Introduction
Malignant obstructive jaundice comprises a group of
diseases that can be caused by primary biliary carcinomas, such as
cholangiocarcinoma and gallbladder cancer, and extra-biliary
carcinomas, such as ampullary, pancreatic and gastric cancer and
hepatocellular carcinoma (1).
Malignant obstructive jaundice can lead to hyperbilirubinemia,
anorexia, pruritus, cholangitis, septicemia and liver failure.
Generally, surgical resection remains the primary treatment for
malignant obstructive jaundice; however, in numerous cases the
malignant obstructive jaundice is detected when the disease is
already at an advanced stage (2).
For the patients that are unable to undergo surgery, urgent
treatment is required to improve hepatic function, in order to
facilitate the addition of subsequent anti-tumor therapy to their
treatment regimen. The average survival time of patients with
obstructive jaundice is <3 months (3). Percutaneous transhepatic biliary
drainage (PTBD) and stenting are emerging alternative treatments
for malignant obstructive jaundice that exhibit good clinical
efficacy and few complications and lead to limited patient
suffering. PTBD and stenting is the first choice for elderly
patients, patients with inoperable malignant obstructive jaundice,
and patients with postoperative recurrence, diabetes, or
cardiovascular disease.
Case report
Case 1
The patient was a 51-year-old man who presented with
~3 weeks' history of obstructive jaundice. The patient was admitted
to Fuyan People's Hospital (Fuyang, China) on June 12, 2014. Liver
and kidney function analyses, and routine blood tests were
conducted upon admission; and heaptic bilirubin levels were higher
than normal. Abdominal computed tomography (CT) showed pancreatic
cancer, as well as dilation of the intra- and extrahepatic bile
ducts. The patient was at an advanced disease stage and refused to
undergo surgical resection. PTBD and stenting were performed in the
interventional operating room following the provision of informed
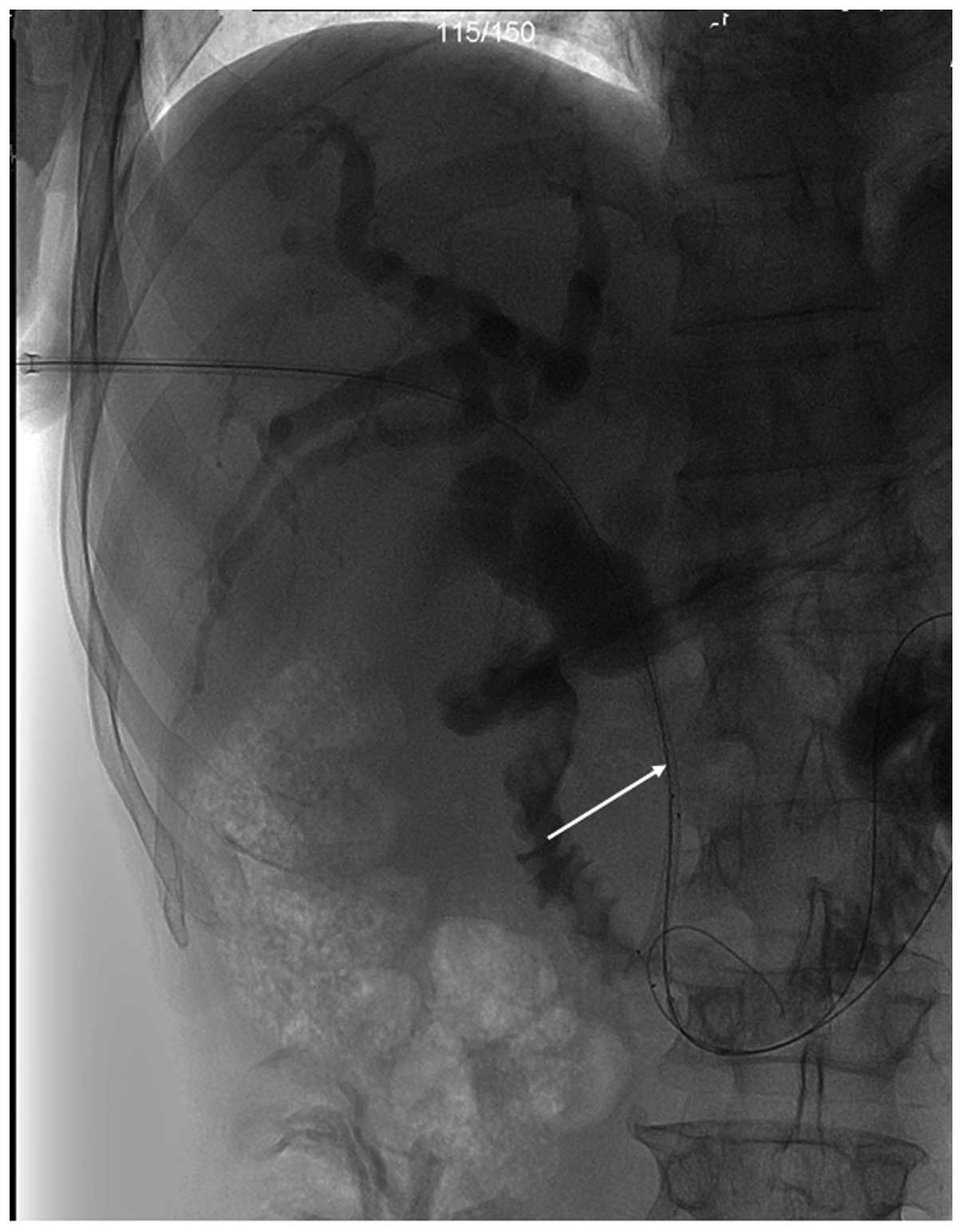
consent by the patient. The procedure to puncture the biliary duct
was guided under ultrasound (US). An 18-G Chiba needle and a
