Introduction
Central venous catheterization is a commonly
performed procedure used in modern clinical practice (1–3), which
is suggested when peripheral veins are inaccessible. Central venous
catheterization may be lifesaving, but its performance requires
critical operator training and experience. A prior study showed
that >15% of patients who received central venous
catheterization suffered from complications (4). Therefore, methods promotion for
reducing the frequency of complications are required. Right
internal jugular vein (RIJV) catheterization with
ultrasound-assisted guidance has been proposed as a simple and
reliable procedure for multimodality intravenous therapy that meets
the requirements of central venous catheterization (4–6).
Furthermore, real-time ultrasound-assisted guidance has been
suggested to improve the success rate of IJV (7). However, the ultrasonic probe and
advancement of the puncture needle can cause the vein to collapse,
which reduces the success rate of the procedure (8). It has been suggested that the catheter
could be modified to minimize the risk of displacement or migration
(9). Morita et al developed a
novel ‘skin traction method’ which increased the compressive force
required to collapse the IJV, and consequently facilitated
catheterization of the IJV (10). In
addition, a study by Lim et al in 2012 indicated that the
bevel-down approach for needle puncture avoided posterior venous
wall damage during IJV catheterization (11). However, as an alternative to this,
the present study describes a novel puncture point-traction method
(PPTM) that has been developed to facilitate RIJV cannulation, in
which it is attempted to retain the puncture point of the skin
directly above the RIJV in its original position by the traction of
surgical suture. The aim of this study was to assess the effect of
the PPTM on RIJV catheterization in anesthetized patients in the
supine position and to consequently verify the application this
novel PPTM.
Materials and methods
Ethical approval
The study was approved by the Ethics Committee of
Fuyang People's Hospital (Fuyang, China), and informed consent was
confirmed by all patients. There were 120 patients who were about
to have surgery with RIJV catheterization and suture fixation. The
patients were divided into physical status grades I–III according
to the American Society of Anesthesiologists (ASA) classification
system (12). Their average age was
65.2±11.4 years (range, 19–73 years), with an average body weight
of 61.9±7.1 kg (range, 48–82 kg) and average height of 168.4±8.2 cm
(range, 160–183 cm) (Table I). All
patients were randomly divided into a PPTM group (n=60, treated
with the PPTM method) and a non-PPTM group (n=60, treated without
the PPTM method). Patients were not included in this study
according to the following exclusion criteria: External neck
injury, previous history of RIJV catheterization, severe
cardiovascular disease, injection-site infection, hematological
disease, thrombogenesis history, obesity and short-term venous
catheterization.
 | Table I.General characteristics of all
patients. |
Table I.
General characteristics of all
patients.
| Variable | Non-PPTM group
(n=59) | PPTM group
(n=60) |
|---|
| Age, years |
65.6±12.4 |
64.8±10.8 |
| Height, cm | 168.5±8.3 | 168.2±7.8 |
| Weight, kg |
61.6±7.2 |
62.4±7.4 |
| Gender,
male/female | 37/22 | 34/26 |
| ASA class
I/II/III | 24/31/4 | 27/26/7 |
Surgical procedure
Heart rate (HR), oxygen saturation and mean arterial
pressure (MAP) were measured continuously. In cases where the MAP
decreased to <60 mmHg and the HR decreased to <60 beats per
minute during venipuncture, which was identified as hypotension and
bradycardia, all patients were placed in the supine position
without using pillows, with the head turned 30° to the left
following the induction of anesthesia. Remedication with 0.1mg/kg
intravenous midazolam was given 10min before induction. Induction
was performed using 2 µg/kg fentanyl followed by 2.5mg/kg propofol.
Tracheal intubation was facilitated using rocuronium with a dose of
1.2mg/kg. An ultrasound probe (L25x, 13–6 MHz; SonoSite, Inc.
Bothell, WA, USA) was used during catheterization, which was
applied perpendicular to the skin without any pressure. The
cross-sectional area (CSA), anteroposterior diameter (AD) and
transverse diameter (TD) of the RIJV at the cricoid cartilage level
were measured with three replicates using electronic calipers on
the ultrasound image in all patients following the induction of
anesthesia and during catheterization (when aspiration of blood
into the syringe occurred during advancement of the needle).
