Introduction
Severe post-traumatic complications, such as
pyohemia and systemic inflammatory response syndrome (SIRS),
comprise the major cause of mortality in hospitals, with a
mortality rate of 30–50%. SIRS can eventually result in multiple
organ dysfunction syndrome (MODS) (1). In the later stages of severe trauma,
blood vessels throughout the body, but particularly small blood
vessels, have a low responsiveness to vasoactive drugs. As a
consequence, the blood pressure cannot be effectively improved; it
becomes difficult to enhance tissue perfusion; cells become subject
to oxygen deficit; the damage progressively worsens and the release
of inflammatory factors is increased, leading to a ‘waterfall
effect’. These events comprise the major pathological factors of
MODS (2,3).
A number of studies have shown that certain
cytokines that are intimately associated with inflammation, such as
endothelin-1 and Toll-like receptors, play an important role in the
development of organ dysfunction (4,5);
however, these results have only been evident in animal studies and
therefore cannot be used to generate a clinical index for the
diagnosis of MODS during its development in humans. Other studies
have found that serum atrial natriuretic peptide (ANP) and β-type
natriuretic peptide (BNP) levels exhibit marked increases in
numerous types of disease, including heart failure, acute lung
injury (ALI), septic shock, burns and electrical injury, and that
these increases are closely associated with the hemodynamic index
(6,7). Compared with traditional inflammatory
markers and trauma scoring systems, however, the correlation
between the levels of serum N-terminal peptide of pro-ANP
(NT-proANP) and N-terminal fragment of BNP (NT-proBNP), which are
used as indicators of the trauma-induced development of MODS, and
the hemodynamic index following severe trauma is rarely reported.
The aim of the present study, therefore, was to evaluate the
prognostic value of serum NT-proANP and NT-BNP in severe trauma
patients with MODS and to perform a correlation analysis between
these indicators and the hemodynamic index.
Materials and methods
Clinical data
One hundred and sixteen severe trauma patients, who
had been admitted to the Emergency Intensive Care Unit of the
General Hospital of Shenyang Military Region (Shenyang, China)
between January 2009 and December 2011, were examined. All the
necessary clinical tests were performed, including vital signs,
blood, urine and liver and kidney function tests and blood gas
analysis. In addition, all patients underwent central venous
catheterization, Pulse index Continuous Cardiac Output (PiCCO)
measurement (Pulsion Medical Systems SE, Munich, Germany),
electrocardiography, blood pressure and heart rate monitoring, and
blood oxygen saturation and blood gas analyses. The inclusion
criteria were as follows: i) No injury history; ii) injury severity
score (ISS), ≥16; iii) age, ≥18 years; iv) time interval between
trauma and admission, <90 h. In addition, patients meeting the
following criteria were excluded from the study: i) Mortality
within 24 h after trauma; ii) main diagnosis, cardiac trauma; iii)
intracranial hemorrhage; iv) heart, liver, kidney or endocrine
history. Following admission, the age, gender, cause of trauma and
medical history of the patients were recorded. The patients were
given 24 h fluid resuscitation and anti-inflammatory treatment, and
the aforementioned tests and observations, including 24-h urine
volume and PiCCO monitoring, were performed. This study was
approved by the ethics committee of the General Hospital of
Shenyang Military Region, and informed consent was obtained from
all patients or patient guardians.
Grouping method
The MODS score (Table
I) was calculated on admission, as well as 24, 48 and 72 h
after the injury. The patients were divided into two groups: Group
A (MODS scores ≤4 points over 2 days) and group B (MODS scores
>4 points).
 | Table I.Multiple organ dysfunction syndrome
scoring. |
Table I.
Multiple organ dysfunction syndrome
scoring.