0.035-inch guide-wire were used to gain access to the biliary
system using a right-sided puncture approach. An 8-F sheath was
inserted to facilitate the procedure. A 0.035-inch hydrophilic
guide-wire was advanced through the stenosis into the duodenum. The
hydrophilic guide-wire was exchanged for a 0.035-inch stiff
guide-wire. Finally, a self-expanding metallic stent [Micro-Tech
(Nanjing) Co., Ltd.] was inserted alongside the guide-wire into the
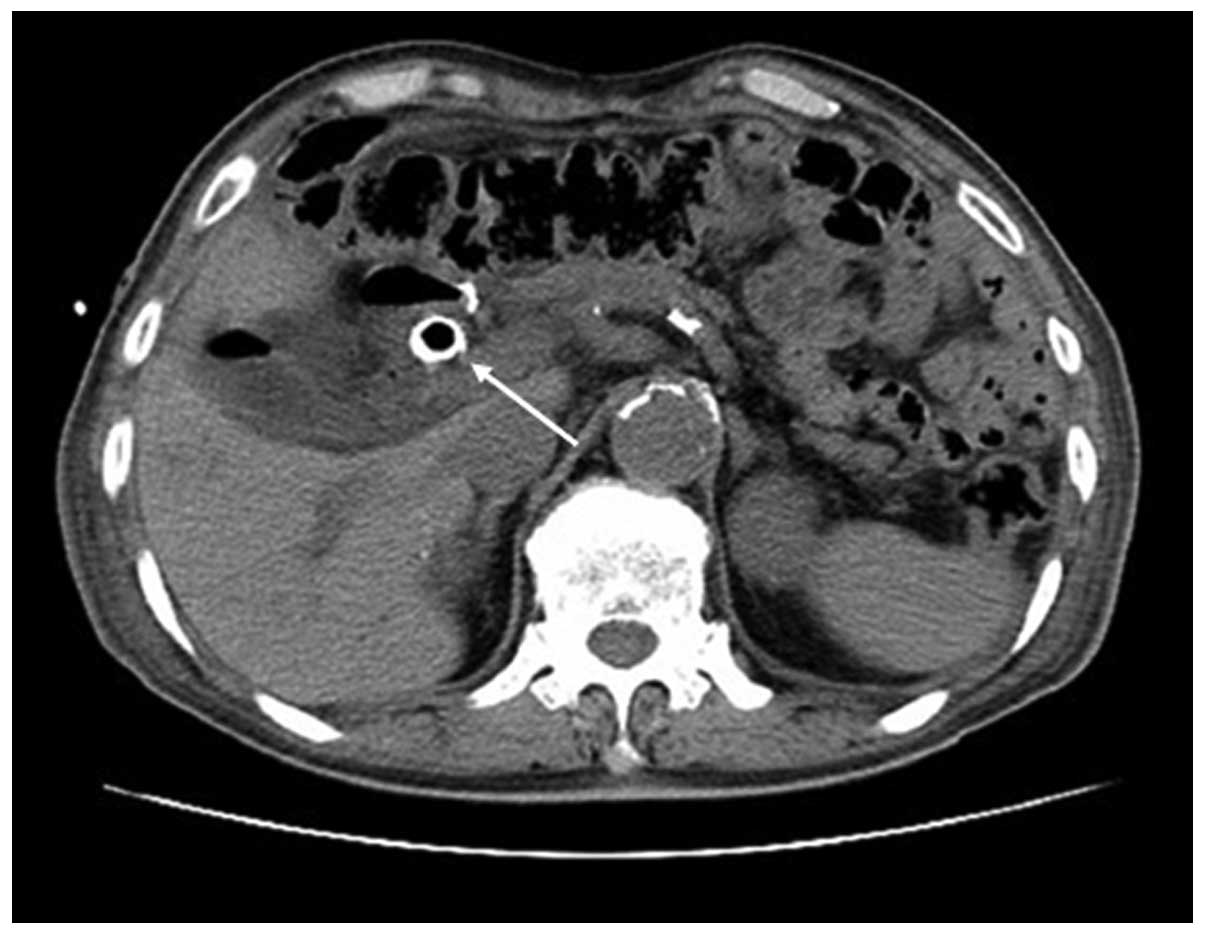
narrow segment (Fig. 1). A CT scan
was performed a month after the PTBD and stenting (Fig. 2), and the patient recovered well
following the surgery.
Case 2
The patient was an 84-year-old man who presented
with ~1 week's history of obstructive jaundice. The patient also
presented with symptoms of pruritus. The patient was admitted to
Fuyan People's Hospital on August 16, 2014. Liver and blood
coagulation function analyses, and routine blood tests were
conducted upon admission. Abdominal CT was used to diagnose
carcinoma of the ampulla of Vater, with extrahepatic bile duct
