Introduction
Severe pneumonia complicated with pulmonary
infection in clinical practice (1,2) is
accompanied by multiple organ dysfunction syndrome characterized by
a physiological and pathological foundation, primarily hypoxia and
hypoperfusion (3,4). Patients with severe pneumonia are
critically ill, and if the disease is not treated in time, proneto
water, electrolyte, acid-base balance disorders may occur, causing
multiple organ dysfunction and even the emergence of septic shock.
Early treatment with antibiotics and supportive therapy is an
important measure to improve the prognosis of patients. In
addition, timely access to a patients response to treatment, in
order to evaluate the prognosis, has important significance for the
prognosis of patients in Intensive Care Units (ICUs) and the
adjustment of a treatment plan.
Blood lactate levels, oxygen metabolism and tissue
perfusion can be used to monitor and assess the systemic index. The
level of lactate in the blood reflects the increase in anaerobic
metabolism, while the oxygenation index (PaO2/FiO2), moving average
for mixed venous oxygen saturation from the whole body perfusion
vascular bed values, reflects the balance between the oxygen supply
and the oxygen required, which can be used to determine the tissue
oxygenation status. Normal values vary between 400 and 500 mmHg
(5,6). C-reactive protein (CRP) is the most
sensitive acute phase protein. In the process of inflammation, a
rapid increase in the blood lactic acid concentration is observed
(7–9). PaO2, CRP three combined test, and
dynamic observation of, can from different aspects to reflect the
association between the oxygen supply and demand and
inflammation.
Therefore, it was hypothesized that blood test
results may correlate with the severity of pneumonia, and certain
parameters may be used as an indicator to identify patients who
require intensive care, and subsequently improve the treatment
efficacy. Thus, the primary objective of the present study was to
assess the correlations between the blood lactic acid level,
oxygenation index and CRP level with the mortality risk scores,
focusing on the prognosis of patients with acute physiology, age
and chronic health evaluation II (APACHE II) score.
Materials and methods
Patient population and sample
preparation
In total, 34 patients with severe pneumonia,
hospitalized at the ICU of the First Hospital of Jilin University
(Changchun, China) between July 1, 2012 and December 31, 2013, were
recruited as research subjects. The study was conducted in
accordance with the Declaration of Helsinki and with approval from
the Ethics Committee of Jilin University. Written informed consent
was obtained from all the participants.
Standard of diagnosis for severe
pneumonia
Recruited subjects were diagnosed with severe
pneumonia according to the diagnostic criteria of severe
community-acquired pneumonia outlined by the American Thoracic
Society (2007) (10). The main
criteria were as follows: i) Respiratory failure requiring
mechanical ventilation of the lungs; ii) invasion expansion of
>50% within 48 h; iii) an infection or requiring the use of
vocative drugs >4 h after the shock; and iv) acute renal
failure, as demonstrated by urine levels of <80 ml/4 h or
non-chronic renal insufficiency patients with serum creatinine
levels of >200 µg/dl. The minor criteria were as follows: i) 7
breaths/>30 owed; ii) PaO2/FiO2 of <250; iii) bilateral or
multi leaf inflammation; and iv) systolic and diastolic blood
pressure of <90 and <60 mmHg, respectively. The patients
exhibited all the major criteria and a minimum of two minor
criteria. In total, 26/34 patients survived who comprised the
survival group, while there were 16 cases of mortality (fatality
group). The demographics of the two groups are shown in Table I.
 | Table I.Patient demographics. |
Table I.
Patient demographics.
| Parameter | Survival group
(n=26) | Fatality group
(n=8) |
|---|
| Age, years | 63.24±18.76 | 62.6±18.34 |
| Gender, male/female,
n | 14/12 | 5/3 |
| Blood lactic acid,
mmol/l | 4.45±1.27 | 4.62±1.43 |
| Oxygenation index,
mmHg | 200±50 | 205±45 |
| C-reactive protein,
mg/l | 52±10 | 52±8 |
| APACHE II score | 22.84±5.12 | 23.75±3.89 |
Exclusion criteria
Patients were excluded from the study if they had
not received antibiotic treatment for their clinical symptoms or
had lung lesions with marked absorption. Furthermore, previous
history of a serious heart, brain, kidney or vascular disease, or
cancer, was used as exclusion criteria. In addition, patients were
excluded if they suffered from an autoimmune disease, or were
suffering from an additional infection. If the patients had
undergone ~1 month of a special treatment history, including
radiation therapy, chemotherapy, biological treatment and surgical
immunosuppressive therapy, they were excluded. Pregnant women were
also excluded from the study. The study was approved by the Ethics
Committee of the First Hospital of Jilin University, and all
subjects signed the informed consent.
