Introduction
Osteonecrosis of the femoral head (ONFH), also known
as avascular necrosis of the femoral head (AVNFH), is a common,
intractable disease. It is a multifactorial disease that occurs at
any age and presents clear clinical symptoms (1). The etiology of the disease, however,
remains unclear, although common contributors are long-term use of
hormones, chronic alcoholism and smoking (2). Approximately 80% of untreated patients
present with femoral head collapse (3). As the incidence of ONFH in adults is
rising, early diagnostic methods and related treatments are
increasingly being developed. Total hip replacement is being
performed more often in young patients, for instance, and should be
approached with great care. Maintaining the integrity of the
femoral head is considered a particularly important topic. Another
significant consideration is how to prevent collapse of a necrotic
femoral head and thus delay joint replacement. Transplantation of
vascularized bone flap grafts not only provides mechanical support
and prevents collapse of the femoral head but also offers a new
source of blood supply, thereby improving blood circulation of the
necrotic femoral head (2). There are
numerous methods of using vascularized bone flap grafts, but the
use of iliac bone flaps pedicled with sartorius muscular fascia
around superficial circumflex iliac vessels is rarely reported.
This study aimed to evaluate the efficacy of iliac bone flaps
pedicled with sartorius muscular fascia around superficial
circumflex iliac vessels for the treatment of ARCO stage II–III
ONFH in young adults.
Materials and methods
General information
Inclusion criteria
Inclusion criteria for the study included the
following: i) Patients had complete data that included clinical and
follow-up material; ii) the affected hip had not undergone surgery;
iii) etiological factors had already been removed, for example,
alcohol drinkers became abstinent and patients taking hormones
stopped using them; iv) patients were aged 10–65 years, with the
diagnosis of ONFH at ARCO stage II–III; v) the femoral head was
intact with no evident collapse and no osteoarthritis; vi) imaging
indicated that femoral head collapse was <2 mm; vii) the lesions
were small or medium sized (<50%); viii) patients were in good
health and had no other complications, including cerebrovascular,
severe heart and lung disease; ix) patients were able to tolerate
surgery; and x) patients and their families requested and agreed
with this surgical treatment.
Exclusion criteria
Exclusion criteria for this study were as follows:
i) Incomplete follow-up results or clinical information that could
not be supplemented; ii) other treatment methods had been used on
the affected hip and it was inappropriate to use this surgical
treatment; iii) risk factors, including drinking and hormone use,
were not removed; iv) patients were senile, aged >65 years, with
the diagnosis of ONFH at ARCO stage IV; v) the femoral head
exhibited collapse and symptoms of osteoarthritis; vi) imaging
indicated that femoral head collapse was >2 mm; vii) patients
had large-sized lesions (>50%); viii) patients were overly obese
or had respiratory, urinary and/or other infections; ix) patients
had mental illness and were unable to cooperate with the treatment;
and x) patients and their families did not agree with the use of
this method.
Patients
In strict accordance with the inclusion and
exclusion criteria, a total of 35 patients (43 hips) were included
in this study, including 27 male and 8 female patients, with both
hips in 8 cases and a single hip in 27 cases. The included patients
were 14–63 years of age, with a mean of 40.26±10.28 years (Table I). The preoperative imaging data were
evaluated by two orthopedic specialists and according to ARCO
staging. There were 14 stage IIA hips, 8 stage IIB hips, 9 stage
IIC hips, 8 stage IIIA hips, 3 stage IIIB hips and 1 stage IIIC
hip. Preoperatively, the incidence rates of these stages were
32.56, 18.60, 20.93, 18.60, 6.98 and 2.33%, respectively (Table II). The etiology of the ONFH was
steroid use in 14 patients, alcohol in 13 patients, trauma in 4
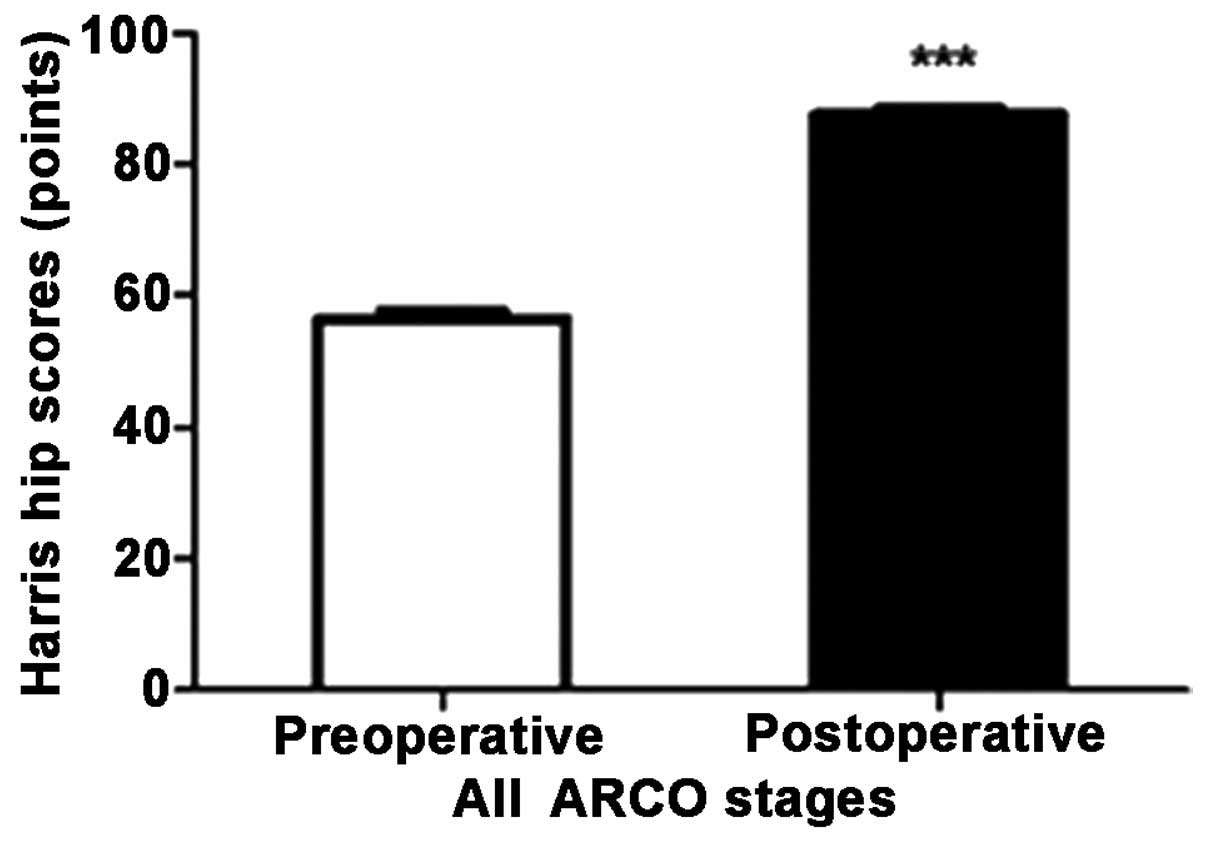
patients and uncertain in 4 patients. The Harris hip scores (HHSs)
ranged from 44 to 72 points preoperatively, average 56.53±7.66
points (Fig. 1). The patients with
steroid-induced ONFH had discontinued steroid application and the
patients with alcohol-induced ONFH had abstained for ≥3 months
prior to admission. The lengths of the affected limbs and their
contralateral limbs were measured preoperatively in all patients.
The difference between the two limbs was <1 cm.
 | Table I.General information of the
patients. |
Table I.
General information of the
patients.
| Variable | Minimum | Maximum | Mean ± SD |
|---|
| Age (years) | 14 | 63 |
40.26±10.28 |
| Follow-up time
(months) |
3 | 96 |
41.71±24.26 |
| Surgery time
(min) | 105 | 320 |
182.71±51.14 |
| Intraoperative blood
loss (ml) | 100a | 1,000b |
478.51±261.58 |
| Hospital stay
(days) | 11 |
36 |
20.29±5.82 |
 | Table II.ARCO stages and incidence rates. |
Table II.
