Introduction
Kawasaki disease (KD), which was first reported by
Dr Tomisaku Kawasaki in 1967 (1), is
a syndrome of unknown cause and causes systemic vasculitis, with
symptoms that include persistent fever, bilateral conjunctival
congestionpolymorphous exanthema and, alterations of the lip, oral
cavity and peripheral extremities (2). It typically affects children under the
age of 5 years. Coronary artery lesion (CAL) is the most severe
complication of KD and it has been regarded as one of the major
acquired heart diseases in children (3). Therefore, KD has been a major focus in
the field of pediatric cardiology research. Although the
introduction of intravenous gamma globulin (IVIG) has effectively
reduced the rate of CALs, further research is required to ensure
early diagnosis and effective treatment of KD (4). Several epidemiologic surveys of KD have
been conducted worldwide since 1970′s, and various features of the
disease have been revealed, such as disease incidence, seasonality,
and the rate of CAL (3). KD has been
reported in numerous countries with a greatly varying incidence,
and the highest incidence of KD has been reported in Japan,
followed by other East Asian countries and districts surrounding
Japan (3). However, the epidemiology
of KD has only been reported in a limited number of regions in
China, and to the best of our knowledge, it has not been previously
determined in the Inner Mongolia Autonomous Region of China.
Therefore, in the present study, a survey was conduced to examine
the epidemiologic features of KD in Inner Mongolia between 2001 and
2013.
Materials and methods
Population
A retrospective study of patients treated for the KD
in Inner Mongolia between January 1st, 2001 and December 31st, 2013
was conducted. Regardless of ethnicity, patients with KD who were
aged <18 years old were identified by the discharge diagnosis
code in the records of 17 hospitals providing pediatric medical
services in Inner Mongolia, including Inner Mongolia Autonomous
Region People's Hospital; Maternal and Child Health Hospital of
Inner Mongolia; Inner Mongolia Medical University Affiliated
Hospital; Ordos Center Hospital; Chifeng Center Hospital;
Affiliated Hospital of Chifeng College; The Second Hospital of
Chifeng; Tongliao City Hospital; Affiliated Hospital of Inner
Mongolia National University; Hulunbuir City People's Hospital; The
First Hospital of Hohhot; Baotou Center Hospital; The Second
Hospital of Baotou; Linhe City Hospital; Baogang Hospital of Inner
Mongolia; The Fourth Hospital of Baotou; and The First and Second
Affiliated Hospital of Baotou Medical College. The medical records
of the patients with KD during the 13-year span of the study were
reviewed. The 5th revised edition of the diagnostic criteria for KD
that was issued by the Japan Kawasaki Disease Research Committee at
the 7th International Kawasaki Disease Symposium in 2002 was used
for the diagnosis of KD in all cases (2). In brief, the patients included in the
study presented at least 5 of the following 6 clinical
manifestations, or at least 4 symptoms along with coronary
abnormalities documented by echocardiography or coronary
angiography: i) Fever persisting for 5 days or longer (including
cases in which the fever has subsided before day 5 in response to
treatment); ii) bilateral conjunctival congestion; iii) alterations
in the lip and oral cavity areas, including diffuse congestion of
oral and pharyngeal mucosa, strawberry-colored tongue or reddening
of the lips; iv) polymorphous exanthema; v) alterations in the
peripheral extremities, such as reddening of the soles and palms,
indurative edema at the initial stages, or membranous desquamation
at the fingertips during the convalescent stage; and vi) acute
nonpurulent cervical lymphadenopathy (5). Patients who did not fulfill the
aforementioned criteria, were diagnosed beyond the specified time
period or were not residents of the Inner Mongolia region were
excluded from the present study.
Survey implementation
The clinical data collected from the eligible
patients included the following: Age, gender, ethnic background,
location of residence, dates of KD onset and diagnosis, days
between symptom onset and hospital visit, clinical signs and
symptoms, cardiac and extracardiac manifestations, laboratory
examination results (routine blood examination, erythrocyte
sedimentation rate and blood chemical tests), echocardiogram
results, treatment and outcome.
Statistical analysis
Parametric data are expressed as the mean ± standard
deviation. Nonparametric analysis was performed using Pearson's
χ2 test or Fisher's exact test. Differences between the
mean values were compared by t-test or one-way analysis of
variance. Single-factor analysis and nonconditional multivariate
logistic regression analysis were performed to analyze the risk
factors for the development of CAL. A value of P<0.05 was
considered to indicate a statistically significant difference. All
analyses were performed using SPSS software version 19.0 (SPSS,
Inc., Chicago, IL, USA).
