Introduction
Peripheral nerve blocks are a type of regional
anesthesia. Local anesthetics (LAs) are injected near a specific
nerve or bundle of nerves in order to block sensations of pain from
a specific area of the body. Transversus abdominis plane (TAP)
block is a newly described peripheral nerve block technique which
can be used for any surgical technique that involves the lower
abdominal wall (1,2). TAP block can be performed by injecting
LAs into the tissue plane between the internal oblique and the
transversus abdominis via a blind technique, based on surface
anatomy landmarks (1,2) and, most recently, an ultrasound
(US)-guided technique under direct vision (3,4). TAP
block has been shown to effectively provide analgesia, without the
requirement for intrathecal morphine, as part of a multimodal
analgesic regimen following cesarean delivery (5). However, the duration of analgesia
provided by a single-injection TAP block has been demonstrated to
be shorter, as compared with that of the intrathecal morphine
(2–4).
There has been an interest in combining LAs with
opioids to improve the duration and quality of peripheral nerve
blocks, since the characterization of the opioid receptors in
peripheral nerves (6,7). Furthermore, various opioids, including
fentanyl and sufentanil, have been shown to exert LA-like effects
(8). However, the effects of opioids
on peripheral nerve blocks are controversial; previous studies have
reported both positive and negative effects for opioids (9–17). To
the best of our knowledge, the use of opioids as analgesic adjuncts
to the TAP block for postoperative analgesia are yet to be
reported. The present study investigated whether the addition of
fentanyl to an US-guided TAP block may prolong the analgesic
duration following elective cesarean delivery under spinal
anesthesia. In the present study, the systemic group,
TRSF, was subcutaneously injected with
fentanyl for comparison with the TRF group, in which
fentanyl was injected into TAP. The aim of the present study was to
investigate whether the analgesic effects of perineural fentanyl
are local or systemic, as the majority of previous studies
investigating the perineural application of fentanyl have not
included a systemic control group (10–13).
Materials and methods
Study subjects
The present study was approved by the Institutional
Ethics Committee of the Jiaxing Maternity and Children Health Care
Hospital (Jiaxing, China). Written informed consent was obtained
from all patients. A total of 150 nulliparous women (>37 weeks)
with an American Society of Anesthesiologists physical status I–II
(18) treated at the Jiaxing
Maternity and Children Health Care Hospital (Jiaxing, China) who
were scheduled for elective cesarean delivery via a Pfannenstiel
incision under spinal anesthesia, were enrolled in the present
study between September 2013 and December 2013. Patients were
excluded if they had a history of allergy to the drugs used in this
study, contraindications to neuraxial anesthesia, tolerance to
opioids or if they had used opioids within 48 h prior to the study.
Three patients were excluded after randomization due to epidural
supplementations; therefore, 147 patients were analyzed. In
addition, patients with a body mass index of >35 kg/m2 were
excluded.
US-guided TAP block procedure
No premedication was administered to the patients.
Upon arrival at the operating room, a 20-gauge IV cannula (BD
Biosciences, Franklin Lakes, NJ, USA) was inserted and standard
monitoring was performed, including electrocardiography, blood
oxygen saturation and non-invasive blood pressure measurements.
Patients were randomly assigned to one of three groups, as follows:
i) Group TR, receiving TAP block with 0.375% ropivacaine
(AstraZeneca, Södertälje, Sweden) (n=48); ii) group
TRSF, receiving TAP block with 0.375%
ropivacaine plus 50 µg subcutaneous fentanyl (Yichang Humanwell
Pharmaceutical Co., Ltd., Yichang, China) (n=49); and iii) group
TRF, receiving TAP block with a mixture of 0.375%
ropivacaine and 50 µg fentanyl (n=50). Randomization was achieved
using computer-generated codes created by SPSS 13.0 software (SPSS
Inc., Chicago, IL, USA), which were maintained in sequentially
numbered opaque envelopes prior to use. Spinal anesthesia was
initiated in all patients in the left lateral position at the L2-3
interspace with 10 mg isobaric bupivacaine (Shanghai Harvest
Pharmaceutical Co., Ltd., Shanghai, China) and 10 µg fentanyl,
using a combined spinal-epidural technique (19). If the sensory level did not reach the
T5 level after 15 min, or the patient complained of pain
intraoperatively, epidural supplementations of 2% lidocaine with
epinephrine (1:200,000; Shanghai Hui Pharmaceutical Co., Ltd.,
Shanghai, China) were administered via an indwelling epidural
catheter, and these patients were excluded from the present
study.
Immediately following the completion of surgery and
measurement of the residual block level, which assesses the level
of dermatomal sensory block of spinal anesthesia following surgery
via a pinprick, the patients underwent a US-guided bilateral TAP
block with 19 ml ropivacaine (0.375%) and 1 ml saline (groups
TR and TRSF) or 1 ml fentanyl (50
µg; group TRF) per side. The TAP block technique used
was similar to the method outlined in a previous study (20). Briefly, with the patient in the
supine position, an L38/10-5 MHz broadband linear array transducer
(SonoSite, Inc., Bothell, WA, USA) was placed transversely onto the
midaxillary line halfway between the iliac crest and the costal
margin, and was adjusted in order to obtain the best possible image
of the three muscle layers. A 100 mm 20-gauge short-bevel regional
block needle (Zhejiang Sujia Medical Equipment Co., Ltd., Jiaxing,
China) was introduced anteriorly through the skin, ~3–4 cm medial
to the US transducer, and was advanced into the fascial plane
between the internal oblique muscle and the transversus abdominis
muscle using an in-plane technique. The correct positioning of the
needle tip was confirmed with injection of 1 ml test dose, which
consisted of 0.375% ropivacaine in group TR and
TRSF, and a mixture of 0.375% ropivacaine and
50 µg fentanyl in group TRF, which resulted in
separation between the internal oblique and transversus abdominis
muscle. Subsequently, the remaining solution was injected in 5 ml
increments following careful aspiration under quantitative US
guidance. Thereafter, the needle was withdrawn to the subcutaneous
tissue, and the patients were subcutaneously administered with 1 ml
fentanyl (50 µg) in the TRSF group or 1 ml
saline in the TR and TRF groups. The same
steps were repeated on the contralateral side. All solutions were
prepared by a nurse anesthetist, who did not participate in the
study, and all procedures were performed by a single operator using
a sterile technique, including sterile gel and probe covers. The US
images were evaluated by an independent investigator, in order to
verify the needle placement and spreading of the solutions
administered.