ARCO stages and incidence rates.
|
| Preoperative | Postoperative |
|---|
|
|
|
|
|---|
| ARCO stage | No. of hips | Incidence rate
(%) | No. of hips | Incidence rate
(%) |
|---|
| IIA | 14 |
32.56 | 16 |
37.21 |
| IIB | 8 |
18.60 | 7 |
16.28 |
| IIC | 9 |
20.93 | 8 |
18.60 |
| IIIA | 8 |
18.60 | 9 |
20.93 |
| IIIB | 3 | 6.98 | 2 | 4.65 |
| IIIC | 1 | 2.33 | 1 | 2.33 |
| Total | 43 | 100.00 | 43 | 100.00 |
Surgical methods
The surgical strategy comprised six steps. i)
Incision: A modified hip anterolateral incision, also known as a
modified Smith-Peterson incision, in which an incision starting
from the middle of the iliac crest was continued along the outer
lip of the iliac crest to the anterior superior iliac spine, and
then turned down for a posterolateral curved extension of 10–12 cm.
ii) Release and exposure: After the skin, subcutaneous tissue and
fascia latae were cut, between the subcutaneous tissue and the
fascia layer, the fascia around the sartorius was freed to a
sufficient size. As the superficial circumflex iliac vessels are
contained in this fascia, care should be taken not to damage it in
during the surgery. Along the gap between the tensor fascia latae
and sartorius muscles, from the outer lip of the iliac crest, the
origin of the tensor fascia latae was peeled from the outer lip of
the iliac crest. The vascular branching between the sartorius and
tensor fascia latae muscles was ligated in order to reduce
bleeding. After retracting the tensor fascia latae muscle and
sartorius, the deep rectus femoris was exposed. The origin of the
rectus femoris and iliopsoas was then freed. From the anterior
superior iliac spine, at the origin of the sartorius, the sartorius
muscular fascia around the superficial circumflex iliac vessels was
freed again. The reflected head of the rectus femoris, part of the
hip joint capsule, was removed from the acetabulum and the hip
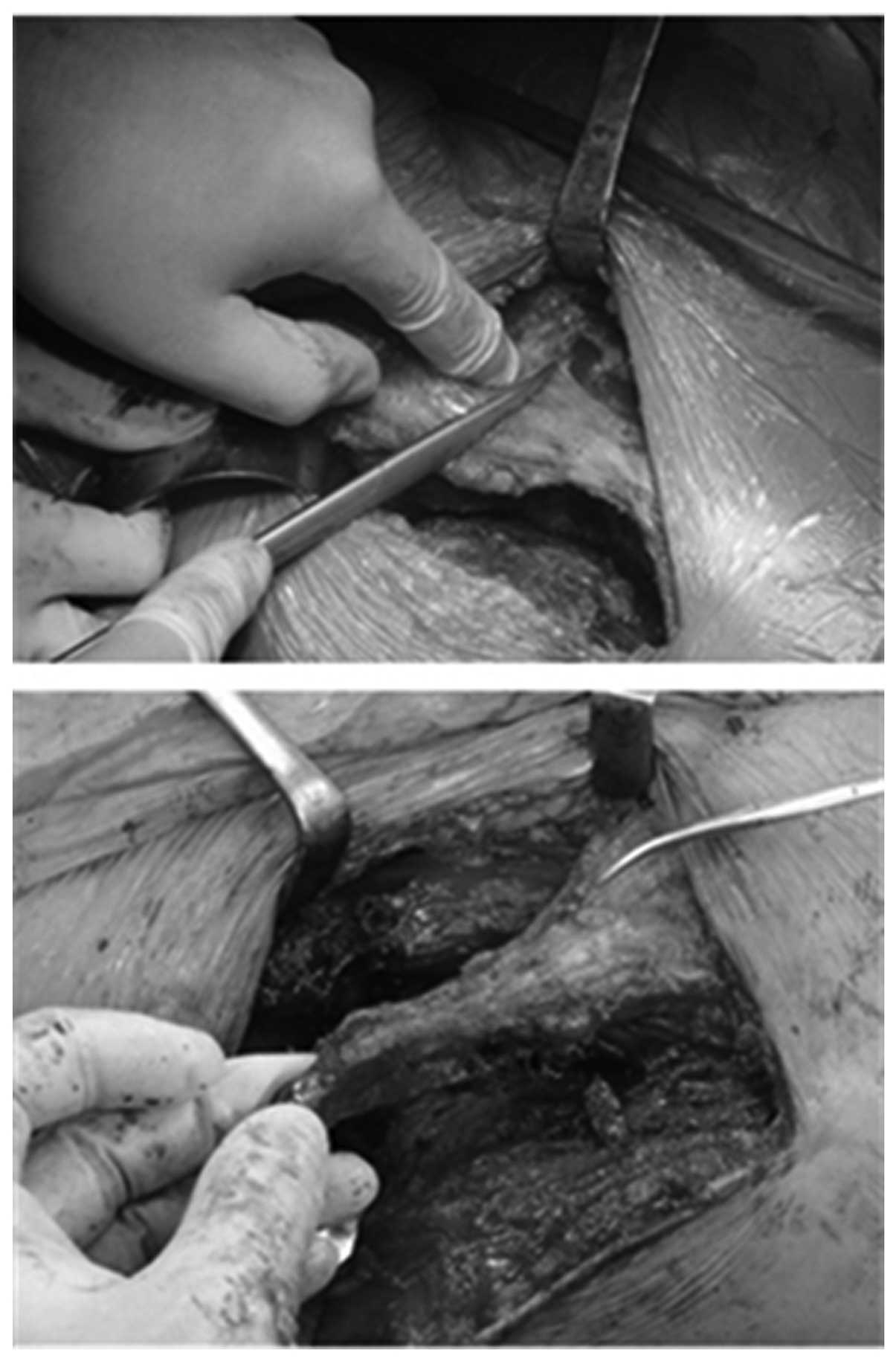
joint capsule was exposed. iii) Decompression by fenestration:
Following the opening of the joint capsule and protection of the
articular cartilage, a bone trough measuring 2×1 cm was established
in front of the junction of the femoral head and neck. Hardened or
cystic lesions around the femoral head were removed using a spatula
scraper or small chisel. When the subchondral femoral head had been
cleaned, it was rinsed with saline. iv) Dissociating and harvesting
the bone flap: The superficial circumflex iliac vessels and
surrounding fascia were isolated, a rectangular bone flap,
measuring 3×2 cm, was cut from the origin of the sartorius at the
anterior superior iliac spine along the iliac crest and trimmed.
Blood circulation of the bone flap was observed while a section of
iliac cancellous bone was harvested by rongeur to fill the space
around the bone flap after the bone flap was implanted. A gelatin
sponge was used for hemostasis. v) Bone flap and implantation: The
iliac flap penetrated the iliopsoas and rectus femoris muscle to
the bone trough in front of the junction between the femoral head
and neck. The bone flap was trimmed again and implanted into the
bone trough; the proximal end was inserted into the femoral head,
and if there was any space around the bone flap, it was filled with
iliac cancellous bone or allogeneic bone. vi) Bone grafting and
fixation: The bone flap was fixed with 1 or 2 absorbable screws
(Fig. 2).
All of the patients were supplied with preemptive
analgesia with analgesics preoperatively, massaged at the adductor
muscle to relieve tension and pressure within the femoral head,
treated with antibiotics at 30 min preoperatively, intraoperatively
and postoperatively to prevent infection, and were also treated
with drugs to promote bone microcirculation and to relieve pain.
The negative pressure drainage tube was removed 24–48 h after the
surgery. The affected hip was placed in 30° flexion and mild
pronation for ≥6 weeks. It was subject to skin traction braking for
6 weeks. During braking, patients underwent training for ankle
joint flexion and isometric contraction of the quadriceps femoris.
Three months later, patients were allowed to walk on crutches while
bearing weight. The walking distance was restricted to a maximum of
500 m and the walking time to a maximum of 30 min each time. At 6
months, the affected limbs were able to bear progressive amounts of
while walking. The walking distance and time were restricted to
1,000 m and 1 h, respectively, each time. At 9 months, the patients
were allowed to walk with only one crutch while bearing weight. The
walking distance and time were restricted to 2,000 m and 2 h,
respectively. The use of crutches was discontinued at 1 year. All
patients were followed up at 1, 3, 6, 9 months and 1 year
postoperatively with radiography to confirm normal pelvic anatomy,
computed tomography (CT) or emission computed tomography (ECT) and
magnetic resonance imaging (MRI) to evaluate the survival of the
bone flap and to adjust the strategy of functional rehabilitation
exercise.
