Introduction
Electrical storm (ES) is a dramatic and
life-threatening syndrome which is defined by three or more
sustained episodes of ventricular tachycardia (VT), ventricular
fibrillation (VF), or appropriate shocks from an implantable
cardioverter-defibrillator within 24 h (1–3). This
pathology is may cause fatal arrhythmia in certain patients with
severe heart disease (4,5). Once an electrical storm occurs, the
control of ventricular tachycardia/fibrillation using standard
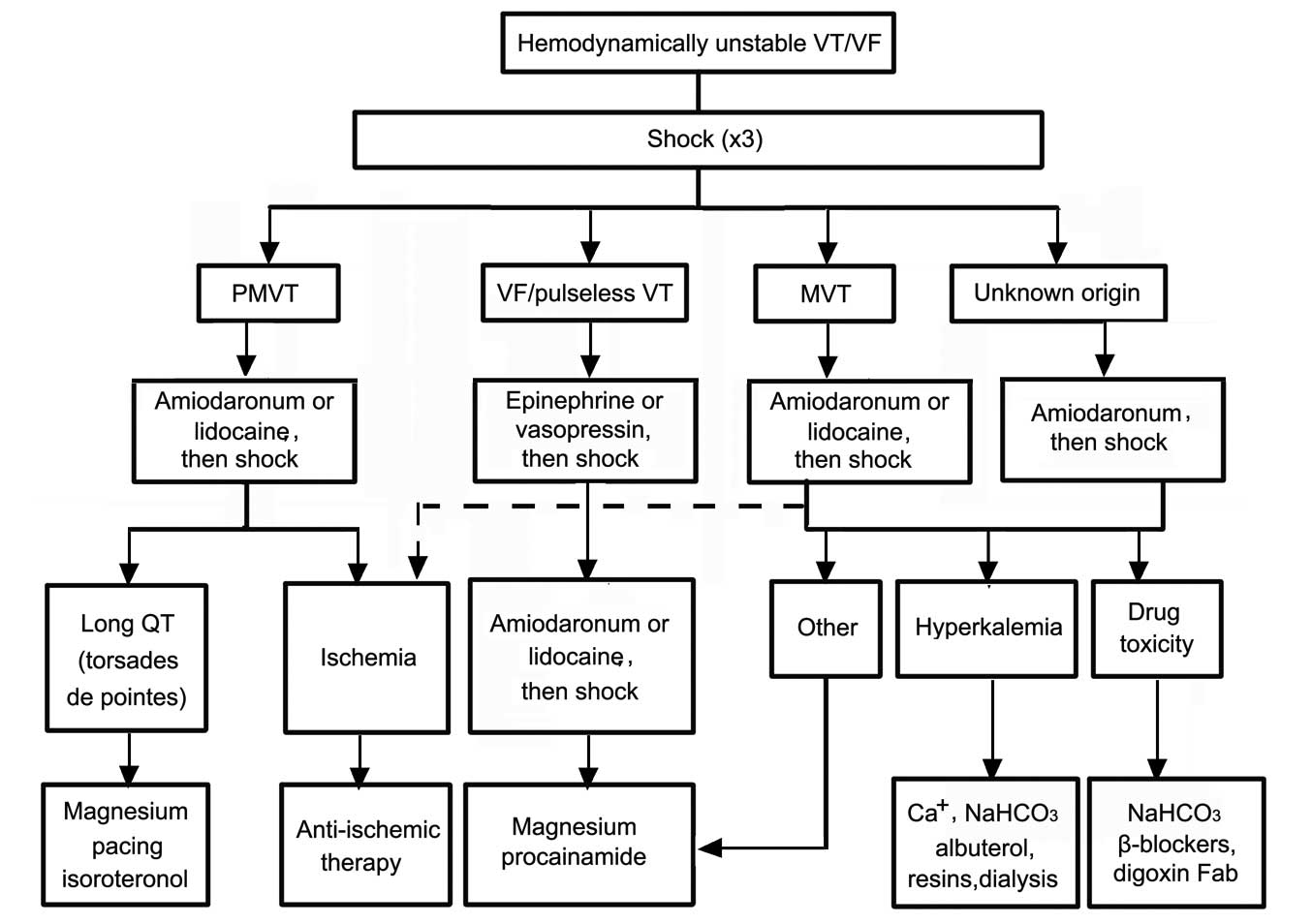
treatment alone is difficult (6–9). A
schematic of the emergent treatment of ventricular arrhythmias is
shown in Fig. 1. ES can manifest
itself during post-infarction ischemic heart disease, various forms
of cardiomyopathy, an implantable cardioverter-defibrillator, or an
inherited arrhythmic syndrome, such as Brugada syndrome (1,10–16). ES
typically has a poor outcome (17).