Postoperative treatment
All patients were treated with a routine
postoperative analgesic regimen, consisting of 50 mg oral
diclofenac (Beijing Novartis Pharmaceutical Co., Ltd., Beijing,
China) and 300 mg rectal paracetamol (Northeast Pharmaceutical Co.,
Ltd., Shenyang, China) every 8 h, combined with patient-controlled
analgesia (PCA) with intravenous fentanyl (bolus dose, 30 µg;
lockout interval, 10 min) for 48 h postoperatively. The time to the
first PCA was recorded as the analgesic duration of the TAP block.
Patients were assessed at 2, 6, 12, 24 and 48 h postoperatively by
an investigator blinded to the group allocation. During each
assessment, cumulative and interval fentanyl consumptions, as well
as the pain severity at rest and during movement (knee flexion),
were recorded. The pain severity was quantified on a 10 cm visual
analog scale (VAS) pain score (21),
in which 0 indicated no pain and 10 indicated severe pain. In
addition, the patients were evaluated for sedation, nausea,
vomiting and complications that may have been associated with the
TAP block. A 4-point scale was used to evaluate the level of
sedation (1, fully awake; 2, somnolent, responding to verbal
stimuli; 3, somnolent, responding to tactile stimuli; and 4,
somnolent, responding to painful stimuli), and nausea severity (1,
none; 2, mild; 3, moderate; and 4, severe). An intravenous drip
administering 4 mg ondansetron was used in cases of reported nausea
and/or vomiting. At 48 h following surgery, the patients were asked
to rate their overall satisfaction with the postoperative pain
management on a 3-point scale: 1, highly satisfied; 2, satisfied;
and 3, dissatisfied.
Statistical analysis
Data are presented as the mean ± standard deviation,
median (range) and count (%), as appropriate. The primary outcome
was the time to first PCA, in which the present study hypothesized
that ≥60 min differences between the three groups were clinically
significant. Previous preliminary results obtained by the authors
of the present study involving 10 patients demonstrated the
duration of the TAP block with 0.375% ropivacaine alone was 140±80
min; therefore, a sample size of ≥47 patients per group was
required, with an alpha risk of 0.05 and a power of 0.8, to detect
this difference between groups. In order to account for any
drop-outs, a total of 50 patients were recruited for each group.
The secondary outcome measures included the cumulative and interval
