Introduction
Non-ST-elevation acute coronary syndromes (NSTE-ACS)
are associated with a higher incidence and mortality rate, as
compared with STE-ACS. NSTE-ACS have varying clinical
manifestations and prognoses, such that the selection of an
appropriate treatment strategy is typically dependent on risk
stratification (1). The NSTE-ACS
guidelines published by the American College of Cardiology
(ACC)/American Heart Association (AHA) and the European Society of
Cardiology (ESC) in 2007, recommended that the risk assessment
system be used for conducting patient risk stratification (2). At present, the risk scoring system,
which was established on the basis of foreign clinical trials and
incorporates Thrombolysis in Myocardial Infarction, PURSUIT and
Global Registry of Acute Coronary Events (GRACE) scoring systems,
is used to conduct risk assessments of NSTE-ACS patients. The
current guidelines from the ACC/AHA and ESC are unclear as to which
of the three risk scoring systems they recommend; thus suggesting
that existing risk stratification methods may discriminate
differently between the clinical risks associated with NSTE-ACS
(1,3). Among the existing multiple risk scoring
systems, GRACE scoring has particular advantages regarding the
prediction of cardiovascular events (4), and is currently the most widely used
risk scoring system (5–10). However, as compared with the other
risk scoring systems, GRACE scoring does not include indices that
may reflect neurohumoral factors and hemodynamic alterations; thus
its accuracy in predicting cardiovascular events may be
limited.
Previous studies have explored the value of
combining novel markers and existing risk scoring systems for
predicting the clinical risks of NSTE-ACS (11,12). The
N-terminal of the prohormone brain natriuretic peptide (NT-proBNP)
is a biomarker produced by myocardial cells, and is released into
the blood when cardiac cells are stretched or when the wall tension
is increased (13). Previous studies
have demonstrated the significance of NT-proBNP in heart failure
(14,15), and have suggested that NT-proBNP may
be used for the risk stratification of ACS (16,17).
Guidez et al (11)
demonstrated that a hybrid risk scoring system, established from a
combination of the plasma BNP concentration and the GRACE scoring
system, was able to improve the accuracy of prognostic predictions
of patients with ACS. This hybrid scoring system was aimed at all
patients with ACS; however, to the best of our knowledge, a hybrid
risk scoring system has yet to be established for the prediction of
cardiac events in patients with NSTE-ACS. The present study aimed
to establish a clinical risk prediction model based on a
combination of the GRACE scoring system and the logarithm of the
plasma NT-proBNP (lgNT-proBNP) concentration, in order to improve
the prediction of major cardiac adverse events (MACE), including
cardiac death, acute myocardial infarction and heart failure, in
patients with NSTE-ACS, and to direct the development of novel
treatment strategies.
Materials and methods
Subjects
A total of 640 patients with NSTE-ACS at the Anzhen
Hospital (Beijing, China) were enrolled in the present study
between January 2009 and August 2011. Patients were randomly
allocated into either the model-establishing group (409 patients,
of which 282 were cases of unstable angina and 127 were cases of
NSTE-myocardial infarction), or the prediction model group (231
patients, of which 161 were cases of unstable angina, and 70 were
cases of NSTE-myocardial infarction). Patients were excluded if
they had: i) Acute ST-elevation myocardial infarction; ii) acute
and chronic heart failure, with left ventricular ejection fraction
<45%; iii) valvular heart disease; iv) a pacemaker; v) severe
liver, kidney or lung diseases; and vi) an infection, cancer or
various other conditions. The general characteristics of all
patients, including age, gender, height, weight, medical history
and situation of current hospitalization, were recorded. The
present study was conducted in accordance with the declaration of
Helsinki, and with approval from the Ethics Committee of China
Capital Medical University (Beijing, China). Written informed
consent was obtained from all participants.
Auxiliary examinations
Venous blood was immediately sampled following
admission in order to detect markers of myocardial injury,
including cardiac troponin 1, creatine kinase and creatine
kinase-MB. The fasting blood was sampled in the morning of day 2
following admission, in order to detect various biochemical markers
and serum lipids, including NT-proBNP, total cholesterol and
low-density lipoprotein cholesterol, and hepatonephric functions
via alanine transaminase, aspartate aminotransferase, urea and
creatinine levels. Echocardiography was performed throughout
hospitalization using a Vivid 7 ultrasound system (GE Healthcare
Bio-Sciences, Pittsburgh, PA, USA).
Determination of plasma NT-proBNP
concentration
The plasma concentration of NT-proBNP in the venous
blood samples collected immediately following admission were
measured using a Dimension RxL Max automatic biochecmical analyzer
(Siemens AG, Munich, Germany), with a measurable range of 0–30,000
ng/l.
GRACE risk assessment
The GRACE risk assessment was conducted immediately
following admission, and included assessment of the following
factors: Age, heart rate, systolic blood pressure, serum creatinine
levels, cardiac function [as determined by Killip classification
(18)], whether the patient was
experiencing cardiac arrest upon admission, ST-segment depression
and cardiac enzyme elevation (19).