| Body system | 0 | 1 | 2 | 3 | 4 |
|---|
| Respiratory system
(PaO2/FiO2) | >300 | 226–300 | 151–225 | 76–150 | ≤75 |
| Kidney system (Cr,
µmol/l) | ≤100 | 101–200 | 201–350 | 351–500 | >500 |
| Liver system
(bilirubin, µmol/l) | ≤20 | 21–60 | 61–120 | 121–240 | >240 |
| Cardiovascular system
(PARa) |
≤10.0 | 10.1–15.0 | 15.1–20.0 | 20.1–30.0 |
>30.0 |
| Coagulation system
(platelets, x109/l) | >120 | 81–120 | 51–80 | 21–50 | ≤20 |
| Nervous system
(Glasgow Coma Score) | 15 | 13–14 | 10–12 | 7–9 |
≤6 |
Testing indices
Venous blood (5 ml) was collected following
admission and 6, 12, 24, 48 and 72 h after the injury. Differences
in serum levels of NT-proANP and NT-proBNP were detected using a
rapid detector (Roche Diagnostics Gmbh, Mannheim, Germany). The
normal serum NT-proANP and NT-proBNP levels are <1,000 and
<100 pmol/l, respectively. The changes in the levels of
C-reactive protein (CRP), white blood cells (WBCs) and neutrophils
were detected and analyzed on admission (in 24 h). The acute
physiology and chronic health evaluation II (APACHE II) scores and
ISSs were collected 72 h after the injury. The hemodynamic
monitoring of the cardiac index (CI) was performed upon admission
and 24, 48, and 72 h after the injury using the PiCCO system.
Statistical analysis
SPSS software (version 15.0; SPSS, Inc., Chicago,
IL, USA) was used for the statistical analysis and the t-test was
used for the comparison between the two groups. The results are
presented as the mean ± standard deviation, and P<0.05 was
considered to indicate a statistically significant difference. In
the correlation analysis, P<0.05 was considered to indicate a
statistically significant linear correlation. The closer the
absolute value of the correlation coefficient (r) to 1, the
stronger its relevance.
Results
Basic patient characteristics
Out of the 116 examined patients, 26 were included
in the study; 16 were assigned to group A and 10 to group B. No
significant differences were found in the basic characteristics and
the ISSs between the two groups (P>0.05); by contrast, the