PCA fentanyl consumptions, VAS pain scores at rest and during
movement, side effects and patient satisfaction. The data were
tested for normality using the Kolmogorov-Smirnov normality test.
Continuous measurements were compared among the groups using
repeated-measures or one-way analysis of variance if normally
distributed, or Kruskal-Wallis H test if abnormally distributed.
Categorical variables were compared using the the χ2 or Fisher's
exact test, as appropriate. All statistical analyses were conducted
using SPSS 13.0 software (SPSS, Inc.). The alpha level for all
analyses was set as P<0.05, and the Bonferroni correction for
multiple comparisons was used where appropriate.
Results
Study subjects
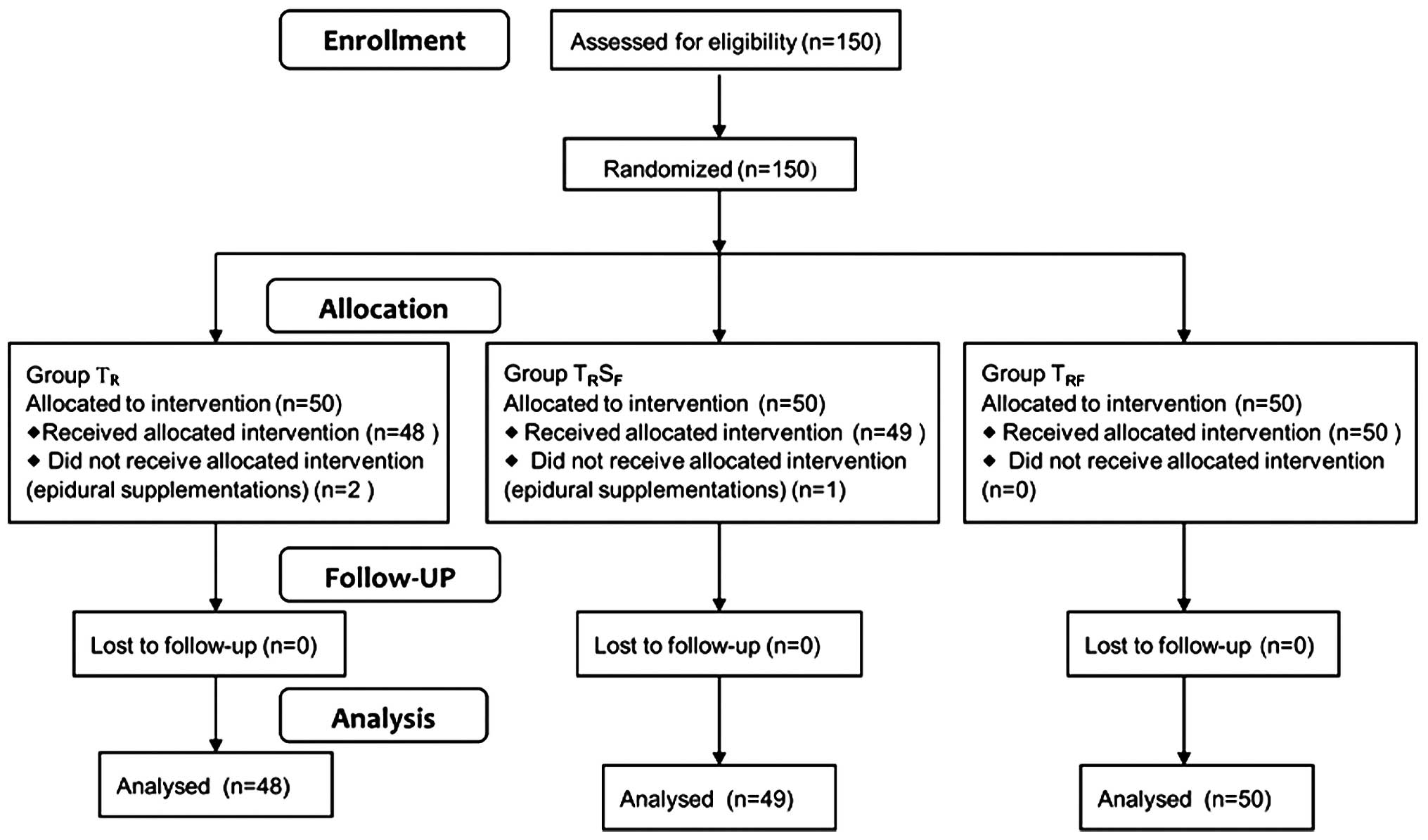
A total of 150 patients were enrolled in the present
study. Following randomization, 2 patients from group TR
and 1 patient from group TRSF were excluded
due to requiring intraoperative epidural supplementations; thus,
147 patients were analyzed (Fig. 1).
There were no statistically significant differences between the
groups in terms of patient characteristics, duration of surgery and
the residual block level at the end of surgery (Table I). The TAP was easily localized by an
US and blocks were uneventfully performed in all patients.
 | Table I.Patient characteristics, duration of
surgery and the block level at the end of surgery. |
Table I.
Patient characteristics, duration of
surgery and the block level at the end of surgery.
|
| Group TR
(n=48) | Group
TRSF (n=49) | Group TRF
(n=50) | P-value |
|---|
| Age, years |
27.0±3.4 |
27.8±3.4 |
27.2±4.1 | 0.653 |
| Weight, kg |
68.7±6.8 |
67.9±6.5 |
70.1±6.9 | 0.473 |
| Height, cm | 160.1±4.2 | 159.2±3.6 | 161.2±4.6 | 0.189 |
| Gestational age,
weeks |
38.9±1.1 |
38.7±1.6 |
39.1±1.2 | 0.438 |
| Duration of
surgery, min |
36.6±8.1 |
37.5±6.8 |
35.8±7.5 | 0.120 |
| Level of sensory
block | T6 (4–9) | T6 (4–8) | T5 (4–9) | 0.345 |
PCA
There was a tendency for earlier PCA in group
TR, as compared with the other two groups; however, the
difference was not significantly different among the three groups
(P=0.640). The median time to the first PCA was 150 min (range,
70–720 min) in group TR, 165 min (range, 90–670 min) in
group TRSF, and 190 min (range, 70–680 min)
in group TRF. Therefore, 2.5 µg/ml fentanyl, whether
administered via TAP or subcutaneous route, was not capable of
significantly prolonging the duration of analgesia, as compared
with ropivacaine alone for TAP block.