Patients and methods
In order to monitor the oxygenation index
(PaO2/FiO2) and CRP levels, blood gas analysis and biochemical
examination were carried out. In addition, various etiological
parameters were recorded in the ICU, as well as the length of stay
in the ICU and the number of days of mechanical ventilation, which
were used to assess the prognosis of the patients. At 6, 24 and 72
h following treatment, all the patients underwent a review, in
which the arterial blood lactate concentration, oxygenation index
(PaO2/FiO2), and the 6-h lactic acid clearance rate were calculated
(11). Furthermore, the changes in
the CRP levels were assessed at 24 and 72 h, and the APACHE II
score was calculated at 72 h. Patients were administered bundle
treatment following diagnosis, including prior to the routine use
of antibiotics and the collection of blood, urine, sputum and any
other relevant specimens for bacterial culture, in the hospital l
day according to the results of bacterial culture and antibiotics
in the treatment of hypotension or experience; blood lactic acid
levels of >4 mmol/l, immediate fluid resuscitation, a dose of 20
ml/kg, such as low blood pressure cannot be corrected, while the
use of vocative drugs was applied to maintain the mean arterial
pressure at >65 mmHg. Sustained hypotension or blood lactic acid
levels of >4 mmol/l, for fluid resuscitation, the central venous
pressure (CVP) >8 mmHg, SaO2 >90%, urine level of >0.5/ml
(kg/h). If the liquid recovery following CVP was 8–12 mmHg, or
dobutamine infusion. According to the adjustment of mechanical
ventilation parameters of blood gas, liquid amount of vocative
drugs, treatment measures. All patients received treatment for 6 h
to achieve these goals. Through monitoring and adjusting the
treatment protocol with mechanical ventilation and the application
of glucocorticoids, hemodynamic stability was maintained and the
blood sugar levels were actively controlled, according to the
requirements of continuous intravenous infusion of insulin to
control the blood sugar level at <8.3 mmol/l.
Statistical analysis
Categorical variables are expressed as a number and
percentage, while continuous variables are expressed as the mean ±
standard deviation or as the median and interquartile range (IQR),
as appropriate. The blood test findings are expressed as the median
and IQR. Correlation analysis was performed using Spearmans rank
correlation, while the 2-test was used to compare categorical
variables. P<0.05 was considered to indicate a statistically
significant difference. The commercial statistical software package
used was SPSS 15.0 (SPSS, Inc., Chicago, IL, USA). Samples were
collected from 34 patients after retro.
Results
Blood test results
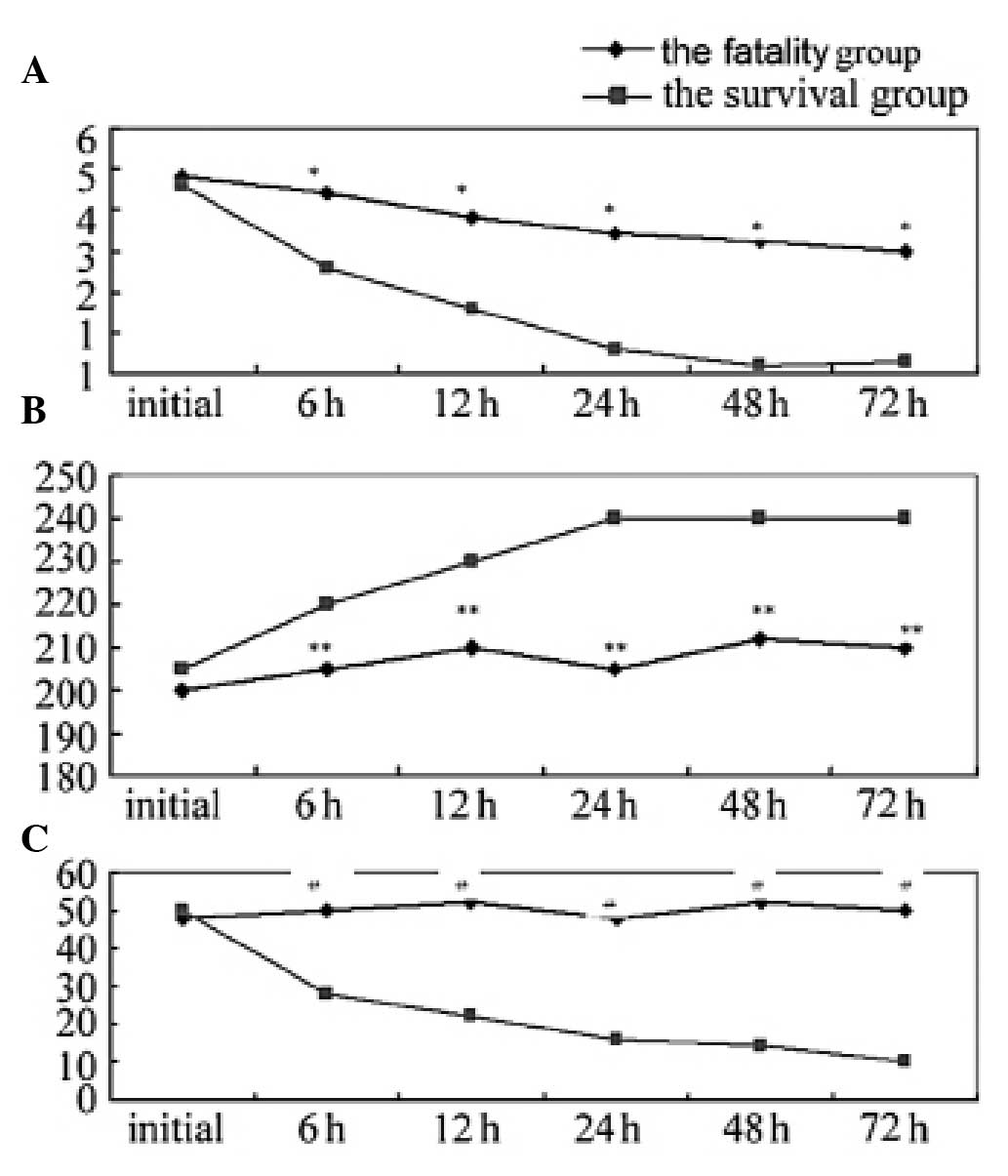
