Introduction
Endometriosis (EMS) is a common benign gynecological
disorder, which is invasive and prone to metastasis (1). It has been estimated that endometriosis
is present in 6–10% of reproductive age women and in up to 20–40%
of infertile women (2). The
mechanism underlying the etiology of EMS remains unclear and no
efficient treatment is available. Seeking an effective therapeutic
approach has been the focus of numerous studies in recent
years.
Mammalian target of rapamycin (mTOR) is a
serine/threonine kinase that integrates a wide range of signaling
pathways, leading to its involvement in divergent physiological
processes, including transcription, translation, ribosome
biogenesis and apoptosis (3). mTOR
has been demonstrated to be a crucial regulator in certain types of
malignant cancer (4,5) and has been shown to be tightly
associated with the occurrence and development of EMS (6). Rapamycin (RAPA), an inhibitor of mTOR,
was found to be involved in the induction of cell apoptosis,
suppression of cancer cell proliferation, invasion and angiogenesis
in tumors (7,8). In addition, Leconte et al
(9) revealed that blocking the mTOR
signaling pathway inhibits the formation of deep infiltrating EMS
nodules in mice. However, the overall effects of mTOR inhibitors on
EMS remain unclear and the possible underlying mechanism is
unknown.
Hypoxia-inducible factor-1α (HIF-1α), which is a
general regulatory factor in the response to hypoxia, regulates the
expression of vascular endothelial growth factor (VEGF) and various
upstream enzymes, resulting in the regulation of the process of
angiogenesis (10). The occurrence
and development of angiogenesis in EMS has been closely associated
with ischemia and hypoxia of the ectopic endometrium (11–13). In
our previous studies, it was demonstrated that HIF-1α is involved
in the process of angiogenesis in EMS (14,15).
Furthermore, previous studies reported that mTOR was able to
enhance the expression of HIF-1α, thereby promoting the expression
of VEGF (16).
In the present study, the effect of RAPA on EMS and
its possible mechanism were investigated in order to provide new
evidence for a targeted EMS therapy. The study investigated the
effect of RAPA on the development of EMS lesions and microvessel
density (MVD), as well as the expression of HIF-1α and VEGF.
Materials and methods
Animals and reagents
A total of 30 female specific pathogen free (SPF)
CB17 severe combined immunodeficiency (SCID) mice (weight,
17.02±0.75 g; age, 6–7 weeks) were purchased from Beijing Vital
River Laboratory Animal Technology Co., Ltd. (Beijing, China). RAPA
was purchased from LC Laboratories (Woburn, MA, USA). Mouse HIF-1α
and VEGF ELISA kits (cat. nos. CSB-E08541m and CSB-E04756m,
respectively) were obtained from Sino-American Biotechnology Co.,
Ltd. (Wuhan, China). Mouse anti-human HIF-1α polyclonal antibody
(1:100; cat. no. BM0912) was purchased from Wuhan Boster Biological
Technology, Ltd. (Wuhan, China). Mouse anti-human VEGF (1:200; cat.
no. RB-9031) and CD34 (1:100; cat. no. MS-363) monoclonal
antibodies, streptomycin avidin-peroxidase (SP) immunochemistry
(cat. no. Kit-9701) and DAB (cat. no. Kit-0017) kits were from
Maxim Biotech, Inc. (Fuzhou, China). Lidocaine and pentobarbital
were obtained from Sigma-Aldrich (St. Louis, MO, USA). Formalin,
paraffin and bovine serum albumin (BSA) Sangon Biotech, Co., Ltd.
(Shanghai, China). Citric acid and sodium citrate were purchased
from Guangzhou Chemical Reagent Factory (Guangzhou, China).
Animal model
Tissue samples were acquired from 15 female patients
during laparoscopic resection of EMS at the Departments of
Obstetrics and Gynecology at the Guangzhou Red Cross Hospital
(Guangzhou, China) between January 2014 and February 2014. The
average age of the participants was 32±8 years. Informed consent
was obtained from all the participants prior to the procedure. The
samples were confirmed to be eutopic secretory endometrial tissues
by a pathologist who was blinded to the research design. The
tissues were sectioned into 1-mm3 fragments and stored
temporarily in a cold sterile bottle with an appropriate volume of
Dulbecco's modified Eagle's medium (GE Healthcare Life Sciences,
Logan, UT, USA) for <1 h. This study was approved by the Ethics
Committee of Zhujiang Hospital of Southern Medical University.
In order to establish an EMS-SCID animal model, 2 ml
of the tissue suspension obtained from the EMS patients was
injected into the abdominal cavity of 30 female SPF CB17 SCID mice
within 60 min after the harvest of the tissue sample. The mice were
maintained in cages (5 mice/cage), under SPF conditions at 22–24°C
and 50–70% relative humidity, and under a 12-h light/dark cycle.