Results
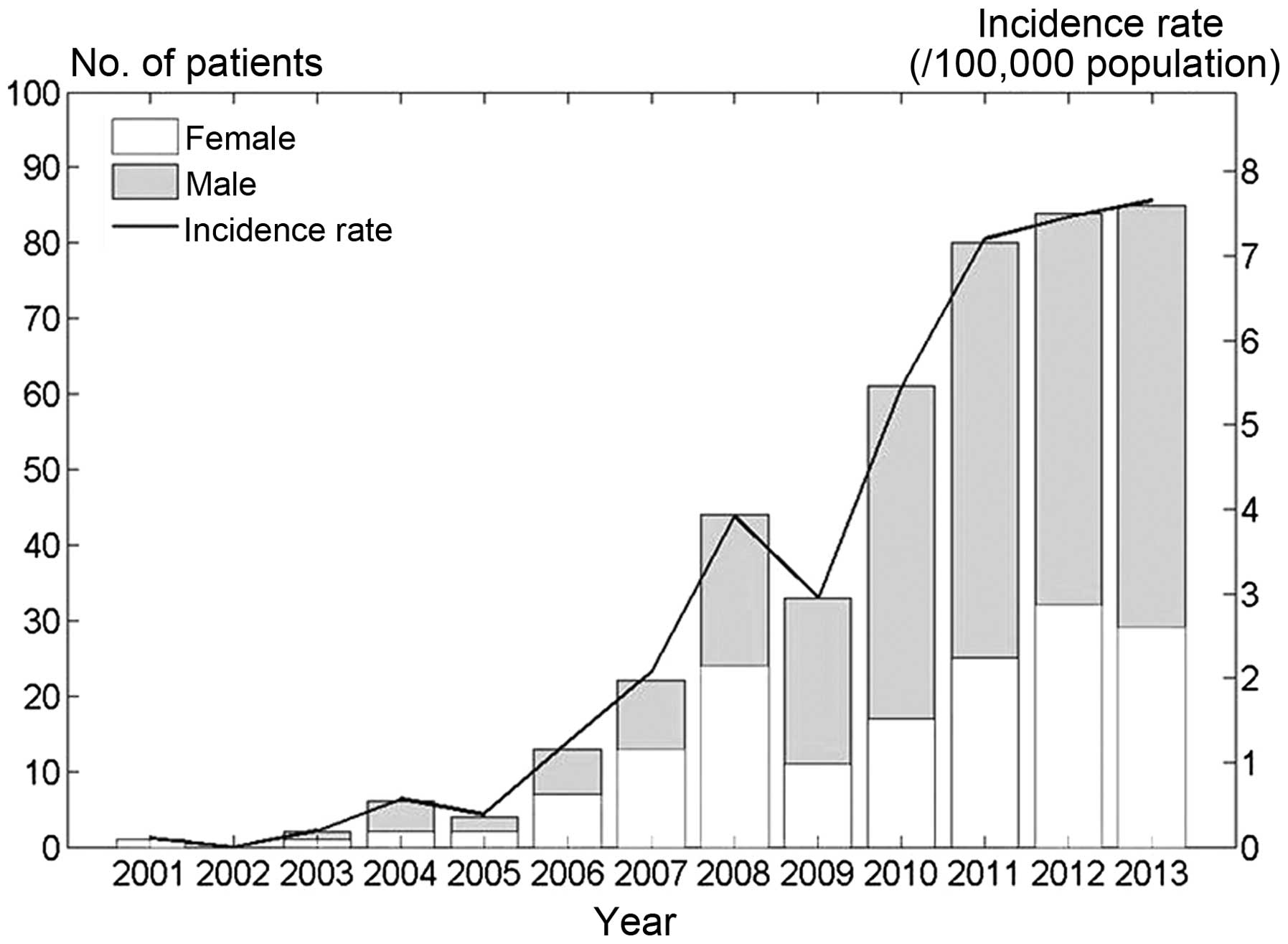
Incidence of KD
A total of 597 KD cases were identified in the
medical records of the included hospitals within the study period.
Of these, 79 cases were excluded through strict quality control,
due to not meeting the study criteria. The remaining 518 KD cases
were enrolled in the present study population. The number of
patients with KD per year, as well as the determined incidence
rates in the surveys, are shown in Fig.
1. Based on the Statistical Yearbook data for Inner Mongolia
(6), the mean annual incidence rate
of KD was 3.55±2.96 per 100,000 children under the age of 5 years
between 2001 and 2013, and the incidence displayed an increasing
trend over this time period. There were 322 (62.2%) males and 196
(37.8%) females, with a gender ratio of 1.64:1, respectively. The
majority of included KD patients were Han Chinese. Three minority
groups were represented by 81 cases (15.8%), including 70
Mongolian, 6 Hui and 5 Manchu patients, and these groups were
dispersed throughout the surveyed population.