Fentanyl consumption and VAS pain
scores
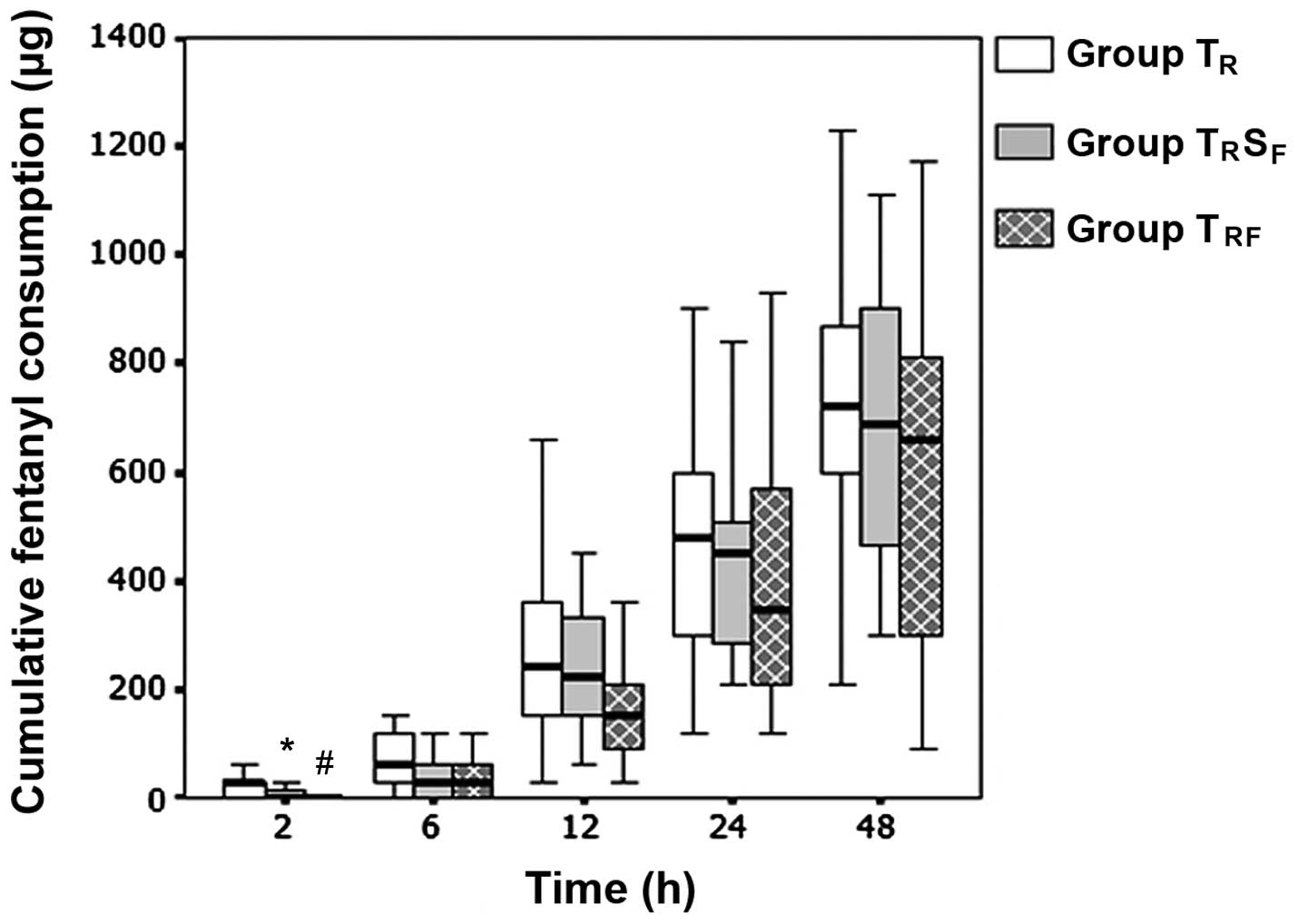
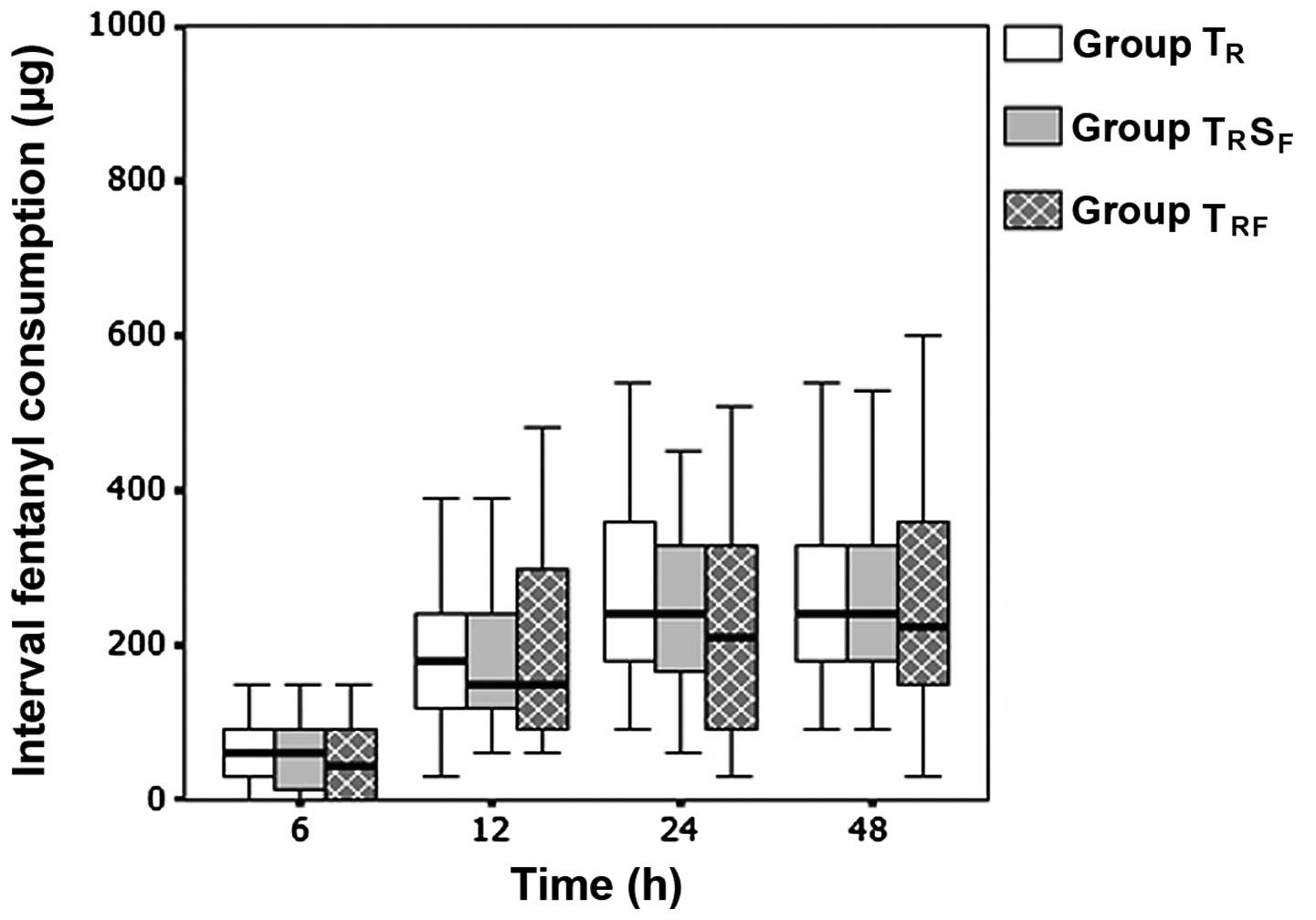
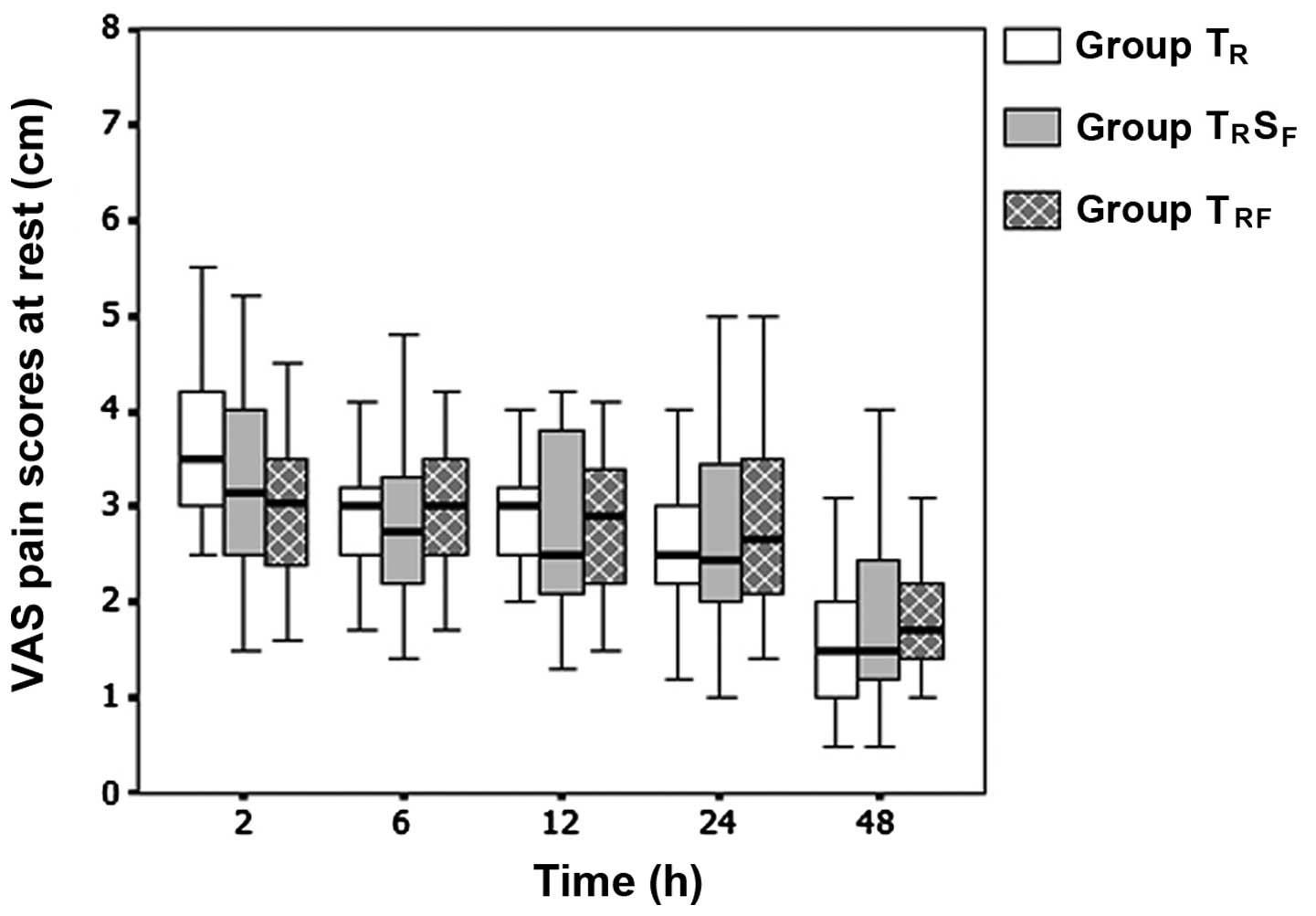
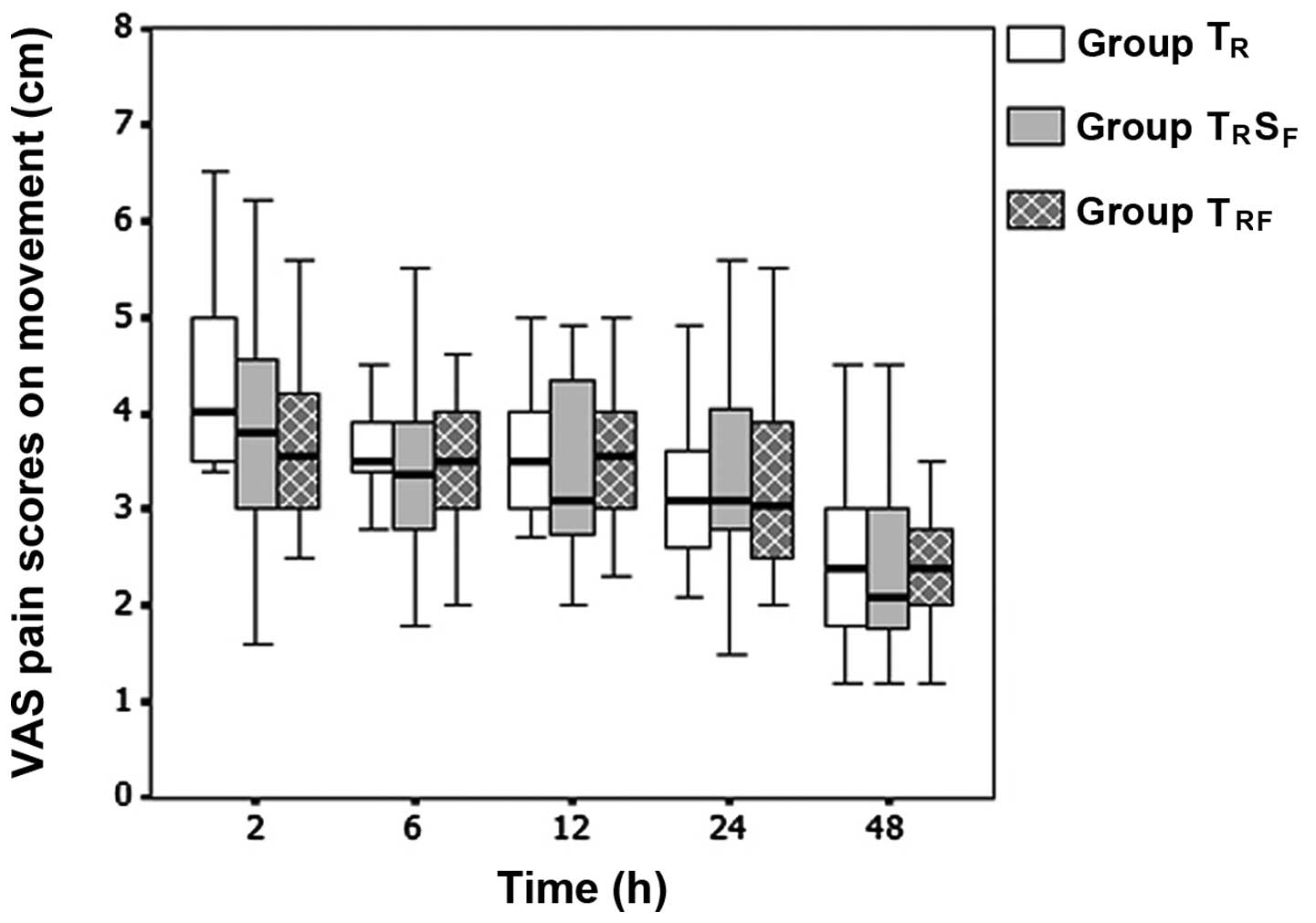
No statistically significant differences were
observed in the cumulative and interval fentanyl consumption
(Figs. 2 and 3) and the VAS pain scores at rest and
during movement (Figs. 4 and
5), among the three groups at all
time points. This indicated that the postoperative analgesic
quality was not improved when 2.5 µg/ml fentanyl was added to the
TAP block. However, the cumulative fentanyl consumption was
significantly lower in the TRSF and
TRFgroups at 2 h postoperatively (P=0.002 and 0.001,
respectively), as compared with that in group TR. By
contrast, no statistically significant difference in the cumulative
fentanyl consumption was observed at this time point between the
TRSF and TRF groups (P=0.273;
Fig. 2). Therefore, the early
analgesic-sparing effects following caesarean delivery in the TRSF