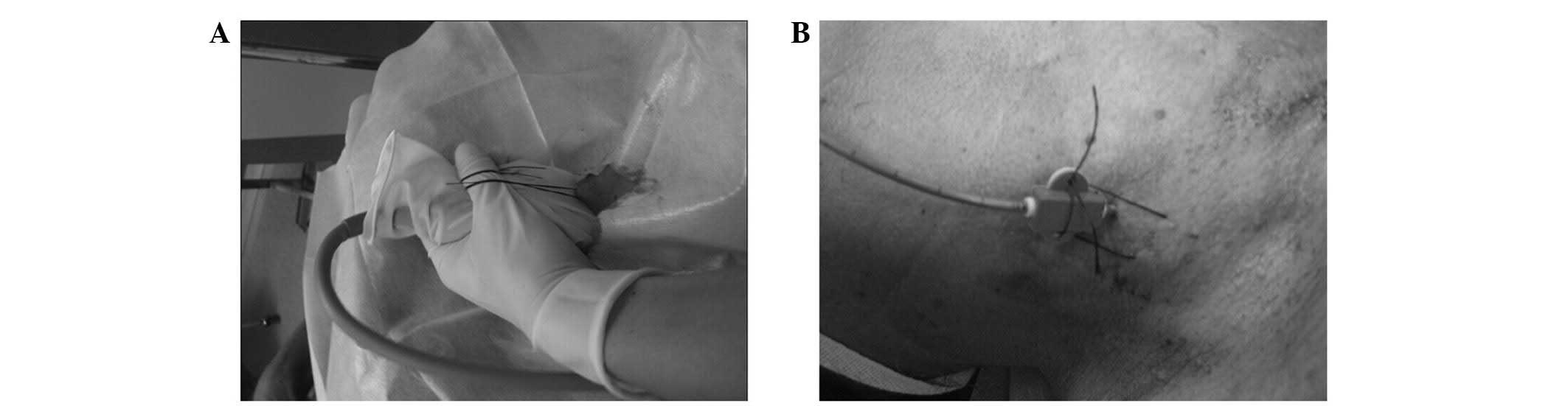
In the PPTM group, the skin directly above the RIJV
at the level of the cricoid cartilage was identified by ultrasound
following disinfection of the right neck skin. A surgical suture
(Péters Surgical, Bobigny, France) was sutured at this position,
without tying a knot, using a skin-suturing needle. The suture was
intradermal for 1 cm with 20-cm lengths of suture outside the skin
at each side. Cannulation was put into place under real-time
ultrasound visualization in the transverse plane. During
catheterization, the two ends of the suture were wound around the
left hand thumb of operator and were held closely to the middle of
the ultrasonic probe, which was directed at the side of the
patient's head (Fig. 1A). A puncture
needle (16 G, 20 cm; Lepu Medical Technology Co., Ltd., Beijing,
China) was advanced slowly and carefully under continuous negative
pressure at the position of the suture in the skin. The angle of
the needle was 35–45° to the skin. During advancement of the
needle, the position of the ultrasonic probe remained unchanged,
and the suture was straightened with the advancement of the needle.
When the ultrasound probe did not touch the patient's skin, they
were brought into contact by pulling the suture using the left
thumb. When blood entered the needle, the position of the needle
was maintained using the left hand and a guidewire was inserted.
Consequently, RIJV catheterization was carried out, and a suture
was applied to fix the catheter (Fig.
1B). In the non-PPTM group, only when the RIJV catheterization
at the level of the cricoid cartilage was completed was the
position of the suture selected and the suture applied to fix the
catheter. The remaining procedures of the surgery in the non-PPTM
group were the same as those in the PPTM group. In cases where the
right internal carotid artery (ICA) was punctured in either group,
RIJV catheterization was abandoned.
Measurements
Age, gender, height, weight and ASA grades of the
patients were recorded. The following variables were also recorded:
CSA, AD and TD of the RIJV at the cricoid cartilage level following
anesthesia induction and during catheterization (when aspiration of
blood into syringe occurred during advancement of needle) in the
two groups. Measurements were performed three times for each
condition. The number with obvious loss of resistance (NOLR), the
number with easy aspiration of blood into syringe (NEABS) during
advancement of the needle, the depth of needle insertion (DNI), the
number of first-pass punctures (NFPP) and total success rate (TSR)
were examined. In addition, the HR, minimum value of MAP,
hypotension, bradycardia and puncture-related complications such as
pneumothorax, hemopneumothorax, local hematoma and ICA puncture
during catheterization were recorded.