The intravenous injection of class III antiarrhythmic drugs,
including, amiodaronum and nifekalant, is used initially to inhibit
ventricular arrhythmia in the majority of patients (18,19).
However, electrical storms can show resistance to, or not be
affected by these drugs, which is a major problem in the
application of emergency medical care (20,21). In
the present study, a case of ventricular electrical storm in a
patient with dilated cardiomyopathy is reported, that was
successfully treated by esmolol infusion.
Case report
A 43-year-old woman was referred to the Department
of Cardiology, Jinan Central Hospital Affiliated to Shandong
University (Jinan, China) on December 3, 2010. She underwent two
defibrillator shocks within 24 h after having survived sudden
cardiac death. The patient presented with a respiratory infection
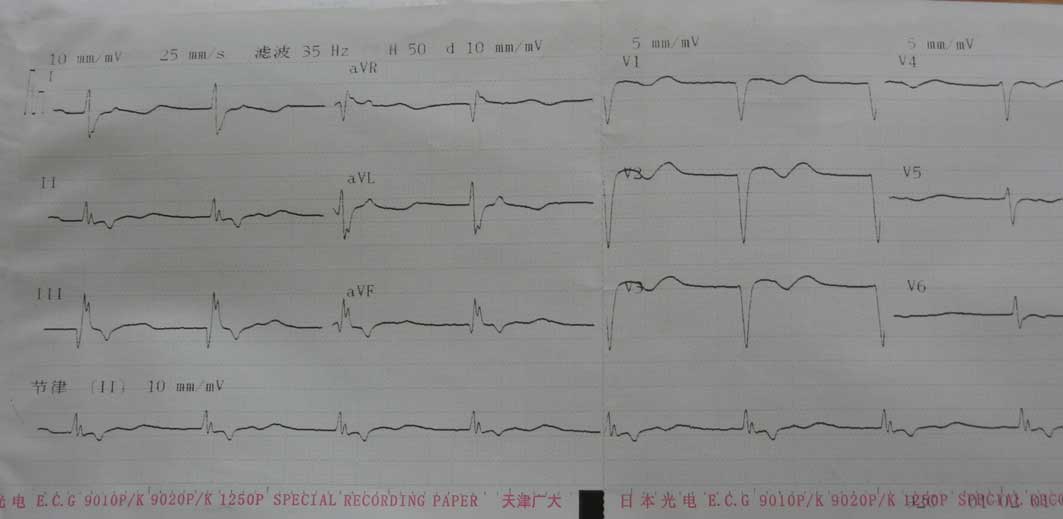
20 days prior to admission. An intercritical electrocardiogram
(ECG) was recorded upon admission using a 6-channel ECG system
(ECG-1250P; Nihon Kohden, Inc., Tokyo, Japan) which detected a
sinus rhythm and intraventricular block (Fig. 2). Transthoracic echocardiography
revealed markedly enlarged left ventricular end-diastolic dimension
[76 mm; normal range (NR), 42.5±7.5 mm] and lowered left
ventricular ejection fraction (18%; NR, 65±5%), mild mitral
regurgitation and mild elevation of pulmonary arterial pressure
(pulmonary artery mean pressure, 34 mm Hg; NR, 10±5 mmHg). Dilated
cardiomyopathy is a myocardial disease characterized by dilatation
and impaired contraction of the left ventricle or both ventricles
(22). The patient presented with
sudden arrhythmic death. Transthoracic echocardiography revealed
dilated cardiomyopathy with severe global left ventricular systolic
dysfunction with an estimated left ventricular ejection fraction of
18%. These symptoms excluded ischemic heart disease and led to a
diagnosis of dilated cardiomyopathy.