GRACE scores of ≤88, between 89–118, and >118 were indicative of
a low-, medium- and high-risk of experiencing a MACE,
respectively.
Coronary angiography
Coronary angiography was perfected throughout the
hospitalization. All patients with unstable angina/acute
NSTE-myocardial infarction were treated with the standard secondary
drug prevention therapy for coronary heart disease throughout
hospitalization, as determined by an experienced physician. These
standard therapies included oxygen, 1 ml morphine (10 mg/ml;
Northeast Pharmaceutical Group Co., Ltd., Shenyang, China) for pain
relief, anti-platelet therapy and anticoagulation with 2 ml heparin
(12,500 U/ml; Sanofi S.A., Paris, France). A total of 2 ml dopamine
(20 mg/ml; Shanghai Harvest Pharmaceutical Co., Ltd., Shanghai,
China) and 2 ml dobutamine (20 mg/ml; Zhejiang Ruixin
Pharmaceutical Co., Ltd., Zhejiang, China) were also administered
if systemic vascular resistance was high. Diuretics and fluids were
given according to the estimated optimal filling pressures and
mechanical ventilation (V60; Maquet Servoi, Berlin, Germany) was
applied if necessary.
Follow-up
Follow-up methods included outpatient visits and
telephone communication. The average follow-up period was 774±217
days.
Statistical analysis
SPSS software, version 16.0 (SPSS, Inc., Chicago,
IL, USA) was used to construct the database and perform statistical
analyses. Continuous variables were analyzed using the normality
test. Data that met the normal distribution initially or following
data conversion are presented as the mean ± standard deviation.
Conversely, the non-normally distributed data are presented as the
median and interquartile range. Bivariate data were analyzed using
linear correlation analysis. P<0.05 was considered to indicate a
statistically significant difference. The categorical variables
were evaluated using the χ2 test, and the area under the receiver
operating characteristic (ROC) curve was used to assess the
predictive ability.
Statistical methods used to assess the
model-establishing group were as follows: i) lgNT-proBNP was made
equal to the magnitude order of GRACE through the standard scores
and, according to the correlation coefficient of lgNT-proBNP and
GRACE scoring (0.507), the hybrid risk model was calculated; ii)
the hybrid risk model was simplified for clinical application; iii)
according to the cutoff point of NT-proBNP, as demonstrated by the
ROC curve, NT-proBNP was divided into high- and low-risk groups,
which were, along with the original three GRACE scoring groups,
regrouped. Based on these regroupings, the hybrid risk model was
re-stratified into three groups.
Results
Determination of NT-proBNP
concentration
The NT-proBNP concentration was converted into the
logarithmic value of NT-proBNP (lgNT-proBNP), which exhibited a
normal distribution. Similarly, the GRACE scores met the normal
distribution. Baseline data are presented in Table I.
 | Table I.Baseline data. |
Table I.
Baseline data.
| Parameter | Model-establishing
group | Prediction model
group |
|---|
| Patients (n) | 409 | 231 |
| Average age
(years) | 60±9 |
61±10 |
| Heart rate
(beats/min) |
71±12 |
70±11 |
| Systolic blood
pressure (mmHg) | 132±18 | 132±20 |
| Males | 284 (69.4%) | 156 (67.5%) |
| History of
smoking | 227 (55.5%) | 127 (55.0%) |
| Hypertension | 265 (64.8%) | 165 (71.4%) |
| Diabetes | 132 (32.3%) | 83
(35.9%) |
| Hyperlipidemia | 116 (28.4%) | 162 (70.1%) |
| Serum creatinine
(µmol/l) |
83±26 |
83±20 |
| NT-proBNP (ng/l) | 305.5 (1.9,
15,070.3) | 879.8 (6.5,
53,900) |
| lgNT-proBNP
(ng/l) |
1.9±0.6 |
2.3±0.6 |
| Cardiac troponin I
(ng/l) | 3.0 (0,
92.6) | 3.16 (0,
88.29) |
| Creatine kinase
(U/l) | 169.5
(16, 4,874) | 210.58
(20, 5,888) |
| Creatine kinase
isoenzyme (U/l) | 22.5
(0.2, 569) | 28.53 (5, 314) |
| Total cholesterol
(mmol/l) | 4.6±1.1 | 4.4±1.1 |
| Triglyceride
(mmol/l) | 2.8±0.8 | 2.7±0.8 |
| HDL cholesterol
(mmol/l) | 1.1±0.8 | 1.1±0.4 |
| LDL cholesterol
(mmol/l) | 2.8±0.8 | 2.7±0.8 |
| Hypersensitive
C-reactive protein (mg/l) | 4.3 (0.08,
33.13) | 5.7 (0.08,
43.66) |
| GRACE score
(points) | 104±26 | 112±34 |
| Follow-up time
(days) |
774±217 |
706±231 |
Model-establishing group
Among the 409 patients in the model-establishing
group, 105, 209 and 95 patients were in the low-, moderate- and
high-risk groups, respectively, according to the GRACE scoring
system. A total of 26 patients experienced MACE (6.4%), including
13 cases of cardiogenic mortality, eight cases of acute myocardial
infarction and five cases of heart failure-induced
rehospitalization.
