paola R, Menegazzi M, Mazzon E, et al:
Protective effects of glycyrrhizin in a gut hypoxia
(ischemia)-reoxygenation (reperfusion) model. Intensive Care Med.
35:687–697. 2009. View Article : Google Scholar
|
|
39
|
Cepinskas G, Rui T and Kvietys PR:
Interaction between reactive oxygen metabolites and nitric oxide in
oxidant tolerance. Free Radic Biol Med. 33:433–440. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Li C, Browder W and Kao RL: Early
activation of transcription factor NF-kappaB during ischemia in
perfused rat heart. Am J Physiol. 276:H543–H552. 1999.PubMed/NCBI
|
|
41
|
Inoue I, Goto S, Matsunaga T, et al: The
ligands/activators for peroxisome proliferator-activated receptor
alpha (PPARalpha) and PPARgamma increase Cu2+,
Zn2+-superoxide dismutase and decrease p22phox message
expressions in primary endothelial cells. Metabolism. 50:3–11.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Yoo HY, Chang MS and Rho HM: Induction of
the rat Cu/Zn superoxide dismutase gene through the peroxisome
proliferator-responsive element by arachidonic acid. Gene.
234:87–91. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Ding GL, Cheng L, et al: PPARdelta
modulates lipopolysaccharide-induced TNFalpha inflammation
signaling in cultured cardiomyocytes. J Mol Cell Cardiol.
40:821–828. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Inoue I, Noji S, Awata T, et al:
Bezafibrate has an antioxidant effect: peroxisome
proliferator-activated receptor alpha is associated with
Cu2+, Zn2+-superoxide dismutase in the liver.
Life Sci. 63:135–144. 1998. View Article : Google Scholar
|
|
45
|
Marx N, Duez H, Fruchart JC and Staels B:
Peroxisome proliferator-activated receptors and atherogenesis:
regulators of gene expression in vascular cells. Circ Res.
94:1168–1178. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Marx N, Sukhova GK, et al: PPARalpha
activators inhibit cytokine-induced vascular cell adhesion
molecule-1 expression in human endothelial cells. Circulation.
99:3125–3131. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Bulhak AA, Jung C, Ostenson CG, et al:
PPARalpha activation protects the type 2 diabetic myocardium
against ischemia-reperfusion injury: involvement of the
PI3-Kinase/Akt and NO pathway. Am J Physiol Heart Circ Physiol.
296:H719–H727. 2009. View Article : Google Scholar : PubMed/NCBI
|