All mice were fed a normal laboratory diet. After 4 weeks, the
EMS-SCID mouse model was successfully established, as confirmed by
endometrial tissue investigation during laparotomy, which showed a
cyst on the internal abdominal wall. For laparotomy, 0.1 ml 2%
lidocaine was injected subcutaneously. The volume of EMS lesions
prior to treatment (V1) were measured, according to the method of
Katsuki (17), the 30 EMS-SCID mice
were then randomly assigned into three groups (n=10 each), as
follows: i) RAPA group, in which the lesions were injected with 250
µg/mouse RAPA once per week; ii) control group, receiving no
treatment; and iii) saline group, receiving lesions were injected
with 0.25 ml/mouse saline once per week. There was no difference in
the V1 among the three groups (P>0.05). At 2 weeks after the
initiation of treatment (V2), blood samples were collected from the
orbit of the mice following removal of the eyeball. Subsequently,
all animals were sacrificed with an overdose of pentobarbital (100
mg/kg), and the volume of EMS lesions following treatment was
measured using the previously mentioned method.
ELISA
Blood samples were obtained from the orbit of the
mice prior to sacrifice. Serum was collected by centrifugation for
15 min at 1,000 × g. Serum HIF-1α and VEGF protein expression
levels were measured by ELISAs, according to the manufacturer's
protocols. The serum concentrations of HIF-1α and VEGF were
quantified using a standard curve constructed according to the
absorbance and concentrations of standard samples.
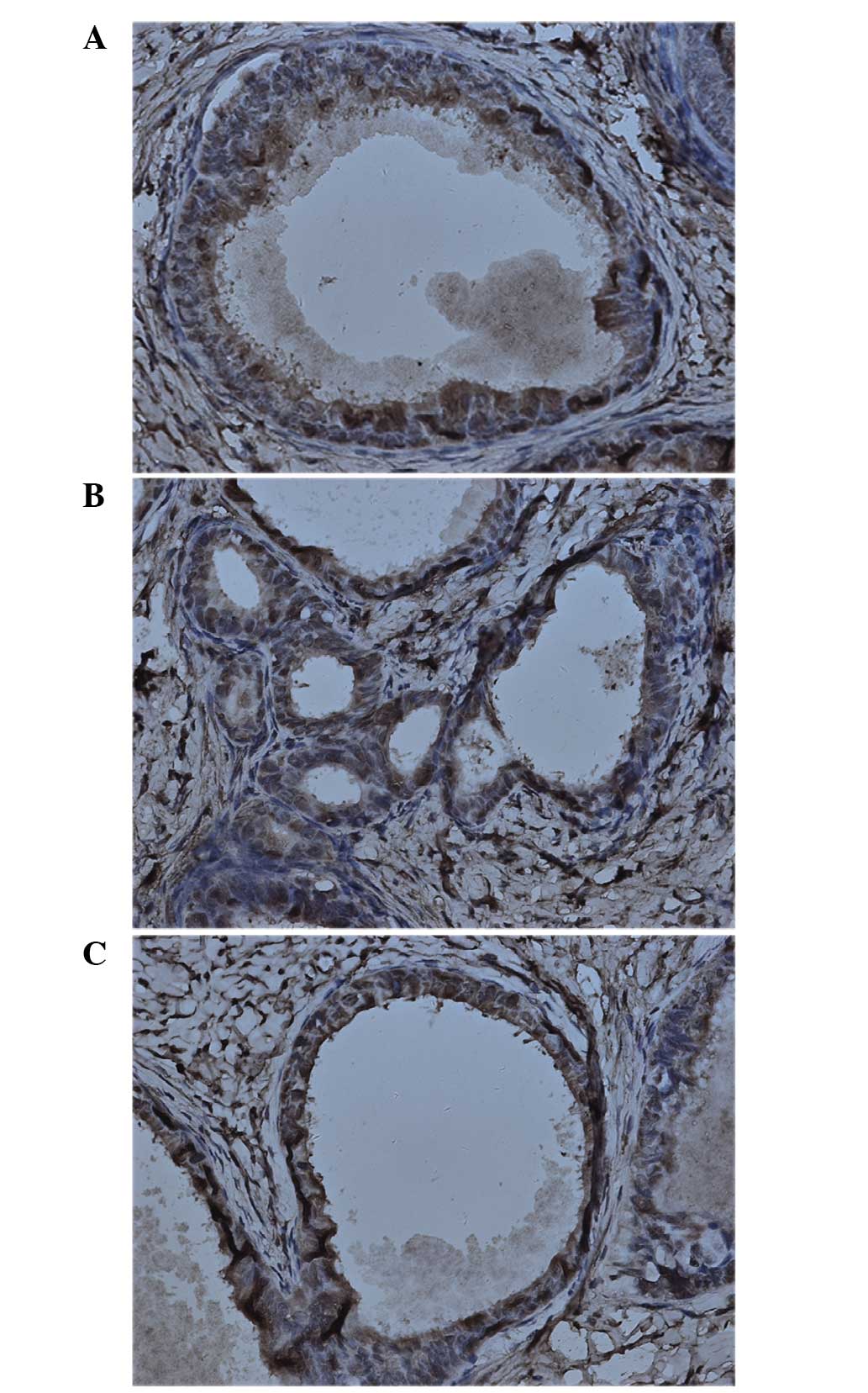
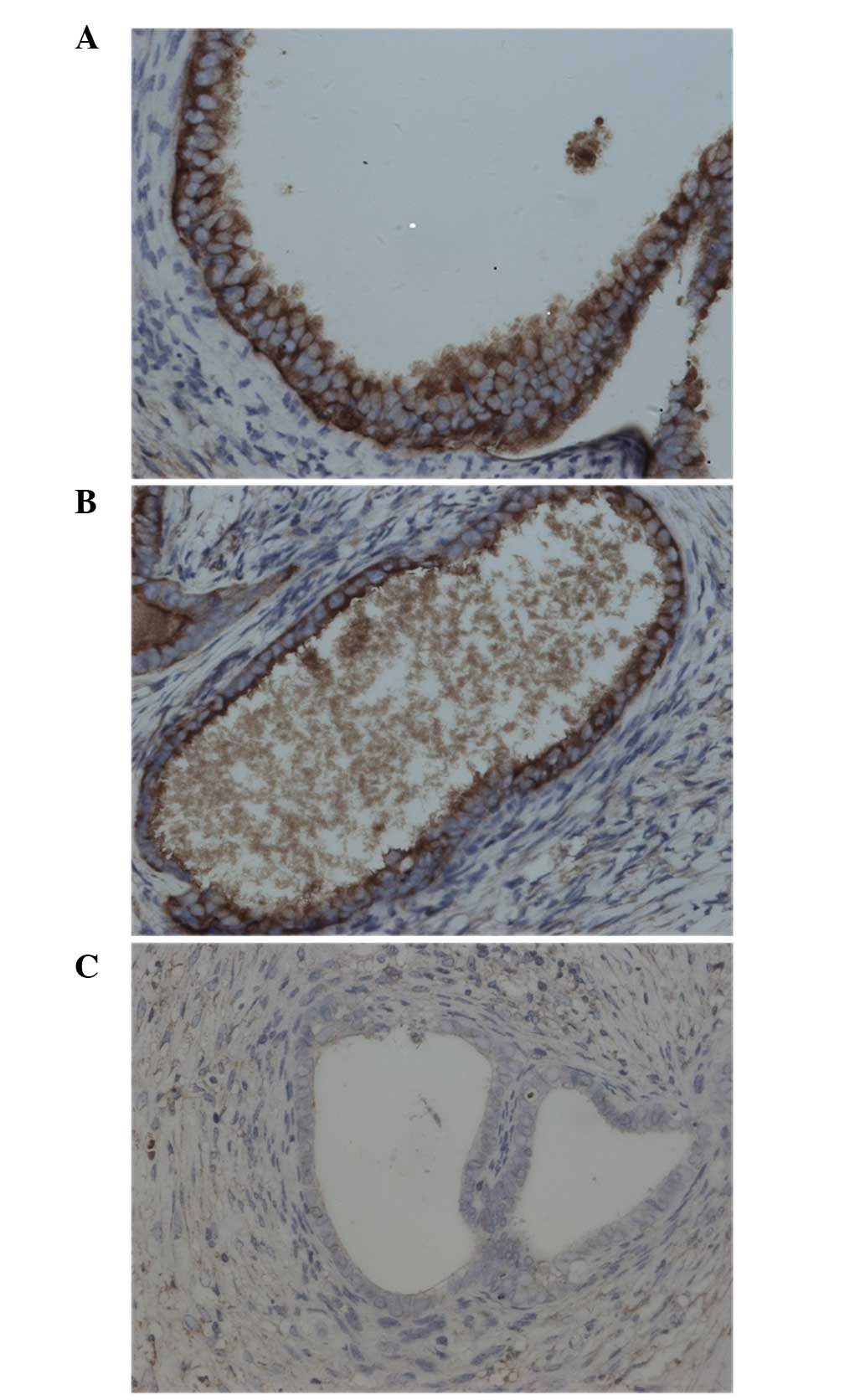
Immunohistochemistry
The protein expression levels of HIF-1α, VEGF and
CD34 in the EMS lesions of the mice were measured by
immunohistochemical analysis. Briefly, the tissue samples of
endometriotic foci obtained after sacrifice were fixed in 10%
formalin and then embedded in paraffin. The tissues were cut into
~4-µm sections. Antigen repair was conducted by microwave heating
in 0.1% citrate buffer (0.4 g citric acid dissolved in 3 g sodium
citrate in 1 L deionized water). After blocking with 5% BSA at room
temperature for 20 min, the slides were incubated overnight at 4°C
with mouse anti-HIF-1α (1:100), anti-VEGF (1:200) or anti-CD34
(1:100) antibodies. Protein expression was detected according to
the protocols of the SP and DAB kits. Brown staining in the
cytoplasm, as observed under a light microscope (Olympus BX51;
Olympus Corporation, Tokyo, Japan), was indicative of HIF-1α, VEGF
or CD34 protein expression.