Prediction model group
The prediction model group consisted of 231
patients, of which 62, 74 and 95 patients were in the low-,
moderate- and high-risk groups, respectively, according to the
GRACE scoring system. A total of 15 patients experienced MACE
(6.5%), including three cases of cardiogenic mortality, six cases
of acute myocardial infarction and six cases of heart
failure-induced rehospitalization.
Association between the NT-proBNP
levels and GRACE scores of patients with NSTE-ACS
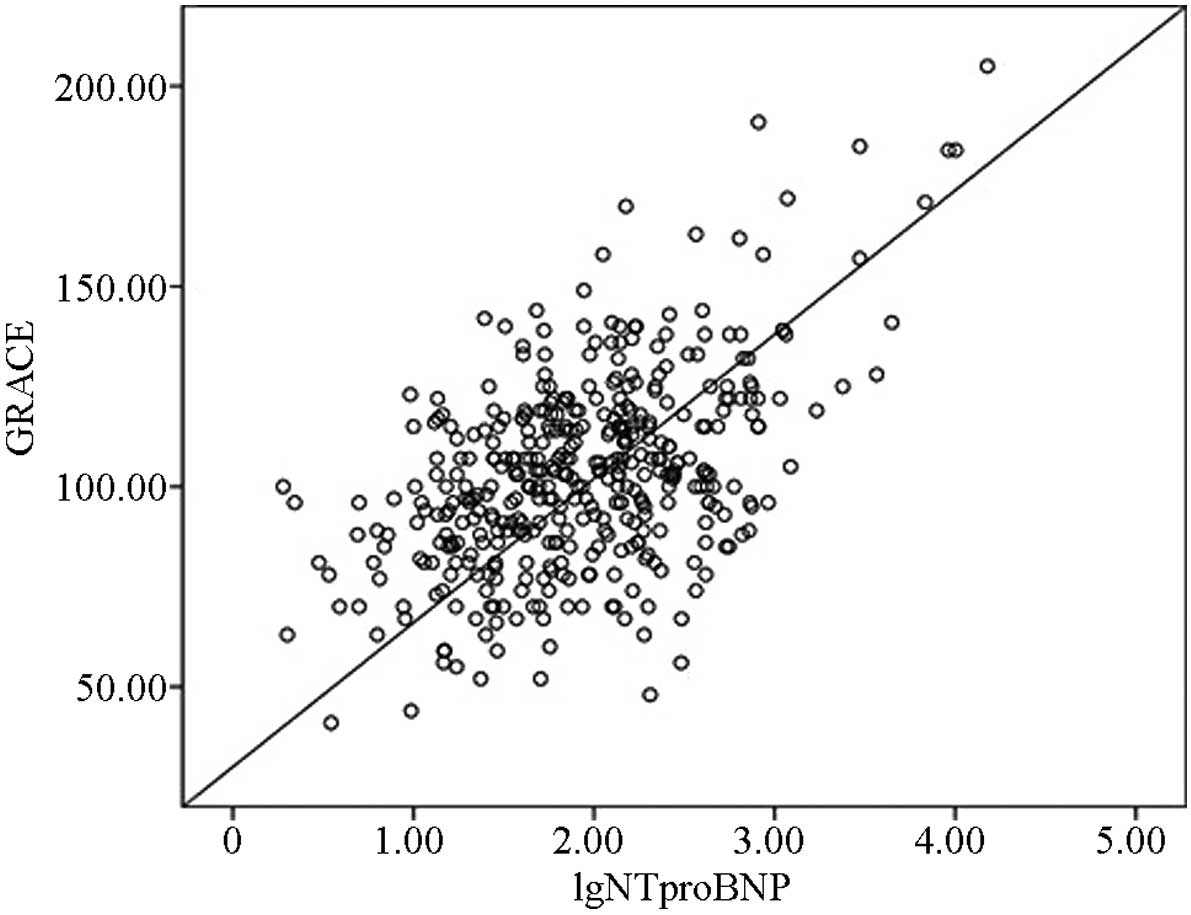
The correlation between the lgNT-proBNP
concentration and GRACE scores was determined using bivariate
correlation analysis; the correlation coefficient (r) was 0.507,
which suggests that these two variables are positively correlated
(P<0.001; Fig. 1).
Hybrid risk model consists of a
combination of the NT-proBNP concentration values and the GRACE
scores
The hybrid risk model was established using the
following formula: Hybrid risk model = GRACE score + 0.507 ×
[lgNT-proBNP - 1.93)/0.63 × 24.11 + 103.54]. In order to facilitate
clinical applications, the hybrid risk model was simplified as
follows: Hybrid risk model = GRACE score + 20 × lgNT-proBNP + 15.