dilatation. The patient's condition was too advanced for surgery to
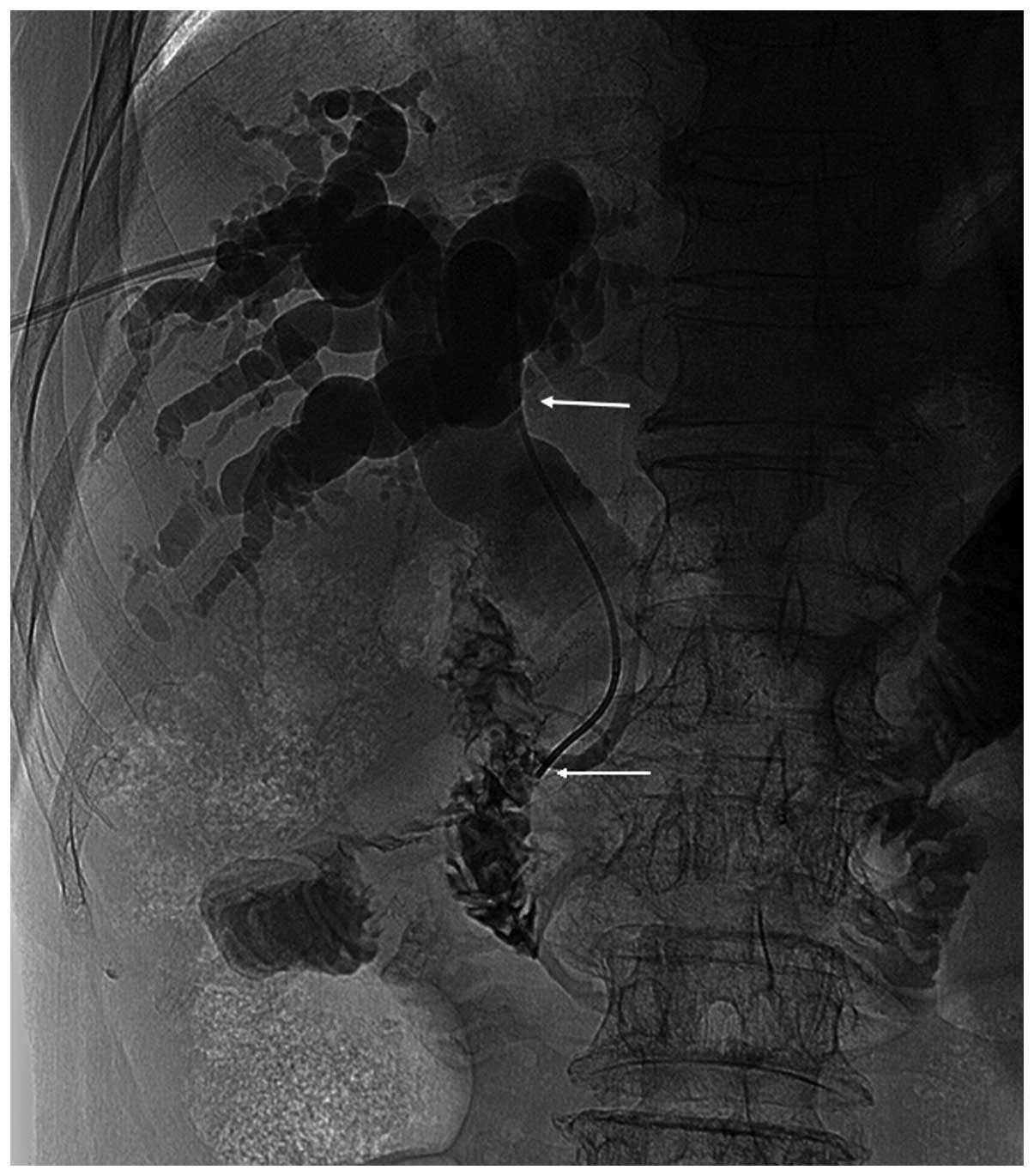
be advisable. PTBD and stenting were performed to resolve the
obstructive jaundice. Cholangiography revealed common bile duct
stenosis in the lower section of the bile duct, which measured ~6
cm (Fig. 3). A minimally invasive
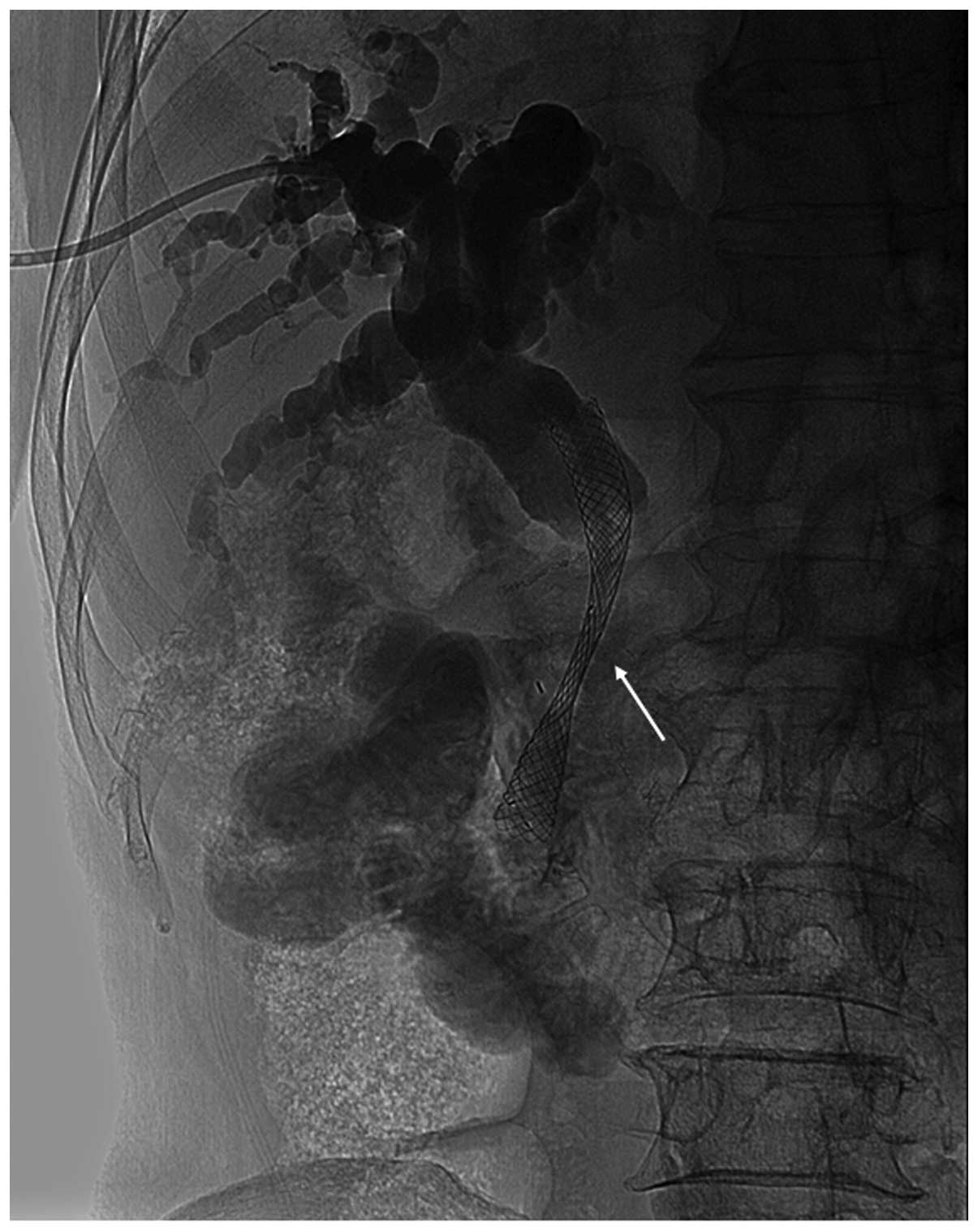
implantation of an 8-F/80×10 mm metal stent was performed. The
biliary stent was implanted successfully to cover the stenotic bile
duct (Figs. 4 and 5). The patient experienced an uneventful
post-procedural outcome. A further CT scan was performed 14 days
after PTBD and stenting (Fig. 6),
which showed that the metal stent was at the correct location, and
no bile duct dilatation was observed.
PTBD and stenting procedure
The PTBD and stenting were performed with US-guided
and digital subtraction angiography. Cholangiography was first used
to evaluate the exact level and extension of the stenosis or
stenoses and to select the most appropriate liver segments for
drainage. Finally, a self-expanding metallic stent [Micro-Tech
(Nanjing) Co., Ltd., Nanjing, China] was inserted alongside the
guide-wire into the narrow segment.
All patients were monitored for vital signs, oxygen
saturation, and liver and kidney function post-surgery, and routine
blood investigations were performed. Rehydration was considered
paramount to protect the liver and prevent infection.
Results
The PTBD and stenting procedures in the two patients
were considered successful and were performed without the
occurrence of procedure-associated complications. The patients were
followed-up for 1 month post-surgery. The patients' liver function
post-procedure (1 month after PTBD and stenting) was notably
improved compared with the pre-procedure (1 day before PTBD and
stenting) liver function (Table I).
In addition, the patients' jaundice was evidently improved. The
present study indicates that PTBD and stenting can exert a
definitive positive effect on hepatic function in patients with
obstructive jaundice.
 | Table I.Liver function of the patients before
and after PTBD and stenting. |
Table I.