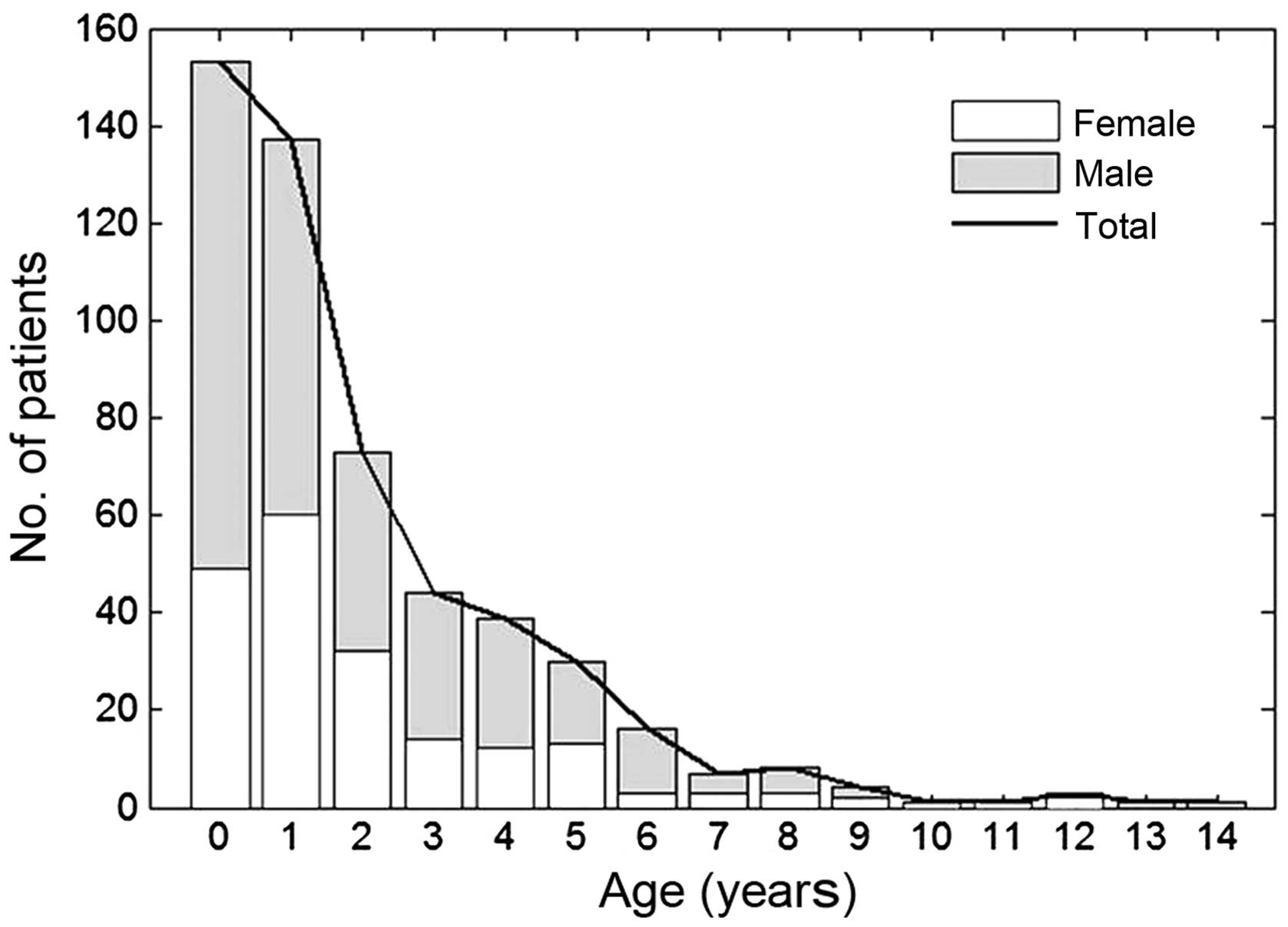
Distribution of age at diagnosis of
KD
The distribution of age at diagnosis of KD is shown
in Fig. 2. The age at diagnosis of
KD, which was derived from the date of the first diagnosis (within
one month of symptom onset) minus the date of birth, ranged between
49 days and 14 years (median, 1.42 years). Cases under the age of 1
year and under the age of 5 years accounted for 56.0% (290 cases)
and 86.1% (446 cases), respectively, of the patient cohort. The
incidence rate was highest among children aged 0–1 years, after
which the incidence decreased sharply with increasing age.
