Introduction
Invasive fungal infections are a considerable cause
of morbidity, mortality, increased hospital stay durations, and
high health care costs in critically ill or immunocompromised
children (1–4). The majority of invasive fungal
infections in children occur in a hospital setting, and the
majority of infections are caused by Candida species
(1,5). In addition to the presence of
Candida species in the blood (candidemia), Candida
infections can disseminate to each main organ, including the brain,
lung, liver, heart, kidneys, eyes and spleen (2,3). As
neonates have immature specific and nonspecific immune functions,
they are more vulnerable to invasion by Candida species
compared with adults and children. The signs and symptoms of
Candida infection are severe and may resemble sepsis
syndrome (2,4), so early diagnosis is crucial, although
it remains challenging (6,7). Therefore, the aim of the present study
was to summarize the clinical characteristics of candidemia in
neonates, and determine whether specific risk factors may be
identified to aid the selection of patients who are more likely to
develop candidemia. Understanding the risk factors, clinical
features and complications affecting the prognosis of candidemia in
the neonatal period may help pediatricians to improve their
protective medical measures and more effectively treat neonatal
candidemia.
In addition, gastrointestinal dysfunction is common
in neonates with congenital gastrointestinal dysfunction (such as
gastrointestinal atresia, stenosis, duplication and malrotation)
and gastrointestinal diseases (such as abdominal infection,
necrotizing enterocolitis, intestinal obstruction, gastrointestinal
perforation and meconium peritonitis). These individuals are a
particularly susceptible population for candidemia, as they are
often confronted with long-term fasting, and are more likely to
undergo surgery and receive intravenous nutrition. Therefore in the
present study, the differences in the symptoms, risk factors and
prognosis for neonatal candidemia with or without gastrointestinal
dysfunction were compared.
Materials and methods
Study design
The study was conducted at the Affiliated Children's
Hospital of the Capital Institute of Pediatrics (Beijing, China),
which is a 400-bed tertiary-level teaching hospital. The neonatal
intensive care unit (NICU) is a nine-bed unit, which has between
750 and 800 admissions each year.
Patients
Candidemia was diagnosed through the use of blood
cultures that yielded Candida species Sabouraud Dextrose
Agar (SDA) medium (Jiangmen Jinzhang Science and Technology
Development Co., Ltd., Tianjin, China) was used to identify the
subspecies of Candida in neonates hospitalized in the NICU.
The blood samples were collected from right and left femoral vein,
or from right jugular vein and right femoral vein simultaneously.
Case patients were identified through the records of the clinical
microbiology laboratory at the Affiliated Children's Hospital of
the Capital Institute of Pediatrics. The retrospective study
included patients in the NICU who had positive cultures for
Candida species, admitted between January 1, 2006 and
December 31, 2010. Patients with positive results of Candida
species from two cultural samples were allocated to the candidemia
group, while individuals with negative results were placed in the
non-candidemia group. The clinical characteristics, prognosis and
previously identified risk factors for the two groups were
recorded. The risk factors included gastrointestinal dysfunctions,
the administration of antibiotics prior to the occurrence of
candidemia, the presence of a central venous cannula, parenteral
nutrition, gastrointestinal and secondary gastrointestinal surgery,
repeated tracheal intubation and the occurrence of maternal
candidal vaginitis. The outcomes and development situation at 6
months after discharge from hospital of the patient were also
followed-up. The study was conducted in accordance with the
Declaration of Helsinki and with approval from the Ethics Committee
of the Affiliated Children's Hospital of the Capital Institute of
Pediatrics. Written informed consent was obtained from parents or
guardians of the participants. The patients were divided into
gastrointestinal dysfunction and non-gastrointestinal dysfunction
group, according to whether the patients were with or without
congenital gastrointestinal dysfunction (gastrointestinal atresia,
stenosis, duplication, malrotation, etc.) and gastrointestinal
diseases (abdominal infection, necrotizing enterocolitis,
intestinal obstruction, gastrointestinal perforation, meconium
peritonitis, etc.).