Liver function of the patients before
and after PTBD and stenting.
|
| Total bilirubin
(µmol/l) | Direct bilirubin
(µmol/l) | ALT (U/l) |
|---|
|
|
|
|
|
|---|
| Case no. | Before | After | Before | After | Before | After |
|---|
| 1 | 333.59 | 106.59 | 229.90 | 71.00 | 196 | 93 |
| 2 | 419.02 |
77.75 | 278.20 | 48.30 | 161 | 27 |
Discussion
Malignant biliary obstruction may be caused by
cholangiocar- non biliary carcinomas (1–3). The
current treatment options for malignant obstructive jaundice
include surgical, interventional therapy and endoscopic therapy.
Surgery is primarily applied in cases of extrahepatic bile duct
obstruction. Surgery may be used to relieve jaundice in addition to
removing lesions and peripheral vascular invasion (1). The patients with a generally poor
condition, diabetes, cardiovascular disease complications or the
elderly may not be suitable to undergo surgery. Interventional
therapy is the preferred treatment for the patients with the
aforementioned conditions (3). At
the time of diagnosis, 90% of patients with malignant obstructive
jaundice may benefit from palliative treatment only (4). The objective of palliation is to
relieve jaundice-related symptoms, preventing cholangitis. In
recent years, with the development of technology and medical
materials, PTBD and stenting have exhibited good efficacy, with few
complications and reduced associated pain, and are emerging as
crucial palliative treatments for malignant obstructive jaundice
(5,6). In addition to prolonging patient
survival time, PTBD and stenting are able to improve quality of
life. In 1981, Fletcher et al first reported three cases of
patients with malignant obstructive jaundice that deposition
199Ir into biliary via a PTCD drainage tube (7). The approach achieved good results in
controlling intraductal tumor growth. However, there were a number
of treatment deficiencies. As 199Ir is a high source of
radiation, and safe levels of human exposure to radiation dose are
limited, resulting in patients received a discontinuous radiation
therapy with long-term drainage tube carrying. The primary
complications associated with PTBD and stenting include the
following: i) Drainage tube or biliary stent dislocation; ii)
cholangitis; iii) hemobilia; and iv) pancreatitis (4,5). No
complications were observed in the cases described in the present
study. In conclusion, PTBD and stenting are able to markedly
improve hepatic function, without serious complications, and thus
represent a potentially safe and feasible intervention for patients
with malignant obstructive jaundice.
Acknowledgements
This study was supported by the Science and
Technology Development Plan of Fuyang City (no. 2014SK013).
References
|
1
|
Barauskas G, Gulbinas A and Pundzius J:
Results of surgical treatment of carcinoma of papilla of Vater.
Medicina (Kaunas). 43:455–462. 2007.PubMed/NCBI
|
|
2
|
Brountzos EN, Ptochis N, Panagiotou I,
Malagari K, Tzavara C and Kelekis D: A survival analysis of
patients with malignant biliary strictures treated by percutaneous
metallic stenting. Cardiovasc Intervent Radiol. 30:66–73. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
van Delden OM and Lameris JS: Percutaneous
drainage and stenting for palliation of malignant bile duct
obstruction. Eur Radiol. 18:448–456. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Qian XJ, Zhai RY, Dai DK, Yu P and Gao L:
Treatment of malignant biliary obstruction by combined percutaneous
transhepatic biliary drainage with local tumor treatment. World J
Gastroentero1. 12:331–335. 2006.
|
|
5
|
Feng GH, Cai Y, Jia Z, Yang DQ, Chen H,
Jin HC, Yu QH, Zhu W and Wang CX: Interventional therapy of
malignant obstructive jaundice. Hepatobiliary Pancreat Dis Int.
2:300–302. 2003.PubMed/NCBI
|
|
6
|
Garcarek J, Kurcz J, Guziński M, Janczak D
and Sasiadek M: Ten years single center experience in percutaneous
transhepatic decompression of biliary tree in patients with
malignant obstructive jaundice. Adv Clin Exp Med. 21:621–632.
2012.PubMed/NCBI
|
|
7
|
Fletcher MS, Brinkley D, Dawson JL,
Nunnerley H, Wheeler PG and Williams R: Treatment of high bileduct
carcinoma by internal radiotherapy with iridium-192 wire. Lancet.
2:172–174. 1981. View Article : Google Scholar : PubMed/NCBI
|