The results of immunohistochemistry were reviewed
independently by two senior pathologists blinded to the outcome of
the tumors. Semi-quantitative analysis of HIF-1α, VEGF and CD34
expression levels was performed by consensus and comprised both the
intensity of staining (negative as 0, light yellow as 1, brown as
2, tan as 3) for each cell and the extent of staining (ratio of
positive cells/counted cells; 1 for 25%, 2 for 25–50%, 3 for 51–75%
and 4 for 75%) for each random field. The scores for the intensity
and extent of staining were multiplied to give a weighted score for
each case (maximum possible score, 12). For statistical analysis,
the weighted scores were grouped into four categories, wherein a
score of 0 was considered negative, scores of 1–4 (+) were regarded
as low positive expression levels, and scores of 5–8 (++) and 9–12
(+++) were regarded as high positive expression levels.
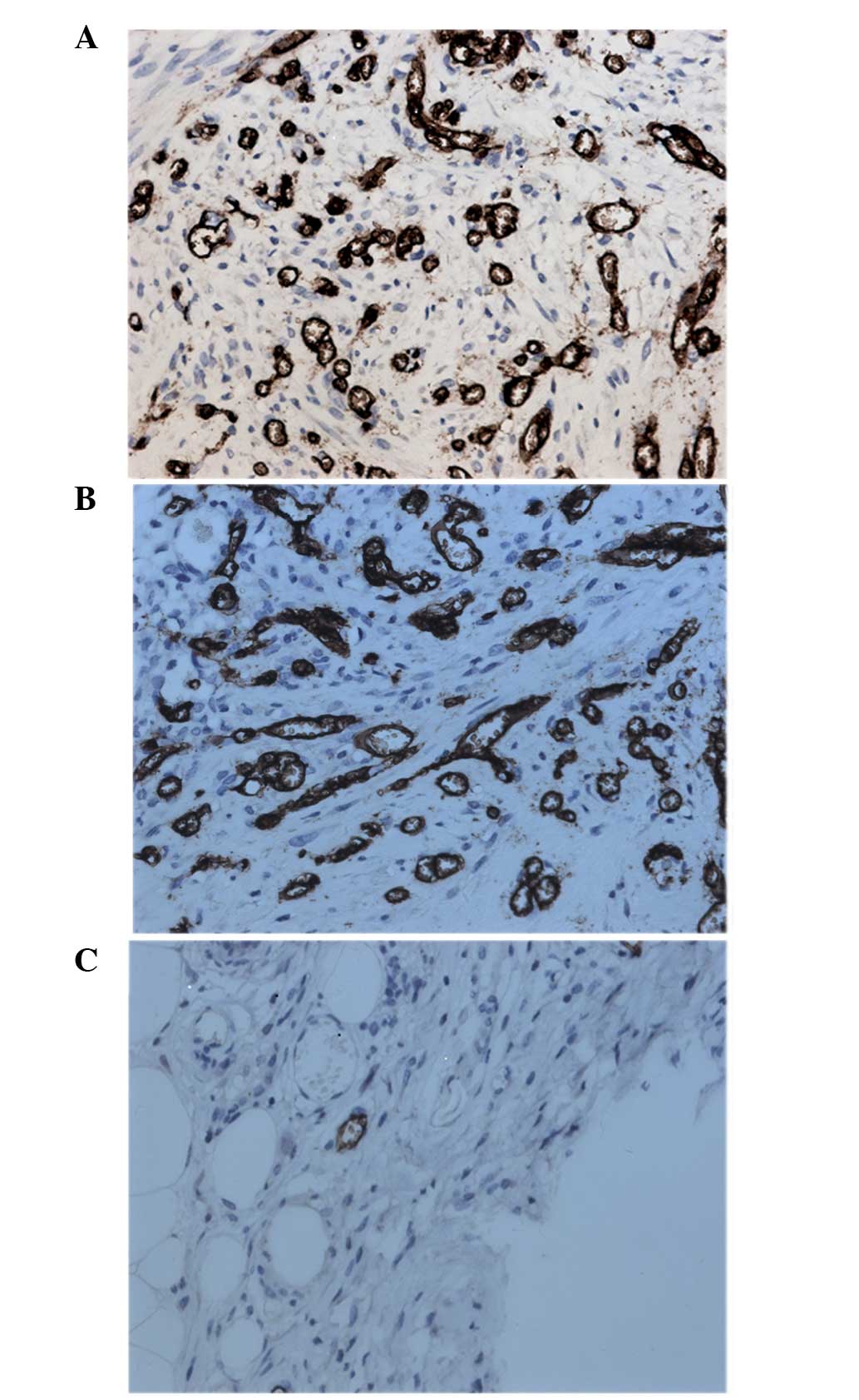
MVD
The MVD was assessed as previously described
(18). Briefly, under a light
microscope (Olympus Corporation), the immunostained section was
scanned at low magnification (×40) and three areas with the highest
density of microvessels were identified as ‘hotspots’. All the
vessels in these ‘hotspot’ areas were then counted at high
magnification (×200), and each slide was examined individually by
two pathologists blinded to the research design.