Control patients
Control patients for the study were selected through
the use of unit-specific patient admission databases. To increase
the statistical efficiency, the individuals included in the
non-candidemia and candidemia groups exhibited no statistically
significant differences with regard to age and gender.
Statistical analysis
Categorical data were analyzed using the
χ2 test, exact probability test and t-test. The
Risk factors significantly related to candidemia according to the
univariate analyses subsequently underwent multivariate analysis to
identify the predictors following adjustment for possible
comorbidities. P<0.05 (two-tailed) was considered to indicate a
statistically significant difference. Statistical analyses were
performed using GraphPad Prism software, version 5 (GraphPad
Software, Inc., San Diego, CA, USA). Patient age, length of
hospital stay, length of ICU stay and treatment duration are
presented as median. The enumeration data are expressed as
percentage, relative risk, odds ratio and confidence interval.
Results
General information
During the study period, 19 case patients with
candidemia were identified (male, 13; female, 6), while 21 patients
(male, 14; female, 7) were included in the control group. The
patients were aged between 1 and 28 days (median age, 13 days).
Candidemia was as a result of Candida albicans in 10
patients (52.63%), and due to non-Candida albicans species
in 9 patients (47.37%). The shortest hospitalization duration was
12 days, while the longest duration was 124 days (median duration,
28 days). The shortest duration in the ICU was 4 days and the
longest was 49 days (median, 12 days). The shortest treatment
duration was 0.42 weeks, while the longest was 8 weeks (median, 4
weeks). In total, 5/19 patients (26.32%) ultimately succumbed to
their illness, of which three mortalities occurred in hospital
(15.71%) and two mortalities occurred within 90 days (10.52%).
Clinical manifestations
Clinical manifestations of the candidemia group were
more severe compared with the non-candidemia group (Table I). The results revealed that the
symptoms of fever, abdominal pain, vomit, edema, serous effusion,
tetter, thrush, shock, gastrointestinal and pulmonary hemorrhage