Initial laboratory tests revealed hypokalemia (2.9
mmol/l; NR, 4.4±0.9 mmol/l), high serum B-type natriuretic peptide
(739 pg/ml; NR, <100 pg/ml), normal magnesium levels, no
hypercalcemia, and normal troponin I and creatine phosphokinase
enzyme levels. Following admission, the patient was under close
observation. Genetic testing was not performed, and the patient had
no family history of dilated cardiomyopathy. Informed consent was
obtained from the patient on the day of admission. The present
study was approved by the Ethics Committee of Jinan Central
Hospital Affiliated to Shandong University.
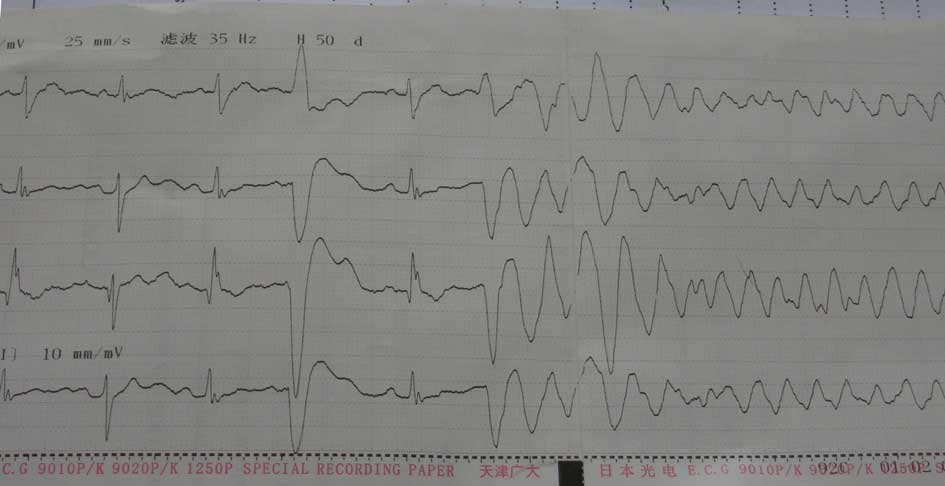
In the following duration of hospital stay, 40
episodes of polymorphic ventricular tachycardia and ventricular
fibrillation occurred within 24 h; recurrent polymorphic
non-sustained and sustained ventricular tachycardia, triggered by
ventricular premature beat, appeared incessantly and degenerated
into polymorphic sustained ventricular tachycardia (Fig. 3). Repeated electrical cardioversion
procedures were performed (54 in total). Firstly, the patient was
prescribed high-dose amiodaronum (2 mg/min; ivp; Sanofi
Pharmaceutical Co., Ltd., Paris, France), which is a class III
antiarrhythmic drug, but gradual tapering of the amiodaronum
infusion resulted in the recurrence of the electrical storm, which
required frequent cardioversions. One day later, 58 episodes of
polymorphic ventricular tachycardia/fibrillation occurred
repeatedly, repeated electrical cardioversion procedures were
performed (66 in total, indicating that the electrical storm
exhibited resistance to amiodaronum. A number of clinical studies
have demonstrated that β-blockers effectively suppress electrical
storm (23–26); therefore, middle-dose esmolol
(0.05–0.2 mg/kg/min; ivp; Oilu Pharmaceutical Co/. Ltd., Jinan,
China), which is a β1-receptor blocker, was prescribed (20,21).
Following an intravenous bolus injection of 0.5 mg esmolol, an
infusion of esmolol at a rate of 0.15 mg/kg/min (ivp) was
administered. No ventricular fibrillation occurred repeatedly
during an interruption of the infusion for 24 h. The patient was
free of ventricular tachycardia/fibrillation, although the
premature ventricular beats persisted for 2 weeks following the
application of esmolol (Fig. 4). The
patient received oral bisoprolol fumarate (β-blockade; 5 mg/day;
Merck Millipore, Darmstadt, Germany) to treat these premature
ventricular beats until she was discharged on January 7, 2011.