APACHE II score of the patients in group B was significantly higher
than that of the patients in group A (P<0.05) (Table II).
 | Table II.Basic patient characteristics and
clinical data 24 h after admission. |
Table II.
Basic patient characteristics and
clinical data 24 h after admission.
| Patient
characteristics | Group A, n=16 | Group B, n=10 | P-value |
|---|
| Males (%) | 67.5 | 75.7 | >0.05 |
| Age (years) |
43±12.9 |
51±14.3 | >0.05 |
| ISS | 31.9±8.3 |
39.2±10.1 | >0.05 |
| APACHE II score | 21.8±3.1 | 28.3±6.9 | <0.05 |
| CRP (mg/l) | 107.7±18.7 | 100.3±13.6 | >0.05 |
| WBCs
(x109/l) | 14.2±8.7 |
12.2±10.0 | >0.05 |
| Neutrophils (%) | 85.9±5.5 | 80.9±7.1 | >0.05 |
MODS score
The MODS scores were calculated on admission, as
well as 6, 12, 24, 48 and 72 h after the injury. The scores of the
patients in group B were significantly higher than those of the
patients in group A at the time of admission, as well as after 24,
48 (P<0.05) and 72 h (P<0.01) (Table III).
 | Table III.Multiple organ dysfunction syndrome
scores of the two groups. |
Table III.
Multiple organ dysfunction syndrome
scores of the two groups.
| Time-point | Group A, n=16 | Group B, n=10 | P-value |
|---|
| Admission | 3.1±0.6 | 4.8±0.8 | <0.05 |
| 24 h | 2.0±0.3 | 5.1±0.4 | <0.05 |
| 48 h | 1.8±0.3 | 5.9±0.8 | <0.05 |
| 72 h | 1.9±0.3 | 7.0±0.8 | <0.01 |
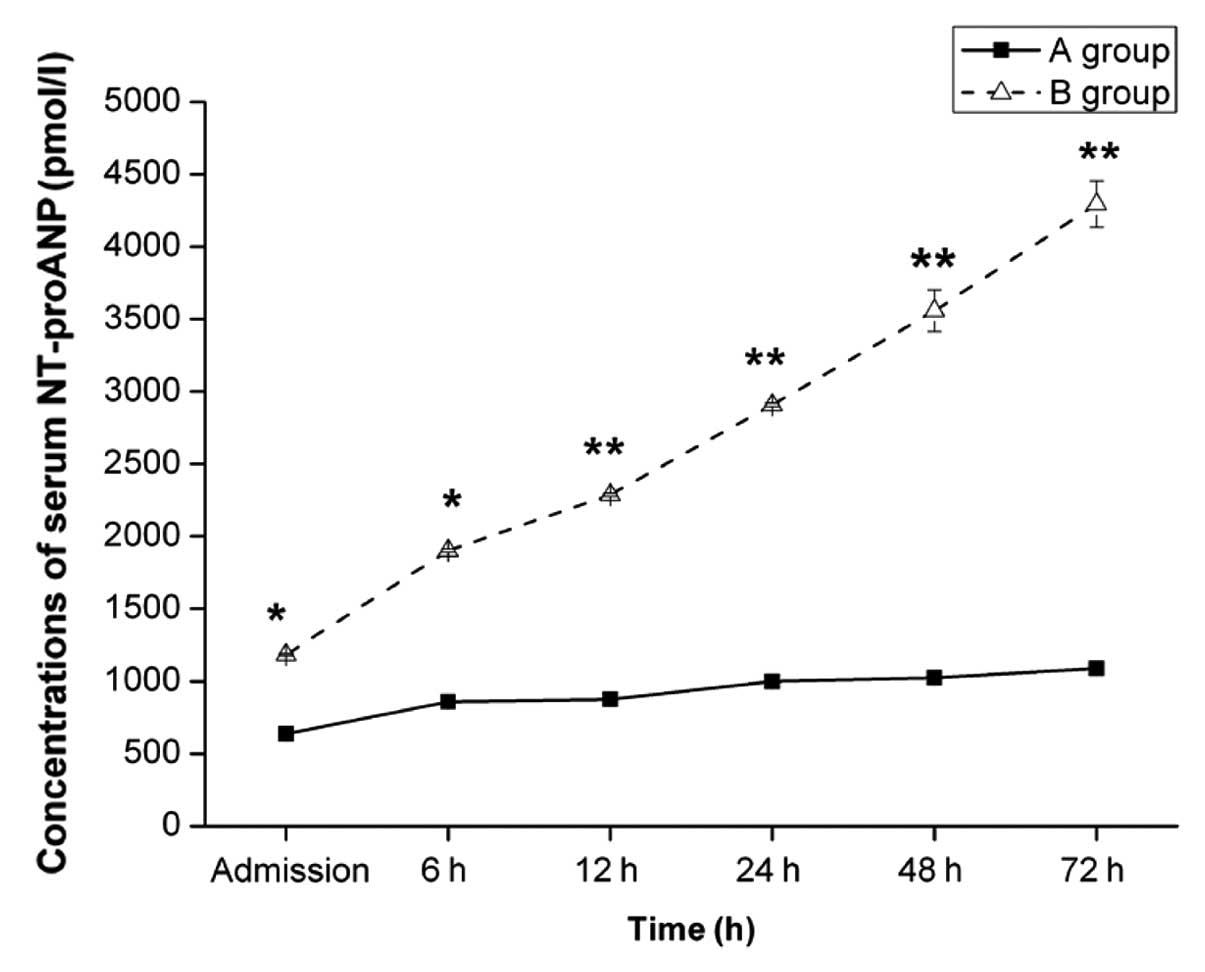
Concentrations of serum NT-proANP and
NT-proBNP
The concentrations of serum NT-proANP and NT-proBNP
were measured on admission, as well as 6, 12, 24, 48 and 72 h after
the injury. In group A, the concentrations of serum NT-proANP at
the respective time-points were 637.3±8.9, 857.4±5.8, 874.1±8.6,
999.3±11.0, 1,024.9±15.6 and 1,087.6±7.5 pmol/l, while in group B
they were 1,185.0±7.2, 1,901.9±11.0, 2,288.3±11.3, 2,908.2±12.0,
3,558.2±143.0 and 4,295.9±160.8 pmol/l. Twelve hours after
admission, the difference in the serum NT-proANP concentration
between the two groups was highly statistically significant
(P<0.01) (Fig. 1).