Statistical analysis
SPSS statistical analysis software, version 13.0
(SPSS, Inc., Chicago, IL, USA) was applied for statistical analysis
and data values are presented as mean ± standard deviation.
Statistically significant differences between groups were assessed
using one-way analysis of variance followed by the Bonferroni
multiple comparison test to evaluate intergroup differences.
P<0.05 indicated a statistically significant difference.
Results
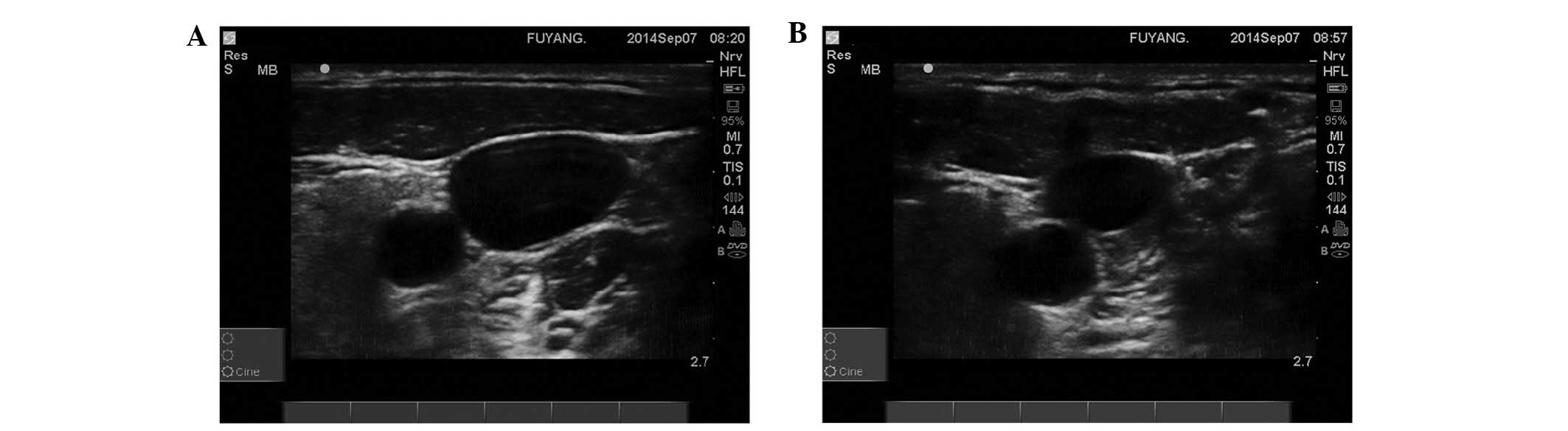
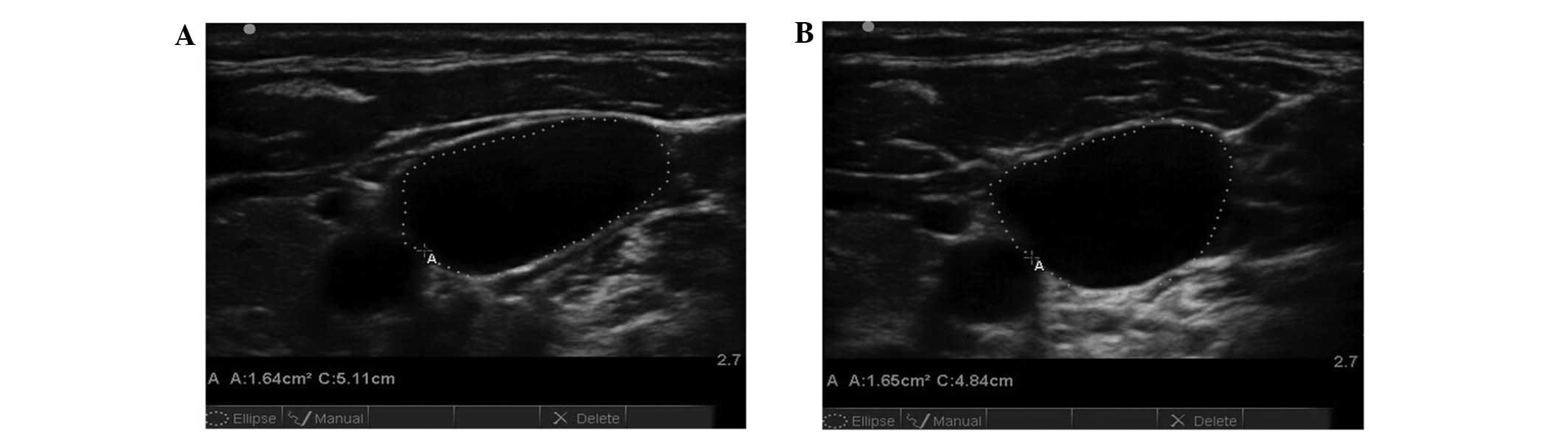
Changes in CSA, AD and TD
The CSA (P<0.01), AD (P<0.01), TD (P<0.05)
of the RIJV at the cricoid cartilage level in the non-PPTM group
were significantly smaller during catheterization compared with
those following the induction of anesthesia (Fig. 2 and Table
II); however, no significant differences (P>0.05) in these
measurements between these two time points were observed in the
PPTM group (Fig. 3 and Table II). The CSA (P<0.01), AD
(P<0.01), TD (P<0.05) of the RIJV at the cricoid cartilage
level during catheterization were larger in the PPTM group compared
with those in the non-PPTM group (Table
II).