Main outcome measures
Joint function was assessed using the HHS (total 100
points), which included assessment of pain (total 44 points), joint
function (total 47 points), range of motion (total 5 points) and
deformity (total 4 points). The excellent, good and poor ratings
corresponded to HHSs of 90–100, 80–89 and <80 points,
respectively. All patients were subjected to pelvic radiography, CT
and MRI evaluation of the femoral head, and systemic bone ECT at
the final follow-up. The findings were compared with preoperative
imaging data to determine if there were any changes in staging. The
clinical success rate was defined on the basis of excellent and
good ratings determined by HHS and no changes in ARCO stage.
Statistical analysis
Collected data were analyzed using SPSS software,
version 21.0 (SPSS, Inc., Chicago, IL, USA) with a paired sample
t-test. P<0.05 was considered to indicate a significant
difference. The results are expressed as the mean ± standard
deviation.
Results
General observations
The 35 patients were followed up postoperatively for
3–96 months (mean, 41.71±24.26 months; Table I). All patients underwent
transplantation of iliac bone flaps pedicled with sartorius
muscular fascia around superficial circumflex iliac vessels. The
surgery duration (including anesthesia time) ranged from 105 to 320
min, with an average of 182.71±51.14 min (Table I). Intraoperative blood loss ranged
from 100 ml unilaterally to 1,000 ml bilaterally (mean,
478.51±261.58 ml; Table I). The
hospital stay was 11–36 days (mean, 20.29±5.82 days; Table I).
HHS
Overall
The HHS improved significantly from the preoperative
status of 56.53±7.66 points to the postoperative status of
87.49±5.89 points (P<0.0001, t-test; Fig. 1). Preoperatively, the maximum score
was 72 points and the minimum score was 44 points; postoperatively,
the maximum score was 97 points and the minimum score was 75
points. A HHS of <80 points was observed in 3 patients;
therefore, the clinical success rate was 91.43%.
HHS according to ARCO stage
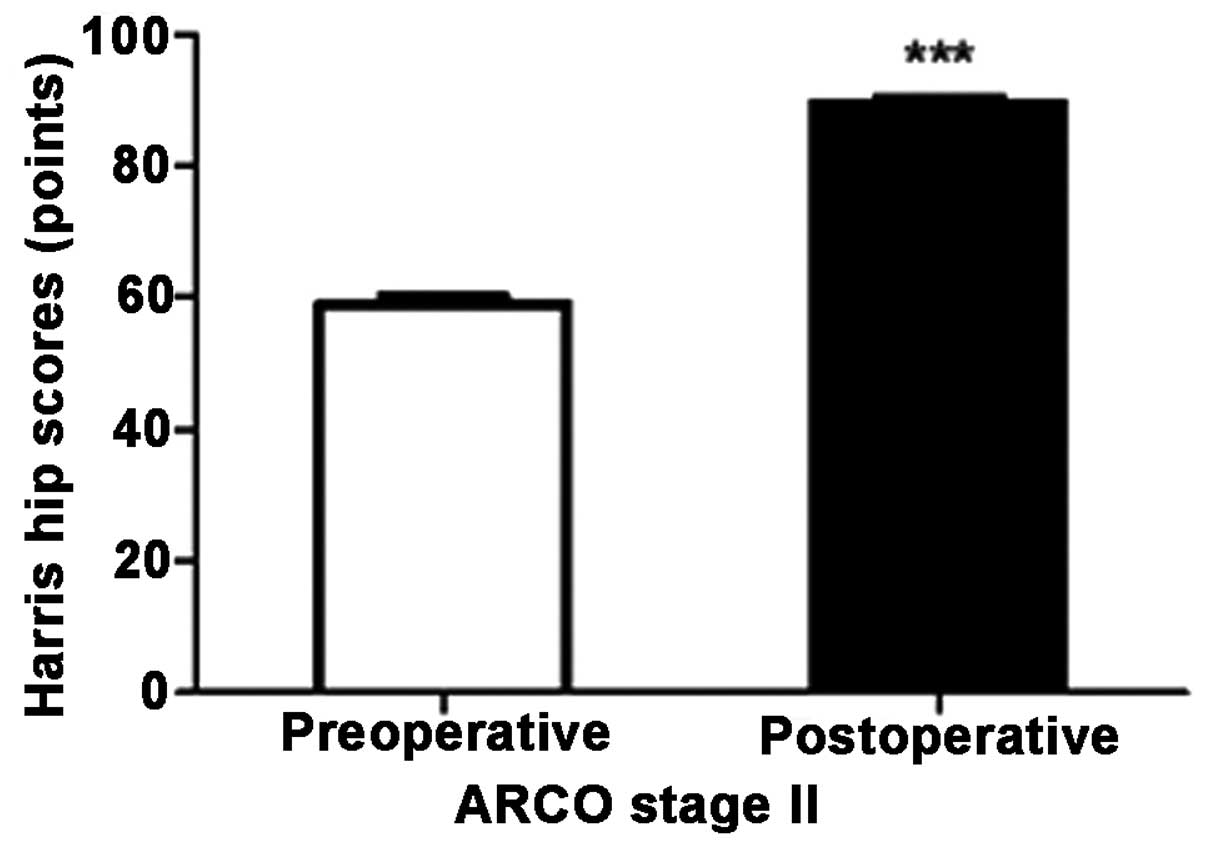
Statistical analysis based on ARCO stage revealed
that the HHS of ARCO stage II improved significantly from a
preoperative status of 58.94±7.13 points to a postoperative status
of 89.55±4.65 points (P<0.0001; Table III). Preoperatively, the maximum
score was 72 points and the minimum was 47 points; at follow-up,
the maximum score was 97 points and the minimum was 87 points
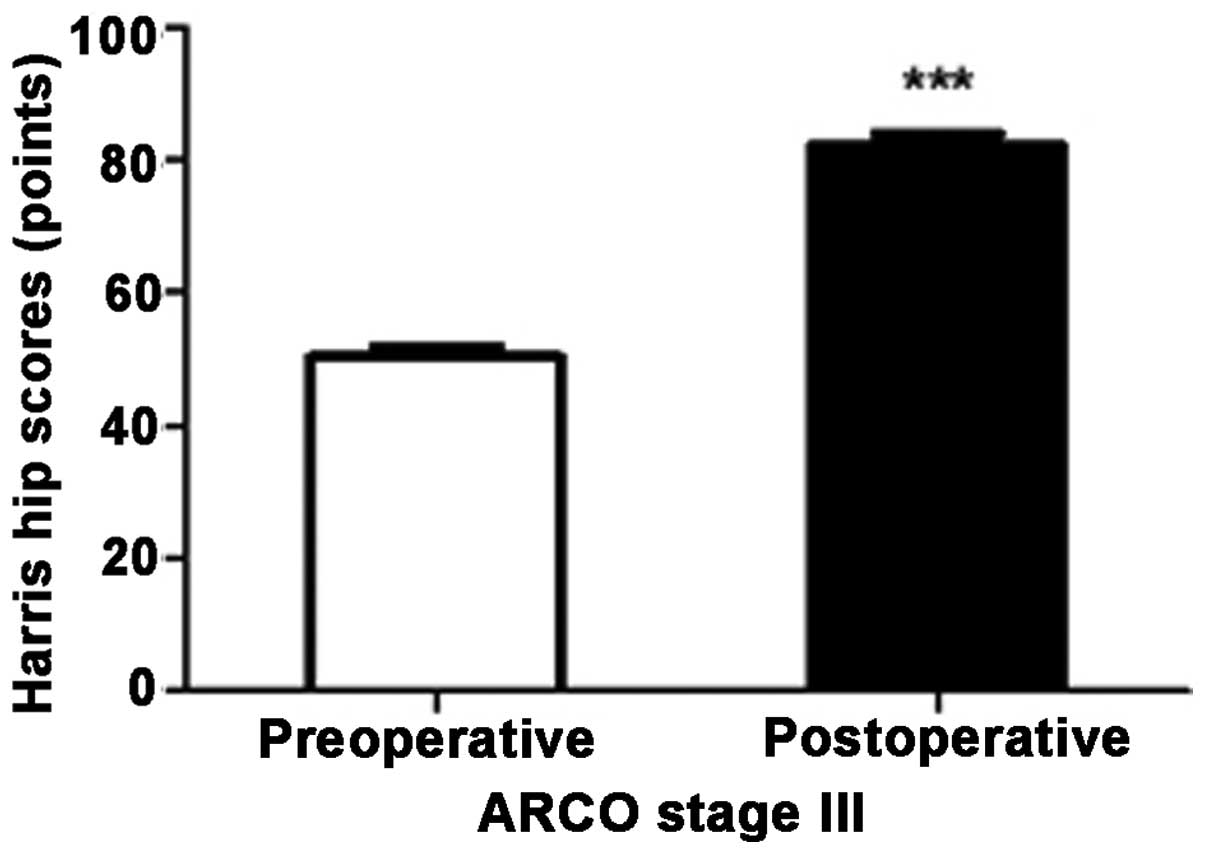
(Fig. 3). The HHS of ARCO stage III
improved significantly from a preoperative status of 50.33±5.71
points to a postoperative status of 82.17±5.81 points (P<0.0001;
Table III). Preoperatively, the
maximum score was 62 points and the minimum was 44 points; at
follow-up the maximum score was 91 points and the minimum was 75
points (Fig. 4).