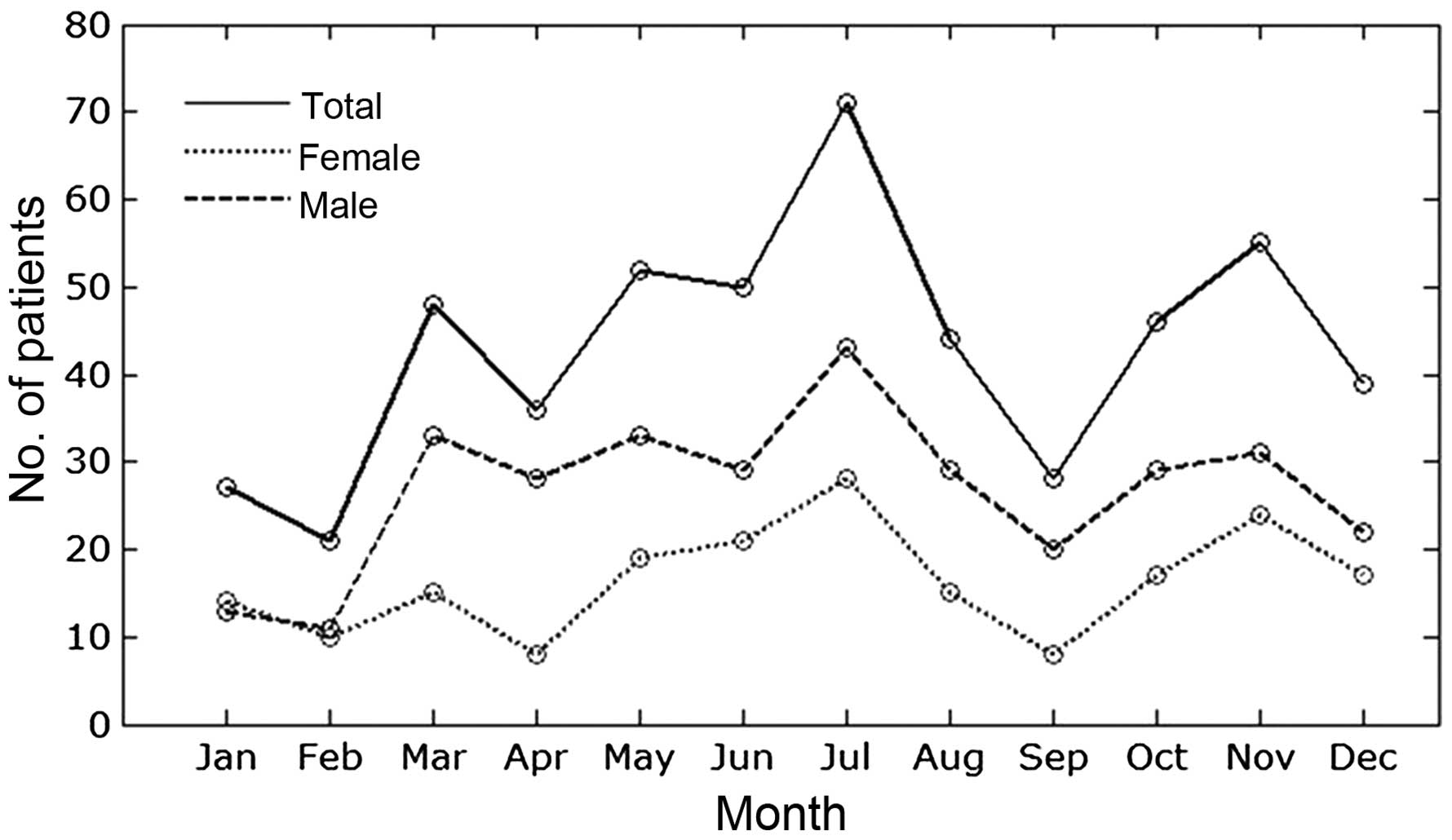
Monthly distribution of KD
Trends in the monthly number of patients are shown
in Fig. 3. During the survey period,
the onset of KD in all patients occurred more frequently in March
(48 cases;9.2%), May (52 cases; 10.0%), July (71 cases; 13.7%) and
November (55 cases; 10.6%), whereas it occurred relatively less
frequently in February (21 cases; 4.1%). Furthermore, the incidence
peak for boys and girls both occurred in July (43 cases, 13.4% and
28 cases, 14.3%, respectively).