and TRF groups may be explained by the systemic absorption of
fentanyl. In addition, no significant differences were identified
in the postoperative sedation and nausea levels, number of patients
that reported vomiting, antiemetic requirements and patient
satisfaction with postoperative analgesia, among the three groups
(Table II). Furthermore, there were
no complications, such as LA systemic toxicity, vascular or
visceral injury, attributed to the TAP block in any of the
groups.
 | Table II.Sedation, nausea, vomiting and
patient satisfaction data. |
Table II.
Sedation, nausea, vomiting and
patient satisfaction data.
| Parameter | Group TR
(n=48) | Group
TRSF (n=49) | Group
TRF (n=50) | P-value |
|---|
| Sedation level |
|
|
|
|
| 2
h | 1 (1–2) | 1 (1–2) | 1 (1–2) | 0.971 |
| 6
h | 1 (1–2) | 1 (1–2) | 1 (1–2) | 0.774 |
| 12
h | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1.000 |
| 24
h | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1.000 |
| 48
h | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1.000 |
| Nausea
severity |
|
|
|
|
| 2
h | 1 (1–3) | 1 (1–3) | 1 (1–3) | 0.352 |
| 6
h | 1 (1–3) | 1 (1–3) | 1 (1–2) | 0.654 |
| 12
h | 1 (1–2) | 1 (1–2) | 1 (1–2) | 0.621 |
| 24
h | 1 (1–2) | 1 (1–2) | 1 (1–2) | 0.923 |
| 48
h | 1 (1–2) | 1 (1–2) | 1 (1–2) | 0.857 |
| Number of patients
reporting vomiting, n (%) | 7 (14.5) | 9 (18.3) | 11 (22.0) | 0.638 |
| Patient
satisfaction | 1 (1–3) | 1 (1–3) | 1 (1–2) | 0.502 |
Discussion
The results of the present study suggested that the
addition of 2.5 µg/ml fentanyl to the TAP block procedure (0.375%
ropivacaine) was unable to improve the duration and quality of
analgesia following caesarean delivery. In addition, as the
cumulative fentanyl consumption was significantly lower in the
TRSF and TRF groups at 2 h
postoperatively, as compared with that in group TR, the
early analgesic-sparing effect associated with perineural fentanyl
may have been mediated by systemic effects due to peripheral
uptake.