 | Table III.Harris hip scores of different ARCO
stages prior to surgery and at the last follow-up. |
Table III.
Harris hip scores of different ARCO
stages prior to surgery and at the last follow-up.
|
|
| Mean HHS
(points) |
|
|---|
|
|
|
|
|
|---|
| ARCO stage | No. of hips | Preoperative | Postoperative | P-value |
|---|
| Stage II | 31 | 58.94±7.13 | 89.55±4.65 | <0.0001 |
| Stage III | 12 | 50.33±5.71 | 82.17±5.81 | <0.0001 |
| Total | 43 | 56.53±7.66 | 87.49±5.89 | <0.0001 |
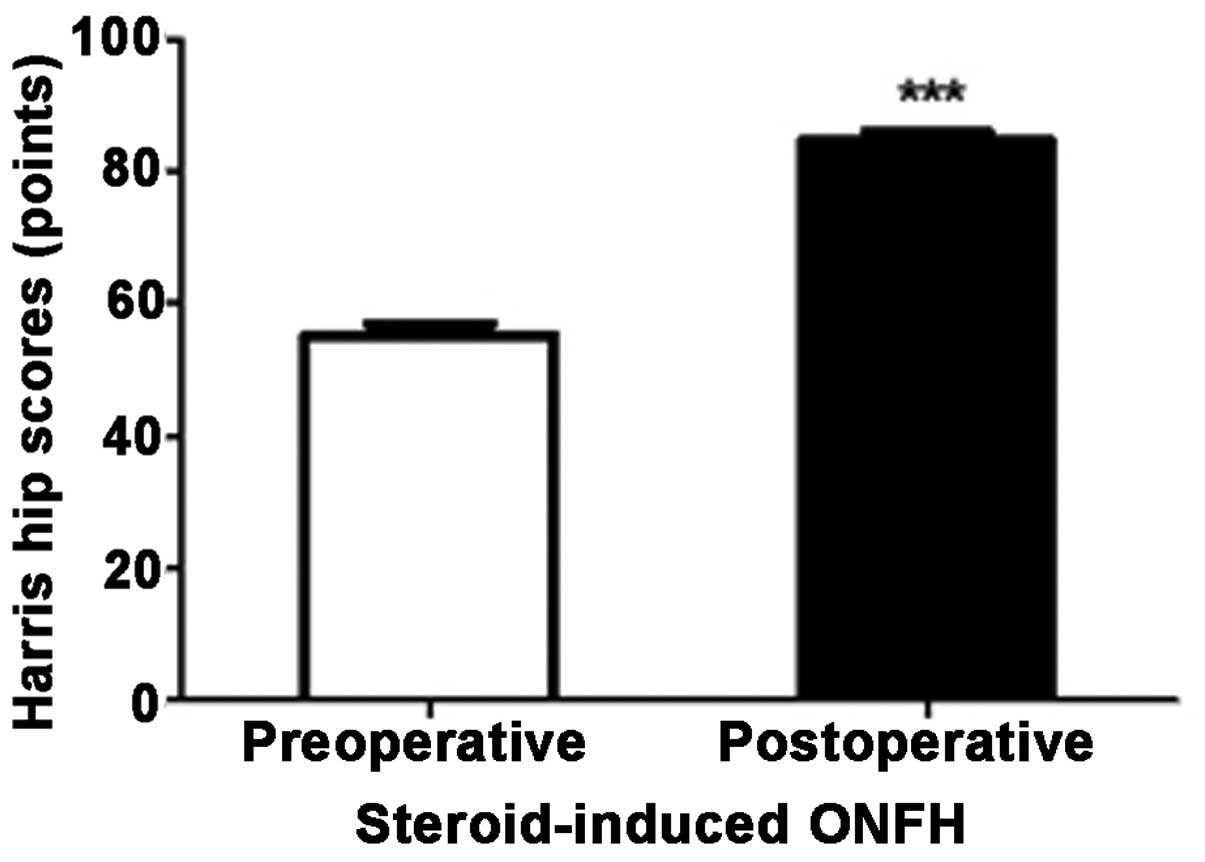
HHS according to etiology
The HHS of steroid-induced ONFH improved
significantly from a preoperative status of 55.28±6.98 points to a
postoperative status of 84.56±5.86 points (P<0.0001; Table III). Preoperatively, the maximum
score was 66 points and the minimum was 45 points; at follow-up the
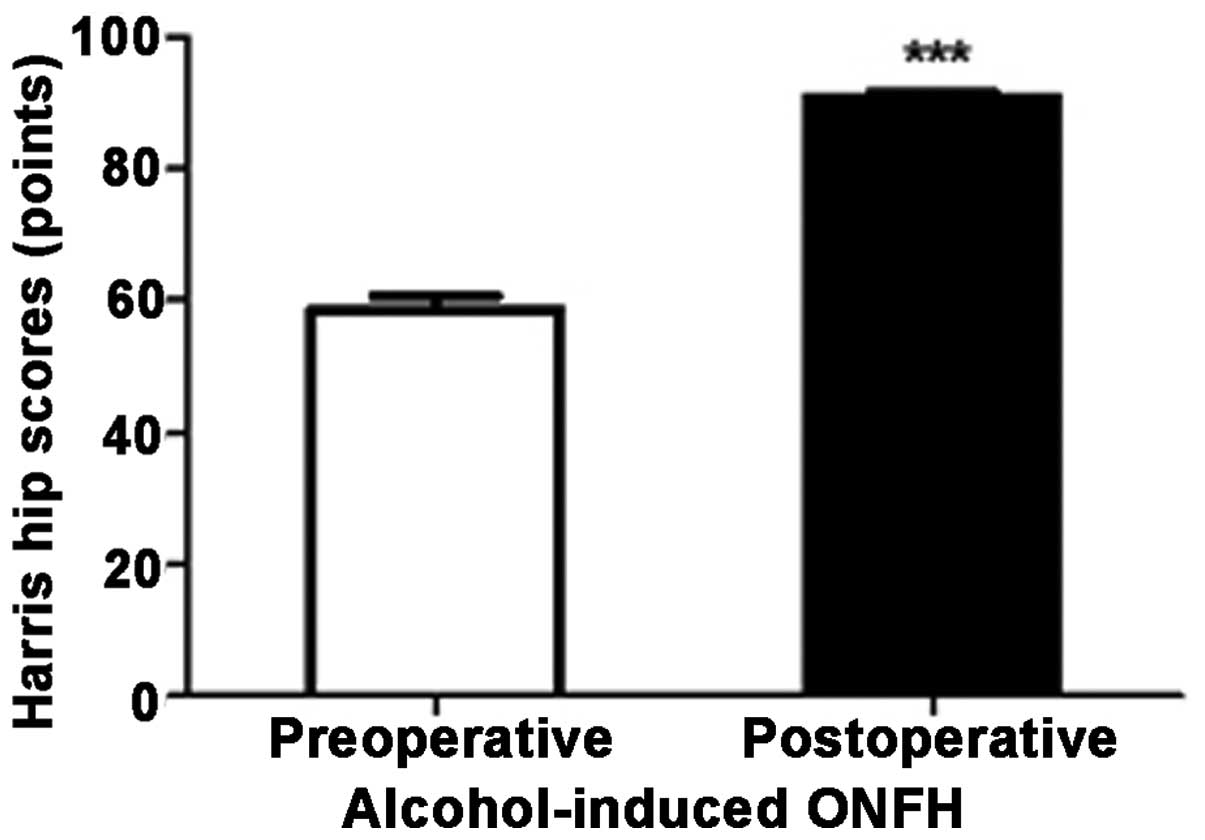
maximum score was 94 points and minimum was 75 points (Fig. 5). Alcohol-induced ONFH improved
significantly from a preoperative status of 58.50±8.26 points to a
postoperative status of 90.75±3.09 points (P<0.0001; Table IV). Preoperatively, the maximum