and multiple organ failure were significantly more common in the
candidemia group when compared with the non-candidemia group. Among
the accompanying examination results, the occurrence of
procalcitonin (PCT) levels of >2 ng/ml, hemoglobin levels of
<10 g/l, C-reactive protein (CRP) levels of >50 mg/l,
thrombocytopenia, liver dysfunction, hypoproteinemia and pathogenic
bloodstream infections other than Candida were significantly
higher in the candidemia group compared with the non-candidemia
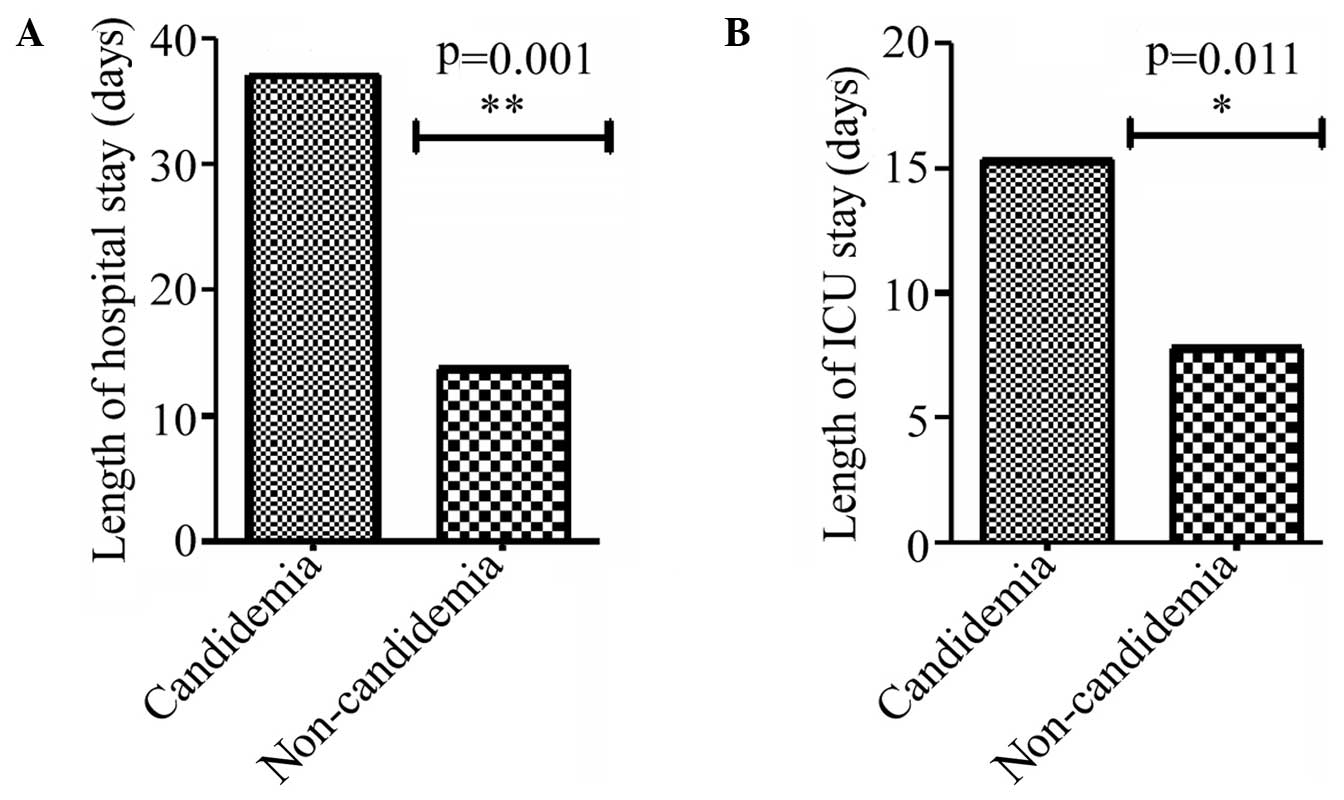
group. In addition, the length of hospital stay and ICU stay in the
candidemia group was significantly longer compared with the
non-candidemia group (Fig. 1).
 | Table I.Characteristics of the patients with
or without Candida-positive cultures. |
Table I.
Characteristics of the patients with
or without Candida-positive cultures.
| Classification | Candidemia, n
(%) | Non-candidemia, n
(%) | P-value | RR (95% CI) | Odds ratio (95%
CI) |
|---|
| Clinical feature |
|
|
|
|
|
|
Fever | 13/19 (68.42) | 3/21 (14.28) | 0.0009c | 4.78
(1.61–14.27) | 13.00
(2.73–61.81) |
| Abdominal
distention | 13/19 (68.42) | 2/21 (9.52) | 0.0001c | 7.18
(1.86–27.81) | 20.58
(3.58–114.40) |
|
Vomiting | 12/19 (63.15) | 2/21 (9.52) | 0.0004c | 6.63
(1.70–25.91) | 16.29
(2.89–91.87) |
|
Edema | 11/19 (57.89) | 4/21 (9.52) | 0.0211a | 3.04 (1.16–7.95) | 5.84
(1.41–24.18) |
| Serous
effusion | 8/19 (42.10) | 2/21 (9.52) | 0.0281a | 4.42
(1.07–18.29) | 6.91
(1.24–38.53) |
|
Tetter | 8/19 (42.10) | 1/21 (4.76) | 0.0072b | 8.84
(1.22–64.33) | 14.55
(1.60–132.00) |
|
Thrush | 8/19 (42.01) | 0/21 (0.00) | 0.0010c |
| 31.78
(1.68–602.00) |
| GI
hemorrhage | 11/19 (57.89) | 1/21 (4.76) | 0.0003c | 12.16
(1.73–85.86) | 27.50
(3.03–249.60) |
|
Pneumorrhagia | 5/19 (26.31) | 0/21 (0.00) | 0.0177a |
| 16.31
(0.84–318.40) |
|
Shock | 10/19 (52.63) | 2/21 (9.52) | 0.005b | 5.52
(1.38–22.10) | 10.56
(1.90–58.55) |
| Multiple
organ failure | 9/19 (47.36) | 1/21 (4.76) | 0.0028b | 9.94
(1.39–71.41) | 18.00
(1.99–162.70) |
| Accompanying
examination |
|
|
|
|
|
|
Leucocytes of
>20×109/l | 11/19 (57.89) | 4/21 (19.05) | 0.0211a | 3.04 (1.16–7.95) | 5.84
(1.41–24.18) |
| Hb of
<10 g/l | 14/19 (73.68) | 2/21 (9.52) |
<0.0001c | 7.73
(2.01–29.72) | 26.60
(4.49–157.7) |
|