Blood lactic acid levels, the APACHE II score and
the change in CRP concentration were assessed. As shown in Fig. 1A, the blood lactate levels were
significantly lower in the survival group when compared with the
fatality group. During the 12–24 h hospital treatment period, the
blood lactic acid levels rapidly decreased to normal levels in the
survival group. However, in the fatality group, during the
observation period, almost no changes were observed in the blood
lactate level, with a sustained high state. Fig. 1B indicates that the oxygenation index
(PaO2/FiO2) in the survival group was significantly higher when
compared with that of the fatality group, and was maintained at a
normal level. However, in the fatality group, the oxygenation index
(PaO2/FiO2) was lower than the normal level and was shown to
continually decline. Furthermore, Fig.
1C shows that the CRP levels in the fatality group at 6, 24 and
72 h were significantly higher when compared with the survival
group, and the difference was statistically significant
(P<0.05). No statistically significant difference was observed
in the CRP level of the fatality group at 24 and 72 h (P=0.17).
Severity of the pneumonia
prognosis
Table II shows the
lactate clearance rate and the incidence of sepsis in the two
groups. The results revealed that the 6-h lactate clearance rate in
the survival group was significantly higher when compared with the
fatality group, while the incidence of sepsis was significantly
lower in the survival group when compared with the fatality group;
the differences were statistically significant (P<0.05). In the
fatality group, the APACHE II scores were shown to increase in
accordance with the arterial blood lactate concentration, and the
APACHE score and blood lactate concentration were found to
correlate (r=0.656, P<0.05).
 | Table II.Lactate clearance rates and the
incidence of sepsis in the two groups. |
Table II.
Lactate clearance rates and the
incidence of sepsis in the two groups.
| Group | Initial lactate
level, mmol/l | 6-h lactate clearance
rate, % | APACHE II score | Sepsis incidence, %
(n) |
|---|
| Survival | 4.45±1.27 | 29.43±9.71 | 14.6±1.43 | 30.77 (16/52) |
| Fatality | 4.62±1.43 | 11.27±2.61 | 23.2±3.9 | 81.25 (13/16) |
| P-value | 0.43 | 0.01 | <0.001 | <0.001 |
Discussion
Severe pneumonia is defined as respiratory
insufficiency, which is caused by tissue hypoxia and metabolic
dysfunction (12,13). Sequential failure, severe pneumonia
in children, the elderly, the frail, immunocompromised patients,
children's basic physiology and pathology of special schools,
elderly patients prior to the onset of the majority of existing
heart, lung disease, mainly in chronic obstructive pulmonary
disease, diabetes, coronary heart disease, low immunity, tumor etc.