Clinical manifestations of KD
Among the main clinical manifestations of patients
with KD in the present study, fever persisting for 5 days or longer
was the most frequent manifestation (516 cases; 99.6%), followed by
changes in the lips and oral cavity (383 cases; 73.9%),
conjunctival congestion (355 cases; 68.6%), polymorphous exanthema
(334 cases; 64.5%), changes in the peripheral extremities at the
initial or convalescent stages (322 cases; 62.1%), and acute
nonpurulent cervical lymphadenopathy (321 cases; 61.9%). Other
manifestations included perianal desquamation (118 cases; 22.8%),
coughing (63 cases; 12.2%), diarrhea (17 cases; 3.3%), and emesis
(12 cases; 2.3%). Respiratory system disorders were identified in
186 cases (35.9%) and liver impairments were observed in 20 cases
(3.9%). Mortality did not occur in any of the cases during the
acute and subacute stages of the disease.
Echocardiographic findings of KD
Echocardiographic examinations were performed in 501
cases (96.7%) within one month after the onset of KD. Among these
patients, abnormal findings were observed in 230 cases (45.9%),
including coronary artery ectasia (203 cases; 40.5%), coronary
artery aneurysm (2 cases; 0.87%), pericardial effusion (13 cases;
5.7%), mitral regurgitation (24 cases; 4.8%), tricuspid
regurgitation (12 cases; 2.4%), patent foramen ovale (11 cases;
2.2%) and patent ductus arteriosus (6 cases; 1.2%). In total, CAL,
defined as ectasia or aneurysm, was observed in 40.9% of all cases
undergoing echocardiographic examination. In certain patients,
various cardiac abnormalities were identified simultaneously.
Therapies and prognosis
Treatment with intravenous immunoglobulin infusion
(human freeze-dried low-pH intravenous gamma globulin; Biochemical
Product Institute of Ministry of Public Health, Chengdu, China) was
performed in 433 patients (83.6%) within one month after KD onset.
The regimens administered to patients included 400 mg/kg/day for 5
consecutive days in 6 cases (1.4%), 1,000 mg/kg twice in 156 cases
(36.0%), 2,000 mg/kg once in 70 cases (16.2%), and an irregular
dose in 154 cases (35.6%). Among these, the treatment regimen of
1,000 mg/kg/day twice was adopted more frequently. No adverse
effects due to this treatment were identified in the current study.
Besides intravenous immunoglobulin therapy, aspirin was
administered orally in 455 cases, and steroids were administrated
in 31 cases. In total, 310 patients were improved after treatment
and were discharged from the hospital, whereas 14 patients were
transferred to a higher level hospital and 194 patients were
discharged without medical advice due to various limitations, such
as financial difficulties and poorly conditioned local medical
institutions.
Risk factors of CAL
Single-factor analysis of risk factors relevant to
CAL incidence was conducted with a focus on patient age, gender,
ethnic group, month of onset, duration of fever (≥5 days), white
blood cell count (≥12×109/l), hemoglobin level (<100
g/l), blood platelet count (≥450×109/l), erythrocyte
sedimentation rate (≥40 mm/h) and creatine kinase-MB level (≥25
U/l). The results of the analysis indicated that ethnic group and
month of onset were associated with the occurrence of CAL, as shown
in Table I.
 | Table I.Single-factor analysis of the relevant
factors for CAL among the included 518 patients with Kawasaki
disease in the Inner Mongolia region between 2001 and 2013. |
Table I.
Single-factor analysis of the relevant
factors for CAL among the included 518 patients with Kawasaki
disease in the Inner Mongolia region between 2001 and 2013.
| Observed
indicator | χ2
test | P-value |
|---|
| Age of ≥5 years |
0.245 | 0.620 |
| Gender |
0.099 | 0.782 |
| Ethnic group |
4.657 | 0.031a |
| Month of onset | 21.040 | 0.029a |
| Fever duration of ≥5
days |
1.010 | 0.315 |
| White blood cell
count of ≥12×109/l |
0.437 | 0.508 |
| Hemoglobin level of
<100 g/l |
3.274 | 0.070 |
| Blood platelet count
of ≥450×109/l |
1.334 | 0.248 |
| Erythrocyte
sedimentation rate of ≥40 mm/h |
1.170 | 0.279 |
| Creatine kinase-MB
level of ≥25 U/l |
0.528 | 0.473 |
Furthermore, nonconditional multivariate logistic
regression analysis was conducted for a single factor that was
associated with CAL in KD. The Han Chinese ethnic group and July as
the month of onset were selected for the multivariate logistic
regression equation, and the corresponding P-values were found to
be <0.05 (Table II). These
results indicated that KD patients in the Han ethnic group were
more likely to be complicated by CAL, whereas KD patients with
onset occurring in July were less likely to be complicated by CAL.