Thrombocytopenia | 14/19 (73.68) | 3/21 (14.28) | 0.0003c | 5.16
(1.75–15.22) | 16.80
(3.41–82.64) |
| PCT of
>2 ng/ml | 15/19 (78.94) | 7/21 (33.3) | 0.0051b | 2.37 (1.24–4.53) | 7.50
(1.78–31.29) |
| CRP of
>50 mg/l | 14/19 (73.68) | 2/21 (9.52) |
<0.0001c | 7.73
(2.01–29.72) | 26.60
(4.49–157.70) |
| Liver
dysfunction | 14/19 (73.68) | 3/21 (14.28) | 0.0003c | 5.16
(1.75–15.22) | 16.80
(3.41–82.64) |
|
Hypoproteinemia | 13/19 (68.42) | 4/21 (19.05) | 0.0109a | 3.25
(1.27–8.35) | 6.91
(1.70–28.04) |
| Other
pathogens |
|
|
|
|
|
|
Bloodstream infections | 10/19 (52.63) | 2/21 (9.52) | 0.005b | 5.52
(1.38–22.10) | 10.56
(1.90–58.55) |
Risk factors
Comparisons between the candidemia and
non-candidemia groups were conducted in terms of the presence of an
underlying disease, risk factors and prognosis (Table II). A gastrointestinal dysfunction
was the most common underlying disease in the patients from the
candidemia group. According to the univariate analysis, the
significant (P≤0.05) risk factors prior to the occurrence of
candidemia in the candidemia group were antibiotic administration
for >2 weeks (P<0.0001), the use of more than three types of
antibiotic (P=0.0019), the presence of a central venous cannula
(P<0.0001), the use of parenteral nutrition for >2 weeks
(P<0.0001), gastrointestinal surgery (P=0.0123), repeated
tracheal intubation (P=0.0027), secondary gastrointestinal surgery
and maternal candidal vaginitis (P=0.0424). When the prognosis of
the two groups was compared, the proportion of patients with growth
retardation 6 months after hospital discharge was significantly
higher in the candidemia group (P=0.001). However, there was no
statistically significant difference with regard to the hospital
mortality rate and 90-day mortality rate when comparing the two
groups. Based on the forward step-wise multivariate regression
analysis, the use of antibiotics for >2 weeks, maternal candidal
vaginitis, repeated tracheal intubation and the use of glycopeptide
antibiotics were demonstrated to be predictors of candidemia.
 | Table II.Differences in the prognosis and risk
factors of patients with or without Candida-positive
cultures. |
Table II.
Differences in the prognosis and risk
factors of patients with or without Candida-positive
cultures.