 | Table II.Changes in CSA, AD, and TD of the RIJV
at the cricoid cartilage level following the induction of
anesthesia and during catheterization, and other
venipuncture-related data for the two groups. |
Table II.
Changes in CSA, AD, and TD of the RIJV
at the cricoid cartilage level following the induction of
anesthesia and during catheterization, and other
venipuncture-related data for the two groups.
| Outcome | Non-PPTM group | PPTM group |
|---|
| CSA,
cm2 |
|
|
| After
anesthesia induction | 1.63±0.38 | 1.61±0.31 |
| During
catheterization |
0.93±0.21a |
1.72±0.33b |
| AD, cm |
|
|
| After
anesthesia induction | 1.55±0.73 | 1.54±0.67 |
| During
catheterization |
1.02±0.16a |
1.48±0.50b |
| TD, cm |
|
|
| After
anesthesia induction | 3.39±1.33 | 3.40±1.31 |
| During
catheterization |
2.18±0.28c |
3.38±0.29d |
| NOLR, n (%) | 4 (6.78) | 55
(91.7)b |
| NEABS during
advancement of the needle, n (%) | 28 (47.5) | 53
(88.3)b |
| NFPP, n (%) | 40 (67.8) | 56
(93.3)b |
Changes in NOLR, NEABS and NFPP
During needle insertion and catheterization, the
NOLR (P<0.01), NEABS (P<0.01) and NFPP (P<0.01) in the
PPTM group were significantly increased compared with those in the
non-PPTM group (Table II). However,
the DNI, catheterization time and TSR were not significantly
different during catheterization between the two groups (P>0.05;
data not shown).
Complications
There was one case of exclusion from the study
because of ICA puncture in the non-PPTM group. Apart from this,
there were no other complications in either of the two groups.
Discussion
Safe and efficient placement of central venous
catheters is an essential skill in many fields of clinical
medicine, which is mainly conducted by direct visualization
methods. Some studies (13–17) have indicated that ultrasound-assisted
guidance of internal jugular vein catheterization increases the
success rate, and reduces the catheterization time and puncture
complications. However, several studies (18–20) have
found that perforation of the posterior vessel wall continues to
occur, even when venipuncture is guided by ultrasound. Studies
(21,22) have found that ultrasound-assisted
guidance cannot completely avoid ICA puncture because application
of the ultrasound probe and advancement of the needle cause RIJV
collapse. Gordon et al (21)
have observed that the CSA and the diameter of the vein influence
the success rate of central vein catheterization. In anesthetized
patients, positive end-expiratory pressure or the Trendelenberg
position increase the CSA of the IJV (23,24). It
was found in the present study that the RIJV could be maintained in
a state of natural fullness by the PPTM, and it prevented the RIJV
from collapsing due to stretching of the skin directly above the
RIJV, with a success rate of 100%.