Statistical analysis
The results are expressed as the mean ± standard
deviation. Statistical analysis was conducted with SPSS 19.0
software (IBM SPSS, Armonk, NY, USA). Comparisons between groups
were performed using one-way analysis of variance test. All the
numerical data were tested for homogeneity and distribution.
Ordinal data were tested by Wilcoxon signed-rank test. A P-value of
<0.05 was considered to indicate a statistically significant
difference.
Results
Effect of RAPA on the growth of
endometriotic lesions in mice
In order to observe the effect of RAPA on the
endometriotic lesions in mice, the volume of lesions was measured
prior to treatment (V1) and after 2 weeks of treatment (V2). As
shown in Table I, the V2 of the
control and saline groups were comparable with V1 of all the
groups. However, the V2 of the RAPA group was significantly
decreased when compared with its corresponding V1, as well as
compared with V2 of the control and saline groups (P<0.05).
These findings indicated that RAPA significantly suppressed the
growth of the endometriosis lesions.
 | Table I.Endometriotic lesion volume in the
mice (mean ± standard deviation; n=10 mice/group). |
Table I.
Endometriotic lesion volume in the
mice (mean ± standard deviation; n=10 mice/group).
| Group | V1
(mm3) | V2
(mm3) |
|---|
| RAPA | 230.85±13.74 |
51.25±9.31a,b |
| Control | 219.56±14.79 | 229.44±10.01 |
| Saline | 231.34±13.41 | 210.71±10.96 |
Effect of RAPA on the serum levels of
HIF-1α and VEGF
In order to investigate the effect of RAPA on the
expression of HIF-1α and VEGF, the serum levels of these factors
were determined by ELISA. As shown in Table II, the serum levels of HIF-1α and
VEGF in the saline groups were comparable with those in the
corresponding control group levels. Notably, there was no
statistically significant difference in the serum HIF-1α levels
among the RAPA, control and saline groups. However, treatment with
RAPA markedly reduced the serum levels of VEGF, when compared with
those in the control and saline groups (P<0.05).
 | Table II.Serum levels of HIF-1α and VEGF in the
mice (mean ± standard deviation; n=10 mice/group). |
Table II.
Serum levels of HIF-1α and VEGF in the
mice (mean ± standard deviation; n=10 mice/group).
| Group | HIF-1α (pg/ml) | VEGF (pg/ml) |
|---|
| RAPA | 1.575±0.290 | 0.128±0.030 |
| Control | 1.668±0.223 | 0.169±0.029 |
| Saline | 1.660±0.205 | 0.162±0.030 |
Effect of RAPA on the expression of
HIF-1α and VEGF in endometriotic lesions
In order to confirm the effect of RAPA on the
location and expression of HIF-1α and VEGF, their expression in
endometriotic lesions was determined by immunohistochemical
staining. The results showed that HIF-1α and VEGF were mainly
present in the cytoplasm of glandular epithelium. In addition, weak
immunoreactivity for HIF-1α and VEGF was observed in the ectopic
endometrial stromal cells in the control group (Figs. 1 and 2). The results of the staining intensity
are summarized in Tables III and
IV. There was no significant
difference in the staining for HIF-1α among the RAPA, control and
saline groups. However, the VEGF expression in the RAPA group was
significantly lower compared with that of the control and saline
groups.
 | Table III.Intensity of immunohistochemical
staining for HIF-1α in endometriotic lesions (n=10 mice/group). |
Table III.
Intensity of immunohistochemical
staining for HIF-1α in endometriotic lesions (n=10 mice/group).
|
| HIF-1α |
|---|
|
|
|
|---|
| Group | − | + | ++ | +++ |
|---|
| RAPA | 0 | 4 | 2 | 4 |
| Control | 0 | 4 | 3 | 3 |
| Saline | 0 | 3 | 4 | 3 |
 | Table IV.Intensity of immunohistochemical
staining for VEGF in endometriotic lesions (n=10 mice/group). |
Table IV.