score was 72 points and the minimum was 46 points; at follow-up the
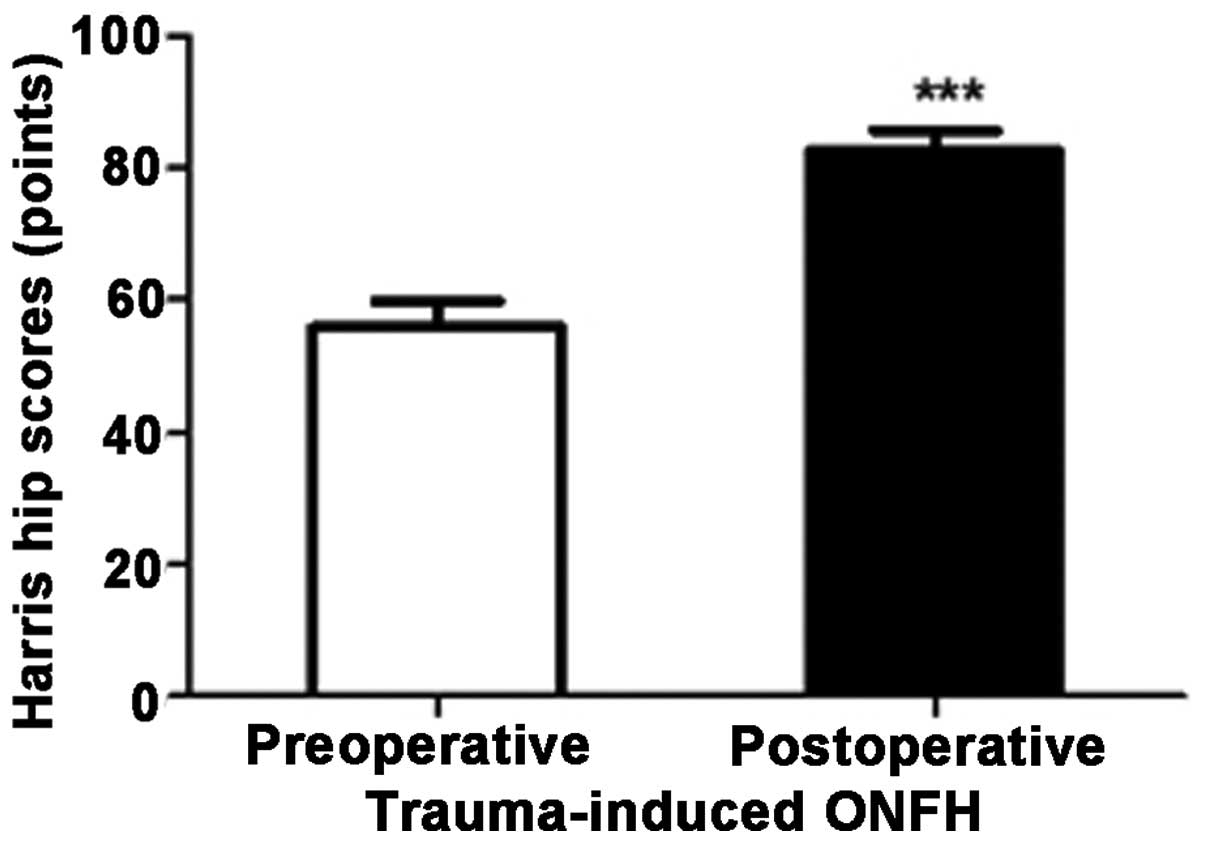
maximum score was 96 points and minimum was 85 points (Fig. 6). Trauma-induced ONFH improved
significantly from a preoperative status of 55.75±8.26 points to a
postoperative status of 82.50±6.35 points (P=0.002; Table III). Preoperatively, the maximum
score was 62 points and the minimum was 44 points; at follow-up,
the maximum score was 91 points and the minimum was 76 points
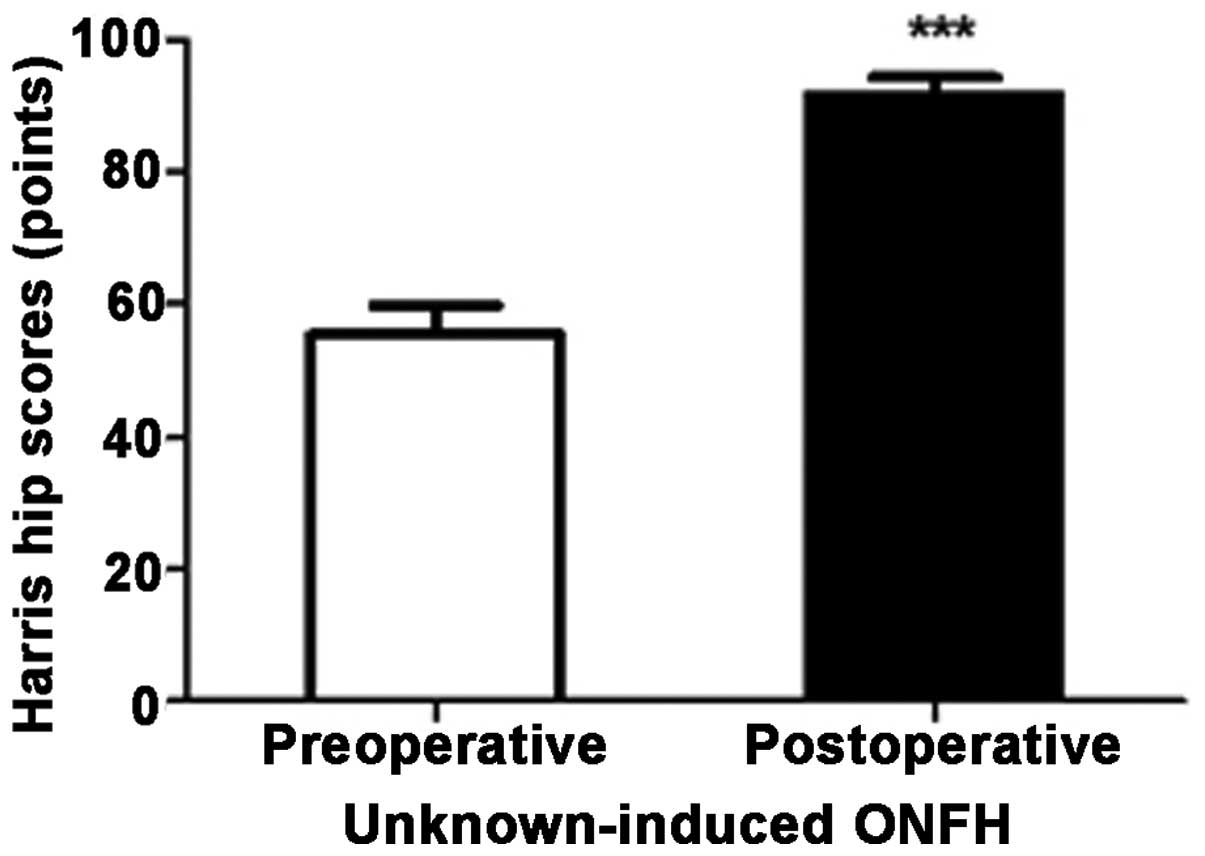
(Fig. 7). ONFH of unknown etiology
improved significantly from a preoperative status of 55.40±9.61
points to a postoperative status of 91.60±5.81 points (P=0.001;
Table III). Preoperatively, the
maximum score was 72 points and the minimum was 47 points; at
follow-up, the maximum score was 97 points and the minimum was 85
points (Fig. 8). Pain. The pain
disappeared in 23 patients. Pain continued to be felt in 12
patients, but was considered tolerable. None of the patients
required oral analgesics.
 | Table IV.Harris hip scores (HHSs) according to
etiology prior to surgery and at the last follow-up. |
Table IV.