The TAP block is commonly used during a cesarean
delivery, in which it forms part of a multimodal postoperative
analgesic regimen (2–5). Previous studies have demonstrated that
a single injection of TAP block was able to significantly improve
post-cesarean analgesia in the absence of spinal morphine; however,
the analgesic duration was limited, as compared with intrathecal
morphine (2–4). Numerous analgesic adjuncts have been
added to LAs in various peripheral nerve blocks in order to improve
the analgesic duration (7); however,
the addition of analgesic adjuncts to the TAP block has rarely been
reported. A previous study has demonstrated that the addition of 8
mg dexamethasone to 20 ml bupivacaine (0.25%) in the TAP block was
associated with a longer time to the first PCA, lower postoperative
pain scores and reduced morphine requirements in patients
undergoing open abdominal hysterectomy (22). By contrast, Bollag et al
(23) reported that the addition of
75 µg clonidine to 0.375% bupivacaine in the TAP block did not
result in improved pain scores following cesarean delivery.
The existence of opioid receptors at peripheral
nerves and the LA-like action of various opioids, including
fentanyl and sufentanil, have been demonstrated in vitro
(6,8); however, there has been controversy
regarding the efficacy of the perineural application of opioids in
clinical trials. Murphy et al (24) reported that opioids had limited
benefits as analgesic adjuncts to the brachial plexus block,
whereas they were shown to exert a definite but mild analgesia
following intraarticular injection in another study (25). Fentanyl is an opioid that has been
widely used as an analgesic adjunct to LAs in clinical practice.
Previous studies have reported improved analgesia following the
addition of fentanyl to LAs in various nerve blocks, including the
axillary brachial plexus (9,10), cervical plexus (11), infraorbital nerve (12), caudal block (13) and paravertebral analgesia (14). Conversely, other studies (15–17) have
been unable to detect improved analgesia following
co-administration of LAs and fentanyl. The conflicting findings of
previous studies may be due to differences in the concentrations
and doses used, as well as due to methodological differences in the
study design, including a lack of systemic control groups, and the
site and technique of nerve blocks. To the best of our knowledge,
the present study is the first to investigate the effects of
fentanyl addition to the TAP block on postoperative analgesia. A
2.5 µg/ml fentanyl dose (total dose, 100 µg) was selected in the
present study, since previous studies have demonstrated that this
concentration of fentanyl was able to significantly improve the
effectiveness of peripheral nerve blocks (9–11,14).
Furthermore, this dose was selected due to concerns regarding
potential dose-dependent adverse systemic effects associated with
fentanyl.
The present study demonstrated that the addition of
2.5 µg/ml fentanyl to ropivacaine was unable to affect the TAP
block analgesia following cesarean delivery, as assessed by the
duration of analgesia, VAS pain scores and post-surgery analgesic
requirements. The reduced requirement for additional analgesia in
the TRSF and TRF groups during the
first 2 h postoperation, as compared with the TR group,
may have been due to the systemic effects of fentanyl, since no
significant difference was detected between the
TRSF and TRF groups. The reasons
why fentanyl was unable to improve the analgesia of the TAP block
are unclear. One plausible explanation may be that fentanyl was
unable to diffuse through the nerve sheath (8). In addition, the median time to first
PCA was markedly shorter in the present study, as compared with
those reported in previous studies, including 220 min (150–380 min)
(2), 3 h (inter-quartile range, 1 h)
(3) and 4 h (0.5–29 h) (4). This may be due to the higher doses of
bupivacaine and fentanyl used for the spinal anesthesia, and the
higher concentrations (and doses) of LAs used for the TAP block in
previous studies (2–4), as compared with the present study.
A limitation of the present study was that the
extent of abdominal wall sensory block following the TAP block was
not assessed, due to a residual sensory block from spinal
anesthesia in the early postoperative period; thus, the failed
blocks were not excluded. However, the TAP blocks were conducted by
an experienced operator, and the US approach allowed for direct
visualization of the needle and of the placement of LAs, which
should have reduced the risk of block failure. Another limitation
was the relatively low concentration of fentanyl used, and the fact
that other adjuncts, including epinephrine, were not assessed in
the present study. Therefore, whether a higher concentration of
fentanyl, or a combination of fentanyl and epinephrine, may improve
the analgesic efficacy of the TAP block should be the focus of
future studies. Large individual variations were detected in
post-cesarean delivery analgesia in the present study, which may be
associated with the characteristics of post-operative analgesia per
se or an inadequate sample size, which may limit the conclusions of
the present study.
In conclusion, the results of the present study
suggested that the addition of 2.5 µg/ml fentanyl to 0.375%
ropivacaine was unable to improve the TAP block analgesia following
cesarean delivery under spinal anesthesia. Future studies should
endeavour to investigate other measures, including the application
of the continuous catheter-based technique, that may prolong the
postoperative analgesic duration of the TAP block.