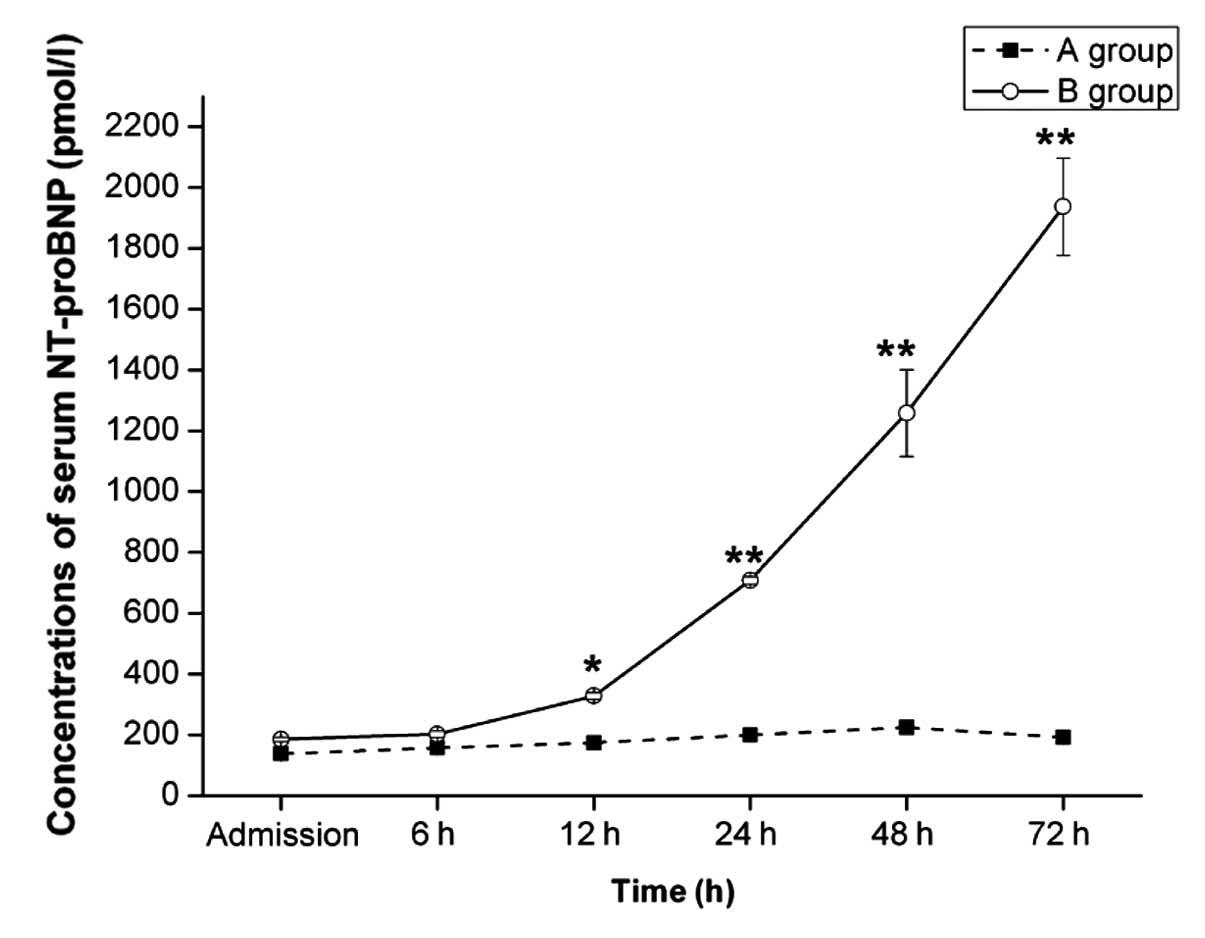
The concentrations of serum NT-proBNP in group A on
admission and at the 6-, 12-, 24-, 48- and 72-h time-points were
137.3±8.9, 157.4±5.8, 174.1±8.6, 199.3±11.0, 224.9±15.6 and
191.6±7.5 pmol/l, respectively, while in group B they were
185.0±7.2, 201.9±11.0, 328.3±11.3, 708.2±12.7, 1,258.2±143.0 and
1,936.9±160.8 pmol/l, respectively. At 24 h, the difference in the
serum NT-proBNP concentration between the two groups was highly
statistically significant (P<0.01) (Fig. 2).