The pathological basis of severe pneumonia infection is the
triggering of a series of inflammatory events, including
inflammatory cytokine release, which results in hemodynamic
changes. For example, elevated endotoxin levels in the blood and an
uncontrolled systemic inflammatory response leads to multiple organ
failure. Changes to the in vivo microenvironment ##and
normal metabolic disorder caused by cells due to a lack of oxygen
are the main reasons for the formation of multiple organ
dysfunction syndrome (14). CRP is a
product of fibrin dissolution, and is increased in inflammatory
diseases. Therefore, the protein can be used as an important index
to evaluate systemic inflammation. In patients with severe
pneumonia, tissue organ effective blood volume reduction, which
further exacerbates tissue hypoxia and increases anaerobic
metabolism. Blood lactic acid is a product of the anaerobic
glycolysis of glucose, and can directly reflect the tissue
hypoperfusion and hypoxia conditions. Lactic acidosis is an
important index of shock, hypoxia and oxygen metabolism, and
quantitative detection and monitoring of the lactic acid levels in
patients undergoing recovery from severe pneumonia is an important
indicator (6,15,16),
with significant value for assessment of the disease. The
oxygenation index (PaO2/FiO2) is an indicator of the oxygen supply
levels reflect the extracellular, is the average mixed venous
oxygen saturation from the whole body perfusion vascular beds
value. The index reflects the state of tissue oxygenation and
perfusion, tissue oxygen supply and oxygen requirements (17–19). In
addition, the oxygenation index (PaO2/FiO2) is an important
predictor of the prognosis of patients in a critical condition.
Through dynamic monitoring of the oxygenation index (PaO2/FiO2),
treatment protocols can be effectively guided, while evaluating the
prognosis. Strengthen the monitoring of oxygen metabolism in
patients with early, early detection and correct body anoxic
condition may improve the survival rate of the patients, the Nguy
-en and so on the oxygenation index (PaO2/FiO2) <300 mmHg as
septic shock early goal-directed therapy can improve prognosis. The
results of the present study demonstrated that the early course of
oxygenation index (PaO2/FiO2) for 2 times less than 250 of
patients, the prognosis is not good. Therefore, monitoring the
oxygenation index (PaO2/FiO2) level, particularly continuous
detection for condition assessment, has important clinical
significance. In patients with persistent pneumonia, the
oxygenation index (PaO2/FiO2) was shown to decrease, indicating
that the body was in severe hypoxia. In ICU, positive measures can
be applied to increase the oxygen intake, improve microcirculation
and reduce oxygen consumption and other measures to correct the
severe hypoxia. However, the oxygenation index (PaO2/FiO2) only
reflects the systemic oxygen supply and consumption balance; thus,
is unable to evaluate the local situation. Therefore, certain
studies have attempted to assess the local oxygen saturation and
oxygen load using additional methods, with the aim to further
understand the tissue oxygen supply for disease detection and the
guidance of treatment (20,21).
CRP is an acute phase protein that is an important
index of inflammation. Thus, the CRP concentration in patients with
infectious diseases, particularly infectious shock and severe
infection, increases significantly. The underlying mechanism is
hypothesized to primarily involve endotoxin or antigen antibody
complexes functioning as activators to directly activate the
release of proinflammatory cytokines. Inflammation can be caused by
the release of a variety of inflammatory factors, which
subsequently leads to hypoxia, acidosis-induced pulmonary
microvascular contraction and a slow blood supply. In the present
study, the CRP level in the survival group was lower when compared
with the fatality group, which exhibited significantly increased
levels. If a decrease in the CRP concentration is not evident, or
the levels continue to increase, the disease prognosis is not good.
Following treatment, Lin Zhejiang (22) detected significantly increased levels
of CRP in 48 elderly patients with severe pneumonia, as compared
with the healthy group, indicating that body in elderly patients
with severe pneumonia in inflammatory activity anomaly detection.