References
|
1
|
McDonnell JG, O'Donnell B, Curley G,
Heffernan A, Power C and Laffey JG: The analgesic efficacy of
transversus abdominis plane block after abdominal surgery: A
prospective randomized controlled trial. Anesth Analg. 104:193–197.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
McDonnell JG, Curley G, Carney J, Benton
A, Costello J, Maharaj CH and Laffey JG: The analgesic efficacy of
transversus abdominis plane block after cesarean delivery: A
randomized controlled trial. Anesth Analg. 106:186–191. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Belavy D, Cowlishaw PJ, Howes M and
Phillips F: Ultrasound-guided transversus abdominis plane block for
analgesia after caesarean delivery. Br J Anaesth. 103:726–730.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kanazi GE, Aouad MT, Abdallah FW, Khatib
MI, Adham AM, Harfoush DW and Siddik-Sayyid SM: The analgesic
efficacy of subarachnoid morphine in comparison with
ultrasound-guided transversus abdominis plane block after cesarean
delivery: A randomized controlled trial. Anesth Analg. 111:475–481.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Abdallah FW, Halpern SH and Margarido CB:
Transversus abdominis plane block for postoperative analgesia after
caesarean delivery performed under spinal anaesthesia? A systematic
review and meta-analysis. Br J Anaesth. 109:679–687. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Stein C and Lang LJ: Peripheral mechanisms
of opioid analgesia. Curr Opin Pharmacol. 9:3–8. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Axelsson K and Gupta A: Local anaesthetic
adjuvants: Neuraxial versus peripheral nerve block. Curr Opin
Anaesthesiol. 22:649–654. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gissen AJ, Gugino LD, Datta S, Miller J
and Covino BG: Effects of fentanyl and sufentanil on peripheral
mammalian nerves. Anesth Analg. 66:1272–1276. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nishikawa K, Kanaya N, Nakayama M,
Igarashi M, Tsunoda K and Namiki A: Fentanyl improves analgesia but
prolongs the onset of axillary brachial plexus block by peripheral
mechanism. Anesth Analg. 91:384–387. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Karakaya D, Büyükgöz F, Bariş S, Güldoğuş
F and Tür A: Addition of fentanyl to bupivacaine prolongs
anesthesia and analgesia in axillary brachial plexus block. Reg
Anesth Pain Med. 26:434–438. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sindjelic RP, Vlajkovic GP, Davidovic LB,
Markovic DZ and Markovic MD: The addition of fentanyl to local
anesthetics affects the quality and duration of cervical plexus
block: A randomized, controlled trial. Anesth Analg. 111:234–237.
2010.PubMed/NCBI
|
|
12
|
Mane RS, Sanikop CS, Dhulkhed VK and Gupta
T: Comparison of bupivacaine alone and in combination with fentanyl
or pethidine for bilateral infraorbital nerve block for
postoperative analgesia in pediatric patients for cleft lip repair:
A prospective randomized double blind study. J Anaesthesiol Clin
Pharmacol. 27:23–26. 2011.PubMed/NCBI
|
|
13
|
Constant I, Gall O, Gouyet L, Chauvin M
and Murat I: Addition of clonidine or fentanyl to local
anaesthetics prolongs the duration of surgical analgesia after
single shot caudal block in children. Br J Anaesth. 80:294–298.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Burlacu CL, Frizelle HP, Moriarty DC and
Buggy DJ: Fentanyl and clonidine as adjunctive analgesics with
levobupivacaine in paravertebral analgesia for breast surgery.
Anaesthesia. 61:932–937. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Fanelli G, Casati A, Magistris L, Berti M,
Albertin A, Scarioni M and Torri G: Fentanyl does not improve the
nerve block characteristics of axillary brachial plexus anaesthesia
performed with ropivacaine. Acta Anaesthesiol Scand. 45:590–594.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fletcher D, Kuhlman G and Samii K:
Addition of fentanyl to 1.5% lidocaine does not increase the
success of axillary plexus block. Reg Anesth. 19:183–188.
1994.PubMed/NCBI
|
|
17
|
Johansson A, Kornfält J, Nordin L,
Svensson L, Ingvar C and Lundberg J: Wound infiltration with
ropivacaine and fentanyl: Effects on postoperative pain and PONV
after breast surgery. J Clin Anesth. 15:113–118. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
American Society of Anesthesiologists: New
classification of physical status. Anesthesiology. 24:1111963.
|
|
19
|
Birnbach DJ and Ojea LS: Combined
spinal-epidural (CSE) for labor and delivery. Int Anesthesiol Clin.
40:27–48. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hebbard P, Fujiwara Y, Shibata Y and Royse
C: Ultrasound-guided transversus abdominis plane (TAP) block.
Anaesth Intensive Care. 35:616–617. 2007.PubMed/NCBI
|
|
21
|
DeLoach LJ, Higgins MS, Caplan AB and
Stiff JL: The visual analogue scale in the immediate postoperative
period: intrasubject variability and correlation with a numeric
scale. Anesth Analg. 86:102–106. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ammar AS and Mahmoud KM: Effect of adding
dexamethasone to bupivacaine on transversus abdominis plane block
for abdominal hysterectomy: A prospective randomized controlled
trial. Saudi J Anaesth. 6:229–233. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Bollag L, Richebe P, Siaulys M, Ortner CM,
Gofeld M and Landau R: Effect of transversus abdominis plane block
with and without clonidine on post-cesarean delivery wound
hyperalgesia and pain. Reg Anesth Pain Med. 37:508–514. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Murphy DB, McCartney CJ and Chan VW: Novel
analgesic adjuncts for brachial plexus block: A systematic review.
Anesth Analg. 90:1122–1128. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Gupta A, Bodin L, Holmström B and Berggren
L: A systematic review of the peripheral analgesic effects of
intraarticular morphine. Anesth Analg. 93:761–770. 2001. View Article : Google Scholar : PubMed/NCBI
|