Intensity of immunohistochemical
staining for VEGF in endometriotic lesions (n=10 mice/group).
|
| VEGF |
|---|
|
|
|
|---|
| Group | − | + | ++ | +++ |
|---|
| RAPA | 7 | 3 | 0 | 0 |
| Control | 0 | 5 | 3 | 2 |
| Saline | 0 | 4 | 5 | 1 |
Effect of RAPA on MVD in entometriotic
lesions
As a marker of endothelial cells, CD34 was assayed
by immunohistochemistry in order to evaluate the effect of RAPA on
MVD in endometriotic lesions. As shown in Table V, the MVD in the saline group was
comparable with that in the control group (Table V). As expected, treatment with RAPA
significantly reduced the MVD when compared with that the in
control and saline groups. In addition, as shown in Fig. 3, positive staining of CD34 was
observed in the endothelial cells, which were comma, stripe or
tube-shaped with clear lumens. The incidence of angiogenesis was
also significantly suppressed in the RAPA-treated group compared
with that in the control group (Fig.
3). Therefore, these findings indicated that RAPA inhibited
endothelial cell proliferation and the resulting angiogenesis.
 | Table V.MVD in endometriotic lesions in mice
(mean ± standard deviation; n=10 mice/group). |
Table V.
MVD in endometriotic lesions in mice
(mean ± standard deviation; n=10 mice/group).
| Group | MVD |
|---|
| RAPA |
5.38±0.18a |
| Control | 35.54±1.19 |
| Saline | 36.26±1.28 |
Discussion
As a common gynecologic disease, the incidence of
EMS has been increasing in recent years (2). The implantation of ectopic endometrium,
the resultant infertility and repeated abdominal pain greatly
affect EMS patients (2,19). A previous study demonstrated that
angiogenesis serves an important role not only in the development
and repair of normal endometrium, but also in the occurrence and
development of EMS (20). Excessive
angiogenesis may be critical for the ectopic implantation and
growth of the endometrium, which results in EMS (21,22). In
the present study, we hypothesized that the effective inhibition of
angiogenesis may block the occurrence and development of EMS.
HIF-1, a heterodimer composed of the HIF-1α and
HIF-1β subunits, is a transcription factor that is widely found in
the tissues of mammals under hypoxic or anoxic stress (23). HIF-1α is the unique oxygen-regulated
subunit and determines the activity of HIF-1. Furthermore, it is a
hypoxia inducible global regulator and contributes to the
transcriptional regulation of the expression of VEGF and certain
enzymes associated with glycolysis (24–26).
Additionally, HIF-1α is the regulator directly involved in the
entire process of angiogenesis (10). VEGF, also known as vascular
permeability factor, is an important proangiogenic factor, which
selectively binds VEGF receptor in endothelial cells, serving a
proangiogenic role (27).
Angiogenesis during EMS has been found to be closely associated
with hypoxia in the endometrium (28). As a regulator of proangiogenic
factors, particularly of VEGF, HIF-1α serves a critical role in the
angiogenesis process in EMS (28).
Our previous study demonstrated that HIF-1α functionally
contributes to angiogenesis during EMS (15).
mTOR, an atypical serine/threonine kinase, is
important for cell growth and is involved in a wide variety of
physiological functions. This kinase also regulates the expression
of proangiogenic factors (such as VEGF) at the transcriptional and
translational levels. An abnormal mTOR signaling pathway has been
identified in various types of malignant neoplasm, while the
aberrant activation of mTOR has been confirmed to mediate
angiogenesis and contribute to neoplasm development (29). Based on these functions, the mTOR
signaling pathway has been a novel target in the treatment of
neoplasm and mTOR inhibitors have been identified as the third
generation of antiangiogenic pharmaceuticals (30). RAPA is the first identified specific
inhibitor of mTOR. A previous study has demonstrated that RAPA is
able to significantly inhibit the growth of cell lines derived from
various tumors, including breast, lung, colorectal and renal
carcinoma (31). In addition, RAPA
has an anti-angiogenesis activity, and this effect is most probably
due to at least the following two mechanisms: i) Direct inhibition
of the proliferation of endothelial cells mediated by VEGF; and ii)
inhibition of the proliferative effect of HIF-1 on endothelial
cells. Hudson et al (32) has
shown that RAPA inhibits the expression levels of VEGF and
platelet-derived growth factor through the downregulation of HIF-1α
expression, leading to suppression of new vascular occurrence in
prostate cancer. Another study found that, in multiple myeloma,
RAPA reduced VEGF receptor expression and therefore inhibited the
endothelial cell differentiation and vascular sprouting, reducing
angiogenesis in multiple myeloma (33). Laschke et al (34) also demonstrated that RAPA attenuated
ectopic endometrium in vivo through inhibition of
angiogenesis and cell proliferation.