During the treatment of the electrical storm, serum
electrolytes (including Mg2+, K+ and
Ca2+) were maintained at high levels by the infusion of
intravenous electrolyte solution. When the acute phase of the
electrical storm was controlled, the focus of treatment shifted
toward maximizing heart-failure therapy and preventing subsequent
ventricular arrhythmias. The patient was prescribed oral losartan
(angiotensin receptor blocker; 50 mg/day; Novartis Pharma AG,
Basel, Switzerland), oral bisoprolol fumarate (β-blockade; 5
mg/day), oral spironolactone (aldosterone antagonist; 20 mg twice
daily), oral digoxin (digitalis; 0.125 mg/day; both Shanghai Xinyi
Pharmaceutical Co., Ltd., Shanghai, China) furosemidum (loop
diuretic; 40 mg twice daily; ivp; Shanghai He Feng Pharmaceutical
Co., Ltd., Shanghai, China). Following this, the patient discharged
on January 7, 2011 in a hemodynamically stable condition.
Discussion
Typically, electrical storms have a poor prognosis;
they are defined as three or more distinct episodes of ventricular
fibrillation, or hemodynamically destabilizing ventricular
tachycardia occurring within a 24-h period, typically requiring
treatment with electrical cardioversion or defibrillation (4).
Enhanced sympathetic nerve activity is associated
with episodes of ES (27,28) and β-blockade has been demonstrated to
reduce the risk of recurrent VT and VF (25). For patients with acute myocardial
infarction, the use of β-blockade decreases the risk of sudden
death, as β-blockers reduce mortality by preventing VT and VF
(26). β-blockers treatment should
be limited in patients with labile hemodynamic compensation or
severe reduction of LV function. An electrical storm in patients
with dilated cardiomyopathy occurs rarely with only a few reported
cases. Once non-ischemic cardiomyopathy occurs, the heart
experiences structural changes. Fibrosis results in scarring, which
leads to regions of conduction block; however, groups of myofibrils
are able to survive, particularly those surrounding the border of
the scar. Slow conduction through these regions can facilitate
electrically stable reentry (29–32).
It is acknowledged that amiodaronum and β-blockers,
particularly the former, are able to treat arrhythmia effectively
in the majority of patients. The present study presents an
organized approach for effectively evaluating and managing
electrical storms. β-blocker administration has antiarrhythmic and
antiadrenergic effect. Its administration should be limited in
patients with severe reduction of LV function or haemodynamic
instability. Esmolol is a selective ultra short β1 blocker. The
present study presents esmolol for effectively managing electrical
storms in dilated cardiomyopathy with severe reduction of LV
function or haemodynamic instability. Firstly, a high dose of
amiodaronum was prescribed to treat cardiac electrical storm in a
patient experiencing dilated cardiomyopathy. However, when gradual
tapering of the amiodaronum infusion did not arrest the electrical
storm, and frequent cardioversions were required, esmolol was
administered in a bolus injection, followed by an infusion.
Following this, there were no further frequent repeats of
ventricular fibrillation. This suggests that esmolol is effective
in suppressing electrical storms, and that enhanced sympathetic
nerve activity is involved in episodes of electrical storms
(26,33).
In conclusion, the results strongly suggest that
esmolol may improve the survival rates of patients experiencing
electrical storms, and should be considered as a primary treatment
option. However, as esmolol can exacerbate heart failure in
patients with poor systolic function, its use in these patients
should be closely monitored.
Acknowledgements
The present study was supported by The National
Natural Science Funds for Young Scholar (grant no. 81200211), the
Shandong Young Scientists Award Fund (grant no. BS2012SW003) and
the Scientific and Technology Development program of Jinan (grant
no. 20120144).
References
|
1
|
Conti S, Pala S, Biagioli V, Del Giorno G,
Zucchetti M, Russo E, Marino V, Dello Russo A, Casella M,
Pizzamiglio F, et al: Electrical storm: A clinical and
electrophysiological overview. World J Cardiol. 26:555–561.