The following analyses were conducted using the simplified risk
model. The hybrid risk model was regrouped for the evaluation of
NT-pro BNP, which generated new risk stratifications as follows:
Low risk, <135 points; moderate-risk, 135–170 points; and
high-risk, >170 points. Each risk layer of the hybrid risk model
underwent the χ2 test (χ2=58.494; V=2; P=0.000), which suggested
that there were significant differences in the incidence of MACE
among these three groups. Following re-stratification, seven cases
in the high-risk group were downgraded to the moderate-risk group,
eight cases from the high-risk group were downgraded to the
low-risk group, and ten cases in the low-risk group were upgraded
to the high-risk group; therefore 6% of all patients were
re-grouped. In addition, among the 15 patients that experienced
MACE, two were upgraded from the moderate-risk group to the
high-risk group; thus accounting for 8% of patients.
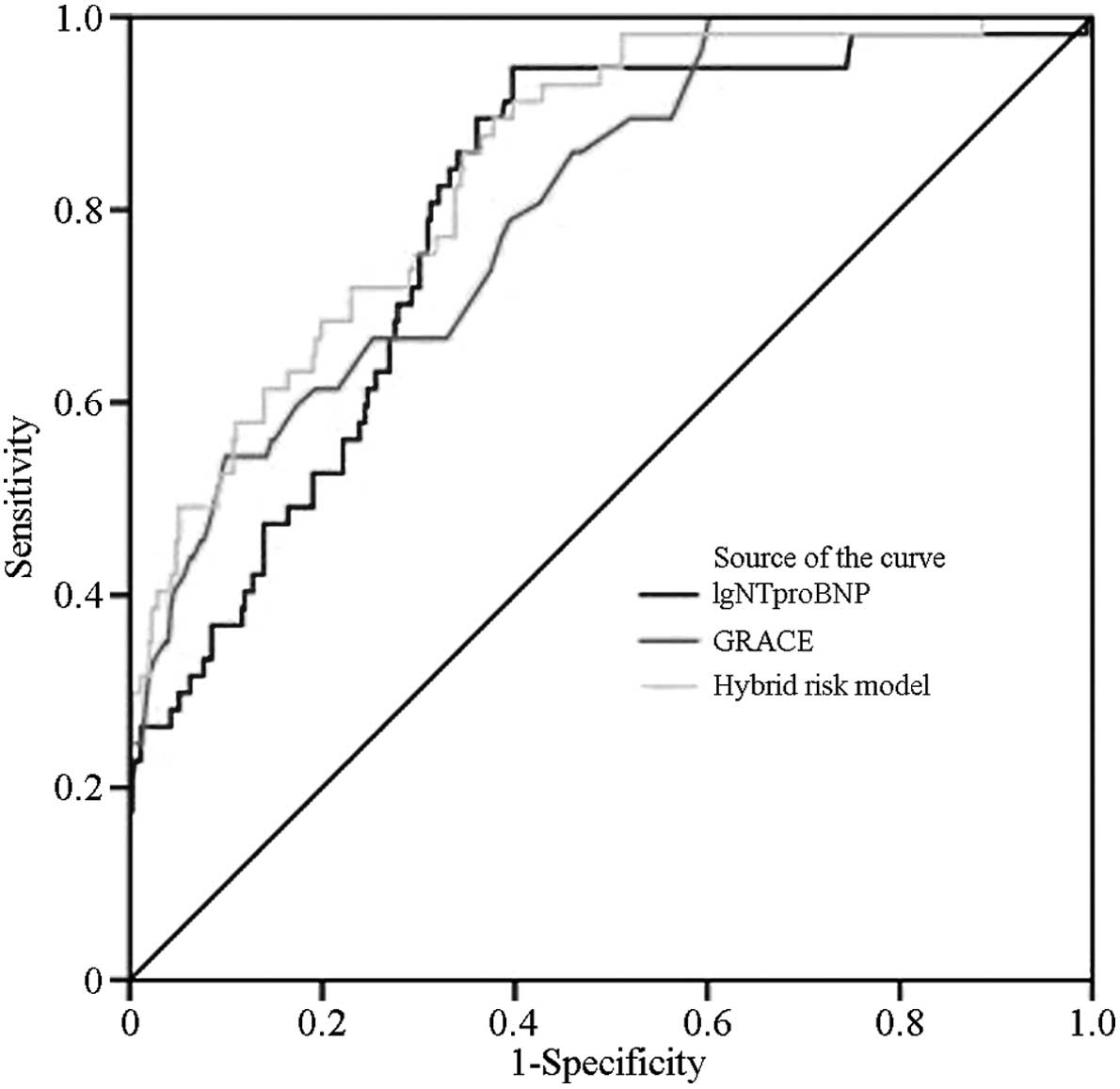
Areas under the ROC curves of the
NT-proBNP concentrations, GRACE scores and the hybrid risk model
indicate an ability to predict MACE
Model-establishing group
The area under the ROC curves for the lgNT-proBNP
concentrations and GRACE scores of the model-establishing group
were 0.798 (P=0.000) and 0.807 (P=0.000), respectively. These
results suggested that both methods are able to predict MACE. The
area under the ROC curve for the hybrid risk model was
significantly increased (0.843), as compared with those of the
GRACE score and the lgNT-proBNP concentration (P<0.05; Fig. 2; Table
II); thus suggesting that the hybrid risk model has a greater
predictive ability, as compared with either of its
constituents.
 | Table II.Comparison of the AUCs of the
lgNT-proBNP concentration, GRACE scores and hybrid risk model of
409 NSTE-ACS patients in the prediction model group. |
Table II.