Therefore, dynamic monitoring of the CRP level may aid the
understanding of the in vivo inflammatory medium water in
patients with severe pneumonia, purification for guiding clinical
use of anti-inflammatory medium drugs or continuous blood (CRRT)
provide the basis, thus reducing the mortality rate. A single blood
lactic acid, is the reflection of the oxygen supply and the
anaerobic metabolism state, the rain during the ICU treatment,
doctors would like to grasp the improving hypoxia in patients after
treatment. Therefore, the dynamic determination of the blood lactic
acid level may be more meaningful. Nguyen et al (11) demonstrated that in patients with
septic shock resuscitation, a 6-h lactic acid clearance rate of
≥10% resulted in the dosage of vocative drugs being significantly
lower when compared with the patients who had a low clearance rate,
and the mortality rate was also significantly reduced. Therefore,
determination of the lactate clearance rate may better reflect the
patient prognosis compared with the pure lactic acid concentration.
Treatment to effectively reduce the blood lactic acid level is
limited; thus, improving the tissue perfusion and oxygenation
status is challenging. Subsequently, the progression of the disease
may deteriorate and the condition may easily develop into septic
shock, with an increased mortality rate. Retrospective analysis of
the present study revealed that patients in the survival group had
a higher lactate clearance rate when compared with the fatality
group, and the decreasing speed, survival group blood lactate
within 24 h were normal, while the fatality group until 72 h
remained significantly higher compared with the survival group. The
APACHE II score is an indicator of vital signs in the patient
response, and is an important index in ICU management. In addition,
the APACHE II score was shown to be closely associated with the
disease state; the higher the score, the more severe the
prognosis.
The present study had a number of limitations.
Firstly, as the study was retrospective, there was a lack of strict
control with regard to case inclusion and exclusion criteria.
Secondly, the detection methods have evidently progressed in modern
ICU treatment; thus, the majority of patients had a good prognosis,
subsequently resulting in the number of cases in the survival and
fatality groups being unequal. Therefore, there may be bias in the
data statistics. The pathological basis of severe pneumonia is
known to be a series of responses to infection, and the present
study observed three downstream indicators of the disease, namely a
balanced supply of blood oxygen, cell anaerobic metabolism and
inflammation. However, the present study only assessed the disease
in terms of the developing reaction, and in order to fully
understand the prognosis and outcome of severe pneumonia (25,26),
other indicators should be considered. For example, numerous
factors, including the age of the patient, the basic disease, lung
inflammation and treatment measures, may affect the prognosis of
patients. Therefore, further study is required in this research
direction.
In summary, dynamic monitoring of the levels of
blood lactic acid, the oxygenation index and CRP in patients with
severe pneumonia can be used to evaluate the therapeutic
efficiency, in addition to functioning as a prognosis indicator for
patients with severe pneumonia. Although the number of patients
included in the present study was low, the results provide a
preliminary basis, and are useful and important data that require
confirmation in further studies.
Acknowledgements
The authors thank Liping Peng for her assistance
with the specimen preparation and processing.
References
|
1
|
Ethan AH and Alvin S: Management of
community-acquired pneumonia. J Assoc Physicians India. 61(Suppl):
20–23. 2013.(In Chinese).
|
|
2
|
Di Pasquale M, Ferrer M, Esperatti M, et
al: Assessment of severity of ICU-acquired pneumonia and
association with etiology. Crit Care Med. 42:303–312. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Menter T, Giefing-Kroell C,
Grubeck-Loebenstein B and Tzankov A: Characterization of the
inflammatory infiltrate in Streptococcus pneumoniae pneumonia in
young and elderly patients. Pathobiology. 81:160–167. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cameron MJ, Ran L, Xu L, et al: Canadian
SARS Research Network: Interferon-mediated immunopathological
events are associated with atypical innate and adaptive immune
responses in patients with severe acute respiratory syndrome. J
Virol. 81:8692–8706. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Jones AE, Shapiro NI, Trzeciak S, et al:
Emergency Medicine Shock Research Network (EMShockNet)
Investigators: Lactate clearance vs central venous oxygen
saturation as goals of early sepsis therapy: a randomized clinical
trial. JAMA. 303:739–746. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dechert RE, Park PK and Bartlett RH:
Evaluation of the oxygenation index in adult respiratory failure. J
Trauma Acute Care Surg. 76:469–473. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kobayashi K and Takeda S: ECMO for the
patients with severe respiratory failure associated with ARDS due
to influenza. Masui. 62:557–562. 2013.(In Japanese). PubMed/NCBI
|
|
8
|
Wang T, Xia Y, Hao D, et al: The
significance of lactic acid in early diagnosis and goal-directed
therapy of septic shock patients. Zhonghua Wei Zhong Bing Ji Jiu Yi
Xue. 26:51–55. 2014.(In Chinese). PubMed/NCBI
|
|
9
|
Marti C, Garin N, Grosgurin O, Poncet A,
Combescure C, Carballo S and Perrier A: Prediction of severe
community-acquired pneumonia: a systematic review and
meta-analysis. Crit Care. 16:R1412012. View
Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mandell LA, Wunderink RG, Anzueto A, et
al: Infectious Diseases Society of America; American Thoracic
Society: Infectious Diseases Society of America/American Thoracic
Society consensus guidelines on the management of
community-acquired pneumonia in adults. Clin Infect Dis. 44(Suppl
2): S27–S72. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nguyen HB, Rivers EP, Knoblieh BP,
Jacobsen G, Muzzin A, Ressler JA and Tomlanovich MC: Early lactate
clearance is associated with improved outcome in severe sepsis and
septic shock. Crit Care Med. 32:1637–1642. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Charlson ME, Pompei P, Ales KL and
MacKenzie CR: A new method of classifying prognostic comorbidity in
longitudinal studies: development and validation. J Chronic Dis.