Harris hip scores (HHSs) according to
etiology prior to surgery and at the last follow-up.
|
|
| Mean HHS
(points) |
|
|---|
|
|
|
|
|
|---|
| Etiology | No. of patients | Preoperative | Postoperative | P-value |
|---|
| Steroid-induced | 14 | 55.28±6.98 | 84.56±5.86 | <0.0001 |
| Alcohol-induced | 13 | 58.50±8.26 | 90.75±3.09 | <0.0001 |
| Trauma-induced | 4 | 55.75±8.26 | 82.50±6.35 | 0.002 |
| Unknown | 4 | 55.40±9.61 | 91.60±5.81 | 0.001 |
| Total | 35 | 56.53±7.66 | 87.49±5.89 |
0.0001 |
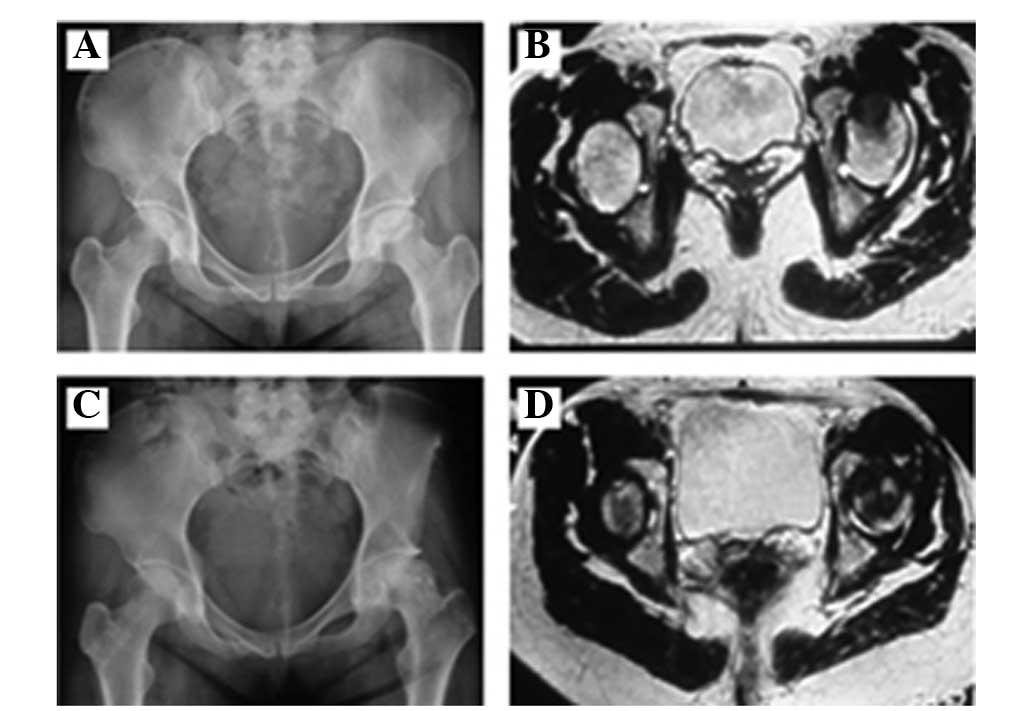
Imaging results
The postoperative imaging data were evaluated by two
orthopedic specialists and according to ARCO staging, there were 16
hips of stage IIA, 7 of stage IIB, 8 of stage IIC, 9 of stage IIIA,
2 of stage IIIB and 1 of stage IIIC. The postoperative incidence
rates were 37.21, 16.28, 18.60, 20.93, 4.65 and 2.33% respectively
(Table I), which the proportion of
stage IIA and IIIA was increased and that of stage IIB, IIC, IIIB
and IIIC was reduced. Postoperative radiography, CT and MRI
revealed no significant differences in the ARCO staging of 32
patients compared with preoperative findings, observing that they
had good osteogenesis (Figs 9 and
10), no appearance of cystic
necrosis, hardening or the ‘crescent sign’. However, another 3
patients at ARCO stage III appeared to have mild collapse (<2
mm) compared with the preoperative collapse. None of the patients
developed osteoarthritis, and none required total hip
arthroplasty.
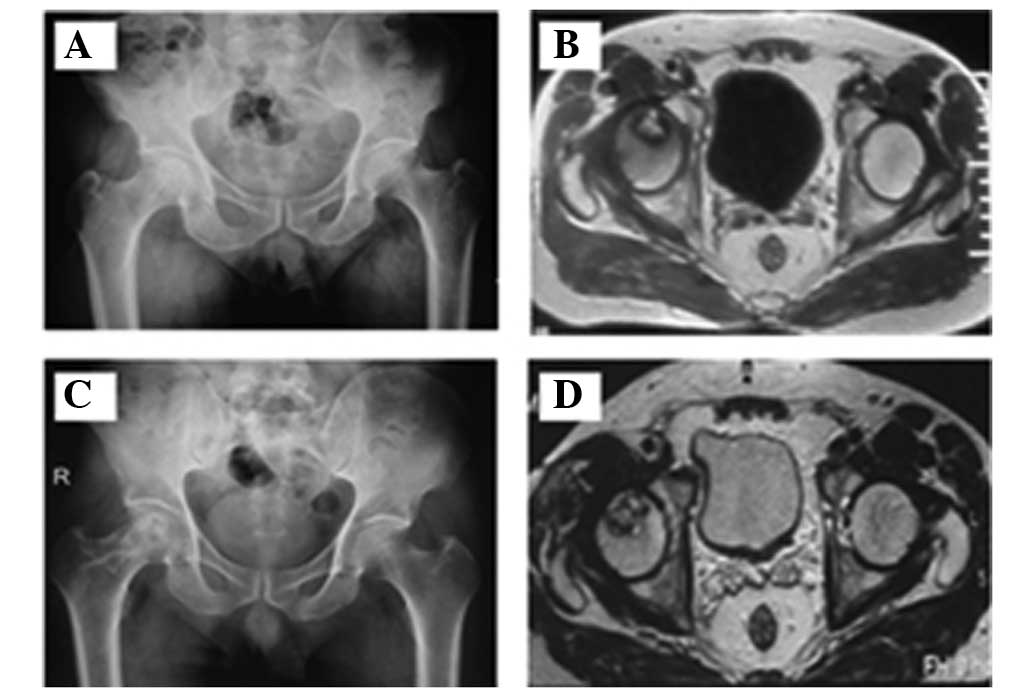
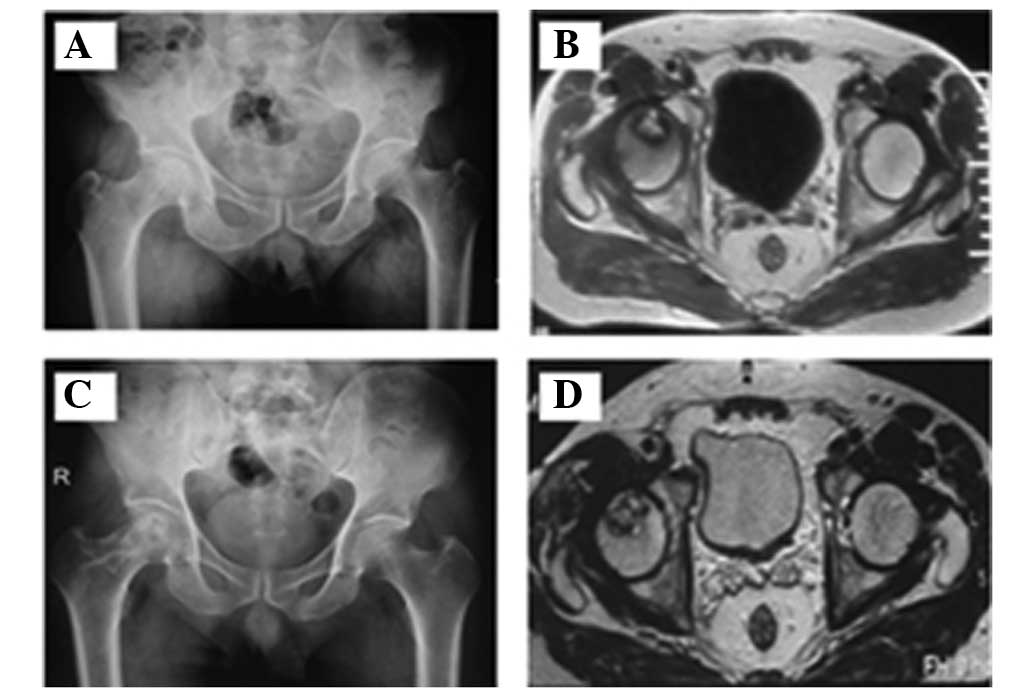 | Figure 9.Preoperative (A) X-ray and (B) MRI and
postoperative (C) X-ray and (D) MRI at the 1-year follow-up. A
49-year-old man with a 30-year history of heavy drinking (average,
50 ml/day) was admitted to hospital on April 29, 2012 with
complaints of right hip pain for more than 3 months and
progressive, aggravated claudication. Physical examination revealed
limited motion of the right hip joint, a positive Patrick's sign,
and feelings of pain under flexion, abduction and extension. The
patient was diagnosed with avascular necrosis of the femoral head
at ARCO stage IIB. On May 8, 2012, the patient underwent
transplantation with iliac bone flaps pedicled with sartorius
muscular fascia around the superficial circumflex iliac vessels.