Comparison of the AUCs of the
lgNT-proBNP concentration, GRACE scores and hybrid risk model of
409 NSTE-ACS patients in the prediction model group.
| Index | AUC | P (<0.05) | 95%CI |
|---|
| lgNT-proBNP | 0.798 | 0.000 | 0.740–0.856 |
| GRACE score | 0.807 | 0.000 | 0.749–0.865 |
| Hybrid risk
model | 0.843 | 0.000 | 0.791–0.895 |
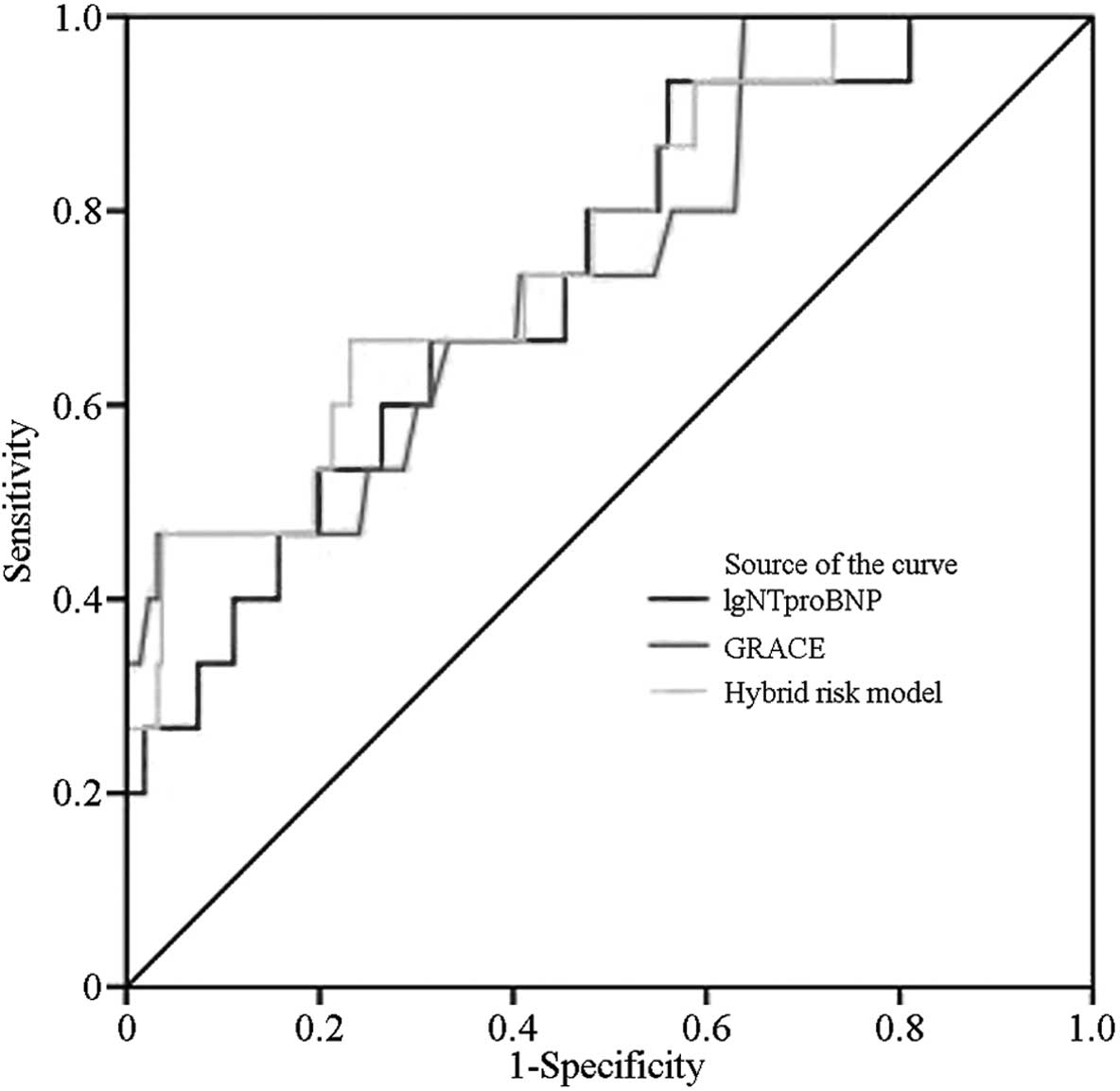
Prediction model group
The area under the ROC curve of the hybrid risk
model of the prediction model group was 0.762, which was
significantly increased, as compared with that of the GRACE score
(0.748; P<0.05; Fig. 3; Table III).
 | Table III.Comparison of AUCs of the lgNT-proBNP
concentration, GRACE scores and hybrid risk model of 231 NSTE-ACS
patients in the prediction model group. |
Table III.