In the present study, RAPA was shown to
significantly attenuate the development of endometriotic lesions,
as well as to inhibit MVD and the expression of VEGF in
endometriotic lesions. However, RAPA had no significant effect on
HIF-1α expression in the lesions, which may be due to the direct
inhibitory role of RAPA in the VEGF expression, supported by
presence of various mTOR-independent pathways to regulate HIF-1α
expression in EMS. Although the role of mTOR in the expression of
HIF-1α remains controversial, it is widely agreed that the ultimate
effect of the complicated signaling pathways regulated by hypoxia
determines the expression of HIF-1α.
In conclusion, the present study observed the effect
of RAPA on the development of endometriotic lesions and
investigated the mechanism of EMS to provide new evidence for the
treatment of the disease with RAPA. mTOR inhibitors, represented by
RAPA in the current study, may be potentially used in targeted
therapy for EMS. However, the clinical efficacy, side effects and
the use of mTOR inhibitors in combination with other targeted
pharmaceuticals require further evaluation. Biomarkers for the
clinical efficacy of mTOR inhibitors also require further
investigation.
Acknowledgements
The present study was funded by Guangzhou Medical
Science and Technology Project 2013 (grant no. 2013A011030016) and
the Guangdong Province Science and Technology Plan Projects 2015
(grant no. 20140212).
References
|
1
|
Zhan L, Wang W, Zhang Y, Song E, Fan Y and
Wei B: Hypoxia-inducible factor-1alpha: A promising therapeutic
target in endometriosis. Biochimie. 123:130–137. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Khan KN, Kitajima M, Fujishita A, Hiraki
K, Matsumoto A, Nakashima M and Masuzaki H: Pelvic pain in women
with ovarian endometrioma is mostly associated with coexisting
peritoneal lesions. Hum Reprod. 28:109–118. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Huynh H: Molecularly targeted therapy in
hepatocellular carcinoma. Biochem Pharmacol. 80:550–560. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Olivares-Reyes JA, Arellano-Plancarte A
and Castillo-Hernandez JR: Angiotensin II and the development of
insulin resistance: Implications for diabetes. Mol Cell Endocrinol.
302:128–139. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Makker A, Goel MM, Das V and Aqarwal A:
PI3K-Akt-mTOR and MAPK signaling pathways in polycystic ovarian
syndrome, uterine leiomyomas and endometriosis: An update. Gnnecol
Endocrinol. 28:175–81. 2012. View Article : Google Scholar
|
|
6
|
McKinnon BD, Kocbek V, Nirgianakis K,
Bersinger NA and Mueller MD: Kinase signalling pathways in
endometriosis: Potential targets for non-hormonal therapeutics. Hum
Reprod Update. Jan 5–2016.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ashworth RE and Wu J: Mammalian target of
rapamycin inhibition in hepatocellular carcinoma. World J Hepatol.
6:776–782. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Beck JT, Ismail A and Tolomeo C: Targeting
the phosphatidylinositol 3-kinase (PI3K)/AKT/mammalian target of
rapamycin (mTOR) pathway: An emerging treatment strategy for
squamous cell lung carcinoma. Cancer Treat Rev. 40:980–989. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Leconte M, Nicco C, Ngô C, Chéreau C,
Chouzenoux S, Marut W, Guibourdenche J, Arkwright S, Weill B,
Chapron C, et al: The mTOR/AKT inhibitor temsirolimus prevents deep
infiltrating endometriosis in mice. Am J Pathol. 179:880–889. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Pugh CW and Ratcliffe PJ: Regulation of
angiogenesis by hypoxia: Role of the HIF system. Nat Med.
9:677–684. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lu Z, Zhang W, Jiang S, Zou J and Li Y:
Effect of oxygen tensions on the proliferation and angiogenesis of
endometriosis heterograft in severe combined immunodeficiency mice.
Fertil Steril. 101:568–576. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lu Z, Zhang W, Jiang S, Zou J and Li Y:
Effect of lesion location on endometriotic adhesion and
angiogenesis in SCID mice. Arch Gynecol Obstet. 289:823–830. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sharkey AM, Day K, McPherson A, Malik S,
Licence D, Smith SK and Charnock-Jones DS: Vascular endothelial
growth factor expression in human endometrium is regulated by
hypoxia. J Clin Endocrinol Metab. 85:402–409. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ren X, He YL, Pan SL and Peng DX:
Expression of hypoxia-inducible factor-1alpha in endometriosis. Nan
Fang Yi Ke Da Xue Xue Bao. 27:538–540. 2007.(In Chinese).