2015.
|
|
2
|
Sesselberg HW, Moss AJ, McNitt S, Zareba
W, Daubert JP, Andrews ML, Hall WJ, McClinitic B and Huang DT:
MADIT-II Research Group: Ventricular arrhythmia storms in
postinfarction patients with implantable defibrillators for primary
prevention indications: A MADIT-II substudy. Heart Rhythm.
4:1395–1402. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Exner DV, Pinski SL, Wyse DG, Renfroe EG,
Follmann D, Gold M, Beckman KJ, Coromilas J, Lancaster S and
Hallstrom AP: AVID Investigators: Electrical storm presages
nonsudden death: The antiarrhythmics versus implantable
defibrillators (AVID) trial. Circulation. 103:2066–2071. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Davis JE, Curtis LA and Rashid H:
Idiopathic cardiac electrical storm. J Emerg Med. 37:264–268. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Marrouche NF, Verma A, Wazni O, Schweikert
R, Martin DO, Saliba W, Kilicaslan F, Cummings J, Burkhardt JD,
Bhargava M, et al: Mode of initiation and ablation of ventricular
fibrillation storms in patients with ischemic cardiomyopathy. J Am
Coll Cardiol. 43:1715–1720. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Koplan BA and Stevenson WG: Ventricular
tachycardia and sudden cardiac death. Mayo Clin Proc. 84:289–297.
2009. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
ECC Committee, Subcommittees Task Forces
of the American Heart Association 2005 American Heart Association:
Guidelines for cardiopulmonary resuscitation and emergency
cardiovascular care. Circulation. 112:IV1–IV203. 2005.PubMed/NCBI
|
|
8
|
Mittadodla PS, Salen PN and Traub DM:
Isoproterenol as an adjunct for treatment of idiopathic ventricular
fibrillation storm in a pregnant woman. Am J Emerg Med.
30:251.e3–e5. 2012. View Article : Google Scholar
|
|
9
|
Miwa Y, Ikeda T, Mera H, Miyakoshi M,
Hoshida K, Yanagisawa R, Ishiguro H, Tsukada T, Abe A, Yusu S and
Yoshino H: Effects of landiolol, an ultra-short-acting
beta1-selective blocker, on electrical storm refractory to class
III antiarrhythmic drugs. Circ J. 74:856–863. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bänsch D, Oyang F, Antz M, Arentz T, Weber
R, Val-Mejias JE, Ernst S and Kuck KH: Successful catheter ablation
of electrical storm after myocardial infarction. Circulation.
108:3011–3016. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yusu S, Ikeda T, Mera H, Miyakoshi M, Miwa
Y, Abe A, Tsukada T, Ishiguro H, Shimizu H and Yoshino H: Effects
of intravenous nifekalant as a lifesaving drug for severe
ventricular tachyarrhythmias complicating acute coronary syndrome.
Circ J. 73:2021–2028. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Remo BF, Preminger M, Bradfield J, Mittal
S, Boyle N, Gupta A, Shivkumar K, Steinberg JS and Dickfeld T:
Safety and efficacy of renal denervation as a novel treatment of
ventricular tachycardia storm in patients with cardiomyopathy.
Heart Rhythm. 11:541–546. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Stefanelli CB, Bradley DJ, Leroy S, Dick M
II, Serwer GA and Fischbach PS: Implantable cardioverter
defibrillator therapy for life-threatening arrhythmias in young
patients. J Interv Card Electrophysiol. 6:235–244. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gatzoulis KA, Andrikopoulos GK,
Apostolopoulos T, Sotiropoulos E, Zervopoulos G, Brili S and
Stefanadis CI: Electrical storm is an independent predictor of
adverse long-term outcome in the era of implantable defibrillator
therapy. Europace. 7:184–192. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Meregalli P, Wilde A and Tan H:
Pathophysiological mechanisms of Brugada syndrome: Depolarization
disorder, repolarization disorder, or more? Cardiovasc Res.
67:367–378. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bettiol K, Gianfranchi L, Scarfo S,
Pacchioni F, Pedaci M and Alboni P: Successful treatment of
electrical storm with oral quinidine in Brugada syndrome. Ital
Heart J. 6:601–602. 2005.PubMed/NCBI
|
|
17
|
Kowey PR: An overview of antiarrhythmic
drug management of electrical storm. Can J Cardiol. 12:3B–8B.