It was observed in the present study that the CSA,
AD and TD of the RIJV at the cricoid cartilage level were smaller
during catheterization than those after anesthesia induction in the
non-PPTM group, which may be attributed to the pressure from the
ultrasonic probe and the advancement of needle. However, there was
no significant change in the CSA, AD and TD of the RIJV at the
cricoid cartilage level between after the induction of anesthesia
and during catheterization in the PPTM group. A sudden loss of
resistance occurred in 91.7% of the patients during venipuncture in
the PPTM group, and it was found that only the anterior vascular
wall was perforated in these patients. Additionally, blood was
easily aspirated in 88.3% of the patients in the PPTM group, which
implied that only the anterior vascular wall was perforated, and it
was found that the advanced needle did not touch the posterior
vascular wall. These findings confirmed that PPTM helped to
maintain the natural state of fullness of the RIJV during
catheterization by providing a counterforce against the pressure
created by the advancement of the needle and the ultrasonic probe,
and the PPTM helped the smooth backflow of blood without repeated
venipuncture.
During venipuncture, we recommend that the suture is
pulled closely to the middle of the ultrasonic probe, which is
pointed at the side of the patient's head. The height of the
ultrasonic probe was kept unchanged, the needle tip was inserted in
a downward direction and it was found that the PPTM reduced the
pressure on the RIJV caused by the ultrasonic probe and the
advancement of needle, and maintained the skin directly above the
RIJV in its original position. If the height of the ultrasonic
probe was reduced with advancement of the needle, the CSA, AD and
TD of the RIJV at the cricoid cartilage level would be influenced
by the pressure of the ultrasonic probe. Therefore, the height of
the ultrasonic probe was kept unchanged. Denys et al
(6) concluded that the success rate
of FPP was 78% using a 16-G puncture needle. In the present study,
a rather higher success rate of FPP (93.3%) was attained by the
PPTM.
Verghese et al (25) suggested that the IJV might be
collapsed by advancement of the needle, which would increase the
possibility of accidental ICA puncture. In the present study, it
was found that the CSA, AD and TD of the RIJV at the cricoid
cartilage level were relatively smaller in the non-PPTM group than
those in the PPTM group during venipuncture, so the possibility of
accidental right ICA puncture was higher in the non-PPTM group than
in the PPTM group. One case was excluded from the present study
because of ICA puncture in the non-PPTM group, although there was
no significant difference between the two groups with regard to
success rate.
In our preliminary experiments, it was found that
suture slippage was more likely when pulling the suture if the ends
of the suture were wound around the right thumb pulp for less than
two turns (data not shown). Therefore, it was decided that at least
two turns of suture winding were necessary. A decision was also
made to pull the suture 1–2 mm above the neck skin, as it was found
that the ultrasonic probe would not touch the skin when the
puncture needle was inserted without pulling the suture. If
excessive force was applied on the suture, the CSA of the RIJV at
the cricoid cartilage level would be shown only partly in the
ultrasound imaging, and the AD at the cricoid cartilage level would
also be increased. Ultrasound imaging of the whole RIJV could not
be obtained completely when the length of suture beneath the skin
was too short or was not in parallel with the cricoid cartilage;
therefore, it was decided to keep the suture >1 cm beneath the
skin in parallel with the cricoid cartilage during
venipuncture.
In conclusion, the findings from this study
confirmed that the PPTM method facilitated the catheterization of
RIJV and improved the success rate of RIJV catheterization in
anesthetized patients in the supine position.
Acknowledgements
The authors would like to thank Fuyang People's
Hospital for financial support.
References
|
1
|
de Jonge RC, Polderman KH and Gemke RJ:
Central venous catheter use in the pediatric patient: Mechanical
and infectious complications. Pediatr Crit Care Med. 6:329–339.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sanford TJ Jr: Internal jugular vein
cannulation versus subclavian vein cannulation. An
anesthesiologist's view: The right internal jugular vein. J Clin
Monit. 1:58–61. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Defalque RJ: Percutaneous catheterization
of the internal jugular vein. Anesth Analg. 53:116–121. 1974.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
McGee DC and Gould MK: Preventing
complications of central venous catheterization. N Engl J Med.
348:1123–1133. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chuan WX, Wei W and Yu L: A
randomized-controlled study of ultrasound prelocation vs anatomical
landmark-guided cannulation of the internal jugular vein in infants
and children. Pediatr Anesth. 15:733–738. 2005. View Article : Google Scholar
|
|
6
|
Denys BG, Uretsky BF and Reddy PS:
Ultrasound-assisted cannulation of the internal jugular vein. A
prospective comparison to the external landmark-guided technique.