| Factors | Candidemia, n | Non-candidemia,
n | P-value | RR (95% CI) | Odds ratio (95%
CI) |
|---|
| Underlying
disease |
|
|
|
|
|
| GI
dysfunctions | 11/19 | 2/21 | 0.0001b | 2.86
(1.537–5.34) | 13.06
(2.34–72.85) |
| Risk factor |
|
|
|
|
|
| Prior
use of antibiotics >2 weeks | 17/19 | 1/21 |
<0.0001c | 10.39
(2.76–39.14) | 170
(14.00–2044) |
| >3
types of antibiotics | 11/19 | 2/21 | 0.0019b | 2.86
(1.53–5.34) | 13.06
(2.34–72.85) |
|
Carbapenems | 13/19 | 3/21 | 0.0009c | 3.250
(1.56–6.758) | 13
(2.734–61.81) |
|
Glycopeptides | 10/19 | 1/21 | 0.001b | 2.93
(1.65–5.20) | 22.22
(2.46–200.90) |
|
Nitroimidazoles | 8/19 | 1/21 | 0.0072b | 2.51
(1.48–4.25) | 14.55
(1.60–132.00) |
| Central
venous cannula | 16/19 | 2/21 |
<0.0001c | 6.52
(2.25–18.90) | 50.67
(7.51–341.90) |
|
Parenteral nutrition >2
weeks | 16/19 | 2/21 |
<0.0001c | 6.52
(2.25–18.90) | 50.67
(7.51–341.90) |
| GI
surgery | 9/19 | 2/21 | 0.0123a | 2.37
(1.33–4.21) | 8.55
(1.54–47.43) |
|
Repeated endotracheal
intubation | 7/19 | 0/21 | 0.0027b | 2.75
(1.75–4.32) | 25.80
(1.35–491.50) |
|
Secondary GI surgery | 7/19 | 0/21 | 0.0027b | 2.75
(1.75–4.32) | 25.80
(1.35–491.50) |
|
Maternal candidal
vaginitis | 4/19 | 0/21 | 0.0424a | 2.40
(1.63–3.53) | 12.48
(0.62–249.40) |
| Prognosis |
|
|
|
|
|
|
Hospital mortality | 3/19 | 0/21 | 0.098 |
| 9.1
(0.43–189.3) |
| 90-day
mortality | 5/19 | 1/21 | 0.056 | 5.53
(0.71–43.18) | 7.14
(0.75–68.01) |
| Growth
retardation at 6 months after discharge | 11/19 | 1/21 | 0.001b | 2.93
(1.65–5.20) | 22.22
(2.46–200.90) |
Gastrointestinal dysfunction
In addition, differences in the symptoms, prognosis
and risk factors of neonates with candidemia with or without
gastrointestinal dysfunction were compared (Table III). Overall, 57.9% of the patients
with candidemia exhibited gastrointestinal dysfunction. The
incidence rates of shock, malnutrition, PCT levels of >2 ng/ml
and the presence of other pathogenic bloodstream infections were
significantly higher in the gastrointestinal dysfunction group,
whereas the incidence of premature birth and maternal candidal
vaginitis was significantly higher in the non-gastrointestinal
dysfunction group. The differences between the two groups with
regard to the incidence rates of central venous catheterization,
intravenous nutrition, gastrointestinal surgery, repeated
intubation, secondary gastrointestinal surgery and nitroimidazole
and glycopeptide antibiotic administration were statistically
significant (P<0.05). When comparing the prognosis of the two
groups, who were followed-up for 6 months, all the patients with
gastrointestinal dysfunction suffered growth retardation. A total
of 72.2% of the patients in the gastrointestinal dysfunction group
received mechanical ventilation, whereas 25% of the patients in the
non-gastrointestinal dysfunction group received mechanical
ventilation (P=0.0397). In addition, a total of 63.63% of patients
in the gastrointestinal dysfunction group, compared with 12.5% of
patients in the non-gastrointestinal dysfunction group, were
effectively treated by removal of the central venous cannula, and
the difference was statistically significant (P=0.0258). However,
there was no statistically significant difference with regard to
the efficacy of fluconazole, the utilization rate of human
immunoglobulin, albumin or packed red cells between the two
groups.
 | Table III.Differences in the symptoms,
prognosis and risk factors of candidemia patients with or without
GI dysfunctions. |
Table III.
Differences in the symptoms,
prognosis and risk factors of candidemia patients with or without
GI dysfunctions.