Comparison of AUCs of the lgNT-proBNP
concentration, GRACE scores and hybrid risk model of 231 NSTE-ACS
patients in the prediction model group.
| Index | AUC | P (<0.05) | 95%CI |
|---|
| lgNT-proBNP | 0.734 | 0.002 | 0.606, 0.862 |
| GRACE score | 0.748 | 0.001 | 0.615, 0.881 |
| Hybrid risk
model | 0.762 | 0.001 | 0.633, 0.891 |
Discussion
Risk stratification has an important role in the
evaluation and management of patients with ACS, since these
patients exhibit varying prognoses. The existing guidelines
recommend that patients should undergo a risk assessment upon
hospital admission (20,21); thus suggesting that timely and
accurate risk stratification may go towards improving the prognosis
of a patient. The brain natriuretic peptide (BNP) is a biomarker
that is rapidly released into the blood when myocardial cells are
stretched or the wall tension is increased (13). BNP and NT-proBNP are derived from the
same source and are secreted in equimolar concentrations. NT-proBNP
is more stable in vitro and has a longer half-life, as
compared with BNP; thus, the present study selected NT-proBNP for
incorporation into the hybrid risk model. Previous studies have
demonstrated an association between the levels of BNP and heart
failure; myocardial ischemia led to a decrease in myocardial
contractility and increased wall tension, which in turn initiated
the release of BNP from myocardial cells.
In the model-establishing group in the present
study, ROC curves for the lgNT-proBNP concentrations and GRACE
scores were prepared, in order to compare the abilities of these
variables to predict MACE. The areas under the ROC curves were
>0.7; thus suggesting that both variables were able to
independently predict MACE. In addition, the lgNT-proBNP
concentration was positively correlated with the GRACE score in the
model-establishing group (r=0.507; P<0.001). The hybrid risk
model was obtained by combining lgNT-proBNP with the GRACE score,
and was simplified to the following equation: Hybrid risk model =
GRACE score + 20 × lgNT-proBNP + 15. The ROC curve of the
simplified hybrid risk model overlapped with that of the
un-simplified model (both AUC=0.762); thus suggesting that the
simplified and un-simplified hybrid risk model had identical
clinical values, and that the simplified hybrid risk model may
replace the un-simplified hybrid risk model for clinical
applications.
In the prediction model group, the area under the
ROC curve of the hybrid risk model was 0.762, which was
significantly increased, as compared with that of the GRACE score
(0.748; P=0.001). These results suggested that the hybrid risk
model may be better able to predict MACE, as compared with the
GRACE score alone. Following re-stratification, seven cases in the
high-risk group of the model-establishing group were downgraded to
the moderate-risk group, eight cases of the high-risk group were
downgraded to the low-risk group, and 10 cases of the low-risk
group were upgraded to the high-risk group; thus 6% of patients
were re-grouped. Among the 26 MACE cases, one case in the
moderate-risk group was upgraded to the high-risk group, and three
cases in the low-risk group were upgraded to the moderate-risk
group; thus 15% of MACE cases were re-grouped. The results of the
present study suggested that the hybrid risk model was able to
reduce the number of patients in the high-risk group that did not
experience MACE, reduce the number of patients in the low-risk
group that experienced MACE, and improve the predictive ability of
MACE. These results were consistent with a previous study involving
248 patients with ACS, which similarly combined NT-proBNP and the
GRACE scores (17); however, since
this study only involved ACS patients, and the sample size for
model establishment was small, there existed certain limitations.
In particular, the incidences and mortality rates of NSTE-ACS have
been shown to be higher, as compared with STE-ACS; therefore,
NSTE-ACS should be considered separately when generating risk
models for the prediction of MACE.
The present study aimed to establish a hybrid risk
model for the prediction of MACE in patients with NSTE-ACS, by
combining the GRACE scoring system and the lgNT-proBNP
concentration. The NT-proBNP concentration has previously been
associated with patient prognosis; the plasma concentration of
NT-proBNP was demonstrated to be predictive of the prognosis of a
patient with heart failure, stable angina and ACS (22). In addition, NT-proBNP has been shown
to be a marker of heart failure; therefore, cardiac insufficiency
was excluded from the inclusion criteria, in order to reduce its
impact on NT-proBNP concentrations. Numerous previous studies have
reported that patients with ACS and cardiac insufficiency (Killip
grading, grade 2) had a high mortality rate (13,23–25). As
compared with the GRACE scores of such indicators as Killip grading
and cardiac enzymes, NT-proBNP was demonstrated to be an
independent risk factor of ACS in the present study. Furthermore,
NT-proBNP was able to predict the prognosis of patients with ACS in
a way that was more convenient and cheaper, as compared with the
echocardiogram; therefore it may be beneficial to measure plasma
NT-proBNP concentration on patient admission. However, the addition
of the NT-proBNP concentration into a new risk model has been
challenging, and required further study by professional
cardiovascular researchers (26,27).