Circulation. 87:1557–1562. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Takeji S, Hiroshi S, Azumi K, Mamoru N,
Masashi M, Takamitsu T, Katsunori S, Masao S, Tsuyoshi U, Hideki K
and Hideharu H: Ultrasound analysis of the relationship between
right internal jugular vein and common carotid artery in the left
head-rotation and head-flexion position. Heart Vessels. 28:620–625.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sasano H, Morita M, Azami T, Ito S, Sasano
N, Kato R, Hirate H, Ito H, Takeuchi A and Sobue K: Skin-traction
method prevents the collapse of the internal jugular vein caused by
an ultrasound probe in real-time ultrasound-assisted guidance. J
Anesth. 23:41–45. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Redo SF: Modified catheter for prolonged
central venous use. J Pediatr Surg. 30:1544–1545. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Morita M, Sasano H, Azami T, Sasano N,
Fujita Y, Ito S and Sobue K: A novel skin-traction method is
effective for real-time ultrasound-guided internal jugular vein
catheterization in infants and neonates weighing less than 5
kilograms. Anesth Analg. 109:754–759. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lim T, Ryu HG, Jung CW, Jeon Y and Bahk
JH: Effect of the bevel direction of puncture needle on success
rate and complications during internal jugular vein
catheterization. Crit Care Med. 40:491–494. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wolters U, Wolf T, Stützer H and Schröder
T: ASA classification and perioperative variables as predictors of
postoperative outcome. Br J Anaesth. 77:217–222. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Legler D and Nugent M: Doppler
localization of the internal jugular vein facilitates central
venous cannulation. Anesthesiology. 60:481–482. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Randolph AG, Cook DJ, Gonzales CA and
Pribble CG: Ultrasound guidance for placement of central venous
catheters: A meta-analysis of the literature. Crit Care Med.
24:2053–2058. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hind D, Calvert N, McWilliams R, Davidson
A, Paisley S, Beverley C and Thomas S: Ultrasonic locating devices
for central venous cannulation: meta-analysis. British Medical
Journal. 327:361–364. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Mallory DL, McGee WT, Shawker TH, Brenner
M, Bailey KR, Evans RG, Parker MM, Farmer JC and Parillo JE:
Ultrasound guidance improves the success rate of internal jugular
vein cannulation. A prospective, randomized trial. Chest.
98:157–160. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Karakitsos D, Labropoulos N, De Groot E,
Patrianakos AP, Kouraklis G, Poularas J, Samonis G, Tsoutsos DA,
Konstadoulakis MM and Karabinis A: Real-time ultrasound-guided
catheterisation of the internal jugular vein: A prospective
comparison with the landmark technique in critical care patients.
Crit Care. 10:R1622006. View
Article : Google Scholar : PubMed/NCBI
|
|
18
|
Blaivas M and Adhikari S: An unseen
danger: Frequency of posterior vessel wall penetration by needles
during attempts to place internal jugular vein central catheters
using ultrasound guidance. Crit Care Med. 37:2345–2349. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ganesh A and Jobes DR: Ultrasound-guided
catheterization of the internal jugular vein. Anesthesiology.
108:1155–1156. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mallory DL, Shawker T, Evans RG, McGee WT,
Brenner M, Parker M, Morrison G, Mohler P, Veremakis C and Parrillo
JE: Effects of clinical maneuvers on sonographically determined
internal jugular vein size during venous cannulation. Crit Care
Med. 18:1269–1273. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gordon AC, Saliken JC, Johns D, Owen R and
Gray RR: US-guided puncture of the internal jugular vein:
Complications and anatomic considerations. J Vasc Interv Radiol.
9:333–338. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Leung J, Duffy M and Finckh A: Real-time
ultrasonographically-guided internal jugular vein catheterization
in the emergency department increases success rates and reduces
complications: A randomized, prospective study. Ann Emerg Med.
48:540–547. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lobato EB, Florete OG Jr, Paige GB and
Morey TE: Cross-sectional area and intravascular pressure of the
right internal jugular vein during anesthesia: Effects of
Trendelenburg position, positive intrathoracic pressure and hepatic
compression. J Clin Anesth. 10:1–5. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Troianos CA, Jobes DR and Ellison N:
Ultrasound-guided cannulation of the internal jugular vein. A
prospective, randomized study. Anesth Analg. 72:823–826. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Verghese ST, McGill WA, Patel RI, Sell JE,
Midgley FM and Ruttimann UE: Ultrasound-guided internal jugular
venous cannulation in infants: A prospective comparison with the
traditional palpation method. Anesthesiology. 91:71–77. 1999.
View Article : Google Scholar : PubMed/NCBI
|