This may be due to climatic and environmental conditions, or living
habits during different months, which may affect incidence;
however, the possibility that this association was coincidental
cannot be ruled out.
 | Table II.Nonconditional multivariate logistic
regression analysis of Kawasaki disease complicated by coronary
artery lesion among the included 518 patients with Kawasaki disease
in the Inner Mongolia region between 2001 and 2013. |
Table II.
Nonconditional multivariate logistic
regression analysis of Kawasaki disease complicated by coronary
artery lesion among the included 518 patients with Kawasaki disease
in the Inner Mongolia region between 2001 and 2013.
| Factor | Partial regression
coefficient | OR | 95% CI | P-value |
|---|
| Ethnic group (Han
Chinese) |
0.736 | 2.087 | 1.083–4.02 | 0.028a |
| Month of onset
(July) | −0.881 | 0.414 |
0.199–0.864 | 0.019a |
Discussion
KD was first recognized in 1967 (1); however, the etiology of the disease
remains unclear. Various researchers have hypothesized that
infectious agents may trigger the onset of KD (7,8),
however, no certain conclusion can be reached. Therefore, a
large-scale epidemiologic survey is required to identify clues
regarding the etiology and pathogenesis of KD. Currently, KD has
been reported in >60 countries and districts, including in Asia,
Middle East, America, Africa and Europe (3). The incidence rate appears to be the
highest in Japan, followed by East Asian countries and districts,
such as China, Hong Kong, Taiwan, and Korea, with an increasing
trend in numerous countries (3).
According to the results of the present 13-year
survey conducted on KD cases between 2001 and 2013, the incidence
rate was found to be increasing in Inner Mongolia during the study
period, and the latest incidence rate was reported to be 7.7 per
100,000 children in 2013. The increasing trend has also previously
been reported in other countries, districts and different regions
of China (9–13). However, the awareness of this disease
has increased among physicians during the time span, which may
affect the accuracy of reported incidences of KD. Therefore,
continuous monitoring of KD is important to better understand the
incidence trend of this disease.
Regarding the age distribution of patients at onset
of KD, the present data demonstrated that the disease predominantly
occurred in children under the age of 5 years, which accounted for
86.1% of the KD cases, and the peak age of KD onset was 0–1 years
(56.0%). These findings are in consistency with previous reports,
while the male preponderance observed in the current study (male to
female ratio, 1.64:1) was also comparable with previously studies
from other regions of China (5,9–13).
As seasonal variation may be an important
epidemiology characteristic of KD (3), the current study also focused on the
seasonality of KD. According to the present results, the disease
occurred all the year around, but more frequently in March, May to
July, and November. The incidence appeared to peak in July, with
the lowest point appearing in February. The seasonal distribution
of KD occurrence in the present study is similar to that reported
in a survey performed in Jilin province in China (5). However, great seasonal distribution
discrepancies have been reported in studies involving different
countries. For instance, in Japan, the number of patients was
highest in January and lowest in October (14). In Korea, the majority of KD cases
occurred in June, July and August, followed by December and January
(15). In the United States,
seasonal peaks in KD occurrence were observed in the winter and
spring months (16), whereas in
several European counties including England, Denmark and Ireland,
there was a similar peak occurrence of KD in the winter months
(17–19). Although seasonal distribution has
been perceived as an important characteristic of descriptive
epidemiology, the reasons for these discrepancies remain unclear.
Different climatic and environmental conditions, ethnic group and
living habits may possibly contribute to these discrepancies.
In consistency with previous studies (5,10–13),
fever persisting for 5 days or longer was the most frequent
clinical manifestation of KD, followed by changes in the lips and
oral cavity, conjunctival congestion, polymorphous exanthema,
changes in peripheral extremities and acute nonpurulent cervical
lymphadenopathy. Notably, although perianal desquamation is not
included in the diagnostic criteria of KD, it was observed in 22.8%
of the cases included in the present study, and a relative higher
incidence of perianal desquamation was also showed in several other
studies (5,11,20). As
a systemic vasculitis, the present study also identified that KD
affects multiple systems, including the respiratory and digestive
system, and in certain cases, atypical clinical manifestations may
lead to the misdiagnosis of KD (21); therefore, increased awareness of the
spectrum of the clinical presentation of KD is essential for early
diagnosis and treatment.
CAL is the most severe complication and a great
health concern in KD patients. The incidence of CAL was reported to
be 40.2% in the present survey during the acute stage, which was
comparable with the rates reported by Baer et al (22) and Zhang et al (5). However, the rate reported in the
present study was relatively high when compared with that of
certain other reports (9,11,13,16,23),
which may be due to the delayed diagnosis and treatment as a result
of the relatively lower economic level of the Inner Mongolia
region. In addition, this inconsistency in CAL incidence may be due
to differences in ethnicity and region, as well as discrepancy
brought by multifarious diagnostic standards. Besides, regarding
risk factors of CAL in patients with KD, the present study
indicated that patients in the Han ethnic group were more likely to
be complicated by CAL, whereas KD patients whose month of onset was
in July were less likely to be complicated by CAL; however, further
studies are required to further investigate the underlying reasons
for these observations.