1996.PubMed/NCBI
|
|
18
|
Van Herendael H and Dorian P: Amiodarone
for the treatment and prevention of ventricular fibrillation and
ventricular tachycardia. Vasc Health Risk Manag. 6:465–472.
2010.PubMed/NCBI
|
|
19
|
Kurisu K, Hisahara M, Onitsuka H, Sekiya
M, Ikeuchi M, Kozai T and Urabe Y: Nifekalant hydrochloride
terminated electrical storms after coronary surgery. Ann Thorac
Surg. 89:1637–1639. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sorajja D, Munger TM and Shen WK: Optimal
antiarrhythmic drug therapy for electrical storm. J Biomed Res.
29:20–34. 2015.PubMed/NCBI
|
|
21
|
Eifling M, Razavi M and Massumi A: The
evaluation and management of electrical storm. Tex Heart Inst J.
38:111–121. 2011.PubMed/NCBI
|
|
22
|
Richardson P, McKenna W, Bristow M, Maisch
B, Mautner B, O'Connell J, Olsen E, Thiene G, Goodwin J, Gyarfas I,
et al: Report of the 1995 World Health Organization/International
Society and Federation of Cardiology task force on the definition
and classification of cardiomyopathies. Circulation. 93:841–842.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Silva Marques J, Veiga A, Nóbrega J,
Correia MJ and de Sousa J: Electrical storm induced by H1N1 A
influenza infection. Europace. 12:294–295. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Balcells J, Rodriguez M, Pujol M and
Iglesias J: Successful treatment of long QT syndrome-induced
ventricular tachycardia with esmolol. Pediatr Cardiol. 25:160–162.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Moss AJ, Zareba W, Hall WJ, Klein H,
Wilber DJ, Cannom DS, Daubert JP, Higgins SL, Brown MW and Andrews
ML: Multicenter Automatic Defibrillator Implantation Trial II
Investigators: Prophylactic implantation of a defibrillator in
patients with myocardial infarction and reduced ejection fraction.
N Engl J Med. 346:877–883. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Nademanee K, Taylor R, Bailey WE, Rieders
DE and Kosar EM: Treating electrical storm: Sympathetic blockade
versus advanced cardiac life support-guided therapy. Circulation.
102:742–747. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Lombardi F, Verrier RL and Lown B:
Relationship between sympathetic neural activity, coronary dynamics
and vulnerability to ventricular fibrillation induced by myocardial
ischemia and reperfusion. Am Heart J. 105:958–965. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zipes DP: Influence of myocardial ischemia
and infarction on autonomic innervation of heart. Circulation.
82:1095–1105. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Hershberger RE, Morales A and Siegfried
JD: Clinical and genetic issues in dilated cardiomyopathy: A review
for genetics professionals. Genet Med. 12:655–667. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Streitner F, Herrmann T, Kuschyk J, Lang
S, Doesch C, Papavassiliu T, Streitner I, Veltmann C, Haghi D and
Borggrefe M: Impact of shocks on mortality in patients with
ischemic or dilated cardiomyopathy and defibrillators implanted for
primary prevention. PLoS One. 8:e639112013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kolettis TM, Naka KK and Katsouras CS:
Radiofrequency catheter ablation for electrical storm in a patient
with dilated cardiomyopathy. Hellenic J Cardiol. 46:366–369.
2005.PubMed/NCBI
|
|
32
|
Takigawa M, Noda T, Kurita T, Aihara N,
Yamada Y, Okamura H, Satomi K, Suyama K, Shimizu W and Kamakura S:
Predictors of electrical storm in patients with idiopathic dilated
cardiomyopathy - how to stratify the risk of electrical storm. Circ
J. 74:1822–1829. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Burjorjee JE and Milne B: Propofol for
electrical storm; a case report of cardioversion and suppression of
ventricular tachycardia by propofol. Can J Anaesth. 49:973–977.
2002. View Article : Google Scholar : PubMed/NCBI
|