| Factors | GI dysfunctions,
n | No GI dysfunctions,
n | χ2 | P-value | Odds ratio (95%
CI) |
|---|
| Underlying
diseases |
|
|
|
|
|
|
Premature birth | 2/11 | 5/8 | 3.909 | 0.048a | 0.13
(0.02–1.09) |
| Symptom |
|
|
|
|
|
|
Malnutrition | 8/11 | 2/8 | 4.232 | 0.0397a | 8.00
(1.00–64.00) |
|
Shock | 8/11 | 2/8 | 4.232 | 0.0397a | 8.00
(1.00–64.00) |
| Accessory
examination |
|
|
|
|
|
| PCT of
>2 ng/ml | 10/11 | 4/8 | 3.997 | 0.0456a | 10.00
(0.84–119.40) |
| Other
pathogenic bloodstream infections | 9/11 | 3/8 | 3.909 | 0.048a | 7.50
(0.921–61.08) |
| Risk factor |
|
|
|
|
|
|
Parenteral nutrition | 11/11 | 5/8 | 4.868 | 0.027a | 0.07
(0.00–1.57) |
| Central
venous catheter | 11/11 | 5/8 | 4.868 | 0.027a | 14.64
(0.64–335.90) |
| GI
surgery | 9/11 | 0/8 | 12.44 | 0.0004c | 64.60
(2.70–1546.0) |
|
Secondary GI surgery | 5/11 | 0/8 | 4.935 | 0.0263a | 14.38
(0.67–310.10) |
|
Repeated endotracheal
intubation | 7/11 | 1/8 | 4.958 | 0.0258a | 12.25
(1.08–139.10) |
|
Nitroimidazoles | 8/11 | 0/8 | 10.05 | 0.0015b | 41.29
(1.83–928.20) |
|
Glycopeptides | 8/11 | 2/8 | 4.232 | 0.0397a | 8.00
(1.00–64.00) |
|
Maternal candidal
vaginitis | 1/11 | 4/8 | 3.997 | 0.0456a | 0.10
(0.00–1.19) |
| Prognosis |
|
|
|
|
|
| Growth
retardation at 6 months after discharge | 9/9 | 2/7 | 9.351 | 0.0022b | 0.024
(0.00–0.59) |
| Treatment |
|
|
|
|
|
|
Mechanical ventilation | 8/11 | 2/8 | 4.232 | 0.0397a | 8.00
(1.00–64.00) |
| Removal
of the central venous catheter | 8/11 | 0/8 | 10.05 | 0.0015b | 41.29
(1.84–928.60) |
Discussion
The present study is a case-controlled study that
examined the clinical features and risk factors for candidemia
among neonates. Non-specific symptoms, such as fever, abdominal
pain, vomiting, edema, serous effusion and tetter, were found to be
the main clinical manifestations of candidemia. In addition, in
certain cases, thrush may be a specific sign for neonates with
severe candidemia. The high rates of shock, gastrointestinal and
pulmonary hemorrhage and multiple organ failure in the patients
with candidemia indicated that the neonates with candidemia were in
a more severe clinical situation compared with the neonates without
candidemia. Candida species can affect neonates more easily
compared with adults and children, and usually damage multiple
organ systems with increasing PCT and CRP levels when bloodstream
infections occurred. As a result, patients with candidemia require
longer hospital and ICU durations and expensive medical
treatments.
Previous studies that have described risk factors
for neonatal candidemia, in particular premature neonates. Saiman
et al (8) reported limited
data regarding the risk factors for candidemia, including
gestational age of <32 weeks, 5-min Apgar score of <5, shock,
disseminated intravascular coagulopathy, prior use of intralipids,
parenteral nutrition, central venous catheters, H2
blockers, intubation and length of hospital stay of >7 days
prior to candidemia. Yu et al (9) reported that the predominant risk
factors for invasive fungal infections were third-generation
cephalosporin administration, peripherally inserted central venous
catheters, intubation of >6 days, any prior abdominal surgery
and neutropenia (<1.5×109 cells/l) during the first
week of life. Furthermore, Pasqualotto et al (10) demonstrated that a failure to remove
the central venous catheter was an independent risk factor for
early mortality among pediatric patients with candidemia.
Therefore, a number of risk factors for candidiasis in neonates
have been reported, which were also observed in the patients
included in the present study. Although the univariate analysis
performed in the current study indicated that parenteral nutrition,
tracheal intubation and central venous catheters were associated
with candidemia, these associations were not statistically
significant in the multivariate model. In the present study,
independent risk factors for developing candidemia were evaluated.