It has been reported that intravenous immunoglobulin
treatment is able to significantly relieve clinical symptoms and
reduce the rate of CAL; therefore, it has become the main treatment
for KD (24–27). In the current survey, 83.6% of the
cases received treatment with intravenous immunoglobulin infusion
within one month after KD onset. However, the optimal time window,
dosage and the mechanism of the pharmacological effects of this
treatment remain arguable (27,28), and
require further exploration.
There are certain limitations in the current study.
Firstly, the retrospective nature of the study and the reliance on
data from numerous different centers may affect the accuracy of the
study. In addition, certain patients may not be included among the
target hospitals for the survey due to misdiagnosis, economic
limitations and lack of hospital space or of pediatric departments;
the effects of these on the overall results are unlikely to be
substantial.
In conclusion, the present study reported that the
number of patients and incidence rate of KD in Inner Mongolia tend
to increase year by year. The age distribution and clinical
manifestations were similar to those reported in previous studies
involving different region of China. Furthermore, the present study
reported that the onset of KD was more frequent in spring and
summer, and a higher incidence of CAL was reported in comparison
with other studies. Ethnic group and month of onset were also found
to be associated with the incidence of CAL in KD patients.
Continues monitoring of KD and further studies focusing on
identifying the etiology of KD are required to facilitate early
diagnosis and more specific treatment of KD, therefore decreasing
its morbidity and mortality rates.
Acknowledgements
The authors would like to thank all the hospitals
and pediatricians participating in the present survey, and
particularly thank the following hospitals: Maternal and Child
Health Hospital of Inner Mongolia, Inner Mongolia Medical
University Affiliated Hospital, Ordos Center Hospital, Chifeng City
Hospital and Tongliao City Hospital.
Glossary
Abbreviations
Abbreviations:
|
KD
|
Kawasaki disease
|
|
CAL
|
coronary artery lesion
|
References
|
1
|
Kawasaki T: Acute febrile mucocutaneous
syndrome with lymphoid involvement with specific desquamation of
the fingers and toes in children. Arerugi. 16:178–222. 1967.(In
Japanese). PubMed/NCBI
|
|
2
|
Ayusawa M, Sonobe T, Uemura S, Ogawa S,
Nakamura Y, Kiyosawa N and Harada K: Kawasaki Disease Research
Committee: Revision of diagnostic guidelines for Kawasaki disease
(the 5th revised edition). Pediatr Int. 47:232–234. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Uehara R and Belay ED: Epidemiology of
Kawasaki disease in Asia, Europe and the United States. J
Epidemiol. 22:79–85. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kuo HC, Yang KD, Chang WC, Ger LP and
Hsieh KS: Kawasaki disease: An update on diagnosis and treatment.
Pediatr Neonatol. 53:4–11. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhang X, Zhang Z, Liu S and Sun J:
Epidemiologic survey of Kawasaki disease in Jilin from 1999 through
2008. Pediatr Cardiol. 33:272–279. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Inner Mongolia Autonomous Region Bureau of
Statistics. Inner Mongolia Statistical Yearbook 2001–2013. China
Statistical Publishing House. (Beijing). 2013.
|
|
7
|
Shibuya N, Shibuya K, Kato H and
Yanagisawa M: Kawasaki disease before Kawasaki at Tokyo University
Hospital. Pediatrics. 110:e172002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nakamura Y, Yashiro M, Uehara R, Sadakane
A, Chihara I, Aoyama Y, Kotani K and Yanagawa H: Epidemiologic
features of Kawasaki disease in Japan: Results of the 2007–2008
nationwide survey. J Epidemiol. 20:302–307. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Du ZD, Zhao D, Du J, Zhang YL, Lin Y, Liu
C and Zhang T: Beijing Kawasaki Research Group: Epidemiologic study
on Kawasaki disease in Beijing from 2000 through 2004. Pediatr
Infect Dis J. 26:449–451. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Huang WC, Huang LM, Chang IS, Chang LY,
Chiang BL, Chen PJ, Wu MH, Lue HC and Lee CY: Epidemiologic
features of Kawasaki disease in Taiwan, 2003–2006. Pediatrics.
123:e401–e405. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ma XJ, Yu CY, Huang M, Chen SB, Huang MR
and Huang GY: Shanghai Kawasaki Research Group: Epidemiologic
features of Kawasaki disease in Shanghai from 2003 through 2007.