PubMed/NCBI
|
|
15
|
Ren X, He Y and Peng D: The expression of
hypoxia-inducible factor-1α and the relationship with microvessel
density in endometriosis. Guangdong yi xue. 28:229–231. 2007.(In
Chinese).
|
|
16
|
Martin KA and Blenis J: Coordinate
regulation of translation by the PI 3-kinase and mTOR pathways. Adv
Cancer Res. 86:1–39. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Katsuki Y, Takano Y, Futamura Y, Shibutani
Y, Aoki D, Udagawa Y and Nozawa S: Effects of dienogest, a
synthetic steroid, on experimental endometriosis in rats. Eur J
Endocrinol. 138:216–226. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Weidner N: Current pathologic methods for
measuring intratumoral microvessel density with in breast carcinoma
and other solid tumors. Breast Cancer Res Treat. 36:169–180. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Berkes E, Bokor A and Rigó J Jr.: Current
treatment of endometriosis with laparoscopic surgery. Orv Hetil.
151:1137–1144. 2010.(In Hungarian). View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Young VJ, Ahmad SF, Brown JK, Duncan WC
and Horne AW: Peritoneal VEGF-A expression is regulated by TGF-β1
through an ID1 pathway in women with endometriosis. Sci Rep.
5:168592015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Fujimoto J, Sakaguchi H, Hirose R, Wen H
and Tamaya T: Angiogenesis in endometriosis and angiogenic factors.
Gynecol Obstet Invest. 48(Suppl 1): 14–20. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Soysal D, Kizildag S, Saatli B, Posaci C,
Soysal S, Koyuncuoglu M and Dogan O: A novel angiogenesis inhibitor
bevacizumab induces apoptosis in the rat endometriosis model.
Balkan J Med Genet. 17:73–80. 2015.PubMed/NCBI
|
|
23
|
Uchida T, Rossignol F, Matthay MA, Mounier
R, Couette S, Clottes E and Clerici C: Prolonged hypoxia
differentially regulates hypoxia-inducible factor (HIF)-1alpha and
HIF-2alpha expression in lung epithelial cells: Implication of
natural antisense HIF-1alpha. J Biol Chem. 279:14871–14878. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Jian-Lin Z, Hong-Song F, Hao P, Shuang D,
Shen C, Jian-Ping L, Bo Q, Jin-Qing W and Feng L: The relationship
between HIF-2α and VEGF with radiographic severity in the primary
osteoarthritic knee. Yonsei Med J. 57:735–740. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Bae WY, Choi JS, Kim JE and Jeong JW:
Cinnamic aldehyde suppresses hypoxia-induced angiogenesis via
inhibition of hypoxia-inducible factor-1α expression during tumor
progression. Biochem Pharmacol. 98:41–50. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Remels AH, Gosker HR, Verhees KJ, Langen
RC and Schols AM: TNF-α-induced NF-κB activation stimulates
skeletal muscle glycolytic metabolism through activation of HIF-1α.
Endocrinology. 156:1770–1781. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Shibuya M: Vascular endothelial growth
factor and its receptor system: Physiological functions in
angiogenesis and pathological roles in various diseases. J Biochem.
153:13–19. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Machado-Linde F, Pelegrin P,
Sanchez-Ferrer ML, Leon J, Cascales P and Parrilla JJ:
2-methoxyestradiol in the pathophysiology of endometriosis: Focus
on angiogenesis and therapeutic potential. Reprod Sci.
19:1018–1029. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Dufour M, Dormond-Meuwly A, Demartines N
and Dormond O: Tarageting the mammalian target of rapamycin (mTOR)
in cancer therapy: Lessions from past and future perspectives.
Cancers (Basel). 3:2478–2500. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ganjoo K and Jacobs C: Antiangiogenesis
agents in the treatment of soft tissue sarcomas. Cancer.
116:1177–1183. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Sarbassov DD, Guertin DA, Ali SM and
Sabatini DM: Phosphorylation and regulation of AKT/PKB by the
rictor-mTOR complex. Science. 307:1098–1101. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Hudson CC, Liu M, Chiang GG, Otterness DM,
Loomis DC, Kaper F, Giaccia AJ and Abraham RT: Regulation of
hypoxia-inducible factor1 alpha expression and function by the
mammalian target of rapamycin. Mol Cell Biol. 22:7004–7014. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Mirsgahi P, Toprak SK, Faussat AM,
Dubrulle S, Marie JP, Soria C, Soria J and Mirshahi M: Malignant
hematopoietic cells induce an increased expression of VEGFR-1 and
VEGFR-3 on bone marrow endothelial cells via AKT and mTOR
signalling pathways. Biochem Biophys Res Commun. 349:1003–1010.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Laschke MW, Elitzsch A, Scheuer C,
Holstein JH, Vollmar B and Menger MD: Rapamycin induces regression
of endometriotic lesions by inhibiting neovascularization and cell
proliferation. Br J Pharmacol. 149:137–144. 2006. View Article : Google Scholar : PubMed/NCBI
|