The results demonstrated that prior use of antibiotics for >2
weeks, maternal candidal vaginitis, repeated gastrointestinal
surgery and the prior use of glycopeptide antibiotics were
associated with the development of candidemia in neonates.
A number of previous studies have investigated the
association between antibiotic use and candidemia (11–13). In
addition, numerous animal studies have demonstrated that normal
anaerobic gastrointestinal flora provide an important defense
mechanism against infection by inhibiting the growth of potentially
pathogenic organisms (14–16). The translocation of yeast across an
intact gastrointestinal mucosa via persorption has been
demonstrated following the injection of Candida suspensions
into a normal gastrointestinal tract (17). However, the presence of anaerobic
bacteria in the gut has been clearly established to inhibit the
overgrowth of Candida species (18,19). A
previous study (7) reported that
administration of antimicrobials with activity against the
anaerobic gastrointestinal flora is associated with the development
of candidemia. Furthermore, the present analysis revealed that the
administration of glycopeptide antibiotics was an independent risk
factor for candidemia, which was not unexpected since glycopeptide
antibiotics possess N-acetyl glucosamine and mannose
oligosaccharides capable of binding to mannnose-binding lectin
which may decrease the clearance of significant pathogens such as
yeast (20). The normal
gastrointestinal barrier serves a crucial function in preventing
Candida species colonizing the gastrointestinal tract and
spreading into the blood. Therefore, the destruction of the
gastrointestinal barrier by gastrointestinal surgery was a crucial
risk factors for candidemia.
Additionally, differences in the symptoms, prognosis
and risk factors among the patients in the candidemia group with
and without gastrointestinal dysfunctions were compared. Infants
with gastrointestinal diseases or malformations are more likely to
require gastrointestinal surgery, which may result in an increased
risk of candidemia due to the increased application of parenteral
nutrition, antibiotic administration and a central venous catheter.
To a certain extent, repeated tracheal intubation is associated
with secondary gastrointestinal surgery. Prematurity has been
reported as an important risk factor for neonatal candidemia
(21). The results of the present
study indicated that premature birth is a risk factor for
candidemia in neonates without a gastrointestinal dysfunction.
Newborns may have a higher risk of developing invasive candidiasis
if their mother suffered from candidal vaginitis during perinatal
period. Research has shown that isolates of Candida in the
blood stream, the oral cavity of neonates and the vagina of the
mother share a common genotype, which provides direct evidence of
the association between congenital candidiasis in the neonate and
candidal vaginitis in the mother (22). Furthermore, the present study
observed that 4 newborns with candidemia had been associated with
maternal candidal vaginitis during the perinatal period, which is
rarely reported.
With regard to prognosis, the results of the present
study demonstrate that the incidence of growth retardation was
higher in candidemia group compared with the non-candidemia group
at 6 months after discharge from hospital, particularly in the
gastrointestinal dysfunction group. A disorder in gastrointestinal
function may be the primary cause of long-term malnutrition and
growth retardation; therefore, the long-term prognosis of such
infants should be followed-up closely.
In conclusion, candidemia threaten the life of
neonates, in addition to influencing the early development of
survivors. The clinical manifestations of candidemia usually
involve multiple systems, and may resemble septic shock. Prior
administration of antibiotics for >2 weeks, the use of
glycopeptide antibiotics, maternal candidal vaginitis and secondary
gastrointestinal surgery were identified as predictors of neonatal
candidemia by multivariate analysis. In addition, gastrointestinal
dysfunction appeared to be a crucial factor for the development of
candidemia during the neonatal period. Further studies are required
to identify additional risk factors for candidemia in critically
ill neonates.