MRI, magnetic resonance imaging; ARCO, Association for Research on
Osseous Circulation. |
Discussion
In recent years, the incidence of ONFH has been
increasing annually. The reasons for this phenomenon are the wide
application and abuse of hormones as well as changes in lifestyles
(1). Although its etiology,
pathogenesis and treatment have made considerable advances, there
is no effective, universally applicable method of treatment
(2). Currently, surgery is a common
method of curbing the osteonecrotic process and preventing
collapse. Therefore, the key to treating ONFH is to choose the
optimal surgical option (single surgery or a combination of
methods) based on the condition and staging of the patient.
With the rising incidence of ONFH and development of
means to arrive at an early diagnosis, the treatment of ONFH has
been greatly improved. The use of total hip replacement in young
patients, for instance, is being cautiously established.
Maintaining the integrity of the femoral head is a topic of great
interest. Transplantation of vascularized bone flap grafts not only
provides mechanical support and prevents collapse of the femoral
head, but also offers a new source of revascularization and
improves blood circulation of the necrotic femoral head. The
treatments for ONFH involving a muscle pedicle flap that are
currently used in China include: i) a greater trochanter bone graft
of the gluteus medius branch of the lateral femoral circumflex
vessel's ascending branch; ii) an upper-middle periosteal flap of
the femur pedicled with the descending branch of the lateral
femoral circumflex artery; iii) a lateral femoral circumflex artery
transverse branch combined with greater trochanter bone graft of
the gluteus medius branch; iv) a double iliac bone flap with iliac
crest and anteroinferior iliac spine of the lateral femoral
circumflex vessel's ascending branch; v) vascularized fibula graft
with unilateral fibula; vi) vascularized pedicle with an
osteoperiosteal flap of the deep iliac circumflex vessels combined
with a vascular bundle; and vii) iliac bone flaps pedicled with
sartorius muscular fascia and an intermuscular septum vessel
(4–15). Iliac bone flaps pedicled with
sartorius muscular fascia around superficial circumflex iliac
vessels have been rarely reported.
In the application of procedures involving a greater
trochanter bone flap graft of the gluteus medius branch of the
lateral femoral circumflex vessel's ascending branch, Zhao et
al (4,5) found that the outer diameter of the
gluteal muscle branch was 1.0±0.3 mm, the length from the starting
point to the end point of the greater trochanter was 4.0±1.3 mm,
and the bone flap dimension was 1.5×2.5×1.5 cm. This surgery has
many advantages, such as a constant and straight route, easy
harvesting and minimal surgical wounds. It promotes venous return
and new bone regeneration and neovascularization. It increases the
bone supporting force within the femoral head and prevents femoral
head collapse. A total of 17 patients with ONFH at Ficat stages
II–IV were treated with this surgery and were followed up for an
average of 2.6 years. The results indicated that it is a simple and
feasible method causing little trauma that can provide a rich blood
supply for the femoral head and induce osteogenesis. Thus, it is an
effective treatment for avascular necrosis of the femoral head.
When conducting procedures involving an upper-middle
periosteal flap of the femur pedicled with the descending branch of
the lateral femoral circumflex artery, Zhao et al (6) reported that the periosteal branches
originated from 4.0±1.1 cm of the descending artery, the outer
diameter was 1.2±0.5 mm, and the length was 7.1±1.0 cm. There is an
abundant blood supply, a large range of periosteal flap can be
harvested, the vascular pedicle is constant, and the surgical
methods are flexible with less damage to, or no impact on, limb
function. This procedure can antegradely repair femoral neck
fractures and retrogradely repair femoral nonunion and ONFH.
When treatment with a greater trochanter bone graft
of the lateral femoral circumflex artery transverse branch combined
with a gluteus medius branch was carried out, Zhao et al
(7,8)
reported that the outer diameter of the lateral femoral circumflex
artery transverse branch origin was 2.5±0.8 mm. The distance from
the gluteal muscle branch origin to the muscle entering point was
3.5±0.8 cm. This surgery is characterized by a reliable, abundant
blood supply, and is easy to conduct with a flexible surgical
approach. Following its use to treat 32 hips in 32 patients with
ONFH at Ficat stages II–III, the clinical success rate was 90.6%,
with a radiographic success rate of 87.5%. The femoral head
demonstrated revascularization and the procedure had good
efficacy.
According to further studies conducted by Zhao et
al (9,10), where a double iliac bone flap graft
with iliac crest and anteroinferior iliac spine of the lateral
femoral circumflex vessel's ascending branch was used, the length
of the anteroinferior iliac spine of the lateral femoral circumflex
vessel's ascending branch was 5.3±1.0 cm, the outer diameter of the
origin was 1.2±0.3 mm, and the range of the vascularized periosteal
flap harvested in the anteroinferior iliac spine was 2.0×2.0 cm.
This surgery is characterized by a complete arterial and venous
vascularization system, constant anatomical location, easy
dissection, simple surgery and little damage. Combining it with a
periosteal flap in the ascending iliac crest branch, the bone flap
was grafted to the femoral head epiphyseal plate in children, which
is an effective method for treating Perthes disease. When 11
patients with Perthes disease were clinically treated and followed
up for 1.0–3.5 years, the rate of excellent results reached
82%.
According to studies carried out by Liu et al
(11,12), involving a vascularized fibula graft
with unilateral fibula, the outer diameter of the peroneal artery
that supplies the fibula is 1.55 mm. The first arcuate artery gave
rise to one fibular nutrient artery 14.8 cm away from the capitulum
fibula, and its outer diameter was 1.67 mm. A unilateral donor can
provide free fibula of sufficient length and ensure adequate
vascularization, suggesting its safety and feasibility. In
addition, the duration of surgery is shortened, surgical trauma and
blood loss are reduced, body aesthetics are improved, and the
patients are more likely to accept the surgery. When 14 patients
with bilateral ONFH at Steinberg stage II–IV were clinically
treated and followed up for an average of 24 months, the
radiographic results 1 year postoperatively indicated that 23 hips
(82.1%) were improved and 5 hips (17.9%) were kept stable. This
finding indicates that a vascularized fibula graft with unilateral
fibula is an effective treatment for bilateral ONFH due to its
short surgery time, reduced damage and blood loss, and good
postoperative recovery of hip function.
Surgery involving a vascularized pedicle with an
osteoperiosteal flap of deep iliac circumflex vessels combined with
a vascular bundle was carried out by Xian et al (13), The authors treated 42 patients with
ONFH (71 hips) at Ficat stage I–IV using this surgery, and the
rates of excellent and good results were up to 94.1% after a
follow-up of 13.6 years (10–18 years).