In conclusion, the plasma NT-proBNP concentration
and the GRACE scoring system are independent risk factors of MACE
that, when combined into a hybrid risk model in the present study,
showed improved accuracy for the prediction of MACE in patients
with NSTE-ACS.
Acknowledgements
The authors would like to thank Ms Weihong He and Mr
Li Sheng (both Capital Medical University) for their contribution
to the present study.
References
|
1
|
Roffi M, Patrono C, Collet JP, Mueller C,
Valgimigli M, Andreotti F, Bax JJ, Borger MA, Brotons C, Chew DP
and Gencer B: 2015 ESC Guidelines for the management of acute
coronary syndromes in patients presenting without persistent
ST-segment elevation: Task force for the management of acute
coronary syndromes in patients presenting without persistent
ST-segment elevation of the European Society of Cardiology (ESC).
Eur Heart J. 2015.ehv320
|
|
2
|
Anderson JL, Adams CD, Antman EM, Bridges
CR, Califf RM, Casey DE Jr, Chavey WE II, Fesmire FM, Hochman JS,
Levin TN, et al: American College of Cardiology; American Heart
Association Task Force on Practice Guidelines (Writing Committee to
Revise the 2002 Guidelines for the Management of Patients With
Unstable Angina/Non-ST-Elevation Myocardial Infarction); American
College of Emergency Physicians; Society for Cardiovascular
Angiography and Interventions; Society of Thoracic Surgeons;
American Association of Cardiovascular and Pulmonary
Rehabilitation; Society for Academic Emergency Medicine: ACC/AHA
2007 guidelines for the management of patients with unstable
angina/non-ST-elevation myocardial infarction: A report of the
American College of Cardiology/American Heart Association task
force on practice guidelines (writing committee to revise the 2002
guidelines for the management of patients with unstable
angina/non-ST-elevation myocardial infarction) developed in
collaboration with the American College of Emergency Physicians,
the Society for Cardiovascular Angiography and Interventions, and
the Society of Thoracic Surgeons endorsed by the American
Association of Cardiovascular and Pulmonary Rehabilitation and the
Society for Academic Emergency Medicine. J Am Coll Cardiol.
50:e1–e157. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Amsterdam EA, Wenger NK, Brindis RG, Casey
DE Jr, Ganiats TG, Holmes DR Jr, Jaffe AS, Jneid H, Kelly RF,
Kontos MC, et al: American College of Cardiology; American Heart
Association Task Force on Practice Guidelines; Society for
Cardiovascular Angiography and Interventions; Society of Thoracic
Surgeons; American Association for Clinical Chemistry: 2014 AHA/ACC
guideline for the management of patients with non-ST-elevation
acute coronary syndromes: A report of the American College of
Cardiology/American Heart Association Task Force on Practice
Guidelines. J Am Coll Cardiol. 64:e139–228. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Khalill R, Han L, Jing C and Quan H: The
use of risk scores for stratification of non-ST elevation acute
coronary syndrome patients. Exp Clin Cardiol. 14:e25–e30.
2009.PubMed/NCBI
|
|
5
|
Granger CB, Goldberg RJ, Dabbous O, Pieper
KS, Eagle KA, Cannon CP, Van De Werf F, Avezum A, Goodman SG,
Flather MD, et al: Predictors of hospital mortality in the global
registry of acute coronary events. Arch Intern Med. 163:2345–2353.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Eagle KA, Lim MJ, Dabbous OH, Pieper KS,
Goldberg RJ, Van de Werf F, Goodman SG, Granger CB, Steg PG, Gore
JM, et al: A validated prediction model for all forms of acute
coronary syndrome: Estimating the risk of 6-month postdischarge
death in an international registry. JAMA. 291:2727–2733. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kozieradzka A, Kamiński KA, Maciorkowska
D, Olszewska M, Dobrzycki S, Nowak K, Kralisz P, Prokopczuk P and
Musial WJ: GRACE, TIMI, Zwolle and CADILLAC risk scores - do they
predict 5-year outcomes after ST-elevation myocardial infarction
treated invasively. Int J Cardiol. 148:70–75. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lindahl B, Toss H, Siegbahn A, Venge P and
Wallentin L: Markers of myocardial damage and inflammation in
relation to long-term mortality in unstable coronary artery
disease. FRISC study group. Fragmin during instability in Coronary
artery disease. N Engl J Med. 343:1139–1147. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Morrow DA, Antman EM, Giugliano RP, Cairns
R, Charlesworth A, Murphy SA, de Lemos JA, McCabe CH and Braunwald
E: A simple risk index for rapid initial triage of patients with
ST-elevation myocardial infarction: An In TIME II substudy. Lancet.
358:1571–1575. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Meune C, Drexler B, Haaf P, Reichlin T,
Reiter M, Meissner J, Twerenbold R, Stelzig C, Freese M, Winkler K
and Mueller C: The GRACE score's performance in predicting
in-hospital and 1-year outcome in the era of high-sensitivity
cardiac troponin assays and B-type natriuretic peptide. Heart.