References
|
1
|
Maródi L and Johnston RB Jr: Invasive
Candida species disease in infants and children: Occurrence,
risk factors, management and innate host defense mechanisms. Curr
Opin Pediatr. 19:693–697. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zaoutis T: Candidemia in children. Curr
Med Res Opin. 26:1761–1768. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zaoutis TE, Argon J, Chu J, Berlin JA,
Walsh TJ and Feudtner C: The epidemiology and attributable outcomes
of candidemia in adults and children hospitalized in the United
States: A propensity analysis. Clin Infect Dis. 41:1232–1239. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cugno C and Cesaro S: Epidemiology, risk
factors and therapy of candidemia in pediatric hematological
patients. Pediatr Rep. 4:e92012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Filioti J, Spiroglou K, Panteliadis CP and
Roilides E: Invasive candidiasis in pediatric intensive care
patients: Epidemiology, risk factors, management and outcome.
Intensive Care Med. 33:1272–1283. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ariff S, Saleem AF, Soofi SB and Sajjad R:
Clinical spectrum and outcomes of neonatal candidiasis in a
tertiary care hospital in Karachi, Pakistan. J Infect Dev Ctries.
5:216–223. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zaoutis TE, Prasad PA, Localio AR, et al:
Risk factors and predictors for candidemia in pediatric intensive
care unit patients: Implications for prevention. Clin Infect Dis.
51:e38–e45. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Saiman L, Ludington E, Pfaller M, et al:
Risk factors for candidemia in neonatal intensive care unit
patients. The National Epidemiology of Mycosis Survey study group.
Pediatr Infect Dis J. 19:319–324. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yu Y, Du L, Yuan T, et al: Risk factors
and clinical analysis for invasive fungal infection in neonatal
intensive care unit patients. Am J Perinatol. 30:589–594. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Pasqualotto AC, de Moraes AB, Zanini RR
and Severo LC: Analysis of independent risk factors for death among
pediatric patients with candidemia and a central venous catheter in
place. Infect Control Hosp Epidemiol. 28:799–804. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Spiliopoulou A, Dimitriou G, Jelastopulu
E, Giannakopoulos I, Anastassiou ED and Christofidou M: Neonatal
intensive care unit candidemia: Epidemiology, risk factors, outcome
and critical review of published case series. Mycopathologia.
173:219–228. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Juyal D, Sharma M, Pal S, Rathaur VK and
Sharma N: Emergence of non-albicans Candida species in
neonatal candidemia. N Am J Med Sci. 5:541–545. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Vogiatzi L, Ilia S, Sideri G, et al:
Invasive candidiasis in pediatric intensive care in Greece: A
nationwide study. Intensive Care Med. 39:2188–2195. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lawley TD and Walker AW: Intestinal
colonization resistance. Immunology. 138:1–11. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lamousé-Smith ES, Tzeng A and Starnbach
MN: The intestinal flora is required to support antibody responses
to systemic immunization in infant and germ free mice. PLoS One.
6:e276622011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
de Moreno de LeBlanc A and LeBlanc JG:
Effect of probiotic administration on the intestinal microbiota,
current knowledge and potential applications. World J
Gastroenterol. 20:16518–16528. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shan YS, Sy ED, Wang ST, Lee JC and Lin
PW: Early presumptive therapy with fluconazole for occult
Candida infection after gastrointestinal surgery. World J
Surg. 30:119–126. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Almirante B and Pemán J: Current treatment
of candidemia. Role of anidulafungin. Enferm Infecc Microbiol Clin.
26 (Suppl 14):21–28. 2008.(In Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Garsin DA and Lorenz MC: Candida
albicans and Enterococcus faecalis in the gut: Synergy
in commensalism? Gut Microbes. 4:409–415. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sealy PI, Garner B, Swiatlo E, Chapman SW
and Cleary JD: The interaction of mannose binding lectin (MBL) with
mannose containing glycopeptides and the resultant potential impact
on invasive fungal infection. Med Mycol. 46:531–539. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Brenuchon C, Lebas D, Rakza T, Piette F,
Storme L and Catteau B: Invasive fungal dermatitis in extremely
premature newborns: A specific clinical form of systemic
candidiasis. Ann Dermatol Venereol. 133:341–346. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Chen CJ, Weng YH, Su LH and Huang YC:
Molecular evidence of congenital candidiasis associated with
maternal candidal vaginitis. Pediatr Infect Dis J. 25:655–656.
2006. View Article : Google Scholar : PubMed/NCBI
|