Chin Med J (Engl). 123:2629–2634. 2010.PubMed/NCBI
|
|
12
|
Li XH, Li XJ, Li H, Xu M and Zhou M:
Epidemiological survey of Kawasaki disease in Sichuan province of
China. J Trop Pediatr. 54:133–136. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ng YM, Sung RY, So LY, Fong NC, Ho MH,
Cheng YW, Lee SH, Mak WC, Wong DM, Yam MC, et al: Kawasaki disease
in Hong Kong, 1994 to 2000. Hong Kong Med J. 11:331–335.
2005.PubMed/NCBI
|
|
14
|
Nakamura Y, Yashiro M, Uehara R, Sadakane
A, Tsuboi S, Aoyama Y, Kotani K, Tsogzolbaatar EO and Yanagawa H:
Epidemiologic features of Kawasaki disease in Japan: Results of the
2009–2010 nationwide survey. J Epidemiol. 22:216–221. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kim GB, Han JW, Park YW, Song MS, Hong YM,
Cha SH, Kim DS and Park S: Epidemiologic features of Kawasaki
disease in South Korea: Data from nationwide survey, 2009–2011.
Pediatr Infect Dis J. 33:24–27. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Holman RC, Belay ED, Christensen KY,
Folkema AM, Steiner CA and Schonberger LB: Hospitalizations for
Kawasaki syndrome among children in the United States, 1997–2007.
Pediatr Infect Dis J. 29:483–488. 2010.PubMed/NCBI
|
|
17
|
Harnden A, Mayon-White R, Perera R, Yeates
D, Goldacre M and Burgner D: Kawasaki disease in England:
Ethnicity, deprivation and respiratory pathogens. Pediatr Infect
Dis J. 28:21–24. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Fischer TK, Holman RC, Yorita KL, Belay
ED, Melbye M and Koch A: Kawasaki syndrome in Denmark. Pediatr
Infect Dis J. 26:411–415. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lynch M, Holman RC, Mulligan A, Belay ED
and Schonberger LB: Kawasaki syndrome hospitalizations in Ireland,
1996 through 2000. Pediatr Infect Dis J. 22:959–963. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Huang GY, Ma XJ, Huang M, Chen SB, Huang
MR, Gui YH, Ning SB, Zhang TH, Du ZD, Yanagawa H and Kawasaki T:
Epidemiologic pictures of Kawasaki disease in Shanghai from 1998
through 2002. J Epidemiol. 16:9–14. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Royle J, Burgner D and Curtis N: The
diagnosis and management of Kawasaki disease. J Paediatr Child
Health. 41:87–93. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Baer AZ, Rubin LG, Shapiro CA, Sood SK,
Rajan S, Shapir Y, Romano A and Bierman FZ: Prevalence of coronary
artery lesions on the initial echocardiogram in Kawasaki syndrome.
Arch Pediatr Adolesc Med. 160:686–690. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Belay ED, Maddox RA, Holman RC, Curns AT,
Ballah K and Schonberger LB: Kawasaki syndrome and risk factors for
coronary artery abnormalities: United States, 1994–2003. Pediatr
Infect Dis J. 25:245–249. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Newburger JW, Takahashi M, Beiser AS,
Burns JC, Bastian J, Chung KJ, Colan SD, Duffy CE, Fulton DR and
Glode MP: A single intravenous infusion of gamma globulin as
compared with four infusions in the treatment of acute Kawasaki
syndrome. N Engl J Med. 324:1633–1639. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Terai M and Shulman ST: Prevalence of
coronary artery abnormalities in Kawasaki disease is highly
dependent on gamma globulin dose but independent of salicylate
dose. J Pediatr. 131:888–893. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Oates-Whitehead RM, Baumer JH, Haines L,
Love S, Maconochie IK, Gupta A, Roman K, Dua JS and Flynn I:
Intravenous immunoglobulin for the treatment of Kawasaki disease in
children. Cochrane Database Syst Rev: CD004000. 2003. View Article : Google Scholar
|
|
27
|
Baba R, Shibata A and Tsurusawa M: Single
high-dose intravenous immunoglobulin therapy for Kawasaki disease
increases plasma viscosity. Circ J. 69:962–964. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Rigante D, Valentini P, Rizzo D, Leo A, De
Rosa G, Onesimo R, De Nisco A, Angelone DF, Compagnone A and Delogu
AB: Responsiveness to intravenous immunoglobulins and occurrence of
coronary artery abnormalities in a single-center cohort of Italian
patients with Kawasaki syndrome. Rheumatol Int. 30:841–846. 2010.
View Article : Google Scholar : PubMed/NCBI
|