97:1479–1483. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Guidez T, Maréchaux S, Pincon C, Lamour H,
Barrailler S, Decourcelle V, Braun S, Bouabdallaoui N, Bauchart JJ,
Auffray JL, et al: Addition of B-type natriuretic peptide to the
GRACE score to predict outcome in acute coronary syndrome: A
retrospective (development) and prospective (validation)
cohort-based study. Emerg Med J. 29:274–279. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ang DS, Wei L, Kao MP, Lang CC and
Struthers AD: A comparison between B-type natriuretic peptide,
global registry of acute coronary events (GRACE) score and their
combination in ACS risk stratification. Heart. 95:1836–1842. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bosseau C, Galli E and Donal E: Prognostic
value of BNP in heart failure with preserved or reduced ejection
fraction. Heart. 101:1855–1856. 2015.PubMed/NCBI
|
|
14
|
Gong H, Wang X, Ling Y, Shi Y and Shi H:
Prognostic value of brain natriuretic peptide in patients with
heart failure and reserved left ventricular systolic function. Exp
Ther Med. 7:1506–1512. 2014.PubMed/NCBI
|
|
15
|
Tate S, Griem A, Durbin-Johnson B, Watt C
and Schaefer S: Marked elevation of B-type natriuretic peptide in
patients with heart failure and preserved ejection fraction. J
Biomed Res. 28:255–261. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Romel SM, Faruque M, Bari MA, Bari MS,
Aditya GP, Choudhury AK, Khalequzzaman M, Alam MM, Razzaque MA,
Rahman MA, et al: Association between elevated B-Type natriuretic
peptide levels with extent of coronary artery disease in patients
with unstable angina and NSTEMI. Mymensingh Med J. 23:544–551.
2014.PubMed/NCBI
|
|
17
|
Goyal BM, Sharma SM and Walia M: B-type
natriuretic peptide levels predict extent and severity of coronary
artery disease in non-ST elevation acute coronary syndrome and
normal left ventricular function. Indian Heart J. 66:183–187. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Granger CB, Goldberg RJ, Dabbous O, Pieper
KS, Eagle KA, Cannon CP, Van De Werf F, Avezum A, Goodman SG,
Flather MD and Fox KA: Global Registry of Acute Coronary Events
Investigators: Predictors of hospital mortality in the global
registry of acute coronary events. Arch Intern Med. 163:2345–2353.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Fox KA, Dabbous OH, Goldberg RJ, Pieper
KS, Eagle KA, Van de Werf F, Avezum A, Goodman SG, Flather MD,
Anderson FA Jr and Granger CB: Prediction of risk of death and
myocardial infarction in the six months after presentation with
acute coronary syndrome: Prospective multinational observational
study (GRACE). BMJ. 333:10912006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Pollack CV Jr and Braunwald E: 2007 update
to the ACC/AHA guidelines for the management of patients with
unstable angina and non-ST-segment elevation myocardial infarction:
Implications for emergency department practice. Ann Emerg Med.
51:591–606. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bassand JP, Hamm CW, Ardissino D, Boersma
E, Budaj A, Fernandez-Aviles F, Fox KA, Hasdai D, Ohman EM,
Wallentin L, et al: Guidelines for the diagnosis and treatment of
non-ST-segment elevation acute coronary syndromes. Rev Port
Cardiol. 27:1063–1143. 2008.(In Portuguese). PubMed/NCBI
|
|
22
|
Omland T, Sabatine MS, Jablonski KA, Rice
MM, Hsia J, Wergeland R, Landaas S, Rouleau JL, Domanski MJ, Hall
C, et al: Prognostic value of B-Type natriuretic peptides in
patients with stable coronary artery disease: The PEACE Trial. J Am
Coll Cardiol. 50:205–214. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Killip T III and Kimball JT: Treatment of
myocardial infarction in a coronary care unit. A two year
experience with 250 patients. Am J Cardiol. 20:457–464. 1967.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Fathy SA, Abdel Hamid FF, Zabut BM, Jamee
AF, Ali MA and Abu Mustafa AM: Diagnostic utility of BNP, corin and
furin as biomarkers for cardiovascular complications in type 2
diabetes mellitus patients. Biomarkers. 20:460–469. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Salama R, El-Moniem A, El-Hefney N and
Samor T: N-terminal pro-BNP in acute coronary syndrome patients
with ST elevation (STE-ACS) versus non ST elevation (NSTE-ACS). Int
J Health Sci (Qassim). 5(2 Suppl 1): 27–29. 2011.PubMed/NCBI
|
|
26
|
Møller JE, Pellikka PA, Hillis GS and Oh
JK: Prognostic importance of diastolic function and filling
pressure in patients with acute myocardial infarction. Circulation.
114:438–444. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Richardson-Lobbedez M, Maréchaux S,
Bauters C, Darchis J, Auffray JL, Bauchart JJ, Aubert JM, LeJemtel
TH, Lesenne M, Van Belle E, et al: Prognostic importance of tissue
Doppler-derived diastolic function in patients presenting with
acute coronary syndrome: A bedside echocardiographic study. Eur J
Echocardiogr. 9:594–598. 2008. View Article : Google Scholar : PubMed/NCBI
|