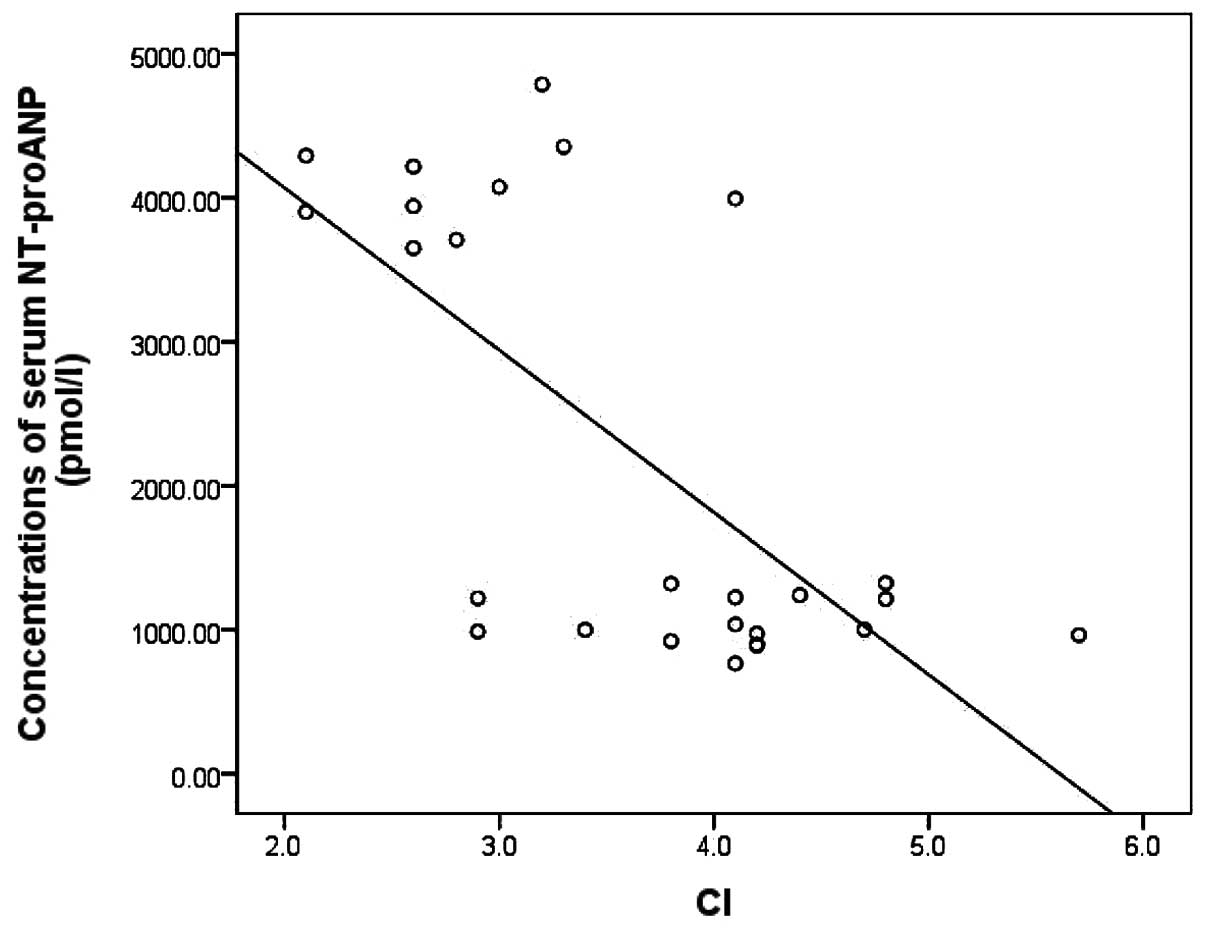
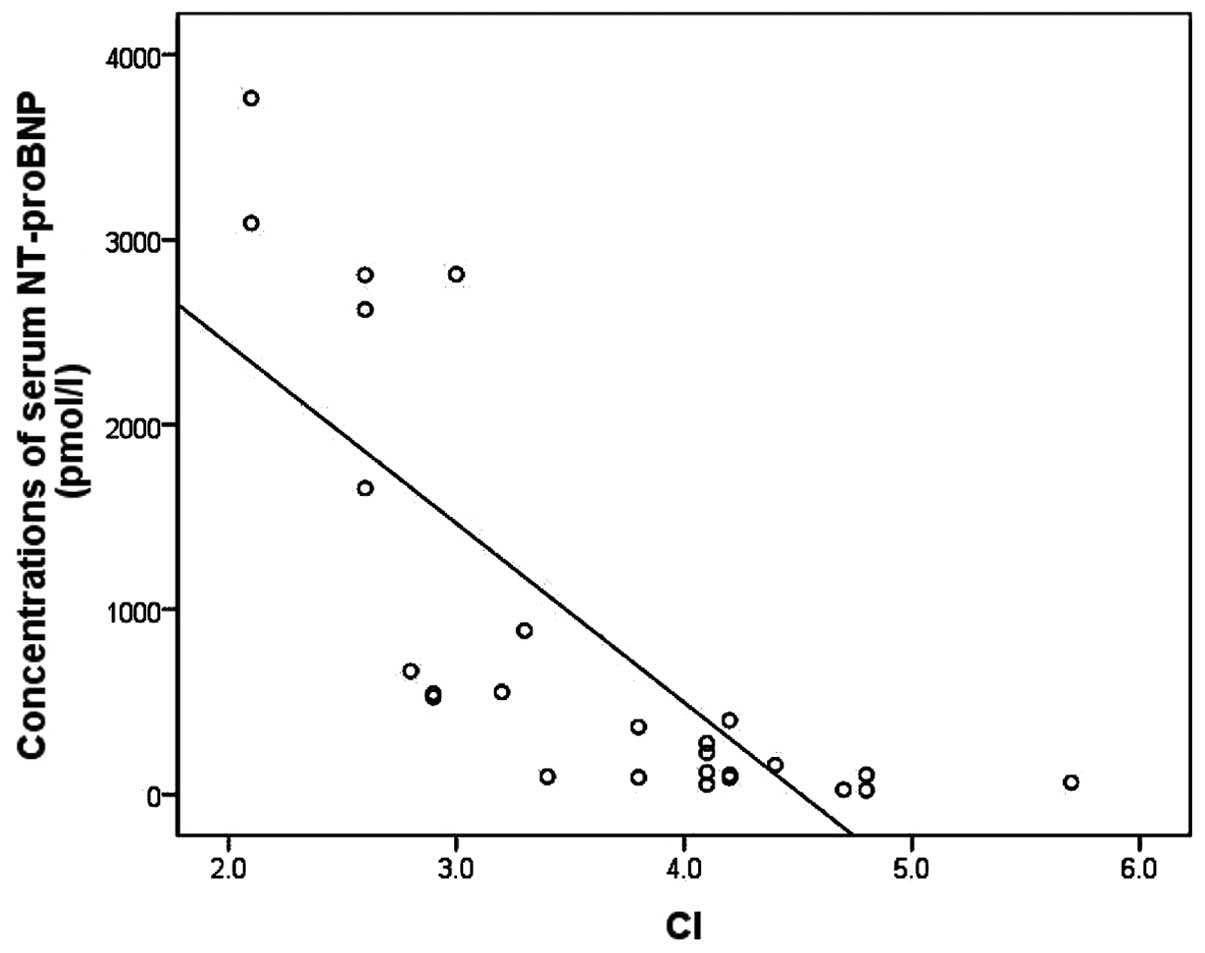
Correlation analysis between the serum
NT-proANP and NT-proBNP concentrations and the hemodynamic
index
Seventy-two hours after the injury, the correlations
between the serum NT-proANP and NT-proBNP concentrations and the CI
(Table IV) and systemic vascular
resistance index (SVRI) were analyzed. The SVRI was determined
directly using the PiCCO machine. An inverse correlation was
observed between the serum NT-proANP/NT-proBNP concentration and CI
(r=-0.679 and −0.772, respectively; P<0.001). The NT-proBNP
level showed a stronger correlation with the CI than the NT-proANP
level (Figs. 3 and 4).
 | Table IV.Cardiac index of the two groups. |
Table IV.
Cardiac index of the two groups.
| Time point | Group A (n=16) | Group B (n=10) |
|---|
| 6 h | 4.0±1.1 | 2.2±0.8 |
| 12 h | 3.6±0.5 | 2.0±0.5 |
| 24 h | 4.0±0.9 | 2.1±0.9 |
| 48 h | 3.8±0.8 | 1.9±1.1 |
| 72 h | 4.1±0.7 | 1.8±1.5 |
Discussion
Trauma is considered by some to be one of the worst
epidemics of the 20th century. The number of recorded trauma
victims has been unprecedented and the subsequent costs severe
(1). Despite the indisputable
development of medical science, traumatic injuries and
post-traumatic complications remain an important problem requiring
an urgent solution.
Natriuretic peptides, including ANP, BNP and C-type
natriuretic peptide, are cardiac hormones synthesized and secreted
by ventricular myocytes. The endocrine activity of these hormones
includes natriuresis, diuresis, dilation of blood vessels and
inhibition of the renin-angiotensin-aldosterone and sympathetic
nervous systems. The hormones are additionally known to play a
positive role in the preload and afterload reduction in patients
with heart failure (8). A previous
study has reported that the physiological effect of ANP is to
control arterial blood pressure by regulating the CI and SVR, while
BNP is involved in the acute inflammatory response to tissue damage
(9). In severe post-traumatic
complications, such as SIRS and MODS, the dysfunction in
microcirculatory vasoconstriction causes a fall in blood pressure,
which leads to little or no urine, dilation of the blood vessels
and inhibition of the sympathetic nervous system, which negatively
affects the state of the severe trauma patients (10).