Chen et al (14) described the use of iliac bone flaps
pedicled with sartorius muscular fascia and intermuscular septum
vessel. They observed that the grafted intermuscular fascia
comprised the proximal segment of the sartorius, tensor fascia
latae, and rectus femoris. The major blood vessels were derived
from the ascending branch of the lateral femoral circumflex artery
(iliac crest, gluteal muscle and anteroinferior iliac spine
branches) and the sartorius segmental vessels from the superficial
iliac circumflex artery and lateral circumflex femoral artery. The
length of the myofascial pedicle was 6–8 cm, and the size of the
bone block was 3×4 cm. The vascularity and route were constant and
abundant. The possibility of lateral femoral cutaneous nerve damage
was reduced, while the morphology of the anterosuperior iliac spine
was retained. Therefore, this is psychologically acceptable to
patients and is considered an easy alternative bone graft for the
treatment of femoral neck lesions. Liu et al (15) treated 56 patients with ONFH at Ficat
stage I–II using sartorius iliac bone flaps. The patients were
followed up for 8–36 months (mean, 18 months). The HHS was 85.2±6.3
points at 12 months postoperatively. The rate of excellent and good
results was up to 92.8%.
In the present study, 35 patients with ONFH at ARCO
stage II–III were treated with iliac bone flaps pedicled with
sartorius muscular fascia around superficial circumflex iliac
vessels. Based on the imaging findings, according to ARCO staging,
the preoperative incidence rates of each stage were IIA 32.56%, IIB
18.60%, IIC 20.93%, IIIA 18.60%, IIIB 6.98% and IIIC 2.33% and the
postoperative rates were IIA 37.21%, IIB 16.28%, IIC 18.60%, IIIA
20.93%, IIIB 4.65% and IIIC 2.33%. The results revealed that
following treatment, the incidence rates of stages IIA and IIB were
increased and those of IIB, IIC and IIIB, IIIC were reduced
compared with the preoperative rates. No significant staging
progression was observed. The average HHSs for stages II and III
were 58.94±7.13 and 50.33±5.71 points, respectively prior to
treatment 89.55±4.65 and 82.17±5.81 points, respectively,
postoperatively. The results showed that the HHS of stage II was
higher than that of stage III. The improvements in scores were
statistically significant, and treatment in the earlier stages
provided better results. According to etiology, the HHSs for
steroid-induced, alcohol-induced and trauma-induced ONFH, and ONFH
of unknown etiology were 55.28±6.98, 58.50±8.26, 55.75±8.26 and
55.75±8.26 points, respectively, prior to treatment, and
84.56±5.86, 90.75±3.09, 82.50±6.35 and 82.50±6.35 points,
respectively, postoperatively. The differences in HHSs between
prior to surgery and postoperatively were significant (P<0.0001,
P<0.0001, P=0.002 and P=0.001, respectively); the P-values for
steroid- and alcohol-induced ONFH were lower than those for
trauma-induced ONFH and ONFH of unknown etiology. Notably, steroids
and alcohol are single factors, unknown etiology is multifactorial
while trauma involves damage to the blood supply of the femoral
head itself.
In conclusion, in young adults aged 10–65 years with
ONFH at ARCO stage II–III, surgery involving iliac bone flaps
pedicled with sartorius muscle fascia around superficial circumflex
iliac vessels is effective in maintaining the integrity of the
femoral head, as it provides abundant blood circulation, good
osteogenesis and functioning of the hip. The effects of the surgery
on steroid-induced and alcohol-induced ONFH are superior to those
on trauma-induced ONFH and ONFH of unknown etiology, and the
effects of ARCO stages IIA and IIIA are better than ARCO stages
IIB, IIC and IIIB, IIIC.
The results of the present study, based on HHSs,
ARCO stages and imaging, revealed that the clinical success rate
was 91.43%, similar to the results of other methods, and better
than some previously reported (8,10).
However, more clinical research and evidence-based medical
investigations are required to verify its results at long-term
follow-up (>10 years) and application prospects.
Acknowledgements
This study was financially supported by The National
Natural Science Foundation of China (No. 81171692).
References
|
1
|
Amanatullah DF, Strauss EJ and di Cesare
PE: Current management options for osteonecrosis of the femoral
head: part 1, diagnosis and nonoperative management. Am J Orthop
(Belle Mead NJ). 40:E186–E192. 2011.PubMed/NCBI
|
|
2
|
Wang XS, Zhuang QY, Weng XS, et al:
Etiological and clinical analysis of osteonecrosis of the femoral
head in Chinese patients. Chin Med J (Engl). 126:290–295.
2013.PubMed/NCBI
|
|
3
|
Seamon J, Keller T, Saleh J and Cui Q: The
pathogenesis of nontraumatic osteonecrosis. Arthritis.
2012:6017632012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhao DW, Xu DC, Ma Y, et al: Anatomical
study for transposition of the greater trochanter bone flap
pedicled with middle gluteal muscle branch of lateral femoral
circumflex vessel. Zhonghua Xian Wei Wai Ke Za Zhi. 27:129–131.
2004.(In Chinese).
|
|
5
|
Zhao DW, Cui X, Li CX, et al: Greater
trochanter bone flap pedicled with middle gluteal muscle branch of
lateral femoral circumflex vessel for the treatment of ischemic
necrosis of femoral head. Zhongguo Gu Yu Guan Jie Sun Shang Za Zhi.
19:4–6. 2004.(In Chinese).
|
|
6
|
Zhao DW, Bao SZ, Wang TN, et al: Applied
anatomy of periosteal flap of up-middle femoral pedicled with
descending branch of lateral femoral circumflex artery. Zhongguo
Lin Chuang Jie Pou Xue Za Zhi. 18:126–127. 2000.(In Chinese).
|
|
7
|
Zhao DW, Zhang Y and Xu CD: Applied
anatomy of greater trochanter bone-periosteum flap pedicled with
transversal and middle gluteal muscle branches of lateral femoral
circumflex artery. Zhongguo Lin Chuang Jie Pou Za Zhi. 23:234–236,
244. 2005.(In Chinese).
|
|
8
|
Zhao DW, Wang WN, Wang BJ, et al:
Treatment of osteonecrosis of the femoral head by using greater
trochanteric bone flap pedicled with double blood vessels. Zhonghua
Xian Wei Wai Ke Za Zhi. 29:167–169. 2006.(In Chinese).
|
|
9
|
Zhao DW, Wang WM, Chen YW, et al: Applied
anatomy for transposition of two periosteal flaps pedicled with
iliac crest and anterior inferior iliac branches of ascending rarus
of lateral femoral circumflex vessel. Zhongguo Lin Chuang Jie Pou
Za Zhi. 21:211–213. 2003.(In Chinese).
|
|
10
|
Zhao DW, Cui X, Sun Q, et al: Two
periosteal flap pedicled with anterior superior iliac and anterior
inferior iliac branches of lateral femoral circumflex vessel
transposition for the treatment of Perthes disease. Zhonghua Xian
Wei Wai Ke Za Zhi. 26:259–261. 2003.(In Chinese).
|
|
11
|
Liu XL, Sheng JG and Zhang CQ: Applied
anatomic study on vascularized fibula graft with unilateral fibula
as the donor for bilateral femoral head necrosis. Guo Ji Gu Ke Xue
Za Zhi. 32:189–191, 201. 2011.(In Chinese).
|
|
12
|
Liu XL, Sheng JH, Zhang CG, et al:
Treatment of bilateral avascular necrosis of femoral head by free
vascularized fibula grafting with unilateral fibula as donor.
Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 25:641–645. 2011.(In
Chinese). PubMed/NCBI
|
|
13
|
Xian BS, Sun Y and Xian RL: Treatment of
osteonecrosis of the femoral head using vascular pedicle bone
graft. Shi Yong Gu Ke Za Zhi. 15:750–753. 2009.(In Chinese).
|
|
14
|
Chen SL, Wang YK, Zheng ZC, et al: Applied
anatomy for transposition of iliac bone flaps pedicled with
sartorius muscular fascia and intermuscular septum vessel and its
clinical application. Zhonghua Xian Wei Wai Ke Za Zhi. 22:555–557.
2004.(In Chinese).
|
|
15
|
Liu C, Peng H, Yin D, et al: Observation
of curative effect of treating early avascular necrosis of femoral
head by grafting sartorius muscle iliac bone flap. Zhongguo
Linchuang Xin Yixue. 5:207–209. 2012.(In Chinese).
|