40:373–383. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Dellinger RP, Carlet JM, Masur H, et al:
Surviving Sepsis Campaign Management Guidelines Committee:
Surviving Sepsis Campaign guidelines for management of severe
sepsis and septic shock. Crit Care Med. 32:858–873. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Marshall JC: Inflammation, coagulopathy,
and the pathogenesis of multiple organ dysfunction syndrome. Crit
Care Med. 29(Suppl): S99–S106. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
James JH, Luchette FA, McCarter FD and
Fischer JE: Lactate is an unreliable indicator of tissue hypoxia in
injury or sepsis. Lancet. 354:505–508. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chalmers JD, Singanayagam A and Hill AT:
Predicting the need for mechanical ventilation and/or inotropic
support for young adults admitted to the hospital with
community-acquired pneumonia. Clin Infect Dis. 47:1571–1574. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Miller MJ: Tissue oxygenation in clinical
medicine: an historical review. Anesth Analg. 61:527–535. 1982.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Journois D and Safran D: Continuous
monitoring of mixed venous blood oxygen saturation. Ann Fr Anesth
Reanim. 12:393–408. 1993.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Krafft P, Steltzer H, Hiesmayr M, Klimscha
W and Hammerle AF: Mixed venous oxygen saturation in critically ill
septic shock patients. The role of defined events. Chest.
103:900–906. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Reinhart K, Kuhn HJ, Hartog C and Bredle
DL: Continuous central venous and pulmonary artery oxygen
saturation monitoring in the critically ill. Intensive Care Med.
30:1572–1578. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kim KM, Ko JS, Gwak MS, Kim GS and Cho HS:
Comparison of mixed venous oxygen saturation after in vitro
calibration of pulmonary artery catheter with that of pulmonary
arterial blood in patients undergoing living donor liver
transplantation. Transplant Proc. 45:1916–1919. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Krüger S, Ewig S, Giersdorf S, et al:
German Competence Network for the Study of Community Acquired
Pneumonia (CAPNETZ) Study Group: Cardiovascular and inflammatory
biomarkers to predict short- and long-term survival in
community-acquired pneumonia: results from the German Competence
Network, CAPNETZ. Am J Respir Crit Care Med. 182:1426–1434. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Borthwick HA, Brunt LK, Mitchem KL and
Chaloner C: Does lactate measurement performed on admission predict
clinical outcome on the intensive care unit? A concise systematic
review. Ann Clin Biochem. 49:391–394. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Rhodes A and Bennett ED: Early
goal-directed therapy: An evidence-based review. Crit Care Med.
32(Suppl): S448–S450. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Dang TT, Eurich DT, Weir DL, Marrie TJ and
Majumdar SR: Rates and risk factors for recurrent pneumonia in
patients hospitalized with community-acquired pneumonia:
population-based prospective cohort study with 5 years of
follow-up. Clin Infect Dis. 59:74–80. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Adamuz J, Viasus D, Jiménez-Martínez E,
Isla P, Garcia-Vidal C, Dorca J and Carratalà J: Incidence, timing
and risk factors associated with 1-year mortality after
hospitalization for community-acquired pneumonia. J Infect.
68:534–541. 2014. View Article : Google Scholar : PubMed/NCBI
|