Hoffmann and Brueckmann (11) measured the serum NT-proBNP level in
57 septic patients using ELISA and observed that the NT-proBNP
concentration was notably increased compared with the levels of the
controls. At an NT-proBNP concentration of >1,400 pmol/l, a
3.9-fold increase in mortality rate was found. NT-proBNP was
therefore established as an indicator of the severity of sepsis
(11). Kotanidou et al
(12) studied 233 patients in a
critical condition but with no heart disease and found that the
serum NT-proBNP concentration increased as the condition of the
patients was aggravated. A positive correlation was noted between
the NT-proBNP concentration and inflammatory factors; therefore,
the serum NT-proBNP concentration could be used independently to
calculate the prognosis of critical patients. Mitaka et al
(13) found that the serum NT-proBNP
level in patients with ALI was positively correlated with the SVRI
and pulmonary vascular resistance index and inversely correlated
with the CI. A positive correlation between NT-proANP and pulmonary
capillary wedge pressure showed that they had value for the
diagnosis of ALI. The present study found that the NT-proANP and
NT-proBNP levels of the 26 patients were higher than the normal
values. The serum peptide concentrations in group B were
significantly higher than those in group A and showed a sustained
increase up to the 72-h time-point. Both indicators were inversely
correlated with CI, which was consistent with the findings of
previous studies (8).
Norepinephrine, a β-receptor agonist, is the first
drug used to elevate blood pressure in cases of hypotension caused
by traumatic hemorrhagic shock. Since β-receptor activation can
increase the CI of severe trauma patients, the administration of
norepinephrine may affect the left ventricular ejection fraction of
the heart, altering left ventricular function. By contrast, the
development of ALI and ARDS as a result of oxygen deficit following
trauma leads to an increase in pulmonary vascular resistance, and
the use of blood pressure-elevating drugs will further increase
this resistance (8). The
administration of catecholamine drugs therefore increases right
ventricular afterload, as well as the concentrations of NT-proANP
and NT-proBNP (14).
Although the ISS and APACHE II have been suggested
to reflect the severity of the traumatic injuries and the
physiological function following trauma, in addition to acting as
predictors of post-traumatic complications and mortality, they have
not, to date, been shown to be capable of predicting the occurrence
of or enabling an early diagnosis of MODS. The results of the
present study revealed that the basic characteristics and ISSs of
the patients exhibited no significant differences; by contrast, the
APACHE II scores in the two groups of patients were significantly
different.
CRP, an acute-phase reactant synthesized in the
liver in response to tissue injury or severe infection, is a marker
of inflammation that is extensively used in the clinic. CRP has the
ability to activate the complement system and improve the activity
and movement of phagocytes. WBCs and neutrophils in the peripheral
blood are indexes for the diagnosis of SIRS (15). It is generally recognized that severe
trauma can produce an abundance of WBC chemotactic factors,
resulting in increases in the number and activation of WBCs and the
release of enzymes, such as elastase and matrix metalloproteinase.
This leads to cell death, damage to the structural organization and
organ dysfunction, and ultimately assists the development of MODS
(16). It has been shown that,
compared with CRP, the prognostic values of ANP and BNP in
diagnosing and predicting the mortality of septic patients is
greater (17). In the present study,
no significant differences in the levels of CRP, WBCs or
neutrophils were found between the two groups of patients
exhibiting different severities of MODS; this suggested that the
three indexes could not be used either to reflect the severity of
MODS or as independent prognostic markers. These results were
consistent with those of other studies (18).
In the past, body fluid states were monitored using
urine volume and central venous pressure measurements or
evaluations of hemodynamics using intrusive methods (Swan-Ganz
method), leading to an increased risk of recurrent trauma and
infection (19,20). The present study determined the fluid
load state of the body by performing continuous hemodynamic
monitoring using the PiCCO system. Point-of-care testing is a
relatively new concept in patient assessment. Point-of-care (or
bedside) testing is defined as medical testing at or near the site
of patient care. These are simple medical blood tests which may be
performed at the bedside. Through the use of this rapid, simple,
convenient and economic testing method, doctors can monitor the
changes in serum NT-proANP and NT-proBNP levels in time and combine
these changes with hemodynamic data in order to improve the
diagnostic and therapeutic decisions for severe trauma
patients.
In conclusion, this study has demonstrated that
serum NT-proANP and NT-proBNP levels are closely correlated with
the CI. Compared with other traditional inflammatory markers,
NT-proANP and NT-proBNP are superior prognostic indicators for the
development of MODS in severe trauma patients.
References
|
1
|
Brongel L: Guidelines for severe multiple
and multiorgan traumatic injuries. Przegl Lek. 60:(60 Suppl 7).
56–62. 2003.(In Polish). PubMed/NCBI
|
|
2
|
Zweifach BW, Benacerraf B and Thomas L:
The relationship between the vascular manifestations of shock
produced by endotoxin, trauma, and hemorrhage. II. The possible
role of the reticulo-endothelial system in resistance to each type
of shock. J Exp Med. 106:403–414. 1957. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zweifach BW and Thomas L: The relationship
between the vascular manifestations of shock produced by endotoxin,
trauma, and hemorrhage. I. Certain similarities between the
reactions in normal and endotoxin-tolerant rats. J Exp Med.
106:385–401. 1957. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Freeman BD, Machado FS, Tanowitz HB and
Desruisseaux MS: Endothelin-1 and its role in the pathogenesis of
infectious diseases. Life Sci. 118:110–119. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Li P, Guo Y, Bledsoe G, Yang ZR, Fan H,
Chao L and Chao J: Kallistatin treatment attenuates lethality and
organ injury in mouse models of established sepsis. Crit Care.
19:2002015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Determann RM, Royakkers AA, Schaefers J,
de Boer AM, Binnekade JM, van Straalen JP and Schultz MJ: Serum
levels of N-terminal proB-type natriuretic peptide in mechanically
ventilated critically ill patients - Relation to tidal volume size
and development of acute respiratory distress syndrome. BMC Pulm
Med. 13:422013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Papanikolaou J, Makris D, Mpaka M, Palli
E, Zygoulis P and Zakynthinos E: New insights into the mechanisms
involved in B-type natriuretic peptide elevation and its prognostic
value in septic patients. Crit Care. 18:R942014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chopra S, Cherian D, Verghese PP and Jacob
JJ: Physiology and clinical significance of natriuretic hormones.
Indian J Endocrinol Metab. 17:83–90. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Siemiatkowski A and Jabłonowska A:
Natriuretic peptides - relevance in intensive care. Anestezjol
Intens Ter. 40:96–102. 2008.(In Polish). PubMed/NCBI
|
|
10
|
Roger F Shere-Wolfe, Samuel M Galvagno Jr,
Thomas E Grissom, et al: Critical care considerations in the
management of the trauma patient following initial resuscitation.
Scand J Trauma Resusc Emerg Med. 20:682012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hoffmann U and Brueckmann M: A new
language of natriuretic peptides in sepsis? Crit Care Med.
36:2686–2687. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kotanidou A, Karsaliakos P, Tzanela M, et
al: Prognostic importance of increased plasma amino-terminal
pro-brain natriuretic peptide levels in a large noncardiac, general
intensive care unit population. Shock. 31:342–347. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mitaka C, Hirata Y, Nagura T, et al:
Increased plasma concentrations of brain natriuretic peptide in
patients with acute lung injury. J Crit Care. 12:66–71. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Behnke BJ, Zawieja DC, Gashev AA, et al:
Diminished mesenteric vaso- and venoconstriction and elevated
plasma ANP and BNP with simulated microgravity. J Appl Physiol
(1985). 104:1273–1280. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Castelli GP, Pognani C, Cita M, et al:
Procalcitonin, C-reactive protein, white blood cells and SOFA score
in ICU: Diagnosis and monitoring of sepsis. Minerva Anestesiol.
72:69–80. 2006.PubMed/NCBI
|
|
16
|
Barati M, Alinejad F, Bahar MA, et al:
Comparison of WBC, ESR, CRP and PCT serum levels in septic and
non-septic burn cases. Burns. 34:770–774. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yucel T, Memiş D, Karamanlioglu B, et al:
The prognostic value of atrial and brain natriuretic peptides,
troponin I and C-reactive protein in patients with sepsis. Exp Clin
Cardiol. 13:183–188. 2008.PubMed/NCBI
|
|
18
|
Yucel T, Memiş D, Karamanlioglu B, Süt N
and Yuksel M: The prognostic value of atrial and brain natriuretic
peptides, troponin I and C-reactive protein in patients with
sepsis. Exp Clin Cardiol. 13:183–188. 2008.PubMed/NCBI
|
|
19
|
Konarzewski W: Pulmonary artery
catheterisation. Pulmonary artery catheters should be banned from
intensive care units. BMJ. 313:13281996. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Simini B: Pulmonary artery catheters in
intensive care. Lancet. 366:435–436. 2005. View Article : Google Scholar : PubMed/NCBI
|